Abstract
Chronic hepatitis B virus (HBV) infection is a major global health problem with an estimated 400 million HBV carriers worldwide. In the natural history of chronic hepatitis B (CHB), spontaneous acute exacerbation (AE) is not uncommon, with a cumulative incidence of 10%–30% every year. While exacerbations can be mild, some patients may develop hepatic decompensation and even die. The underlying pathogenesis is possibly related to the activation of cytotoxic T lymphocyte-mediated immune response against HBV. An upsurge of serum HBV DNA usually precedes the rise of alanine aminotransferase (ALT) and bilirubin. Whether antiviral treatment can benefit CHB with severe AE remains controversial, but early nucleos(t)ide analogues treatment seemed to be associated with an improved outcome. There has been no randomized study that compared the effects of different nucleos(t)ide analogues (NA) in the setting of CHB with severe AE. However, potent NAs with good resistance profiles are recommended. In this review, we summarized current knowledge regarding the natural history, pathogenetic mechanisms, and therapeutic options of CHB with severe AE.
Keywords: hepatitis B, acute exacerbation, antiviral treatment
1. Introduction
Chronic hepatitis B virus (HBV) infection is a major global health problem with an estimate of 400 million HBV carriers worldwide [1]. In the natural history of chronic hepatitis B (CHB), spontaneous acute exacerbation (AE) is not uncommon, with a cumulative incidence of 10%–30% every year [2,3,4]. While exacerbations can be mild, some patients may develop hepatic decompensation and even die [5,6]. The Asian Pacific Association for the Study of the Liver (APASL) had a consensus recommendation on acute-on-chronic liver failure (ACLF), defined as an acute hepatic insult manifesting as jaundice and coagulopathy (international normalized ratio [INR] >1.5), complicated within four weeks by ascites and/or encephalopathy in a patient with previously diagnosed or undiagnosed chronic liver disease [7]. AE of chronic hepatitis B (CHB) represents a distinct disease characterized by the abrupt rise of HBV DNA followed by impairment of liver function. AE of CHB was defined as “an abrupt elevation of serum alanine aminotransferase (ALT) to >5 × ULN or a greater than 3-fold increase in ALT, whichever was higher” [2,8]. Initiating events for the AE in CHB may not be readily identifiable, and these flares are considered to be spontaneous in nature. However, in many instances, precipitating factors for reactivated hepatitis B can be readily identified and are not considered as spontaneous in nature. The precipitating factors include immunosuppressive/cytotoxic medications, anti-viral therapy (interferon, nucleos(t)ide analogues), HBV genotypic variations (precore, core promoter or polymerase mutants), superimposed with other hepatotropic viruses (hepatitis A virus, hepatitis C virus or hepatitis D virus), and interaction with HIV (reactivated hepatitis, effect of immune reconstitution therapy) [9,10,11].
CHB with spontaneous AE is a dynamic process of immune response between HBV, hepatocytes and immune cells of the host [8,10,12,13]. Persistent necroinflammatory changes in liver tissue during CHB with AE are caused by an inadequate immune response to HBV antigens that are expressed on the surface of hepatocytes where they can activate cell-mediated immune responses [14,15]. When the immunologic response to viral antigens are more robust, the likelihood of inflammatory changes, damage to hepatocytes, and progressive fibrosis are greater [5]. The role of antiviral agents in the treatment of CHB with severe AE is unclear. Early lamivudine treatment before the bilirubin level rose above 20 mg/dL seemed to be associated with an improved outcome [16]. Another recent study also found that lamivudine treatment can improve the outcome for patients with a model for end stage liver disease (MELD) score below 30 [17]. However, the choice of different antiviral agents remains controversial. In this review, we summarized the natural history, pathogenetic mechanism of CHB with spontaneous severe AE, and compared the effects of different antiviral agents.
2. Natural History
Typical chronic HBV infection acquired perinatally involves three phases: immune tolerant, immune clearance, and inactive residual [18,19]. Severe exacerbation of CHB usually occurs in the immune clearance phase but can also happen in some patients in the inactive phase, inducing immune-mediated liver injury that resembles the events in the immune clearance phase [19]. A prospective study from Taiwan found that during an average follow-up of 23.5 months, AE occurred in 197 HBeAg-positive patients and 56 anti-HBe-positive patients, with a calculated annual incidence of 28.6% and 10.3%, respectively [20]. Another prospective study from Hong Kong reported that the cumulative probabilities of developing exacerbations at the end of one and four years were 6.3% and 15%, respectively in patients with serum alanine aminotransferase (ALT) levels below 200 IU/L, 24% and 47%, respectively in patients with ALT levels above 200 IU/L, and up to 8% of patients may develop hepatic decompensation [21]. The clinical presentation of CHB with spontaneous AE varies from either asymptomatic or symptomatic to a feature similar to overt acute hepatitis. It may also complicate with hepatic decompensation and even lead to death [19,20,21]. CHB with AE may also occur in cirrhotic patients and is associated with a higher rate of hepatic decompensation and mortality compared with CHB patients without cirrhosis [22]. Predisposing factors of spontaneous severe AE include elevated ALT levels at presentation, male sex, and the presence of HBeAg [3]. Yuen et al. [23] suggested that the prognostic factors in CHB with spontaneous severe AE not receiving antiviral treatment included pre-existing cirrhosis, high Child-Pugh score, low albumin level, high bilirubin level, prolonged prothrombin time (PT), and low platelet count, while prognostic factors for subsequent monitoring were high peak bilirubin level, long peak PT, duration to reach peak PT, development of encephalopathy, and presence of ascites. The prognostic factors reported by Tsai et al. [24] included high AST level, low albumin level, high bilirubin level, prolonged PT, and low platelet count.
3. HBV Genotypes and Variants in Acute Exacerbation
HBV genotypes (Table 1) and mutations in the precore and core promoter region of the HBV genome (Table 2) have been suggested to be associated with AE of CHB. In two studies from Hong Kong, genotype B HBV was found to be the predominant HBV strain among patients with severe AE [25,26]. Imamura et al. [27] also reported that HBV genotype B occurred more frequently in patients with acute forms of liver disease than in patients with chronic liver disease, and more frequently in patients with fulminant hepatitis than in those with acute self-limited hepatitis. Ren et al. [28] found that patients with CHB infected with genotype B were more likely to develop HB-ACLF than those with genotype C. However, Tsai et al. [24] found no significant association of genotype B HBV in CHB with severe AE. Liu et al. [29] in a case control study found that the distribution of HBV genotypes in HBV carriers with fulminant and subfulminant hepatitis was similar to control patients. Yuen et al. [30] in a recent study also found that there were no differences in the cumulative risk and severity of acute exacerbation between patients with genotypes B and C. Omata et al. [31] reported that a point mutation at the A1896 was associated with the development of fulminant hepatitis. However, further clinical studies on precore and core promoter mutations did not have consistent results. While Yuen et al. [26] found no association between precore mutation of HBV and severe AE of HBV, Tsai et al. [24] reported that precore mutation of HBV had a protective effect on the occurrence of hepatic decompensation in CHB with AE. On the other hand, Yuen et al. [26] found that core promoter mutation of HBV is associated with severe AE of HBV, Yuan et al. [32] also found that core promoter mutations were independently associated with the occurrence of acute exacerbation after HBeAg seroclearance. Ren et al. [28] found that single mutations including T1753V (C/A/G), A1762T, G1764A, G1896A and G1899A were more frequently detected in patients with HB-ACLF than in patients with CHB and patients with precore mutation had increased risk of a fatal outcome. Kusumoto et al. [33] found that Mutations in the core promoter (A1762T/G1764A) and precore region (G1896A) were more frequent in patients with acute exacerbation of chronic hepatitis than acute hepatitis. But Tsai et al. [24] reported no significant association between core promoter mutation of HBV and severe AE of HBV, and Liu et al. [29] in a case control study also found that the distribution of precore and core promoter mutations in HBV carriers with fulminant and subfulminant hepatitis were similar to control patients. Ehata et al. [34] found that clustering changes in a segment of 16 amino acids (codon 84–99 from the start of the core gene) were present in all seven fulminant and severe exacerbation patients infected with adr subtype HBV and a different segment with clustering substitutions (codon 48–60) was also found in seven of eight fulminant and severe exacerbation patients infected with adw subtype HBV. Mutations in the core region may play an important role in the pathogenesis of HBV, and such mutations are related to severity of liver damage. Liu et al. [35] discovered that after exacerbation of CHB, about half of the patients were repopulated by a different viral variant and mean nucleotide change per genome was 0.2 at virologic peak but increased to 4.4 and 8.1 at and after biochemical peak respectively, which was likely an effect of immune selection. Liu et al. [36] also found that HBV viral strain in the serum reflects the intrahepatic strain of the AE and random reactivation of the original HBV pool, rather than a sequential evolution of one strain, causes the onset of repeated AE.
