Abstract
We investigated factors hypothesized to moderate the effects of cognitive behavioral group-based (CB group) and bibliotherapy depression prevention programs. Using data from two trials (N = 631) wherein adolescents (M age = 15.5, 62% female, 61% Caucasian) with depressive symptoms were randomized into CB group, CB bibliotherapy, or an educational brochure control condition, we evaluated the moderating effects of individual, demographic, and environmental factors on depressive symptom reductions and major depressive disorder (MDD) onset over 2-year follow-up. CB group and bibliotherapy participants had lower depressive symptoms than controls at posttest but these effects did not persist. No MDD prevention effects were present in the merged data. Relative to controls, elevated depressive symptoms and motivation to reduce depression amplified posttest depressive symptom reduction for CB group, and elevated baseline symptoms amplified posttest symptom reduction effects of CB bibliotherapy. Conversely, elevated substance use mitigated the effectiveness of CB group relative to controls on MDD onset over follow-up. Findings suggest that both CB prevention programs are more beneficial for youth with at least moderate depressive symptoms, and that CB group is more effective for youth motivated to reduce their symptoms. Results also imply that substance use reduces the effectiveness of CB group-based depression prevention.
Keywords: Depression, Prevention, Adolescence, Cognitive-behavioral, Moderators
Depression is one of the most prevalent psychiatric disorders experienced by adolescents and often recurs during adulthood (Costello, Mustillo, Erkanli, Keeler, & Angold, 2003). Adolescent depression is associated with suicidal behavior, substance abuse, interpersonal problems, academic failure, and comorbid psychopathology (e.g., Klein, Torpey, & Bufferd, 2008). Despite the significance of depressive disorders, less than 50% of depressed adolescents receive treatment (Kessler, Avenevoli, & Ries Merikangas, 2001), suggesting the need for effective depression prevention programs that could be widely implemented.
Various cognitive-behavioral (CB) depression prevention programs have reduced depressive symptoms and future depressive disorder onset in adolescents, but the average magnitudes of effect have been small to moderate, with smaller average effects for universal versus selective or indicated programs (Horowitz & Garber, 2006; Stice, Shaw, Bohon, Marti, & Rohde, 2009). However, the effectiveness of such programs can vary considerably depending on individual, environmental, and demographic factors, highlighting the need to investigate potential moderators of depression prevention program effects, a central concept in personalized medicine. Moderational analyses are important for several reasons. First, knowledge about moderators provides information regarding the conditions under which optimal prevention effects occur. Second, neglecting potential moderators of prevention effects can lead to misinterpretation of results (Tram & Cole, 2000). Third, determining which individuals are most or least likely to benefit from an intervention can inform optimum inclusion and exclusion criteria. For instance, through moderation analyses youth that are unlikely to benefit from a specific prevention program or even experience iatrogenic effects can be identified, and this may provide direction regarding alternative intervention for those individuals. Fourth, moderation analyses may also lead to program refinement because important aspects that contribute to the effectiveness of a program for a specific population can be discovered. Conversely, documenting that there are few moderators for an intervention in an adequately powered evaluation would suggest that the intervention is effective for a broad range of individuals and could be widely implemented. Information about all of these aspects helps to maximize economical and cost-effective program dissemination. Thus, moderators can serve to provide specific, novel, and valuable information which guides future modification of intervention decision making and program development.
We examine potential moderators of the effects of a 6-hour CB depression prevention group program and an individual CB bibliotherapy program relative to an educational brochure control condition and to each other among adolescents with elevated depressive symptoms. The approach taken has several strengths that allow us to extend previous literature. First, by examining two active interventions relative to each other and a control condition, it is possible to directly compare which of the two active interventions works best for participants with certain characteristics. Second, the availability of data through 2-year follow-up makes it possible to identify moderators that affect program effects on a long-term basis. Third, by focusing on two outcomes – depressive symptom severity and major depressive disorder (MDD) onset – we evaluate potential subgroup effects on two critical prevention outcomes. Whereas depressive symptom severity as an outcome has been investigated in several moderation studies (e.g., Curry et al., 2006; Garber et al., 2009; Gau, Stice, Rohde, & Seeley, 2012), to our knowledge, only one previous study has examined moderators of the effect of depression prevention programs on depressive disorder onset (Garber et al., 2009); these investigators examined whether current parental depression, current adolescent depressive symptoms and adolescent history of mood disorder moderated the impact of CB prevention on depressive disorder onset, finding that current parental depression reduced the efficacy of CB group, a moderating effect that persisted over follow-up (Beardslee et al., 2013). Although reduction of depressive symptoms is an important objective of depression prevention programs especially in selective and indicated programs, the ultimate goal of depression prevention efforts is the prevention of depressive disorder onset. Therefore, it is vital to extend previous literature examining moderators of depressive symptom reductions by also investigating moderators of depression onset. Fourth, as previous moderation analyses have generally been conducted with data from a single trial and subsequently had limited power to identify moderators, we created a merged data set from a large efficacy trial (Stice, Rohde, Seeley, & Gau, 2008) and a large effectiveness trial (Rohde, Stice, Shaw, & Brière, 2014). Merging data sets provides us with the opportunity to investigate moderating effects of the depression prevention programs on MDD onset in a more adequately powered sample. Merging data results in higher statistical power from larger sample size and a greater representation of specific subgroups and risk factors. This maximizes sensitivity to detect moderating effects. Furthermore, pooling data from multiple trials provides a cost- and resource-effective alternative to gather information prior to collecting new data on the effectiveness of a specific program.
The efficacy trial investigated a 6-hour CB depression prevention group program, an individual CB bibliotherapy program, and a supportive-expressive group intervention versus an educational brochure control condition in 341 adolescents with elevated depressive symptoms (Stice, Rohde, et al., 2008). At posttest, CB group participants showed significantly greater depressive symptom reductions than participants in all other conditions. All three interventions led to significantly greater symptom reductions versus controls at 6-month follow-up. By 1-year follow-up, participants in the CB group showed significantly greater symptom reductions than controls and by 1- and 2-year follow-up also compared to CB bibliotherapy but not to supportive-expressive group participants. By 2-year follow-up, CB group and CB bibliotherapy participants showed significantly lower rates of major/minor depressive disorder onset than controls (Stice, Rohde, Gau, & Wade, 2010). The effectiveness trial tested whether the effects of these two CB prevention programs remained, relative to educational brochure controls, when school clinicians recruit adolescents with depressive symptoms and deliver the interventions under ecologically valid conditions with 378 adolescents with elevated depressive symptoms (Rohde, Stice, Shaw, & Brière, 2014). CB group participants scored lower on depressive symptoms than controls at posttest. By 6-month follow-up CB group participants showed a significantly lower MDD onset relative to bibliotherapy and control participants; this effect was maintained by 2-year follow-up comparing CB group to CB bibliotherapy, though the difference compared to controls did not reach significance (Rohde, Stice, Shaw, & Gau, in press).
The combined sample for this study included data from 631 participants assigned to three conditions (we did not include those randomized to supportive-expressive group because that condition was not included in the effectiveness trial) from 11 high schools in 2 regions of the US. We examine eight potential moderators of the effects of CB interventions on depressive symptoms: four individual factors (depressive symptom severity, substance use, motivation to reduce depression, attributional style), two sociodemographic factors (sex, age), and two environmental factors (social support from friends and family, negative life events).
