Professor Eugenio Pompeo is Associate Professor of Thoracic Surgery (research center) at the Tor Vergata University of Rome in Italy (Figure 1). He is Director of the program ‘Innovative techniques in diagnosis and surgical therapy of pulmonary emphysema’ appointed by the Fondazione Policlinico Tor Vergata. He is member of several International Scientific Societies including the European Society of Thoracic Surgeons (ESTS) and the American Association for Thoracic Surgery. He is reviewer for the main scientific journals with an interest in thoracic surgery including The Journal of Thoracic and Cardiovascular Surgery, The Annals of Thoracic Surgery, The European Journal of Cardiothoracic Surgery, Lancet Respiratory Medicine and The Journal of Thoracic Disease. He participated as an invited speaker to several international meetings and courses in Europe, Asia, the United States and South America.
Figure 1.

Professor Eugenio Pompeo (Sezione di patologia polmonare medica e chirurigca, Dipartimento di Biomedicina e Prevenzione, Università Tor Vergata, Rome, Italy).
Recently he has promoted the creation of an international working group on non-general anesthesia thoracic surgery under appointment of the ESTS. He is the Editor of the first e-monograph published worldwide on awake thoracic surgery and he is author or co-author of more than 200 scientific articles most of which are published in peer reviewed journals.
His research interests include video-assisted thoracoscopic surgery, surgical treatment of emphysema, lung cancer, myasthenia gravis and esophageal diseases. He also developed the awake thoracic surgery program at the Tor Vergata University and is currently actively dedicating to the clinical research in this field.
Professor Eugenio Pompeo has guest-edited a focused issue on “Non-Intubated Thoracic Surgery”, which is published on the journal Annals of Translational Medicine (Vol 3, No 8): http://www.atmjournal.org/issue/view/300.
In July 2015, Professor Eugenio Pompeo had his second trip to China, with the major visits to four large hospitals in Hangzhou, Shanghai, Xi’an and Guangzhou. After this fulfilled trip, we were honored to interview Professor Pompeo, who has shared his opinions on the differences of thoracic surgery departments between China and Europe, and his valuable experience and views in the minimally invasive thoracic surgery, including the non-intubated thoracic surgery (NITS), uniportal thoracic surgery and robotic thoracic surgery.
AME: What are the impressive differences between Chinese and European thoracic surgery departments after your visit to the four hospitals in China?
Prof. Pompeo: There are several important things recalled after this visit. First, I have been impressed by the excellent experience in minimally invasive thoracic surgery of thoracic surgeons in China. Most of them are not only trained with the standard three-port approach, they are also skilled with the uniportal approach, even though I can say that quite many are still somewhat reluctant to accept comprehensively the uniportal approach, because there exist still some problems to be resolved.
In contrast with thoracic surgery departments in Italy, the departments that I have visited in China are much larger on average than our own departments. Let’s say, the thoracic department in Xi’an Tangdu Hospital is a department of 393 beds (Figure 2). I am quite certain that this may be a bigger amount of beds than that we can count by summing up the beds in all the thoracic surgery departments in Rome. This is an important difference. But anyway, most of the thoracic departments we visited are over 100-bed large and very well-organized. As a result, there is a huge amount of thoracic procedures performed every day, so China has potentially a very big advantage against much of the other Institutions in most of European countries. There exists an enormous amount of data to be employed and analyzed for clinical research purposes as you already do, but this can be done even better by increasing the number of multi-institutional studies. So in my opinion, these huge amounts of data should be employed for large clinical trials, hopefully also in conjunction with Institutions from other countries including Italy of course.
Figure 2.
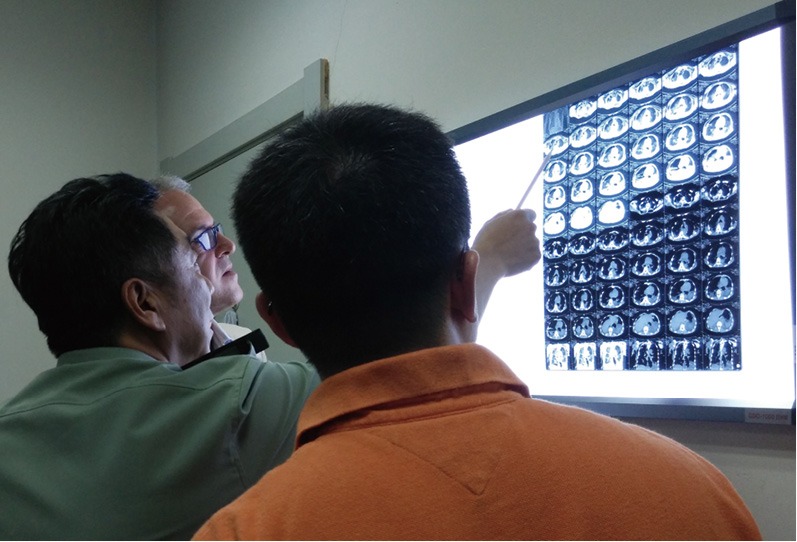
Professor Xiaofei Li (Director of Thoracic Surgery Department in Tangdu Hospital) was introducing a difficult case to Professor Pompeo.