Table 1.
Hepatitis B virus genotypes in acute exacerbation, NA: not analyzed.
| Authors | Disease | Patient No. | Genotype (%) | p-Value |
|---|---|---|---|---|
| Chan et al.[25] | Severe icteric flare up | 21 | B (91%) | <0.001 |
| Asymptomatic carrier | 31 | B (39%) | ||
| Early cirrhosis | 49 | B (20%) | ||
| Decompensated cirrhosis | 31 | B (32%) | ||
| Yuen et al. [26] | Hepatic decompneation | 28 | B (71%) | 0.0001 |
| No hepatic decompensation | 39 | B (28%) | ||
| Imamura et al. [27] | Acute hepatitis | 45 | B (31%) | <0.001 |
| Fulminent hepatitis | 16 | B (63%) | ||
| Chronic liver disease | 531 | B (12%) | ||
| Ren et al. [28] | Acute on chronic live failure | 75 | B (31%) | 0.009 |
| Chronic hepatitis B | 328 | B (17%) | ||
| Tsai et al. [24] | Hepatic decompensation | 20 | B (70%) | 0.346 |
| No hepatic decompensation | 31 | B (80%) | ||
| Liu et al. [29] | Fulminent/subfulminent hepatitis B | 18 | B (78%) | |
| Hepatitis B carrier | 18 | B (67%) | >0.05 | |
| Yuen et al. [30] | Acute exacerbation | NA | B (NA) | 0.95 |
| No acute exacerbation | NA | B (NA) | ||
| Severe exacerbation | NA | B (NA) | 0.12 | |
| Mild exacerbation | NA | B (NA) |
Table 2.
Hepatitis B virus variants in acute exacerbation.
| Authors | Disease (Patient No.) | Variants (%) | p-Value |
|---|---|---|---|
| Ren et al. [28] | Acute on chronic live failure (75) | G1896A (45%) | 0.038 |
| G1899A (16%) | |||
| A1762T (77%) | 0.013 | ||
| G1764A (83%) | |||
| T1753V (28%) | <0.001 | ||
| Chronic hepatitis B (328) | G1896A (32%) | ||
| G1899A (6%) | <0.001 | ||
| A1762T (52%) | |||
| G1764A (54%) | 0.012 | ||
| T1753V (16%) | |||
| Tsai et al. [24] | Hepatic decompneation (20) | Precore mutant (60%) | 0.046 |
| Core promoter mutant (55%) | |||
| No hepatic decompensation (31) | Precore mutant (65%) | 0.747 | |
| Core promoter mutant (42%) | |||
| Omata et al. [31] | Fatal hepatitis B (9) | G1896A (100%) | <0.05 |
| Acute self-limited hepatitis B (10) | G1896A (0%) | ||
| Yuen et al. [26] | Severe exacerbation (24) | Precore mutant (17%) | NS |
| Core promoter mutant (25%) | |||
| Mild exacerbation (96) | Precore mutant (18%) | ||
| Core promoter mutant (60%) | 0.004 | ||
| No exacerbation (96) | Precore mutant (14%) | ||
| Core promoter mutant (46%) | |||
| Kusumoto et al. [33] | Acute exacerbation (36) | Precore mutant (58%) | <0.001 |
| Core promoter mutant (81%) | |||
| Acute hepatitis (36) | Precore mutant (6%) | <0.001 | |
| Core promoter mutant (19%) | |||
| Yuan et al. [32] | Acute exacerbation (56) | Precore mutant (38%) | 0.12 |
| Core promoter mutant (86%) | |||
| Without acute exacerbation (145) | Precore mutant (51%) | 0.003 | |
| Core promoter mutant (64%) | |||
| Liu et al. [29] | Fulminent/subfulminent hepatitis B (18) | Precore mutant (67%) | >0.05 |
| Core promoter mutant (17%) | |||
| Hepatitis B carrier (18) | Precore mutant (50%) | NS | |
| Core promoter mutant (17%) |
NS: non-significant.
4. Pathogenesis
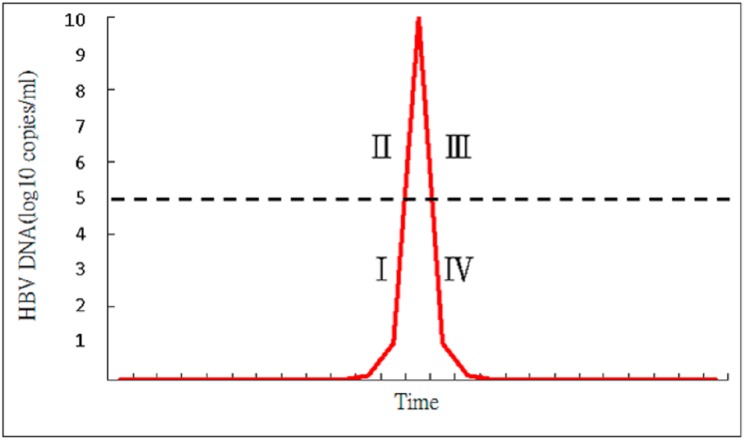
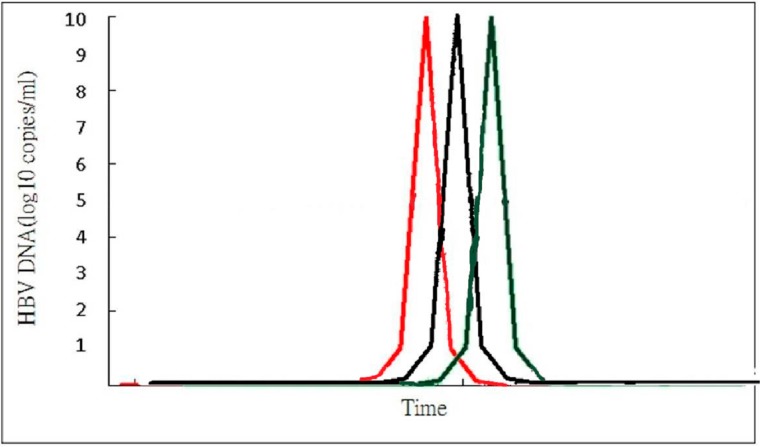
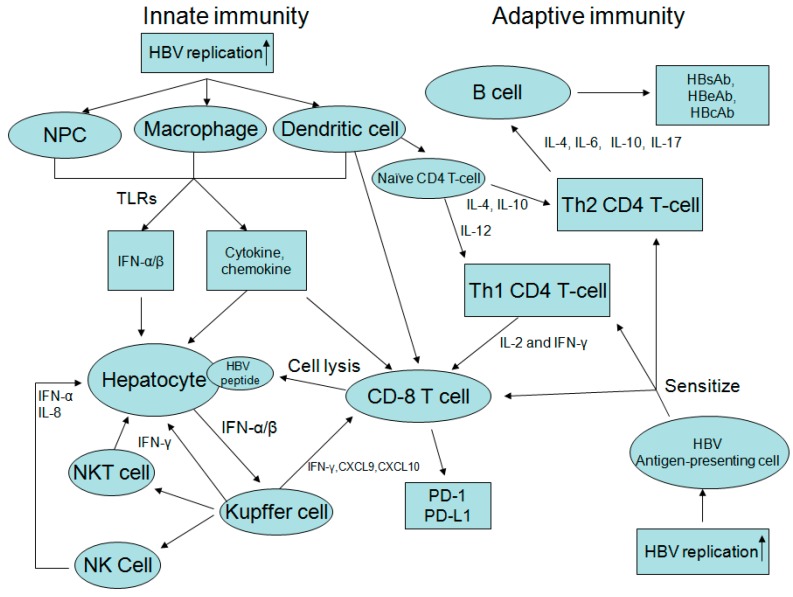
Acute exacerbation of CHB is the result of dynamic changes of both innate and adaptive immune responses with human leukocyte antigen class I (HLA-I)-restricted, cytotoxic T lymphocyte (CTL)-mediated immune cytolysis of HBV antigen(s) expressing hepatocytes [8,10,37,38]. Spontaneous AE of CHB is usually precipitated by reactivated infection, and there is usually an upsurge of serum HBV DNA prior to the abrupt elevation of alanine aminotransferase (ALT) or bilirubin level [39,40] (Figure 1). The clinical course of CHB with AE can be divided into four stages according to the changes in HBV DNA level (Figure 2). In the ascending limb, HBV DNA <105 copies/mL denotes Stage I while HBV DNA ≥105 copies/mL represents Stage II. In the descending limb, HBV DNA ≥105 copies/mL denotes Stage III while HBV DNA <105 copies/mL represents Stage IV. Patients in Stage I are usually asymptomatic and will seldom seek medical help. Therefore, in clinical practice, patients who visit the hospital due to CHB with spontaneous AE are usually in Stage II, III or IV. If patients visited the doctor at Stage IV, the immune storm due to flare-up of HBV has already been initiated and got exacerbated, which induces the rapid decline of HBV DNA, so the success of antiviral treatment is not anticipated. Moreover, patients in Stage IV have a low HBV DNA level which is also decreasing rapidly, so the benefits of antiviral treatment are expected to be insignificant. Liver injury during these spontaneous AE appears to be mediated by expanded numbers of T cells that are reactive to hepatitis B e antigen (HBeAg) and c antigen (HBcAg) [12,41]. Immunopathologic studies during AE of CHB have shown that the cellular infiltrates at the site of necroinflammatory reaction are mainly CD8 + CTL, which are generally considered to be directed to HBcAg peptides on the surface of hepatocytes [42,43]. Immunologic studies showed a significant elevation of HBcAg/HBeAg-specific precursor T cell, an increase in HBcAg/HBeAg-specific T cell proliferation, a decrease in HBcAg-specific regulatory T cell (Treg) frequencies associated with an increase in HBcAg-specific cytotoxic T lymphocyte (CTL) frequencies. Non-parenchymal