Individual factors
First, we hypothesized stronger intervention effects for youth with higher initial depressive symptoms. Meta-analyses indicate that programs targeting participants with high initial symptoms typically produce stronger depressive symptom reductions than universal programs (Horowitz & Garber, 2006; Stice et al., 2009). Individual trials have also found that symptom reductions in prevention trials are stronger for participants with high versus low baseline symptoms (e.g., Jaycox, Reivich, Gillham, & Seligman, 1994; Spence, Sheffield, & Donovan, 2003; Tandon et al., 2015; Wilksch & Wade, 2014). Theoretically, those with elevated symptoms have greater potential to show symptom reductions. Moreover, those youth who already suffer from high depressive symptoms at baseline are able to apply the skills taught in the CB programs to their current negative mood state and cognitions, and are also more likely to experience a higher level of suffering which should lead to greater motivation to work on reducing their symptoms. Second, we anticipated stronger effects for participants with more initial motivation to reduce depressive symptoms. Readiness to change should provide motivation to participate in the program exercises and homework assignments, which should promote skill acquisition (Stice, Marti, Shaw, & O’Neil, 2008). Trials with various psychiatric disorders in adults have found that high motivation to reduce initial symptoms predicts participants’ treatment response (Keijsers, Schaap, Hoogduin, Hoogsteyns, & de Kemp, 1999) and that adolescents with higher motivation during participation in a depression prevention program experienced greater depressive symptom reductions at follow-up (Kindt, Kleinjan, Janssens, & Scholte, 2014). In our efficacy prevention trial, motivation to reduce depressive symptoms did not moderate program effects (Gau et al., 2012), but we expect that the larger data set used for this report will provide a more sensitive test of this potential moderator. Third, we hypothesized that substance use would moderate CB intervention effects with concurrent substance users benefitting less from the CB intervention than non-users. Depressive symptoms and substance use are correlated in youth (O’Neil, Conner, & Kendall, 2011) and substance use may contribute to depression onset and maintenance, possibly reducing participants’ motivation to apply the skills taught in the program (Brook, Brook, Zhang, Cohen, & Whiteman, 2002; Rohde, Lewinsohn, Kahler, Seeley, & Brown, 2001). Moreover, substance use predicted a poorer response to CB treatment in depressed adolescents (Gilbert, Fine, & Haley, 1994; Rohde et al., 2001). Fourth, we anticipated that negative attributional style would moderate the effects of CB programs, as those with a more negative attributional style would theoretically benefit more from the cognitive restructuring element of the CB interventions. In support, one depression treatment trial found that negative cognitive distortions moderated treatment outcomes (Curry et al., 2006) and another found that high and average baseline levels of hopelessness, a related concept, moderated intervention effects on depressive symptoms (Gillham et al., 2012).
Demographic factors
We hypothesized that sex would moderate the effects of the CB programs with females benefitting more from participation than males. Though the opposite pattern has emerged in some studies, depression prevention programs and interventions have generally produced stronger effects for females versus males in meta-analyses (Horowitz & Garber, 2006; Stice et al., 2009) and single trials (e.g., Donker et al., 2013; Gillham, Hamilton, Freres, Patton, & Gallop, 2006; Seligman, Schulman, DeRubeis, & Hollon, 1999). Theoretically this pattern of effects has emerged because female adolescents are approximately twice as likely to develop MDD (Nolen-Hoeksema & Girgus, 1994) and report greater depressive symptoms than male adolescents (e.g., Castelao & Kröner-Herweig, 2013). We also expected that CB program effects would be larger for older versus younger participants based on meta-analytic findings (Horowitz & Garber, 2006; Stice et al., 2009) and single trials (e.g., Stasiak, Hatcher, Frampton, & Merry, 2014). Older adolescents may have struggled with depressive symptoms for a longer duration, which might improve engagement in the interventions, and younger adolescents may have more difficulty understanding and implementing the CB skills conveyed in these programs.
Environmental factors
We hypothesized that individuals with less social support from parents and peers would show significantly greater depressive symptom reductions if they participated in the CB group intervention as previous research found that adolescents who experience low levels of parental support showed small but significant reductions in depressive symptoms if they had participated in a universal depression prevention program versus a control condition (Spence et al., 2014). Our hypothesis is further based on evidence that low social support increases the risk for depression in adolescents and young adults (Lewinsohn et al., 1994; Sheeber, Hops, & Davis, 2001). Finally, we hypothesized that elevated negative life events would mitigate CB program effects, based on previous trials indicating that negative life events reduced the effects of a CB group program (Gau et al., 2012) and predicted poorer response to CB treatment for depression in adults (Jayson, Wood, Kroll, Fraser, & Harrington, 1998). Even though strategies to detect and restructure negative thoughts regarding negative life events, and encouragement to engage in pleasant activities are major aspects of CB programs, we assume that the unfavorable effects of negative life events cannot completely be countered in relatively short prevention efforts.
In addition to investigating moderators of the effects of CB interventions on depressive symptoms, we also tested whether these factors moderated the effects of the two CB interventions on MDD onset. We expect the direction of moderation hypotheses of CB group and bibliotherapy on MDD onset to be the same as moderators on depressive symptoms for all of the examined factors. Specifically, we hypothesized that higher initial depressive symptoms, motivation to reduce depression, negative cognitive style, as well as female sex, older age, and lower social support, negative life events and substance use would lead to greater differences in MDD onset between CB intervention and control group participants.
Method
Participants and Procedure
For this report, we combined data from an efficacy trial (trial 1; Stice, Rohde, et al., 2008) and an effectiveness trial (trial 2; Rohde, Stice, Shaw, & Brière, 2014) involving high school students. In total, 631 participants between 13 and 19 years of age at pretest (M age = 15.5, SD = 1.20; 62% female) were randomized to one of the three conditions. The combined sample was composed of 2% Asian/Pacific Islander, 5% African American, 17% Hispanic, 1% Native American, 61% Caucasian, and 14% who specified other or mixed racial heritage. Parental education was 25% high school graduate or less, 24% some college, 32% college graduate, and 19% advanced graduate/professional degree. Thirty-three percent had received treatment in the 12-month period prior to enrollment. Rates of treatment did not differ by condition but were significantly higher in Study 2 (72% vs. 63%).
Participants were recruited at schools using direct mailings, flyers, and posters inviting students who experienced sadness to participate in a research study aiming to improve current and future mood and promote emotional well-being. Recruitment occurred between 2004–2007 (trial 1) and 2009–2011 (trial 2). Recruitment letters included a study description, consent forms and a 1-page screen assessing depressive symptoms using the Center for Epidemiologic Studies-Depression Scale (CES-D; Radloff, 1977) in trial 1, and a simplified 2-point response choice version in trial 2 (rarely/a little vs. occasionally/most of the time). Students who returned a signed consent form and scored 20 or above on the CES-D (trial 1) or endorsed two or more symptoms (trial 2) were invited to a pretest assessment with research staff to obtain baseline data and assess exclusion criteria (we could not estimate differences in CES-D levels for Studies 1 and 2 because the screener was completed in Study 2 prior to consent). All participants were given treatment referral information at study entry and advised to seek treatment if their symptoms escalated. Students who met criteria for MDD or acute suicidal ideation (n = 111) at pretest were excluded and project staff spoke with the student and contacted the parents to contract for safety, reiterate the importance of seeking treatment, and provide additional referral information.
All participants (N = 631) were randomly assigned to condition within blocks created by sex and school to one of the conditions: (a) CB group (n = 215), (b) CB bibliotherapy (n = 208), or educational brochure control (n = 208). They completed a survey and diagnostic interview at pretest, posttest, 6-month follow-up, 1-year follow-up, and 2-year follow-up (trial 1) and at the same timepoints with an additional 18-month follow-up in trial 2. They were paid for completing assessments. Assessments and groups were conducted at schools. The local institutional review boards approved this project.
Intervention Groups
CB group depression prevention program
The CB group program was identical in both trials, with the exception of a more scripted manual for facilitators in trial 2. The 6 weekly 1-hr sessions were conducted in single-sex groups of 5–9 participants at schools. Sessions focused on establishing group rapport, enhancing participants’ engagement in pleasant activities (e.g., generating a personal list of fun activities, rewards for engaging in these activities), and identifying negative cognitions in order to replace them with more positive ones (e.g., strategies such as “Where’s the Evidence?”). Motivational enhancement exercises, behavioral exercises, and group activities were used to support skill acquisition. Exercises were conducted in sessions (to apply the skills taught in the program) and as homework (to encourage participants to apply the skills in their daily life). Research clinicians facilitated groups in trial 1; school counselors or nurses facilitated groups in trial 2. If a participant missed a session, a brief (10–15 min) individual make-up session was conducted. Intervention content and facilitator training/supervision is presented in detail elsewhere (Rohde, Stice, Shaw, & Brière, 2014; Stice, Rohde, et al., 2008).