Another difference that I have noticed between the practices in Chinese thoracic surgery departments entails health care costs. I know the patients in China need an insurance to be operated and receive healthcare even in public hospitals, but for the insurances, the length of hospitalization is less important in China than in Italy, so this entails a further difference in the timing for discharge of the operated patients. In Italy, we need to carefully consider the timing of discharge of operated patients due to the high daily cost of in-hospital beds and on average, due to the limited number of beds of most of the thoracic surgery departments. As a result in China, surgeons are not under pressure to send patients home and overall hospitalization times are somewhat longer. This is easier for the patients but it is not as good to make comparisons with experiences from Institutions in other countries.
ATM: In your career as a thoracic surgeon, what is the most impressive thing you have seen in China?
Prof. Pompeo: The most impressive thing I have seen is the great number of thoracic procedures, which can be performed in China hospitals every day. Let me say for example, for a thoracic surgeon who is interested in esophageal surgery like me, being aware of Institutions performing more than 700 or 1,000 esophagectomies each year is quite impressive. I have also liked to notice how comfortable Chinese thoracic surgeons can find performing a technically demanding procedure such as radical esophagectomies and lymphadenectomy with cervical esophagogastric anastomosis.
During my postgraduate training I had spent a highly profitable clinical fellowship in Leuven (Belgium), in the thoracic surgery department of Tony Lerut who is a recognized master of esophageal surgery, and during my career I have performed quite a meaningful number of esophagectomies for esophageal cancer. Nonetheless, I have been impressed by the minimally invasive approaches employed in China to minimize the overall invasiveness of esophageal cancer resection, particularly that entailing the combination of both thoracoscopic and laparoscopic access.
ATM: As the non-intubated thoracic surgery (NITS) is still controversial in China and other countries, what is the major impediment of its development?
Prof. Pompeo: Yes, these novel surgical strategies are still not widely accepted not only in China, but also in Italy, in other European countries as well as in USA. We have performed a survey amongst the ESTS members, which has been recently published and we have seen that several Institutions are still reluctant to adopt NITS although about 70% of responders declared to foresee an increasing adoption of NITS in the near future. I am convinced that reluctance is mainly to be attributed to the fact that many thoracic surgeons have never attempted NITS procedures or did not even see such procedures being performed by an experienced team. As a result there survive some fears of an incomplete lung collapse, coughing and excessive movement of the lung while operating with an open pneumothorax in a conscious and spontaneously ventilating subject. Instead, in most of instances during NITS, the degree of lung collapse parallels that achieved by double lumen tube intubation with single-lung ventilation and the coughing reflex is not frequently evoked and can be easily controlled by simple maneuvers including slight sedation or intra-thoracic vagal block. So I believe that every team could start taking confidence with this strategy by performing first simple procedures such as management of recurrent pleural effusion, bullectomy for spontaneous pneumothorax and simple pleural, pulmonary and mediastinal biopsies. Subsequently, the surgeon can proceed step by step with more demanding procedures including lung volume reduction surgery (LVRS), thymectomy and anatomical lung resection.
An important aspect that should be taken into account when looking to the future of NITS is the overall aging of the population. The average life expectancy of the human population is increasing worldwide. So in the near future, we will be called to operate older and older patients and we have noticed that when operating a patient, let’s say, older than 90 years old, use of NITS can undoubtedly offer several advantages if compared with intubated anesthesia. Few weeks ago, we have operated on a 91 years old patient who had been declared medically inoperable in several other Institutions. We performed a pleural-pulmonary biopsy and talcage for undetermined malignant pleural effusion by a uniportal VATS with sole local anesthesia with mild sedation and we could discharge him uneventfully 24 h after the operation. It would have been almost impossible to achieve a similar fast recovery of such a delicate patient by using general anesthesia with double-lumen tube intubation and mechanical ventilation.