cell, dendritic cells and macrophages can also produce interferon α/β, cytokine and chemokine after recognition of HBV. Increased production of Th1 cytokines (interleukin (IL)-2 and IFN-γ), Th2 cytokines (IL-4, IL-6, and IL-10), an increase in IL-17-producing CD4+ T cells, natural killer (NK) cell-mediated pathways (IFN-α and IL-8), high serum levels of IFN-γ inducible chemokines Chemokine (C-X-C motif) ligand 9 (CXCL)-9 and CXCL-10, programmed cell death protein 1 (PD-1) and its ligand PD-L1 during AE of CHB [44,45,46,47,48,49,50]. Cytokine production is associated with activation of toll-like receptors (TLR) and increased expression of TLR-2, TLR-4, TLR-3, TLR-5,TLR-7, TLR-9, TLR-10 are also observed in CHB with AE (Figure 3) (Table 3) [51,52]. However, the event that triggers spontaneous AE of CHB in immune clearance or inactive phase remains unclear.
Figure 1.
The clinical course of chronic hepatitis B (CHB) with acute exacerbation (AE) can be divided into four stages according to HBV DNA level. In the ascending limb, HBV DNA level <105 copies/mL denotes Stage I while HBV DNA level ≥105 copies/mL represents Stage II. In the descending limb, HBV DNA level ≥105 copies/mL denotes Stage III while HBV DNA level <105 copies/mL represents Stage IV.
Figure 2.
Spontaneous AE of CHB is usually precipitated by reactivated infection, and there is usually an upsurge of serum HBV DNA prior to the abrupt elevation of ALT or bilirubin level. Red line: HBV DNA; Black line: Alanine Aminotransferase (ALT); Green line: Bilirubin.
Figure 3.
Acute exacerbation of CHB is the result of dynamic changes of both innate and adaptive immune responses. Spontaneous AE of CHB is usually precipitated by reactivated infection, and there is usually an upsurge of serum HBV DNA prior to the abrupt elevation of alanine aminotransferase (ALT) or bilirubin level. Liver injury during these spontaneous AE appears to be mediated by T cells sensitized by HBV antigen presenting cells. Virus-specific CD8+ cytotoxic T cells (with help from CD4+ T cells) can recognize viral antigens presented on infected hepatocytes and lead to direct lysis of the infected hepatocyte. Non-parenchymal cells (NPC), dendritic cells, and macrophages can also produce interferon (IFN) α/β, cytokine and chemokine after recognition of HBV. Increased production of Th1 cytokines, Th2 cytokines, natural killer (NK) cell-mediated pathways, high serum levels of IFN-γ inducible chemokines Chemokine (C-X-C motif) ligand 9 (CXCL)-9 and CXCL-10, programmed cell death protein 1 (PD-1), and its ligand PD-L1, and activation of toll-like receptors (TLR) during AE of CHB are also observed in CHB with AE. IL: interleukin; NKT cell: natural killer T cell; Th1 cell: type I helper T cell; Th2 cell: type II helper T cell.
Table 3.
Immune profile during spontaneous acute exacerbation of chronic hepatitis B virus (HBV).
| Immune Profile | Activity |
|---|---|
| HBV-specific T cell response | |
| HBV-specific regulatory T | Decrease |
| HBV-specific cytotoxic T cell | Increase |
| NK cell pathway | |
| IFN-α | Increase |
| IL-8 | Increase |
| Th1 cytokines | |
| IL-2 | Increase |
| IFN-γ | Increase |
| Th2 cytokines | |
| IL-4 | Increase |
| IL-6 | Increase |
| IL-10 | Increase |
| Chemokines | |
| CXCL-9 | Increase |
| CXCL-10 | Increase |
| PD-1 | Increase |
| PD-L1 | Increase |
| Toll-like receptors | |
| TLR-2 | Increase |
| TLR-3 | Increase |
| TLR-4 | Increase |
| TLR-5 | Increase |
| TLR-7 | Increase |
| TLR-9 | Increase |
| TLR-10 | Increase |
IFN: interferon; IL: interleukin; PD-1: programmed cell death protein 1; PD-L1: programmed death-ligand 1; Tc: cytotoxic T cell; Treg: regulatory T cell; TLR: toll like receptor; CXCL: Chemokine (C-X-C motif) ligand.
5. Treatment
Aggressive supportive treatments applied for acute-on-chronic liver failure (ACLF) due to CHB with severe AE include close monitoring of vital signs, fluid status, nutritional status, electrolytes, liver function, antibiotics use for infection, treatment for hepatic encephalopathy, and terlipressin and albumin for hepatorenal syndrome. Extracorporeal liver support systems that replace the detoxification, synthetic, and regulatory functions of the native liver represent a potential solution, but all the devices currently available are still far from ideal [53]. In general, artificial (cell-free) and bioartificial liver support devices have shown their ability to decrease some circulating toxins and to ameliorate hepatic encephalopathy and other intermediate variables. Although they are relatively safe, their effects on the survival of patients with ACLF have not been confirmed [53,54,55]. Recent randomized controlled studies in ACLF patients failed to identify any survival benefit of extracorporeal liver support systems, such as fractionated plasma separation and adsorption (FPSA) and molecular adsorbent recirculating system (MARS) [56,57].
5.1. Antiviral Treatment
Interferon therapy is contraindicated in CHB with severe AE as it will cause liver function impairment and exacerbate hepatic decompensation. Nucleos(t)ide analogues (NA) have the profound effect of viral suppression and show good safety profiles in patients with hepatic decompensation, so NA are the drug of choice in CHB with severe AE.