CB bibliotherapy
Participants in CB bibliotherapy were provided with the book Feeling Good (Burns, 1980) which is the only self-help book that met the criterion for probably efficacious treatment of depression (Malouff & Rooke, 2007) and has successfully been used in previous bibliotherapy studies for the treatment and prevention of depression in adults and adolescents (Gregory, Schwer Canning, Lee, & Wise, 2004; Jamison & Scogin, 1995). It provides relevant and practical CB techniques for preventing and reducing negative moods. Written at a high-school reading level, the book covers topics such as understanding feelings of sadness, building self-esteem, overcoming guilt, and coping with stress. Participants were told, “This book has been shown to be helpful to some individuals who are feeling sad or depressed. This copy is yours to keep, so feel free to write or highlight in it as you read. We encourage you to use this as a self-help resource.” In an effort to encourage utilization of the book, the school personnel in trial 2 were asked to make two brief scripted reminder phone calls to CB bibliotherapy participants encouraging them to continue or start reading the book and to complete as many exercises in the book as possible, but we did not track reminder calls.
Educational brochure control condition
Participants were given a National Institute of Mental Health brochure at pretest that describes depression and recommends treatment for depressed youth (National Institute of Mental Health, 2001), and information about local treatment options (as were all participants). Participants in this condition completed the same assessments as those in the other conditions, enabling us to monitor depression and suicidal ideation, and contact parents to provide treatment referrals as needed (done in all conditions). Participants and their parents were asked to contact research staff if they believed that the youth’s symptoms had worsened.
Measures
Depressive symptoms
Depressive symptoms were assessed by research staff using 16 items from the semistructured Schedule for Affective Disorder and Schizophrenia for School-Age Children (K-SADS; Puig-Antich & Chambers, 1983). No other parts of the K-SADS were administered in this study. Participants indicated the severity of each symptom over their lifetime (trial 1) or the past 12 months (trial 2) at baseline and since the last assessment on a monthly basis at subsequent assessments (trials 1 and 2). Items used an expanded response format (1 = not at all to 4 = severe symptoms; with ratings of 3 and 4 reflecting diagnostic levels). Severity ratings for each symptom were averaged, as was the case for the other scales. This measure has shown test-retest reliability (i.e., the same assessor interviewing a participant twice over a 1–2 week period) (κ = .63–1.00), inter-rater reliability (i.e., two assessors interviewing the same participant) for depression diagnosis (κ = .73–1.00), internal consistency (α = .68–.84), and predictive validity (Nolen-Hoeksema, Stice, Wade, & Bohon, 2007; Stice, Rohde, Seeley, & Gau, 2010). In trial 1 inter-rater reliability was κ = .83 for depression diagnoses and test-retest reliability was κ = .83. In trial 2 inter-rater reliability was κ = .98 at the item level and κ = 1.00 for depression diagnosis. Trial 2 showed test-retest reliability (κ = .99) and inter-item correlation for the continuous depressive symptom composite (ICC = .99). The present study showed inter-rater reliability for depression diagnoses (κ = .93) and inter-item correlation for the continuous depressive symptoms composite (ICC = .92). Assessors, blind to condition, had at least a BA in psychology, received 40 hours of training in semistructured interviews, and demonstrated high inter-rater agreement (κ ≥ 0.80) with expert raters using training interviews and interview role-plays. They also had to demonstrate inter-rater κ values ≥ 0.80 for a randomly selected 10% of taped interviews throughout the study.
Substance use
Substance use was assessed with 10 items (Stice, Barrera, & Chassin, 1998). Participants indicated the frequency of intake of beer/wine/wine coolers/hard liquor over the past 30 days; their frequency of heavy drinking (five or more drinks in a row); frequency of times drunk; and frequency of use of marijuana, stimulants, downers, inhalants, and hallucinogens using a 6-point response scale ranging from 0 (never) to 5 (3 to 7 times a week). This scale has shown internal consistency (α = .79), 1-year test-retest reliability (r = .72), and predictive validity (Stice, Rohde, Seeley, et al., 2010; α = .79 at baseline).
Motivation to reduce depression
Motivation to reduce depression was assessed with a 4-item scale (e.g. “I have been struggling with the feeling of depression for a long time and am really ready to tackle this problem now”) using a 5-point response format developed by our workgroup (Gau et al., 2012). It has shown internal consistency (α = .93) and 1-week test-retest reliability of r = .83 (Gau et al., 2012; α = .88 at baseline).
Negative attributional style
A short version of the Adolescent Cognitive Style Questionnaire (ACSQ; Hankin & Abramson, 2002) assessed negative attributional style. For 12 hypothetical negative events, participants rated (a) the degree to which the cause of the negative event is internal, stable, and global, (b) the likelihood that further negative consequences will result from the negative event, and (c) the degree to which the negative event signifies that the person is fundamentally flawed. This 36-item scale has shown internal consistency (α = .82), 1- week test-retest reliability (r = .89), and correlates with BDI scores (r = .36; Stice, Rohde, Seeley, et al., 2010; α = .85 at baseline).
Perceived parental/peer support
Perceived peer and parental support was assessed using 12 items from the Network of Relationships Inventory (Furman & Buhrmester, 1985) assessing aspects of relationships (e.g., companionship, guidance, affection) between the adolescent and his/her peers and parents. This scale has shown internal consistency (α = .88), test-retest reliability (r = .69), and predictive validity (Burton, Stice, & Seeley, 2004; α = .89 and .88, for the parental and peer support scales at baseline).
Negative life events
Participants reported the occurrence of 14 negative life events during the past year (Lewinsohn et al., 1994). This scale has shown 1-week test-retest reliability (r = .90; Brière, Rohde, Shaw, & Stice, 2014) and predictive validity (Monroe, Rohde, Seeley, & Lewinsohn, 1999).
Preliminary Analysis and Statistical Methods
Distributions of the outcomes were examined for excessive violations of normality. Participants in the three conditions did not differ on demographics or outcomes at pretest. Rates of missing data for hypothesized moderators were 1–5%. Attrition for diagnostic data was 4% at posttest, 11% at 6-month, 11% at 1-year, and 15% at 2-year follow-up. Attrition did not differ between conditions (p-values > .20) or between Studies 1 and 2. On average participants completed 5.1 of 6 assessments (SD = 1.1). Attrition was not associated with any study variables except substance use (t[604] = 2.93, p = .009); those who completed all assessments had lower baseline substance use than those who did not. Thirty-five percent of participants reported receiving mental health treatment during the 2-year follow-ups; rates did not differ by condition or between Studies 1 and 2. Of those receiving treatment, 62% received individual therapy, 8% group or family therapy, 20% took medication, and 33% a combination of treatment types. Treatment type during the follow-up did not significantly differ by condition.
Changes in depressive symptoms were evaluated with random effects growth models and fit with SAS PROC MIXED. Change in symptoms from posttest to 2-year follow-up was the outcome with pretest depressive symptoms a covariate. The data is considered partially nested because group CB was administered in a group setting and CB bibliotherapy and brochure control was not. Therefore, data were nested within group and CB bibliotherapy and brochure control participants were each treated as their own group (Bauer, Sterba, & Hallfors, 2008). When constructing the longitudinal portion of the model we (a) examined empirical growth plots; (b) evaluated an unconditional means model; (c) fit an unconditional linear growth model; and (d) fit an unconditional linear plus quadratic growth model. Various longitudinal change models were compared using the Bayesian Information Criterion and the linear plus quadratic growth model showed superior fit. We conducted three planned contrasts: CB group (coded 1) versus controls (coded 0); CB bibliotherapy (coded 1) versus controls (coded 0); and CB group (coded 1) versus CB bibliotherapy (coded 0). We used multiple-imputation to replace missing values (Graham, 2009) using the IVEWare program. Missing data points were replaced with imputed data in 10 data sets, which were analyzed separately. Model parameters and standard errors were combined following Rubin (1987) as implemented in SAS PROC MIANALYZE. Effect sizes were estimated as d-statistics using pooled raw standard deviations and model parameters involving the condition effects with formulas provided by Feingold (2009, 2013). MDD incidence was examined using discrete-time hazard models. As hazard models were designed to accommodate right censoring, we did not impute missing MDD incidence data; however, we did use multiple imputed data for missing moderators. The model specified onset of MDD in months and fit with SAS PROC PROBIT (SAS Institute Inc., 2011) using a logit link function. We conducted three planned group contrasts described above.