ATM: As you are the very surgeon who has performed the largest number of non-intubated thoracic surgery (NITS) in Italy, how do you look at the future of non-intubated thoracic surgery (NITS)?
Prof. Pompeo: Following my second visit to the University Institution of Dr. Jianxing He, who has matured a very important experience with NITS as we have done at our own Institution, I am now even more convinced that NITS will be increasingly employed in the near future (Figure 3). There survive some reluctance in accepting NITS but according to our own experience, for selected cohorts, the advantages of NITS strategies can be very important. In my opinion, one of the major indications is poor pulmonary function as it can be found in subjects with severe emphysema. We have a very good experience with an original awake LVRS method that we have developed and which we call non-resectional LVRS. We routinely perform it in fully awake patients although I have experienced in Guangzhou that it can be safely performed also by target control sedation with the advantage of having the patient unconscious while keeping the important advantages related to the avoidance of intubation, mechanical ventilation and diaphragm paralysis.
Figure 3.
Professor Jianxing He (President of the First Affiliated Hospital of Guangzhou Medical University, Director of Thoracic Surgery Department) was introducing the Thoracic Surgery Department to Professor Pompeo on the ward round.
In fact, as an interesting novel perspective I can mention that during my stay in Guangzhou I have had the opportunity to operate on by NITS a patient with giant bullous emphysema and an obliterated pleural cavity due to post-tuberculosis fibrous pleural adhesions. In that case it has been offered me the possibility to employ an innovative glasses-less 3D technology that is being developed at the First Affiliated Medical University of Guangzhou by Dr. He and his team. This technology improves meaningfully both ergonomics and precision of surgical maneuvering during demanding VATS procedures offering the advantage of a 3D vision without the difficulties and adverse affects related to the need of 3D-lenses.
In Guangzhou at the Dr. He’s Institution, I have also admired technically demanding procedures such as sleeve lobectomy and tracheal resection carried out by NITS. Worthy of note tracheal resection and reconstruction was completely performed by VATS under non-intubated anesthesia. The operation was completed smoothly and it was impressive how the patient oxygenation could be kept at satisfactory levels throughout the procedure. In fact, almost every delicate surgical maneuver can be done very safely with this kind of approach if the surgical and anaesthetic teams are well trained.
We still need some basic research to show more objectively the advantages in terms of pre- to postoperative changes in physiologic and immunologic outcomes data by comparing thoracic surgery procedures performed by intubated vs. non-intubated aesthesia, but I am quite certain that NITS might become the favorite strategy for a number of surgical procedures in the near future.
ATM: Compared with the non-intubated thoracic surgery (NITS), how do you look at the future of other minimally invasive surgery, such as the uniportal thoracic surgery and robotic thoracic surgery?
Prof. Pompeo: The uniportal approach is an important one, because it has been developed in the same direction of NITS that means to minimize the overall invasiveness of surgery. So the attempt to reduce the patients’ discomfort and improve the cosmetic outcome by this type of approach is an important aspect to be taken into account particularly from the patient’s perspective and goes in the same direction. Undoubtedly, as it happens for NITS, uniportal VATS still poses some problems awaiting a solution. One relates to multiple instruments passed through a single incision making surgical maneuvers more demanding for the surgeon. So even though uniportal VATS is better for the patients, so far it is not as comfortable for the surgeon as the two or three-portal approach. The surgeon has to be very well trained with this approach since hand movements are not so natural when dealing with uniportal procedures. Moreover, the surgeon accomplishes by one hand the role of the assistant that is grasping and aspirating blood whereas uses one hand only for surgical dissection. This is ergonomically unfavorable and if I can make a joking parallel with the Chinese way of eating, a surgeon operating through a uniportal approach is like if he or she was eating using one chopstick instead than two. But I believe this is not an unsolvable problem. New instrumentation can be developed to improve the ergonomics of the uniportal approach and in my mind this will be possible in the near future because so far the surgeons have to be very skilled through a uniportal approach and they are obliged to carry also some excessive risks, particularly when dealing with major surgical procedures. Even though I have seen many well-trained thoracic surgeons operating through a uniportal approach in a quite comfortable way, still this is not yet the optimal way for doing that in my opinion.
ATM: What about the robotic surgery?