5.2. Lamivudine
There has been no randomized study that compared the efficacy of lamivudine vs. symptomatic treatment in CHB with severe AE (Table 4). Chan et al. [58] in a retrospective study that compared the treatment effect of lamivudine in 28 CHB patients with severe AE vs. 18 controls found that six (21.4%) lamivudine-treated patients vs. five (27.8%) controls died or received a liver transplant (p = 0.62). Multivariate analysis found that platelet ≤1.43 × 1011/L and bilirubin >172 micromol/L, but not lamivudine treatment, were independent predictors of liver-related mortality. Similarly, Tsubota et al. [59] compared retrospectively the treatment effect of lamivudine in 25 CHB patients with severe AE vs. 25 controls. They found hepatic failure developed in six lamivudine-treated patients (24%) and seven controls (28%); and in patients with hepatic failure, three lamivudine-treated patients (12%) and two controls (16%) survived (p > 0.15). Lamivudine monotherapy did not prevent progression to hepatic failure or mortality. Multivariate analysis discovered baseline serum bilirubin ≥6 mg/dL, pre-existing cirrhosis, and baseline prothrombin time <40% as independent determinants of rapid progression to hepatic failure. In another retrospective study, Chien et al. [16] compared the treatment effect of lamivudine in 60 CHB patients with severe AE vs. 31 controls and found that 38% of treated patients and 29% of the controls died (p = 0.166). Stepwise logistic regression analysis revealed that both prolonged PT and baseline Child-Pugh scores were significant predictors of mortality, but treatment with lamivudine is not an independent predictor of survival. However, the present study found that of the patients with serum bilirubin <20 mg/dL, all 25 lamivudine-treated patients survived, but five (25%) of 20 untreated patients died (p = 0.013). On the contrary, in patients with serum bilirubin level ≥20 mg/dL, the mortality between lamivudine-treated and untreated patients were similar. These results suggest that lamivudine may prevent fatality in CHB patients with hepatic decompensation if therapy starts early enough or before serum bilirubin level rises above 20 mg/dL, which is usually in Stage II or III during CHB with severe AE (Figure 2), but lamivudine helps little if serum levels already exceed 20 mg/dL, which is usually in Stage IV (Figure 2). Sun et al. [17] in a matched retrospective cohort study that compared the treatment effect of lamivudine in 130 CHB patients with severe AE vs. 130 controls found that the mortality (50.7%, 38/75) of lamivudine-treated patients with MELD scores of 20–30 was lower than that (75.7%, 56/74) of the control group (p = 0.002). Moreover, the mortality of lamivudine-treated patients with MELD scores above 30 was 98.0% (48/49) and 100.0% (53/53) in the control group, showing no significant difference between the two groups (p = 0.296). A recent meta-analysis showed no benefit of lamivudine vs. untreated controls for transplant-free survival in patients with spontaneous severe AE of CHB (OR = 0.98 (95% CI, 0.50–1.92; p = 0.956)) [60]. According to the reports of previous studies, lamivudine treatment did not seem to improve survival in CHB with severe AE, but if lamivudine is started early enough before bilirubin level exceeds 20 mg/dL or in patients with less severe liver disease indicated by a MELD score of 20–30, lamivudine treatment is associated with improved survival.
Table 4.
Lamivudine treatment for chronic hepatitis B with severe acute exacerbation.
| Authors | Design | Treatment (Patient Number) | HBV DNA | Mortality (%) | p-Value | Prognostic Factors |
|---|---|---|---|---|---|---|
| Chan et al. [58] | Retrospective study | LMV (28) | N/A | 21.4% | 0.62 | Platelet |
| Control group (18) | 27.8% | Bilirubin | ||||
| Tsubota et al. [59] | Retrospective study | LMV (25) | 220 * | 12% | 0.15 | Bilirubin |
| Cirrhosis | ||||||
| Control group (25) | 120 * | 16% | Prothrombin time | |||
| Chien et al. [16] | Retrospective study | All patients | Prothrombin time | |||
| LMV (60) | 22 ** | 38% | 0.166 | Child–Pugh scores | ||
| Control group (31) | 58.6 ** | 29% | ||||
| Bilirubin > 20 mg/dL | ||||||
| Bilirubin LMV (35) | N/A | 66% | NS | |||
| Control group (11) | N/A | 36% | ||||
| Bilirubin < 20 mg/dL | ||||||
| LMV (25) | N/A | 0% | 0.013 | |||
| Control group (20) | N/A | 25% | ||||
| Sun et al. [17] | Retrospective study | MELD: 20–30 | LMV treatment | |||
| LMV (76) | 86 *** | 50.7% | 0.002 | HBV DNA | ||
| Control group (76) | 89 *** | 75.7% | Decline of HBV DNA | |||
| MELD > 30 | ||||||
| LMV (54) | 65 *** | 98% | 0.296 | |||
| Control group (54) | 67 *** | 100% |
LMV: lamivudine; MELD: the model for end-stage liver disease; N/A: not analyzed; NS: non-significant; * MEq/mL; ** pg/mL; *** Percentage >105 copies/ML.
5.3. Entecavir
Several retrospective studies compared the effect of entecavir and symptomatic treatment in CHB with severe AE (Table 5). Chen et al. [61] in a retrospective cohort study that compared the treatment effect of entecavir in 55 CHB patients with severe AE vs. 74 controls found that 36 (65.5%) entecavir-treated patients vs. 55 (74.3%) controls survived for more than three months (p = 0.28), although the entecavir-treated group had a significantly greater HBV DNA suppression at 3 months compared with the control group. In a retrospective study that compared the treatment effect of entecavir in 42 CHB patients with severe AE vs. 34 controls, Chen et al. [62] found that nine (21.4%) in the entecavir-treated group and 20 (58.8%) in the control group died (p = 0.007). Ma et al. [63] in a retrospective cohort study that compared the treatment effect of entecavir on CHB patients with severe AE vs. controls found that 1- and 3-month survival rates of patients in the entecavir-treated group (n = 124) were 72.58% and 61.29%, respectively, which were significantly higher than 53.23% and 45.97%, respectively in the control group (n = 124) (p = 0.022). Survival benefit of entecavir in CHB patients with severe AE has not been proved in randomized controlled studies, although several retrospective studies found that entecavir may achieve better survival than symptomatic treatment. A recent meta-analysis by Zhang et al. [64] found that entecavir significantly improved survival at 12 weeks (p = 0.0008). Another meta-analysis by Yu et al. [65] also found that CHB related ACLD receiving NA including entecavir had significantly lower 3-month mortality (p < 0.01) as well as incidence of reactivation (p < 0.01). Lange et al. [66] found the development of lactic acidosis may likely be the consequence of mitochondrial toxicity in 5 out of 16 patients with cirrhosis and advanced liver disease and a MELD score >20 treated with ETV. So the authors advised caution in administration of ETV in patients with severe liver function impairments. However, the actual risk of lactic acidosis in patients with acute exacerbation or decompensated CHB who received ETV treatment remains controversial and most probably low [67,68].
Table 5.
Entecavir treatment for chronic hepatitis B with severe acute exacerbation.
| Authors | Design | Treatment (Patient Number) | HBV DNA | Mortality (%) | p-Value | Prognostic Factors |
|---|---|---|---|---|---|---|
| Chen et al. [61] | Retrospective study | ETV (55) | 5.7 * | 29.5% | 0.28 | Albumin |
| Bilirubin | ||||||
| Control group (74) | 5.1 * | 34.5% | Prothrombin time (INR) | |||
| MELD score | ||||||
| Chen et al. [62] | Retrospective study | ETV (42) | 7.0 ** | 21.4% | 0.007 | Bilirubin |
| Cholesterol | ||||||
| Control group (34) | 5.7 ** | 58.8% | Prothrombin activity MELD-Na score | |||
| Ma et al. [63] | Retrospective study | ETV (124) | 6.2 | 39% | 0.022 | Bilirubin |
| Prothrombin time (INR) | ||||||
| Control group (124) | 6.4 | 54% | More than 2 comlications | |||
| Zhang et al. [64] | Meta-analysis | ETV (115) | N/A | 43% | 0.0008 | N/A |
| Control group (109) | 66% | |||||
| Yu et al. [65] | Meta-analysis | ETV/LMV (495) | N/A | 45% | <0.01 | N/A |
| Control group (270) | 73% |
LMV: lamivudine; MELD: the model for end-stage liver disease; * log copies/mL; ** Log IU/mL; N/A: not analyzed.