The intercorrelations between hypothesized moderators are shown in Table 2. The average correlation among moderators was r = .13 (range = .01 – .35). Each moderator was tested in separate moderation models. For depressive symptom growth models the moderator main effect, and their interaction terms with condition, and linear and quadratic time scores were added. A significant condition by moderator interaction term would indicate the level of the moderator impacted the effect of the intervention from pretest to the posttest assessment; a significant condition by moderator by time (linear and quadratic) interaction would indicate the moderator impacted the magnitude of the effect of condition on change in the outcome from posttest to 2-year follow-up. For MDD incidence data the moderator main effect and interaction with condition were added to the discrete-time hazard models. A significant condition by moderator interaction term would indicate the moderator impacted the effect of condition on the risk of MDD onset. Significant interactions were probed by computing sample estimated intercepts and slope trajectories at conditional levels of the moderator for growth models and by comparing estimated probabilities at conditional levels of the moderator for hazard models. We selected values at one standard deviation (SD) below the mean-centered moderator, at the mean, and at one SD above the mean to represent low, moderate, and high levels of baseline moderator, respectively, following Aiken and West (1991).
Table 2.
Correlation Matrix for Pretest Hypothesized Moderators
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | ||
|---|---|---|---|---|---|---|---|---|---|
| 1 | MDD symptom score | 1.0 | |||||||
| 2 | Motivation to reduce depression | .31 | 1.0 | ||||||
| 3 | Attributional style | .35 | .31 | 1.0 | |||||
| 4 | Substance use | .15 | −.01 | .17 | 1.0 | ||||
| 5 | Major life events | .13 | .12 | .15 | .26 | 1.0 | |||
| 6 | Social support | −.29 | −.11 | −.29 | −.11 | −.17 | 1.0 | ||
| 7 | Sex | .12 | .07 | .03 | .03 | .01 | .01 | 1.0 | |
| 8 | Age | .07 | .08 | .13 | .14 | −.03 | −.05 | −.01 | 1.0 |
Prior to evaluating the impact of the hypothesized moderators on intervention effects we examined the potential influence of study (i.e., efficacy trial data versus effectiveness trial data) as a moderator of condition effects. Study did not moderate any effects involving condition for the depressive symptoms growth model, however, for the MDD incidence discrete-time hazard models significant condition by study interactions were found for the CB group versus CB bibliotherapy (estimate = 1.79, p = .017) and CB bibliotherapy versus control (estimate = −1.90, p = .008) comparisons. To control for the influence of study its main effect and interaction with condition were added to the discrete-time hazard models for comparisons involving CB bibliotherapy.
Results
Intervention Effects for Change in Depressive Symptoms
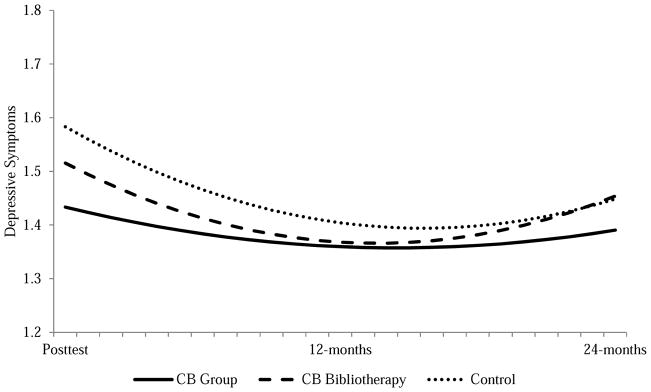
Table 1 shows the group means for depressive symptoms across assessments. Figure 1 presents the model-implied trajectories for depressive symptom change over follow-up. Comparing CB group to brochure control, condition had two significant effects. First, the condition effect (estimate = −.150; p < .001, d = .36, a moderately small effect) indicated that, compared to controls, CB group participants had lower depressive symptom scores at posttest. Second, the condition x time effect (estimate = .014, p = .015, d = .14, a small effect) was positive, indicating that the linear decrease for controls was more steep than for CB group participants, suggesting that controls began to catch up with CB group participants over follow-up. In the symptom contrasts comparing CB group versus CB bibliotherapy, CB group participants had significantly lower depressive symptom scores at the posttest assessment (estimate = −.081, p = .035, d = .20), reflecting a small effect. No other condition effects were significant.
Table 1.
Mean and Standard Deviations for Depressive Symptoms
| CB Group (n = 215) | CB Bibliotherapy (n = 208) | Brochure Control (n = 208) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Outcome measures | Mean | SD | 1% MDD | Mean | SD | % MDD | Mean | SD | % MDD |
| Depressive symptoms | |||||||||
| Pretest | 1.58 | 0.43 | 0.0 | 1.54 | 0.39 | 0.0 | 1.55 | 0.40 | 0.0 |
| Posttest | 1.45 | 0.33 | 0.5 | 1.54 | 0.40 | 2.9 | 1.58 | 0.40 | 4.8 |
| 6-mo follow-up | 1.36 | 0.39 | 2.8 | 1.33 | 0.36 | 4.8 | 1.45 | 0.43 | 8.7 |
| 12-mo follow-up | 1.39 | 0.39 | 7.4 | 1.41 | 0.44 | 10.6 | 1.42 | 0.43 | 12.0 |
| 18-mo follow-up | 1.35 | 0.33 | 8.4 | 1.39 | 0.41 | 13.5 | 1.38 | 0.34 | 14.4 |
| 24-mo follow-up | 1.41 | 0.39 | 10.7 | 1.44 | 0.45 | 16.8 | 1.45 | 0.43 | 17.3 |
Note. Means and standard deviations averaged across ten imputed data sets. Cumulative percent of cases that met criteria for major depressive disorder (MDD) from pretest through the 24-month follow-up period.
Figure 1.
Model implied depressive symptom severity trajectories for the three study groups.
Moderation of Intervention Effects in Depressive Symptoms
Two significant 2-way moderation interactions were found for the CB group versus control comparison; pretest depressive symptoms amplified the effects of condition at posttest (t [240] = 2.36, p = .018), as did baseline motivation to reduce depression (t [240] = 2.17, p = .030). Simple intercept analyses showed CB group participants had significantly lower posttest depressive symptoms for participants with high (adjusted posttest symptom level for CB group and brochure control = 1.56 and 1.77, respectively; t [240] = −4.60, p < .001, d = .50) and moderate (adjusted posttest symptom level for CB group and brochure control = 1.42 and 1.56, respectively; t [240] = −4.10, p < .001, d = .35) pretest depressive symptom levels versus controls, but for participants with low baseline symptom levels (adjusted posttest symptom level for CB group and brochure control = 1.29 and 1.35, respectively; t [240] = −1.38, p = .169, d = .15) the two conditions did not differ at posttest. Similarly, CB group participants had significantly lower posttest depressive symptoms for participants with high (adjusted posttest symptom level for CB group and brochure control = 1.65 and 1.45, respectively; t [240] = −4.58, p < .001, d = .48) and moderate (adjusted posttest symptom level for CB group and brochure control = 1.56 and 1.42, respectively; t [240] = −4.11, p < .001, d = .34) pretest levels of motivation to reduce depression versus controls, but not for participants with low motivation levels (adjusted posttest symptom level for CB group and brochure control = 1.40 and 1.47, respectively; t [240] = −1.53, p = .127, d = .17).
One 2-way interaction and one 3-way interaction emerged for the CB bibliotherapy versus control comparison; pretest depressive symptoms amplified the effects of condition at posttest (t [412] = 3.62, p < .001) and the effects of condition x linear change (t [1656] = −2.30, p = .021). Simple intercept analyses showed CB bibliotherapy participants had significantly lower posttest depressive symptoms versus controls for participants with high (adjusted posttest symptom level for CB bibliotherapy and brochure control = 1.60 and 1.81, respectively; t [412] = −3.96, p < .001, d = .45) and moderate (adjusted posttest symptom level for CB bibliotherapy and brochure control = 1.51 and 1.59, respectively; t [412] = −2.06, p = .039, d = .18) pretest depressive symptom levels, but for participants with low pretest symptom levels CB bibliotherapy participants had significantly higher scores at posttest (adjusted posttest symptom level for CB bibliotherapy and brochure control = 1.43 and 1.36, respectively; t [412] = 2.58, p = .010, d = .13) compared to controls. Graphs of simple slopes (Figure 2) show that CB bibliotherapy participants had similar linear change in depressive symptoms over follow-up compared to control participants at low and moderate levels of pretest depressive symptoms, but at high levels controls showed steeper linear decline in depressive symptoms over follow-up than CB bibliotherapy participants.