Prof. Pompeo: Robotic surgery is the natural or maybe unnatural evolution of thoracic surgery for the future, because we are progressively increasing the use of robots, not only in the operating room, but in everyone’s daily life. So robots are coming to substitute humans for many simple jobs within the next few years. I know about the existence of projections calculating that within 20 years about 50% of human jobs will be done by robots although the most complicated ones will still be dealt by humans. So it is likely that in robotic thoracic surgery as well in which the job is done by humans under assistance of robotized arms and hands, this technology will be increasingly employed. Obviously the robots must evolve. Now there are four arms passing through different incisions. I believe that in the next future, the robots’ arms maybe will pass through one or two incisions, as it happens with standard surgery. I think the robots will evolve in the near future to be ergonomically more suitable to perform surgical procedures with not so many incisions, not so many arms, and reduced encumbrance of the entire apparatus.
Another important problem with the robots is the cost. There is only one manufactory which is now producing operative robots, so there is no competition, and the cost may prove high. I don’t know which will be the future, but anyway with an increasing use of robots, the cost will decrease as well. For the future generation of thoracic surgeons, robotic thoracic surgery will be increasingly important to be learned (Figure 4).
Figure 4.
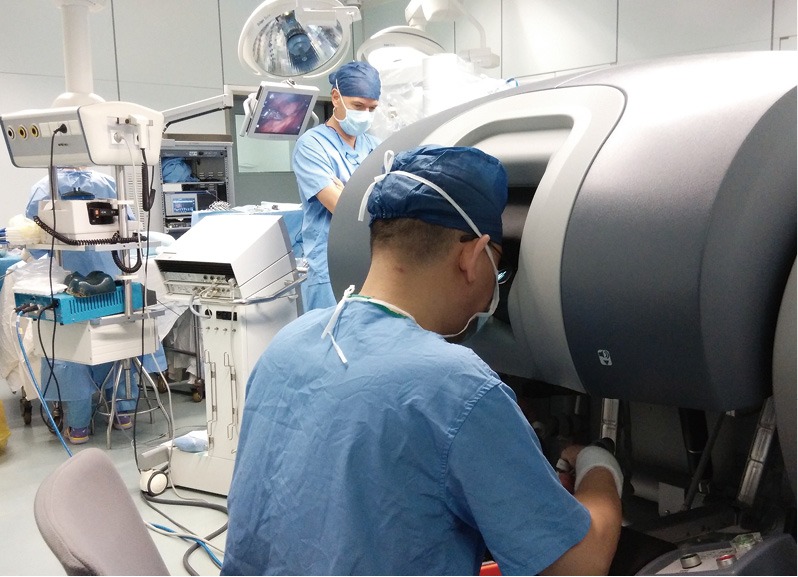
Professor Pompeo was watching a robotic thoracic procedure conducted by Professor Qingquan Luo in Shanghai Chest Hospital.
ATM: Can the non-intubated thoracic surgery (NITS) and the uniportal or robotic surgery be combined and work more efficiently?
Prof. Pompeo: I am sure the future will offer the opportunity to combine these approaches, because they all move toward a globally minimally invasive thoracic surgery management. Maybe the robots will be included in combined approaches a little bit later, but something that we can start now is to combine uniportal VATS and NITS to achieve a faster and smoother recovery associated with an optimal cosmesis. But combining all the three aspects, robotics, uniportal and NITS might potentially offer the least invasive thoracic surgery management in the future.
ATM: As you are good at the awake non-resectional lung volume reduction surgery (LVRS), do you have some experience to share with the non-experienced young surgeons?
Prof. Pompeo: I can say that currently LVRS is largely underused despite its recognized effectiveness. We all know, looking at the available data that LVRS can offer very reproducible results in improving pulmonary function and quality of life of many patients with severe emphysema. Nonetheless, the major problem of this procedure is prolonged air-leaks, a minor complication that is not dangerous but can constrain the patients to long hospitalization times and elevated costs.
Recently, several new techniques including some endoscopic LVRS methods have been proposed in an attempt to overcome this problem. Unfortunately, so far no endoscopic method has demonstrated to be as effective as surgical LVRS in improving both pulmonary function and quality of life of patients with severe emphysema due to several technical and physiologic problems. This is the reason that has led us to develop an original non-resectional LVRS method, which does not require any resection of lung tissue, can be safely performed in awake conditions by regional anesthesia, and has shown to reduce in a significative manner the incidence of prolonged air leaks. I am quite certain that in the near future this procedure will be used also in other Institutions within well constructed clinical trials to confirm the efficacy of this very simple and as yet effective procedure.
ATM: What are the indications for awake non-resectional lung volume reduction surgery (LVRS)?