5.5. Tenofovir
A recent study from India by Garg et al. [69] found that the probability of survival in patients with severe spontaneous reactivation of CHB presenting as acute-on-chronic liver failure was higher in the tenofovir than the placebo group (8/14 [57%] vs. 2/13 [15%], respectively; p = 0.03). Moreover, >2 log reduction in HBV DNA levels at two weeks was found to be an independent predictor of survival (Table 6). The present findings also confirm that if an antiviral agent has profound viral suppression at two weeks, a survival benefit is anticipated. In this study, only patients with HBV DNA levels exceeding 105 copies/mL, who were in Stage II or III but not Stage IV of AE (Figure 2), were enrolled. In patients in Stage IV of AE, the immune storm due to flare-up of HBV has already been initiated and got exacerbated, which induces the rapid decline of HBV DNA, so the success of antiviral treatment is not anticipated (Figure 2). Many previous studies failed to show the benefit of nucleos(t)ide analogue in the treatment of CHB with severe AE, probably because most of these studies enrolled patients not only in Stages II, III and but also Stage IV of AE (Figure 1B).
Table 6.
Tenofovir treatment for chronic hepatitis B with severe acute exacerbation.
| Authors | Design | Treatment (Patient Number) | HBV DNA (IU/mL) | Mortality (%) | p-Value | Prognostic Factors |
|---|---|---|---|---|---|---|
| Garg et al. [69] | Randomized study | TDF (14) | 7.5 × 105 | 43% | 0.03 | >2 log reduction in HBV DNA at 2 weeks |
| Cotnrol group (13) | 1.7 × 106 | 85% |
TDF: tenofovir.
5.6. Treatment Efficacy of Different Nucleos(t)ide Analogues
5.6.1. Lamivudine vs. Entecavir
Comparison of the treatment efficacy of lamivudine vs. entecavir is shown in Table 7. Cui et al. [70] in a retrospective study that compared the treatment effect of entecavir in 33 CHB patients with severe AE vs. that of lamivudine in 34 counterparts found that 48.5% entecavir-treated vs. 50% lamivudine-treated patients survived for more than three months (p = 0.72). Chen et al. [61] in a retrospective study that compared the treatment effect of entecavir in 42 CHB patients with severe AE vs. that of lamivudine in 30 counterparts found that three-month mortality was 33% in entecavir-treated vs. 40% in lamivudine-treated patients (p = 0.374). Lai et al. [71] in a retrospective study that compared the treatment effect of entecavir in 93 CHB patients with severe AE vs. that of lamivudine in 89 counterparts found that the mortality rate was 91.7% in entecavir-treated vs. 92% in lamivudine-treated patients (p = 0.680). Liu et al. [72] in a retrospective study that compared the treatment effect of entecavir in 31 CHB patients with severe AE vs. that of lamivudine in 34 counterparts found that the mortality rate was 0% in entecavir-treated vs. 3% in lamivudine-treated patients (p = 0.385). Zhang et al. [73] in a retrospective study that compared the treatment effect of entecavir in 65 CHB patients with severe AE vs. that of lamivudine in 54 counterparts found that 51 (78.5%) in the entecavir group and 35 (64.8%) in the lamivudine group survived at day 60 (p = 0.066). Chen et al. [74] in a retrospective study that compared the treatment effect of entecavir in 107 CHB patients with severe AE vs. that of lamivudine in 215 counterparts found that the overall mortality in the entecavir and lamivudine groups at 24 week was 21.2% and 12.3%, respectively (p = 0.02). However, in the present study, the lamivudine group had a significantly lower albumin level and a higher MELD score at baseline. In addition, multivariate analysis did not identify entecavir treatment as an independent factor associated with survival. But the entecavir group achieved better virological response than the lamivudine group at week 24 and 48. Wong et al. [75] in a retrospective study that compared the treatment effect of entecavir in 36 CHB patients with severe AE vs. that of lamivudine in 117 counterparts found that seven (19%) patients in the entecavir group and five (4%) patients in the lamivudine group died (p = 0.010). Multivariate analysis also identified entecavir treatment as an independent factor associated with mortality. But entecavir treatment resulted in more rapid and complete viral suppression, with more patients achieving undetectable HBV DNA at week 48, compared to the lamivudine group. Previous studies by Chien et al. [16] and Sun et al. [17] have found that if lamivudine was given in an earlier stage of severe AE, such as in Stage II or III (Figure 2), a survival benefit could be attained. Most of the previous studies that compared the efficacy of lamivudine and entecavir enrolled patients with mild and severe liver disease in Stages II, III and also Stage IV of AE (Figure 2). In a recent retrospective study, Tsai et al. [76] compared the treatment effect of entecavir vs. lamivudine in CHB patients with severe AE having HBV DNA levels above 105 copies/mL and bilirubin levels below 15 mg/dL. They found that 5 out of 40 patients (12.5%) in the entecavir group and 1 out of 59 patients (1.7%) in the lamivudine group died. Multivariate analysis found that entecavir treatment was associated with more mortality than lamivudine (p = 0.035). Early entecavir treatment for CHB with severe AE seemed to have a higher mortality than lamivudine treatment. Ye et al. [77] in a recent meta-analysis of 12 randomized controlled studies that compared treatment of lamivudine (N = 450) with entecavir (N = 423) in decompensated HBV cirrhosis found that, despite the better suppression of viral load in entecavir recipients, the mortality rate in lamivudine and entecavir recipients with decompensated cirrhosis was similar ranging between 7.89% and 6.37% respectively. In this meta-analysis the safety record for both anti-viral agents was similar. Another meta-analysis by Yu et al. [65] also found that there is no difference in short term mortality in patients treated with entecavir or lamivudine (36.4% vs. 40.4% respectively) in HBV-related acute-on-chronic liver failure. According to previous findings, there is no firm conclusion on whether entecavir or lamivudine treatment promises a better outcome for CHB with severe AE. Further randomized study that compare the efficacy of lamivudine vs. entecavir is required. However, lamivudine is limited by its high rate of resistance in the treatment of CHB [78,79]. Long-term follow-up study also found that lamivudine treatment for CHB with SAE resulted in a high rate of drug resistance and virological breakthrough [80]. Current AASLD (2009) and EASL (2012) guidelines do not recommend a specific NA for treatment of decompensated chronic liver disease or acute exacerbation, although there is a consensus that suggested treatment with a potent anti-viral agent [81,82]. Lamivudine is not inferior to entecavir in the treatment of CHB with severe AE, but lamivudine is cheaper than entecavir and is still widely used in many countries, especially in those with poor economic condition. Early short-term lamivudine use to prevent resistance followed by potent NA such as tenofovir may be another treatment option.
Table 7.