Figure 2.
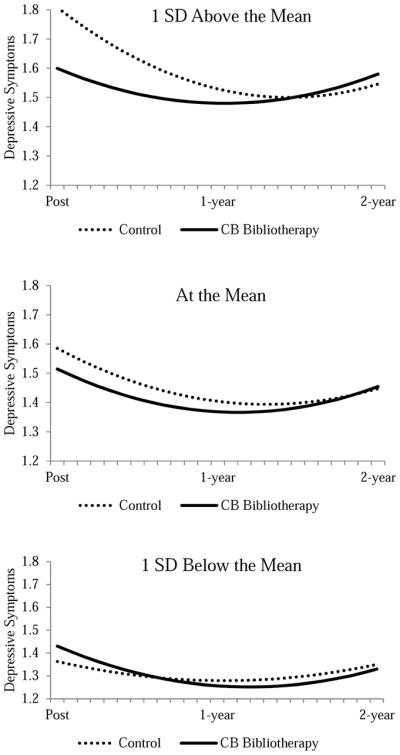
Simple slopes at low, medium, and high levels of pretest depressive symptoms for CB bibliotherapy versus brochure controls.
No significant moderating effects were detected for the CB group versus CB bibliotherapy comparison.
Intervention Effects for Major Depressive Disorder Onset
By 2-year follow-up, 84 participants (13%) showed MDD onset: 31 controls (15%), 31 CB bibliotherapy participants (15%), and 22 CB group participants (10%). Each condition contrast was entered separately as a predictor in the discrete-time hazard model to determine whether the risk of MDD onset during the course of the study (i.e., logit hazard function) differed by condition. No statistically significant group differences for MDD onset at 2-year follow-up were detected for the merged sample.
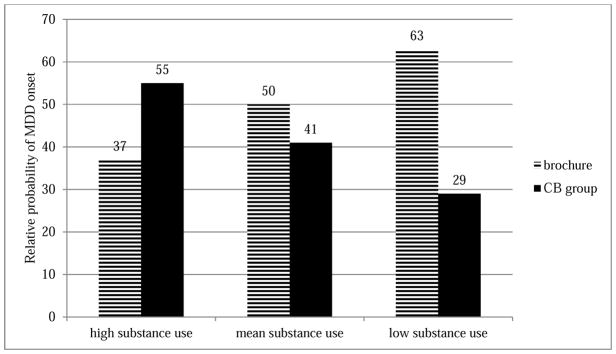
Moderation of Intervention Effects in Major Depressive Disorder Onset
One significant moderator x group effect was found: pretest substance use (which did not significantly differ by gender) moderated the logit hazard function for the CB group versus control contrast (odds = 2.95, p= .035), a medium-to-large effect. Logit parameters from the models were used to compute estimated probabilities of developing MDD for prototypical cases with comparisons made to a reference group (Figure 3). For the CB group versus brochure control comparison, the effect of CB group was weaker at high substance use levels, with CB group participants having an 18% higher likelihood of developing MDD than controls. Conversely, at low substance use levels the preventive effect of CB group was much stronger, with CB group participants having a 34% lower likelihood of developing MDD than controls.
Figure 3.
Interpretation of Significant Interaction Terms (Relative probability of MDD onset over 2-year follow-up). Brochure controls with mean substance use formed the reference group (50% probability) for the CB group vs. brochure controls contrast.
Discussion
Moderation of Intervention Effects in Depressive Symptom Reductions
Those receiving CB group had significantly lower depressive symptoms at posttest compared to both brochure controls (d = .52) and CB bibliotherapy participants (d = .27), reflecting a medium and small effect, respectively; symptom differences between CB bibliotherapy participants and brochure controls were nonsignificant at post and follow-up. Results also indicated that CB bibliotherapy participants and brochure controls caught up with CB group participants over time, consistent with both a regression to the mean effect and the natural remission of depression for most individuals, given time (data from representative samples of adolescents using this version of the depression interview are not available, so we do not know whether symptom levels were normalized or remain somewhat elevated). Our finding is in line with previous research by our group and others (e.g., Horowitz & Garber, 2006) that has shown that preventive effects of depressive symptoms tend to be strongest at posttest and often diminish over time. An implication of this finding could be that we do need to look at additional components that might enhance or prolong more long-term effects, for instance by introducing booster sessions.
Pretest depressive symptom levels amplified the effects of the CB group program on depressive symptom reductions versus brochure controls. CB group was superior to brochure control when adolescents entered the study with moderate or high baseline depressive symptoms but not low levels (the mean symptom level roughly corresponded to two full threshold MDD symptoms or four symptoms at subthreshold levels); the evaluated CB group was not beneficial for adolescents who are currently experiencing fewer depressive symptoms. Results converge with our hypothesis and align with evidence from past trials and meta-analyses that showed stronger effects for participants with higher versus lower initial symptoms (e.g., Jaycox et al., 1994, Horowitz & Garber, 2006; Stice et al., 2009). There are several potential explanations for this moderation effect, including the CB group being more appropriate for these youth because they have more opportunities to apply the CB skills to current negative cognitions and (consistent with the second moderation effect) a higher degree of clinical distress leading to increased motivation or readiness to change (e.g., the two variables were correlated r = .31 in the present study). Further, a statistical explanation for the emergence of this effect is that those with low initial symptoms may have less room for reductions than those with high initial symptoms.
Pretest depressive symptoms also showed a slightly stronger moderating effect of CB bibliotherapy versus brochure controls. Results suggest that CB bibliotherapy requires a minimum level of depressive symptoms (approximately two full threshold symptoms or four symptoms at subthreshold levels) for effectiveness. Fortunately, Figure 2 suggests that the course of depressive symptoms over follow-up for CB bibliotherapy and controls were nearly identical, implying that there were no long-term iatrogenic effects for CB bibliotherapy among the subset of participants with low depressive symptoms.
Elevated initial motivation to reduce depression likewise amplified the effects of the CB group program on depressive symptom reductions compared to brochure controls. This moderation effect is consistent with evidence that motivation to reduce symptoms predicted the response of patients to CB treatment (Keijsers et al., 1999) but is, to our knowledge, novel in the area of depression prevention. The fact that this moderating effect was not significant in the individual trials (Brière et al., 2014; Gau et al., 2012) highlights the value of merging data sets using identical measures to increase sensitivity to detect moderating effects, which can be small. Though more studies are needed to explore whether this moderation finding replicates, this result suggests that increasing participants’ motivation for engagement and change, for example by including motivational interviewing into the initial CB prevention program sessions, might be an appropriate way to enhance participants’ benefit from the program. As the current sample was combined from one efficacy and one effectiveness trial, it is important to note that study did not moderate any condition effects for the depressive symptoms growth model. This indicates that the findings on moderators reported herein are alike irrespective of whether a research clinician (trial 1) or a school counselor or nurse (trial 2) delivered the program.
No significant moderating effects were found over follow-up, and although CB group produced lower posttest depressive symptoms than CB bibliotherapy, none of the examined variables moderated the effects of CB group versus bibliotherapy on depressive symptom reductions. The two conditions differed on delivery modality but shared a CB content, and the lack of moderators implies that the examined variables had a similar impact on the effects of both CB-based approaches. The fact that both CB group and bibliotherapy were superior to brochure control at higher pretest depressive symptom levels suggests that the moderator of symptom severity may be more general rather than intervention specific. It seems intuitive that some youth would benefit from a group intervention whereas others would do best with an unassisted self-help book but we did not identify such moderators, if differences truly exist. Given the increased availability of unassisted internet-based programs for depression treatment and prevention (e.g., Van Voorhees et al., 2009), the issue of whether subgroups of at-risk adolescents do or do not benefit from self-guided programs requires more attention.