Prof. Pompeo: The proper indications for the awake non-resectional LVRS are the same pointed out for the standard resectional technique. The most important aspect is looking at an emphysema patient with poor pulmonary function and with an impaired quality of life despite maximized medical therapy because we know that therapy of chronic obstructive pulmonary disease (COPD) patients is centered on pharmacological therapy and rehabilitation. Unfortunately in patients with emphysema, pharmacological therapy is ineffective when the disease has progressed leading to an unsolvable worsening of quality of life. At this advanced stage LVRS and lung transplantation remain the only salvage options but for many patients LVRS can represent the only chance due to the greater invasiveness of transplantation and the strict age limit for eligibility in lung transplantation lists. In addition, there exist today some strategies, which can help to achieve a very long and relatively stable improvement in quality of life, let’s say, for 7–12 years, by performing, for example, a staged bilateral procedure. This means that a first LVRS is performed in the most damaged lung whereas the contralateral LVRS is postponed until when the benefit achieved after the first procedure is lost.
As a result, in patients with severe emphysema associated to an impaired pulmonary function which is not controlled by pharmacological therapy, the most important criterion is based on radiologic morphology of emphysema. The ideal candidates are those with heterogenous emphysema, that means having evidence at high resolution computed tomography, of highly destroyed upper lobes and better preserved middle/lower lobes. These are the best criteria predicting maximized benefit following LVRS independent by the type of anesthesia.
ATM: As you mentioned the Chinese young surgeons are well trained in China, would you mind introducing how are the young thoracic surgeons trained in Italy?
Prof. Pompeo: The training of thoracic surgeons in Italy is being progressively uniformed to the programs in other European countries. Obviously there exist some differences between each country in Europe so far. The residency program in thoracic surgery in Italy is 5 years long, coming after a 6-year medical degree studies. To be accepted in a postgraduate school of thoracic surgery, there are competitive examinations and the positions available per each school are published yearly on a nationwide basis.
In Italy, the training is improving in my opinion, because now clinical practice, surgical training at the table and education to clinical research are integral components of the training programs and are becoming better and better. This is actually the same feeling that I have had in China, because in your country also I have had the opportunity to interact with young thoracic surgeons during their residency program. They also are trained not only theoretically and in the operating room, but in performing research as well. This is very important, because they start learning how to design and conduct a scientific research and how to write a scientific paper. I am very satisfied of this aspect and I congratulate the Chinese Professors that I met in China for the local residency programs, which are modern, effective and competitive in my opinion.
ATM: How do you define fast-track recovery and how do you look at the non-intubated thoracic surgery (NITS) is related to the fast-track recovery?
Prof. Pompeo: I believe the fast-track recovery is a real need and will be the future for many surgical procedures. Maybe in Italy the pressure for this is even stronger than in China, because of the problem we were talking about before, the need to accelerate the patient’s turnover to offer adequate health care to everyone who need it. Within such a scenario combining NITS with fast-track recovery seems a natural evolution of thoracic surgery for the next future.
I believe, for example that, most of the simple procedures such as management of pleural effusion and management of pneumothorax can be performed through non-intubated anesthesia approaches with fast-track recovery and even within 1-day surgery programs. These strategies will be increasingly adopted in many Institutions in the future in my opinion.
ATM: Is there any training program for non-intubated thoracic surgery (NITS) in your department or Italy?
Prof Pompeo: In Italy, maybe the main experience on NITS is the one we have matured at our own Institution. We have included NITS in the training program at our department. I don’t know if there are other training programs including NITS in Italy but I believe that one further key to increase the reliability of NITS will be to create multidisciplinary teams. NITS is something that is not only for thoracic surgeons, there should be a well-trained and cooperative team including thoracic surgeons, anesthesiologists, and also other specialists such as pulmonologists, radiologists and pathologists as we have done at our Institution. In this regard one further crucial issue will be to promote joint multidisciplinary international meetings. Recently we have had a stimulating occasion at the last ESTS meeting in Lisbon. The meeting program included one joint session between thoracic surgeons of the ESTS and A in anesthesiologists of the European Association of Cardiothoracic Anesthesia (EACTA), which was entirely devoted to NITS. I believe this was probably one of the very first occasions during which anesthesiologists and thoracic surgeons met each other to discuss extensively about this topic. In the future, we should implement this kind of meetings in order to collect experiences and results, and discuss together the various unresolved issues. I am confident that one of the next joint international meetings on NITS will be held in Rome in the near future.
ATM: Thank you very much for your precious time for the interview!
Acknowledgements
None.
Footnotes
Conflicts of Interest: The author has no conflicts of interest to declare.