Comparison of the treatment outcome of lamivudine and entecavir in chronic hepatitis B with severe acute exacerbation.
| Authors | Design | Treatment (Patient Number) | HBV DNA (Log copies/mL) | Mortality (%) | p-Value | Prognostic Factors |
|---|---|---|---|---|---|---|
| Cui et al. [70] | Retrospective study | ETV (33) | 5.9 | 51.5% | 0.72 | Age |
| LMV (34) | 5.9 | 50% | cholinesterase | |||
| MELD score | ||||||
| Chen et al. [61] | Retrospective study | ETV (42) | 6.4 | 51.5% | 0.374 | Bilirubin |
| LMV (30) | 5.6 | 50% | Cholesterol | |||
| Prothrombin activity MELD-Na score | ||||||
| Lai et al. [71]. | Retrospective study | ETV (93) | 6.4 | 51.5% | 0.680 | Bilirubin |
| LMV (89) | 5.6 | 50% | Creatinine | |||
| Prothrombin time MELD score | ||||||
| Liu et al. [72] | Retrospective study | ETV (31) | 6.2 | 0% | 0.385 | N/A |
| LMV (34) | 7.0 | 3% | ||||
| Zhang et al. [73] | Retrospective study | ETV (65) | 7.0 | 21.5% | 0.066 | Gender |
| HBeAg(+) | ||||||
| MELD score | ||||||
| Child–Pugh scores | ||||||
| LMV (54) | 7.2 | 35.2% | Undetectable HBV at 30 days | |||
| Chen et al. [74] | Retrospective study | ETV (107) | 6.5 | 21.2% | 0.02 | MELD score |
| LMV (215) | 6.5 | 12.3% | Ascites | |||
| Hepatic enceophalopathy | ||||||
| Wong et al. [75] | Retrospective study | ETV (36) | 7.3 | 19% | 0.010 | Prothrombin time |
| LMV (117) | 7.6 | 4% | ETV treatment | |||
| Tsai et al. [76] | Retrospective study | ETV (40) | 8.3 | 12.5% | 0.035 | Prothrombin time |
| LMV (59) | 8.4 | 1.7% | ETV treatment | |||
| Ye et al. [77] | Meta-analysis | ETV (423) | N/A | 6.4% | NS | N/A |
| LMV(450) | 7.9% | |||||
| Yu et al. [65] | Meta-analysis | ETV (192) | N/A | 36.4% | 0.35 | N/A |
| LMV (148) | 40.5% |
ETV: entecavir; LMV: lamivudine; MELD: the model for end-stage liver disease; HBeAg: hepatitis B e antigen; N/A: not analyzed; NS: non-significant.
5.6.2. Entecavir vs. Tenofovir
There is only one study that compared the efficacy of entecavir vs. tenofovir in CHB with severe AE (Table 8). Hung et al. [83] in a retrospective study that compared the treatment effect of entecavir in 148 CHB patients with severe AE vs. that of tenofovir in 41 counterparts found that 23 (16%) patients in the entecavir group and 7 (17%) patients in the tenofovir group died or received liver transplantation (p = 0.749). Tenfovir and entecavir produce similar treatment responses and clinical outcomes in CHB patients with severe AE. Although tenofovir and entecavir seemed to have similar efficacy in the treatment of CHB with severe AE, a further randomized study that compared the efficacy of tenofovir vs. entecavir is required.
Table 8.
Comparison of the treatment outcome of tenofovir and entecavir in chronic hepatitis B with severe acute exacerbation.
| Authors | Design | Treatment (Patient Number) | HBV DNA (Log copies/mL) | Mortality (%) | p-Value | Prognostic Factors |
|---|---|---|---|---|---|---|
| Hung et al. [83] | Retrospective study | ETV (148) | 6.5 | 16% | 0.797 | Hypertension |
| HBV DNA | ||||||
| Platelet | ||||||
| MELD score | ||||||
| Ascites | ||||||
| Hepatic encephalopathy | ||||||
| TDF (41) | 7.0 | 17% | Hepatorenal syndrome |
ETV: entecavir, TDF: tenofovir, MELD: the model for end-stage liver disease.
5.6.3. Treatment Emergence Mutants
Nucleos(t)ide analogue treatment for chronic HBV is usually associated with the development of resistance mutant. Lamivudine treatment is associated with a resistance rate of 15%–25% per year and at five years up to 70% of patients may develop lamivudine resistance mutants [84,85]. Resistant viruses show a characteristic mutation of the 550th amino acid methionine in the tyrosine-methionine-aspartate-aspartate (YMDD) motif of DNA polymerase to isoleucine (YIDD) or valine (YVDD) [86,87]. Among chronic HBV patients with severe acute exacerbation treated with lamivudine, virological breakthrough is common [80]. Wong et al. [80] in a long-term follow-up study found that lamivudine treatment in patients with severe acute exacerbation had higher HBeAg seroconversion rates and lower risks of virological breakthrough. However 33% of patients developed lamivudine resistance mutant in five years. Among the fifteen patients with lamivudine resistance mutants, six had rtM204I, one had rtM204V, one had both rtM204I and rtM204V mutations and seven patients had rtL180M mutation. Another study by Akuta et al. [88] found the cumulative occurrence rates of YMDD mutations in SAE and non-SAE groups were 5.6% and 19.3% at one year, 34.5% and 37.3% at two years, and 34.5% and 37.3% at three years, respectively and the emergence of YMDD mutations tended to happen later in the SAE group than in the non-SAE group. Zang et al. [89] in chronic HBV with acute exacerbation under lamivudine treatment found that apart from mutations at the YMDD motif, no shared mutations were shown and strains with high replicative activity might be selected from the total HBV quasispecies during treatment, and amongst these strains, those with core promoter mutations were most likely to be related to severe clinical exacerbations. Resistance to entecavir in HBV appears to occur through a two-hit mechanism with initial selection of M204V/I mutation followed by amino acid substitutions at rtT184, rtS202, or rtM250 [90]. However resistance related to entecavir treatment in CHB is extremely low [81,82]. To date, primary resistance to tenofovir in patients with CHB mono-infection has also never been reported [81,82]. A study of CHB and HIV co-infected patients suggested a possible role of rtA194T mutation in tenofovir resistance [91]. HBV with the rtA194T mutation was shown to have a reduced susceptibility to tenofovir when combined with lamivudine resistance rtM204V and rtL180M mutations in vitro [92]. The clinical impact of the rtA194T mutation remains to be determined; tenofovir has been found to be effective in restricting the replication of HBV in patients with the rtA194T mutation [92]. The hepatitis B virus (HBV) polymerase and envelope genes overlap in such a way that resistance mutations to antiviral agents in the reverse transcriptase gene may influence the antigenicity of the HBV surface antigen [93]. Two types of surface proteins mutants are recognized. The first type occurred due to amino acids substitutions caused by primary and compensatory resistance mutations in the polymerase gene, which generates S gene mutations and the second type arose due to prolonged viral suppression leading to seroclearance of surface antigen, where vaccine-escape-like mutations might be selected [93]. A triple mutations (rtV173L + rtL180M + rtM204V) causing lamivudine resistance has recently been shown to enhance HBV replication, compared with rtL180Mt + rtM204V alone [94]. This triple HBV mutant resulted in two amino acid changes in the overlapping surface gene (sE164D + sI195M), which decrease anti-HBs binding to levels seen only with the vaccine escape mutant sG145R [95,96]. Selection of an sP120A mutation in CHB patients treated with lamivudine is also associated with the apparent HBsAg seroconversion and this mutation produces a reduced anti-HBs binding, which explains the failure to detect HBsAg [97]. Yeh et al. [98] discovered in patients treated with lamivudine who developed an rtA181T mutation that in an in vitro phenotypic assay was confirmed to be associated with lamivudine resistance and this mutation generates a stop codon in the surface antigen (sW172stop), which causes decreased secretion of the HBsAg and decreased viral fitness. Interestingly, neither the adefovir-associated resistance mutation rtN236T nor the tenofovir-associated resistance mutation rtA194T causes changes in the HBV surface gene [99]. Sloan et al. [100] in CHB treated with lamivudine, adenofovr and entecavir found that the mutations rtF166L/sF158Y (lamivudine-related, compensatory) and rtl169T/sF161L (entecavir-related, primary) acting alone, and the mutations rtV173L/sE164D (lamivudine-related, compensatory) and rtSilent/sD144E (antibody escape-related) each when combined with rtM204V/sl195M (lamivudine-associated, primary) resulted in decreases in antibody reactivity to epitopes in the first or second loop, or in both loops. HBV was also found to be able to develop the commensurate rtV173L mutation in the polymerase protein, which restore the replication phenotype of lamivudine resistant HBV [94,101].