Moderation of Intervention Effects in MDD Onset
Unlike our previous single-trial results, we found no long-term depressive disorder prevention effects in the merged data set. This appears to be due to the differential disorder prevention effects for CB bibliotherapy (and to a lesser extent CB group) in the two trials. In the efficacy trial, CB bibliotherapy had a very low onset incidence of MDD and minor depression (3%) with both CB bibliotherapy and CB group (14%) having significantly lower rates of depression onset than brochure controls (23%). In the effectiveness trial, MDD onset by 2-year follow-up was significantly lower in CB group (10%) than CB bibliotherapy (25%) but did not significantly differ from brochure controls (17%). Merging data resulted in a 10% MDD incidence for CB group, which was not statistically superior to either CB bibliotherapy or brochure controls, which both had a 15% MDD incidence. Potentially, this nonsignificant effect for MDD onset occurred because of merging data from a tightly controlled efficacy trial and an effectiveness trial in which recruitment procedures were streamlined and high school counselors and nurses conducted the CB groups. As we noted (Rohde et al., in press), the lack of a significant MDD prevention effect for CB group versus brochure control implies that CB prevention may not be ready for dissemination for delivery by high school personnel.
A novel contribution of the present report is the findings on substance use as a moderator of MDD onset. For youth with low substance use, strong MDD preventive effects were evident for CB group versus controls: low substance-using adolescents assigned to CB group showed the lowest MDD onset whereas the low substance-using adolescents assigned to the educational brochure control condition showed higher MDD onset. Conversely, for adolescents who entered the study with high substance use (and depressive symptoms), MDD onset was intermediate and there was no indication that CB group reduced MDD onset; in fact, the opposite pattern was noted– this was the only instance in which CB group appeared to be potentially iatrogenic: MDD onset among adolescents with high substance use was nearly 50% higher if they were in the CB group versus receiving the brochure. A potential explanation for this finding might be that the depressive problems of youth with high substance abuse are primarily a consequence of their substance abuse, either because of impairments in functioning or a physiological response to the substances. If true, the risk of MDD onset might significantly decrease once the substance abuse is addressed. With regard to depression symptom reductions, we found no significant effect. As a frame of reference, 51% of participants reported no substance use at pretest and the mean baseline substance use score was 0.39, which would correspond to drinking one beer 1–3 times a month, whereas a high substance use score (0.97 = 1 SD over the M) could be obtained by consuming 2 or 3 alcohol drinks 1–2 times weekly in the past month. We had predicted that high substance use would dampen the effect of CB group on depressive symptom reductions and the degree to which CB group prevented MDD onset. Results align with prior evidence that substance abuse might be a factor that affects onset and/or maintenance of depressive symptoms and might decrease participants’ motivation to actively engage in the program and apply the skills (Brook et al., 2002; Gau et al., 2012). Consistent with the present findings, previous research has suggested that some individuals with substance use problems experience deterioration in both psychiatric symptoms and substance use following their participation in substance abuse prevention or treatment programs (Moos, 2005). Even though the CB group provides a powerful context for change for the majority of individuals, adolescents with high substance use might be more prone to experiencing negative outcomes that can occur in all social settings, such as confrontation, high emotional arousal and insufficient coping strategies, as well as frustration with their inability to keep up with other participants’ progress. Stagnation or deterioration of symptoms might account for the subsequent higher MDD onset rates observed in this subgroup. The current results suggest that adolescents with a confluence of elevated depression levels and substance use do not appear appropriate for a CB group focused on depression prevention and should probably receive help reducing their substance use prior to efforts aimed directly at reducing depressive symptoms.
No evidence of moderating effects emerged for the other five factors investigated in this study. This is perhaps most surprising with regard to the demographic factors sex and age that have emerged as moderators in previous meta-analyses (Horowitz & Garber, 2006; Stice et al., 2009), though replication of moderating effects can be especially difficult in prevention science (Supplee, Kelly, MacKinnon, & Barofsky, 2013). Another factor that may explain the lack of other moderating effects is the mixed nature of previous results. For instance, even though the majority of studies on sex as a moderator have shown stronger effects in females (e.g., Gillham et al., 2006; Seligman, Schulman, DeRubeis, & Hollon, 1999), there are also studies that report stronger effects in males (e.g., Clarke, Hawkins, Murphy, & Sheeber, 1993) or no moderation effect (e.g., Gillham et al., 2012). Some of the hypothesized moderators that did not produce significant effects (i.e., negative attributional style, negative life events, perceived social support from family and friends) were measured with short questionnaires and may have required more fine-grained assessment procedures to fully address the construct or detect moderation effects.
Several limitations should be considered when interpreting these findings. First, we relied on self-report data from interviews and surveys, raising the possibility of reporter bias. Second, we merged data from two trials that used slightly different approaches to recruitment and facilitation to maximize the sensitivity to detect moderation effects that can be small in magnitude. We cannot rule out the possibility that this approach introduced noise into the data. Third, CB bibliotherapy engagement in trial 1 was higher (e.g., 28% read at least half the book in trial 1 vs. 15% in trial 2). Although the book is long (over 600 pages), the general model of cognitive therapy for depression is presented to the reader in the first 50 pages. Therefore, even a limited “dose” of the CB bibliotherapy may be sufficient. The CB bibliotherapy was designed to provide an easy to administer and low-cost alternative to the CB program. Important directions for future studies are to enhance adherence to reading the book, and to assess the percentage of activities completed among individuals in the CB bibliotherapy group. Fourth, pretest substance use was associated with greater attrition over 2-year follow-up, though there was no evidence of differential attrition across conditions at 2-year follow-up for high substance use participants (p = .67). Fifth, we did not collect data on current parental depression, which moderated the effect of CB group in another trial (Beardslee et al., 2013; Garber et al., 2009). Sixth, though our results align with prior evidence that substance abuse might decrease participants’ motivation to actively engage in interventions and apply the skills learned (Brook et al., 2002; Gau et al., 2012; Rohde et al., 2001), there was no significant correlation at baseline between substance abuse and motivation to reduce depression in the current study. This might be due to the fact that motivation to reduce depression has different behavioral consequences than motivation to engage in a program and apply the skills taught. To disentangle the motivational context, future research is needed in which factors such as in-session engagement and effective use of the skills outside of session are investigated. Finally, the moderating effects of motivation on depressive symptoms and substance use on MDD onset are new findings and replication is necessary to increase confidence in the reliability of these effects. Nonetheless, the novel moderation effect of motivation to reduce depression is consistent with prior research on patients’ response to CB treatment (Keijsers et al., 1999) and the moderation effect of substance use on MDD onset was medium in magnitude, which increase confidence in these results. Our finding that higher baseline depressive symptoms amplify the intervention effects has previously emerged in multiple trials (e.g., Jaycox et al., 1994; Spence et al., 2003; Tandon et al., 2015), thus providing greater confidence in its reliability.
Collectively, results suggest some options for enhancing the effectiveness of CB depression prevention efforts with at-risk adolescents. We replicated what has probably been the most consistent moderator effect in depression prevention literature: program effects are stronger among those individuals with higher baseline symptoms. Thus, indicated prevention efforts, rather than selective or universal approaches, may produce the greatest depressive symptom reductions. The examination of both depressive symptom levels and MDD onset as separate outcomes illustrates that prevention programs can have both acute and long-term effects that are distinguishable. Second, the present findings suggest that requiring at least a moderate degree of motivation to reduce depression for enrollment in CB depression prevention programs or beginning a prevention program with a motivational enhancement component might amplify depressive symptom reduction effects. Last, the moderation effects for MDD onset suggest that it may be prudent to exclude youth who have current elevated levels of substance use from brief CB group depression prevention programs, as data imply that they do not benefit from such programs.
Highlights.
CB group and bibliotherapy prevention interventions reduce depressive symptoms for a range of youth
Intervention effects on depressive symptom reductions were greatest at posttest
The programs are most helpful for youth with at least moderate depressive symptoms
Youth with both depressive symptoms and substance use did not benefit from CB group
Youth with a confluence of depressive symptoms and substance use may require alternative interventions
Acknowledgments
This study was supported by National Institutes of Health Research Grants (MH67183, MH80853) and as part of the LEAD Graduate School [GSC1028], a project of the Excellence Initiative of the German federal and state governments. Sina Müller is a doctoral student of the LEAD Graduate School. Thanks go to project research assistants; the Austin Independent School District; the Bethel, 4J (Eugene), and Springfield School Districts; and the participants who made this study possible.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Sina Müller, University of Tübingen.
Paul Rohde, Oregon Research Institute.
Jeff M. Gau, Oregon Research Institute.
Eric Stice, Oregon Research Institute.
References
- Aiken LS, West SG. Multiple Regression: Testing and Interpreting Interactions. Newbury Park, CA: Sage Publications; 1991. [Google Scholar]
- Bauer DJ, Sterba SK, Hallfors DD. Evaluating group-based interventions when control participants are ungrouped. Multivariate Behavioral Research. 2008;43:210–236. doi: 10.1080/00273170802034810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beardslee WR, Brent DA, Weersing VR, Clarke GN, Porta G, Hollon SD, Garber J. Prevention of depression in at-risk adolescents: Longer-term effects. JAMA Psychiatry. 2013;70(11):1161–1170. doi: 10.1001/jamapsychiatry.2013.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brière FN, Rohde P, Shaw H, Stice E. Moderators of two indicated cognitive-behavioral depression prevention approaches for adolescents in a school-based effectiveness trial. Behaviour Research and Therapy. 2014;53:55–62. doi: 10.1016/j.brat.2013.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brook DW, Brook JS, Zhang C, Cohen P, Whiteman M. Drug use and the risk of major depressive disorder, alcohol dependence, and substance use disorders. Archives of General Psychiatry. 2002;59:1039–1044. doi: 10.1001/archpsyc.59.11.1039. [DOI] [PubMed] [Google Scholar]
- Burns DD. Feeling good: The new mood therapy. New York, NY: Morrow; 1980. [Google Scholar]
- Burton E, Stice E, Seeley JR. A prospective test of the stress-buffering model of depression in adolescent girls: No support once again. Journal of Consulting and Clinical Psychology. 2004;72:689–697. doi: 10.1037/0022-006X.72.4.689. [DOI] [PubMed] [Google Scholar]
- Castelao CF, Kröner-Herwig B. Different trajectories of depressive symptoms in children and adolescents: Predictors and differences in girls and boys. Journal of youth and adolescence. 2013;42(8):1169–1182. doi: 10.1007/s10964-012-9858-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke GN, Hawkins W, Murphy M, Sheeber L. School-based primary prevention of depressive symptomatology in adolescents: findings from two studies. Journal of Adolescent Research. 1993;8(2):183–204. [Google Scholar]
- Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry. 2003;60:837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- Curry J, Rohde P, Simons A, Silva S, Vitiello B, Kratochvil C, March J. Predictors and moderators of acute outcome in the treatment for adolescents with depression study (TADS) Journal of the American Academy of Child & Adolescent Psychiatry. 2006;45(12):1427–1439. doi: 10.1097/01.chi.0000240838.78984.e2. [DOI] [PubMed] [Google Scholar]
- Donker T, Batterham PJ, Warmerdam L, Bennett K, Bennett A, Cuijpers P, Christensen H. Predictors and moderators of response to internet-delivered Interpersonal Psychotherapy and Cognitive Behavior Therapy for depression. Journal of affective disorders. 2013;151(1):343–351. doi: 10.1016/j.jad.2013.06.020. [DOI] [PubMed] [Google Scholar]
- Feingold A. Effect sizes for growth-modeling analysis for controlled clinical trials in the same metric as for classical analysis. Psychological Methods. 2009;14(1):43–53. doi: 10.1037/a0014699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feingold A. A regression framework for effect size assessments in longitudinal modeling of group differences. Review of General Psychology. 2013;17(1):111–121. doi: 10.1037/a0030048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzmaurice GM, Laird NM, Ware JH. Applied Longitudinal Analysis. Hoboken, NJ: John Wiley & Sons, Inc; 2004. [Google Scholar]
- Furman W, Buhrmester D. Children’s perceptions of the personal relationships in their social networks. Developmental Psychology. 1985;21:1016–1024. [Google Scholar]
- Garber J, Clarke GN, Weersing VR, Beardslee WR, Brent DA, Gladstone TR, Iyengar S. Prevention of depression in at-risk adolescents: A randomized controlled trial. Journal of the American Medical Association. 2009;301(21):2215–2224. doi: 10.1001/jama.2009.788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gau JM, Stice E, Rohde P, Seeley JR. Negative life events and substance use moderate cognitive behavioral adolescent depression prevention intervention. Cognitive Behaviour Therapy. 2012;41:241–250. doi: 10.1080/16506073.2011.649781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert M, Fine S, Haley G. Factors associated with dropout from group psychotherapy with depressed adolescents. The Canadian Journal of Psychiatry/La Revue canadienne de psychiatrie. 1994;39:358–359. doi: 10.1177/070674379403900608. [DOI] [PubMed] [Google Scholar]
- Gillham JE, Hamilton J, Freres DR, Patton K, Gallop R. Preventing depression among early adolescents in the primary care setting: A randomized controlled study of the Penn Resiliency Program. Journal of Abnormal Child Psychology. 2006;34:195–211. doi: 10.1007/s10802-005-9014-7. [DOI] [PubMed] [Google Scholar]
- Gillham JE, Reivich KJ, Brunwasser SM, Freres DR, Chajon ND, Kash-MacDonald VM, et al. Evaluation of a group cognitive-behavioral depression prevention program for young adolescents: a randomized effectiveness trial. Journal of Clinical Child & Adolescent Psychology. 2012;41(5):621–639. doi: 10.1080/15374416.2012.706517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham JW. Missing data analysis: Making it work in the real world. Annual Review of Psychology. 2009;60:549–576. doi: 10.1146/annurev.psych.58.110405.085530. [DOI] [PubMed] [Google Scholar]
- Gregory RJ, Schwer Canning S, Lee TW, Wise JC. Cognitive Bibliotherapy for Depression: A Meta-Analysis. Professional Psychology: Research and Practice. 2004;35(3):275. [Google Scholar]
- Hankin BL, Abramson LY. Measuring cognitive vulnerability to depression in adolescence: Reliability, validity, and gender differences. Journal of Clinical Child and Adolescent Psychology. 2002;31:491–504. doi: 10.1207/S15374424JCCP3104_8. [DOI] [PubMed] [Google Scholar]
- Horowitz JL, Garber J. The prevention of depressive symptoms in children and adolescents: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2006;74:401–415. doi: 10.1037/0022-006X.74.3.401. [DOI] [PubMed] [Google Scholar]
- Jamison C, Scogin F. The outcome of cognitive bibliotherapy with depressed adults. Journal of consulting and clinical psychology. 1995;63(4):644. doi: 10.1037//0022-006x.63.4.644. [DOI] [PubMed] [Google Scholar]
- Jaycox LH, Reivich KJ, Gillham J, Seligman ME. Prevention of depressive symptoms in school children. Behaviour Research and Therapy. 1994;32:801–816. doi: 10.1016/0005-7967(94)90160-0. [DOI] [PubMed] [Google Scholar]
- Jayson D, Wood A, Kroll L, Fraser J, Harrington R. Which depressed patients respond to cognitive-behavioral treatment? Journal of the American Academy of Child & Adolescent Psychiatry. 1998;37:35–39. doi: 10.1097/00004583-199801000-00014. [DOI] [PubMed] [Google Scholar]
- Keijsers GP, Schaap CP, Hoogduin C, Hoogsteyns B, de Kemp E. Preliminary results of a new instrument to assess patient motivation for treatment in cognitive-behaviour therapy. Behavioural and Cognitive Psychotherapy. 1999;27:165–179. [Google Scholar]
- Kessler RC, Avenevoli S, Ries Merikangas K. Mood disorders in children and adolescents: an epidemiologic perspective. Biological psychiatry. 2001;49:1002–1014. doi: 10.1016/s0006-3223(01)01129-5. [DOI] [PubMed] [Google Scholar]
- Kindt K, Kleinjan M, Janssens JM, Scholte RH. Evaluation of a school-based depression prevention program among adolescents from low-income areas: A randomized controlled effectiveness trial. International journal of environmental research and public health. 2014;11(5):5273–5293. doi: 10.3390/ijerph110505273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein DN, Torpey DC, Bufferd SJ. Depressive disorders. In: Beauchaine TP, Hinshaw SP, editors. Child and Adolescent Psychopathology. New Jersey: John Wiley & Sons, Inc; 2008. pp. 477–510. [Google Scholar]