6. Prognostic Factors
The mortality rate of CHB with severe AE after introduction of antiviral agents has been examined. In patients who received lamivudine, the mortality rate ranged from 12%–98% according to the severity of disease at exacerbation (Table 2). Dai et al. [102] in a study of 96 patients of CHB with severe AE who received lamivudine treatment found that The MELD and Index scoring systems were good predictors of 6-month survival. In patients who received lamivudine before bilirubin rose above 20 mg/dL, the mortality rate was 0%, whereas if lamivudine was started after bilirubin exceeded 20 mg/dL, the mortality rate increased to 66% [16]. In patients with MELD scores of 20–30, lamivudine treatment had a mortality rate of 50.7% but in patients with MELD scores exceeding 30, the mortality rate rose to 98% [17]. The prognostic factors associated with lamivudine treatment included platelet count, bilirubin level, prothrombin time, cirrhosis of liver and Child-Pugh scores (Table 4). In patients who received entecavir, the mortality rate ranged from 21% to 51.5%. Yan et al. [103] in a retrospective study that evaluated the prognostic factors of entecavir treatment of 109 CHB patients with severe AE found that MELD score ≥30 predicted very poor prognosis due to fatal liver failure. The prognostic factors associated with entecavir treatment included age, albumin, bilirubin, prothrombin time, ascites, hepatic encephalopathy and MELD score (Table 5). In patients who received tenofovir, the mortality rate ranged from 17% to 43%. The prognostic factors associated with tenofovir treatment included >2 log reduction in HBV DNA at two weeks, hypertension, HBV DNA, platelet count, MELD score, ascites, hepatic encephalopathy, and hepatorenal syndrome (Table 6 and Table 7). In general, liver reserve on presentation including albumin, bilirubin, and prothrombin time and MELD score is the major prognostic factor in CHB with severe AE under antiviral treatment.
An early and accurate prognostic system based on the integration of laboratory indicators, clinical events and some mathematic logistic equations is needed to optimize treatment for patients of CHB with SAE. Several scoring systems have been developed to predict the prognosis of CHB with severe AE. The MELD score was the most common and the donor-MELD was the most innovative for patients on the waiting list for liver transplantation [104,105]. The guideline of the Asian Pacific Association for the Study of the Liver (APASL) recommended that patients with HBV reactivation with intermediate MELD should be assessed for early transplant if cirrhosis, bilirubin > 10 mg/dL, PT < 40%, and platelet < 1.00 × 1011/L [106]. Greater than 2 log reduction in HBV DNA at 2 weeks is the most important on-treatment prognostic factor in CHB with SAE. The role of HBV DNA as an independent prognostic factor in CHB with severe AE is controversial. Many studies did not confirm the prognostic role of HBV DNA [16,58,59,61,62,63]. Only few studies identified HBV DNA as an independent prognostic factor in CHB with severe AE undergoing antiviral treatment. Hung et al. [83] in a retrospective study that compared the treatment effect of entecavir and tenofovir in CHB with severe AE found that baseline HBV DNA is an independent factors for mortality or liver transplantation. Hsu et al. [107] in another retrospective study of 66 CHB patients with severe AE who received antiviral treatment found that pretreatment HBV DNA level stratified the risk of death. In a study on lamivudine treatment for CHB with severe AE, Chien et al. [16] found that patients with undetectable serum HBV DNA levels had significantly higher bilirubin levels than those with detectable serum HBV DNA. Apart from this, similar clinical features and mortality rates were observed between those with undetectable and detectable serum HBV DNA levels in both groups (5/11 or 45% vs. 18/49 or 37% in the lamivudine treated group and 0/3 or 0% vs. 10/28 or 36% in the control group; p > 0.05). The role of HBV DNA as an independent prognostic factor in CHB with severe AE undergoing antiviral treatment has not been confirmed.
7. Conclusions
CHB with spontaneous AE is not uncommon. These exacerbations can be mild, but some patients may develop hepatic decompensation and even die. The underlying pathogenesis of CHB with spontaneous AE is a dynamic process of immune response between HBV and the host. The benefit of nucleos(t)ide analogues (NA) treatment in CHB with severe AE is controversial. Early lamivudine treatment before the bilirubin level exceeded 20 mg/dL or a MELD score below 30 seemed to be associated with an improved outcome. Tenofovir has also been found to be associated with better outcomes in CHB with severe AE with a high HBV DNA level. The survival benefit of different NAs has not been confirmed in a randomized study in the setting of CHB with severe AE. However, early NA use with potent agents and good resistance profile is recommended in all CHB patients with severe AE.
Author Contributions
Wei-Lun Tsai collected data and wrote the manuscript, Wei-Chi Sun collected data, Jin-Shiung Cheng collected data and gave comments.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Lee W. Hepatitis B infection. N. Engl. J. Med. 1997;337:1733–1745. doi: 10.1056/NEJM199712113372406. [DOI] [PubMed] [Google Scholar]
- 2.Lok A.S., Lai C.L. Acute exacerbations in Chinese patients with chronic hepatitis B virus (HBV) infection. Incidence, predisposing factors and etiology. J. Hepatol. 1990;10:29–34. doi: 10.1016/0168-8278(90)90069-4. [DOI] [PubMed] [Google Scholar]
- 3.Seeff L.B., Koff R.S. Evolving concepts of the clinical and serological consequences of hepatitis B infection. Semin. Liver Dis. 1986;6:11–22. doi: 10.1055/s-2008-1040788. [DOI] [PubMed] [Google Scholar]
- 4.Liaw Y.F. Acute exacerbation and superinfection in patients with chronic viral hepatitis. J. Formos. Med. Assoc. 1995;94:521–528. [PubMed] [Google Scholar]
- 5.Sheen I.S., Laiw Y.F., Tai D.I., Chu C.M. Hepatic decompensation associated with hepatitis B e antigen clearance in chronic type B hepatitis. Gastroenterology. 1985;89:732–735. doi: 10.1016/0016-5085(85)90566-9. [DOI] [PubMed] [Google Scholar]
- 6.Davis G.L., Hoofnagle J.H., Waggoner J.G. Reactivation of chronic type B hepatitis B presenting as acute viral hepatitis. Ann. Intern. Med. 1985;102:762–765. doi: 10.7326/0003-4819-102-6-762. [DOI] [PubMed] [Google Scholar]
- 7.Sarin S., Kumar A., Almeida J. Acute-on-chronic liver failure: Consensus recommendations of the Asian Pacific Association for the Study of the Liver (APASL) Hepatol. Int. 2009;3:269–282. doi: 10.1007/s12072-008-9106-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chang M.L., Liaw Y.F. Hepatitis B flares in chronic hepatitis B: Pathogenesis, natural course, and management. J. Hepatol. 2014;61:1407–1417. doi: 10.1016/j.jhep.2014.08.033. [DOI] [PubMed] [Google Scholar]
- 9.Lok A.S., McMahon B.J. Practice guidelines committee, American Association for the study of liver diseases: Chronic hepatitis B. Hepatology. 2001;34:1225–1241. doi: 10.1053/jhep.2001.29401. [DOI] [PubMed] [Google Scholar]