- Lewinsohn PM, Roberts RE, Seeley JR, Rohde P, Gotlib IH, Hops H. Adolescent psychopathology: II. Psychosocial risk factors for depression. Journal of Abnormal Psychology. 1994;103:302–315. doi: 10.1037//0021-843x.103.2.302. [DOI] [PubMed] [Google Scholar]
- Malouff JM, Rooke SE. Empirically supported self-help books. Behaviour Therapist. 2007;30(6):129. [Google Scholar]
- Monroe SM, Rohde P, Seeley JR, Lewinsohn PM. Life events and depression in adolescence: Relationship loss as a prospective risk factor for first onset of major depressive disorder. Journal of Abnormal Psychology. 1999;108:606–614. doi: 10.1037//0021-843x.108.4.606. [DOI] [PubMed] [Google Scholar]
- Moos RH. Iatrogenic effects of psychosocial interventions for substance use disorders: prevalence, predictors, prevention. Addiction. 2005;100(5):595–604. doi: 10.1111/j.1360-0443.2005.01073.x. [DOI] [PubMed] [Google Scholar]
- National Institute of Mental Health. Let’s talk about depression. Washington, DC: U.S. Government Printing Office; 2001. NIH Publication No. 01-4162. [Google Scholar]
- Nolen-Hoeksema S, Girgus JS. The emergence of gender differences in depression during adolescence. Psychological Bulletin. 1994;115:424–443. doi: 10.1037/0033-2909.115.3.424. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Stice E, Wade E, Bohon C. Reciprocal relations between rumination and bulimic, substance abuse, and depressive symptoms in female adolescents. Journal of Abnormal Psychology. 2007;116:198–207. doi: 10.1037/0021-843X.116.1.198. [DOI] [PubMed] [Google Scholar]
- O’Neil KA, Conner BT, Kendall PC. Internalizing disorders and substance use disorders in youth: Comorbidity, risk, temporal order, and implications for intervention. Clinical Psychology Review. 2011;31:104–112. doi: 10.1016/j.cpr.2010.08.002. [DOI] [PubMed] [Google Scholar]
- Puig-Antich J, Chambers WJ. Schedule for Affective Disorders and Schizophrenia for School-Age Children (6–18 years) Pittsburgh, PA: Western Psychiatric Institute; 1983. [Google Scholar]
- Radloff LS. The CES-D scale a self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Rohde P, Lewinsohn PM, Kahler CW, Seeley JR, Brown RA. Natural course of alcohol use disorders from adolescence to young adulthood. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40:83–90. doi: 10.1097/00004583-200101000-00020. [DOI] [PubMed] [Google Scholar]
- Rohde P, Stice E, Shaw H, Brière FN. Indicated cognitive behavioral group depression prevention compared to bibliotherapy and brochure control: Acute effects of an effectiveness trial with adolescents. Journal of Consulting and Clinical Psychology. 2014;82:65–74. doi: 10.1037/a0034640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohde P, Stice E, Shaw H, Gau JM. Effectiveness trial of an indicated cognitive-behavioral group adolescent depression prevention program versus bibliotherapy and brochure control at 1- and 2-year follow-up. Journal of Consulting and Clinical Psychology. doi: 10.1037/ccp0000022. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosnow RL, Rosenthal R. Assessing the effect size of outcome research. In: Nezu AM, Nezu CM, editors. Evidence-based outcome research: A practical guide to conducting randomized controlled trials for psychosocial interventions. New York, NY: Oxford University Press; 2008. pp. 379–401. [Google Scholar]
- Rubin DB. Multiple imputation for nonresponse in surveys. New York, NY: Wiley; 1987. [Google Scholar]
- Seligman ME, Schulman R, DeRubeis RJ, Hollon SD. The prevention of depression and anxiety. Prevention & Treatment. 1999;2:Article 8. [Google Scholar]
- Sheeber L, Hops H, Davis B. Family processes in adolescent depression. Clinical Child and Family Psychology Review. 2001;4:19–35. doi: 10.1023/a:1009524626436. [DOI] [PubMed] [Google Scholar]
- Spence SH, Sawyer MG, Sheffield J, Patton G, Bond L, Graetz B, Kay D. Does the absence of a supportive family environment influence the outcome of a universal intervention for the prevention of depression? International journal of environmental research and public health. 2014;11(5):5113–5132. doi: 10.3390/ijerph110505113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spence SH, Sheffield JK, Donovan CL. Preventing adolescent depression: An evaluation of the problem solving for life program. Journal of Consulting and Clinical Psychology. 2003;71:3–13. doi: 10.1037//0022-006x.71.1.3. [DOI] [PubMed] [Google Scholar]
- Stasiak K, Hatcher S, Frampton C, Merry SN. A pilot double blind randomized placebo controlled trial of a prototype computer-based cognitive behavioural therapy program for adolescents with symptoms of depression. Behavioural and cognitive psychotherapy. 2014;42(4):385–401. doi: 10.1017/S1352465812001087. [DOI] [PubMed] [Google Scholar]
- Stice E, Barrera M, Chassin L. Prospective differential prediction of adolescent alcohol use and problem use: Examining the mechanisms of effect. Journal of Abnormal Psychology. 1998;107:616–628. doi: 10.1037//0021-843x.107.4.616. [DOI] [PubMed] [Google Scholar]
- Stice E, Marti N, Shaw H, O’Neil K. General and program-specific moderators of two eating disorder prevention programs. International Journal of Eating Disorders. 2008;41(7):611–617. doi: 10.1002/eat.20524. [DOI] [PubMed] [Google Scholar]
- Stice E, Rohde P, Gau JM, Wade E. Efficacy trial of a brief cognitive–behavioral depression prevention program for high-risk adolescents: Effects at 1-and 2-year follow-up. Journal of Consulting and Clinical Psychology. 2010;78:856–867. doi: 10.1037/a0020544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Rohde P, Seeley JR, Gau JM. Brief cognitive-behavioral depression prevention program for high-risk adolescents outperforms two alternative interventions: a randomized efficacy trial. Journal of Consulting and Clinical Psychology. 2008;76:595–606. doi: 10.1037/a0012645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Rohde P, Seeley J, Gau J. Testing mediation of intervention effects in randomized trials: An evaluation of three depression prevention programs. Journal of Consulting and Clinical Psychology. 2010;78:273–280. doi: 10.1037/a0018396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Shaw H, Bohon C, Marti CN, Rohde P. A meta-analytic review of depression prevention programs for children and adolescents: factors that predict magnitude of intervention effects. Journal of Consulting and Clinical Psychology. 2009;77:486–503. doi: 10.1037/a0015168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Supplee LH, Kelly BC, MacKinnon DP, Barofsky MY. Introduction to the special issue: subgroup analysis in prevention and intervention research. Prevention Science. 2013;14:107–110. doi: 10.1007/s11121-012-0335-9. [DOI] [PubMed] [Google Scholar]
- Tandon SD, Latimore AD, Clay E, Mitchell L, Tucker M, Sonenstein FL. Depression Outcomes Associated With an Intervention Implemented in Employment Training Programs for Low-Income Adolescents and Young Adults. JAMA psychiatry. 2015;72(1):31–39. doi: 10.1001/jamapsychiatry.2014.2022. [DOI] [PubMed] [Google Scholar]
- Tram JM, Cole DA. Self-perceived competence and the relation between life events and depressive symptoms in adolescence: Mediator or moderator? Journal of Abnormal Psychology. 2000;109(4):753. doi: 10.1037//0021-843x.109.4.753. [DOI] [PubMed] [Google Scholar]
- Van Voorhees BW, Fogel J, Reinecke MA, Gladstone T, Stuart S, Gollan J, et al. Randomized clinical trial of an internet-based depression prevention program for adolescents (Project CATCH-IT) in primary care: 12-week outcomes. Journal of Developmental & Behavioral Pediatrics. 2009;30:23–27. doi: 10.1097/DBP.0b013e3181966c2a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilksch SM, Wade TD. Depression as a moderator of benefit from Media Smart: A school-based eating disorder prevention program. Behaviour research and therapy. 2014;52:64–71. doi: 10.1016/j.brat.2013.11.004. [DOI] [PubMed] [Google Scholar]