- 10.Perrillo R.P. Acute flares in chronic hepatitis B: The natural and unnatural history of an immunologically mediated liver disease. Gastroenterology. 2001;120:1009–1022. doi: 10.1053/gast.2001.22461. [DOI] [PubMed] [Google Scholar]
- 11.Hoofnagel J.H. Reactivation of hepatitis B. Hepatology. 2009;49:S156–S165. doi: 10.1002/hep.22945. [DOI] [PubMed] [Google Scholar]
- 12.Tsai S.L., Chert P.J., Lai M.Y., Yang P.M., Sung J.L., Huang J.H., Hwang L.H., Chen D.S. Acute exacerbations of chronic type B hepatitis are accompamed by increased T cell responses to hepatitis B core and e antigens. Implicabons for hepatitis B e atigen seroconversion. J. Chin. Investig. 1992;89:87–96. doi: 10.1172/JCI115590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Milich D.R., McLachlan A., Stahl S., Wingfleld P., Thornton G.B., Hughes J.L., Jones J.E. Comparative immunogeniclty of hepatitis B virus core and E antigens. J. Immunol. 1988;141:3617–3624. [PubMed] [Google Scholar]
- 14.Waters J.A., O’Rourke S., Schhct H.J., Thomas H.C. Cytotoxic T cell responses in patients with chronm hepatltrs B virus infection undergoing HBe antigen/antibody seroconverslon. Chin. Exp. Immunol. 1995;102:314–319. doi: 10.1111/j.1365-2249.1995.tb03783.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bertolettl A., Ferrari C., Flaccadon F., Penna A., Margolskee R., Schhcht H.J., Fowler P., Gullhot S., Chsarl F.V. HLA class I-restricted human cytotoxic T cells recognize endogenously synthesized hepatitis B virus nucleocapsid antigen. Proc. Natl. Acad. Sci. USA. 1991;88:10445–10449. doi: 10.1073/pnas.88.23.10445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chien R.N., Lin C.H., Liaw Y.F. The effect of lamivudine therapy in hepatic decompensation during acute exacerbation of chronic hepatitis B. J. Hepatol. 2003;38:322–327. doi: 10.1016/S0168-8278(02)00419-1. [DOI] [PubMed] [Google Scholar]
- 17.Sun L.J., Yu J.W., Zhao Y.H., Kang P., Li S.C. Influential factors of prognosis in lamivudine treatment for patients with acute-on-chronic hepatitis B liver failure. J. Gastroenterol. Hepatol. 2010;25:583–590. doi: 10.1111/j.1440-1746.2009.06089.x. [DOI] [PubMed] [Google Scholar]
- 18.Chu C.M., Karayiannis P., Fowler M.J., Maujardino J., Liaw Y.F., Thomas H.C. Natural history of chronic hepatitis B virus infection in Taiwan: Studies of hepatitis B virus DNA in serum. Hepatology. 1985;5:431–434. doi: 10.1002/hep.1840050315. [DOI] [PubMed] [Google Scholar]
- 19.Liaw Y.F., Chu C.M. Hepatitis, B virus infection. Lancet. 2009;373:582–592. doi: 10.1016/S0140-6736(09)60207-5. [DOI] [PubMed] [Google Scholar]
- 20.Liaw Y.F., Tai D.I., Chu C.M., Pao C.C., Chen T.J. Acute exacerbation in chronic type B hepatitis: Comparison between HBeAg and antibody positive patients. Hepatology. 1987;7:20–23. doi: 10.1002/hep.1840070106. [DOI] [PubMed] [Google Scholar]
- 21.Hsu Y.S., Chien R.N., Yeh C.T., Sheen I.S., Chiou H.Y., Chu C.M., Liaw Y.F. Long-term outcome after spontaneous HBeAg seroconversion in patients with chronic hepatitis B. Hepatology. 2002;35:1522–1527. doi: 10.1053/jhep.2002.33638. [DOI] [PubMed] [Google Scholar]
- 22.Liaw Y.F., Chen J.J., Chen T.J. Acute exacerbation in patients with liver cirrhosis: A clinicopathological study. Liver. 1990;10:177–184. doi: 10.1111/j.1600-0676.1990.tb00455.x. [DOI] [PubMed] [Google Scholar]
- 23.Yuen M.F., Sablon E., Hui C.K., Li T.M., Yuan H.J., Wong D.K., Doutreloigne J., Bogaerts V., Wong B.C., Fan S.T., et al. Prognostic factors in severe exacerbation of chronic hepatitis B. Clin. Infect. Dis. 2003;36:979–984. doi: 10.1086/374226. [DOI] [PubMed] [Google Scholar]
- 24.Tsai W.L., Lo G.H., Hsu P.I., Lai K.H., Lin C.K., Chan H.H., Chen W.C., Cheng J.S., Liu Y.C., Huang T.S., et al. Role of genotype and precore/basal core promoter mutations of hepatitis B virus in patients with chronic hepatitis B with acute exacerbation. Scand. J. Gastroenterol. 2008;43:196–201. doi: 10.1080/00365520701745693. [DOI] [PubMed] [Google Scholar]
- 25.Chan H.L., Tsang S.W., Wong M.L., Tse C.H., Leung N.W., Chan F.K., Sung J.J. Genotype B hepatitis B virus is associated with severe icteric flare-up of chronic hepatitis B virus infection in Hong Kong. Am. J. Gastroenterol. 2002;97:2629–2633. doi: 10.1111/j.1572-0241.2002.06065.x. [DOI] [PubMed] [Google Scholar]
- 26.Yuen M.F., Sablon E., Wong D.K., Yuan H.J., Wong B.C., Chan A.O., Lai C.L. Role of hepatitis B virus genotypes in chronic hepatitis B exacerbation. Clin. Infect. Dis. 2003;37:593–597. doi: 10.1086/376988. [DOI] [PubMed] [Google Scholar]
- 27.Imamura T., Yokosuka O., Kurihara T., Kanda T., Fukai K., Imazeki F., Saisho H. Distribution of hepatitis B viral genotypes and mutations in the core promoter and precore regions in acute forms of liver disease in patients from Chiba, Japan. Gut. 2003;52:1630–1637. doi: 10.1136/gut.52.11.1630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ren X., Xu Z., Liu Y., Li X., Bai S., Ding N., Zhong Y., Wang L., Mao P., Zoulim F., et al. Hepatitis B virus genotype and basal core promoter/precore mutations are associated with hepatitis B-related acute-on-chronic liver failure without pre-existing liver cirrhosis. J. Viral Hepat. 2010;17:887–895. doi: 10.1111/j.1365-2893.2009.01254.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liu C.J., Kao J.H., Lai M.Y., Chen P.J., Chen D.S. Precore/corepromoter mutations and genotypes of hepatitis B virus inchronic hepatitis B patients with fulminant or subfulminant hepatitis. J. Med. Virol. 2004;72:545–550. doi: 10.1002/jmv.20024. [DOI] [PubMed] [Google Scholar]
- 30.Yuen M.F., Sablon E., Yuan H.J., Wong D.K., Hui C.K., Wong B.C., Chan A.O., Lai C.L. Significance of hepatitis B genotype in acute exacerbation, HBeAg seroconversion, cirrhosis-related complications, and hepatocellular carcinoma. Hepatology. 2003;37:562–567. doi: 10.1053/jhep.2003.50098. [DOI] [PubMed] [Google Scholar]
- 31.Omata M., Ehata T., Yokosuka O., Hosoda K., Ohto M. Mutations in the precore region of hepatitis B virus DNA in patients with fulminant and severe hepatitis. N. Engl. J. Med. 1991;324:1699–1704. doi: 10.1056/NEJM199106133242404. [DOI] [PubMed] [Google Scholar]
- 32.Yuan H.J., Yuen M.F., Wong D.K., Sum S.M., Doutreloigne J., Sablon E., Lai C.L. Determinants for the occurrence of acute axacerbation of hepatitis B virus infection in Chinese patients after HBeAg sero clearance. J. Clin. Microbiol. 2005;43:1594–1599. doi: 10.1128/JCM.43.4.1594-1599.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kusumoto K., Yatsuhashi H., Nakao R., Hamada R., Fukuda M., Tamada Y., Taura N., Komori A., Daikoku M., Hamasaki K., et al. Detection of HBV core romoter and precore mutations helps distinguish flares of chronic hepatitis from acute hepatitis B. J. Gastroenterol. Hepatol. 2008;23:790–793. doi: 10.1111/j.1440-1746.2008.05391.x. [DOI] [PubMed] [Google Scholar]
- 34.Ehata T., Omata M., Chuang W.L., Yokosuka O., Ito Y., Hosoda K., Ohto M. Mutations in core nucleotide sequence of hepatitis B virus correlate with fulminant and severe hepatitis. J. Clin. Investig. 1993;91:1206–1213. doi: 10.1172/JCI116281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Liu C.J., Chen P.J., Lai M.Y., Kao J.H., Chang C.F., Wu H.L., Shau W.Y., Chen D.S. A prospective study characterizing full-length hepatitis B virus genomes during acute exacerbation. Gastroenterology. 2003;124:80–90. doi: 10.1053/gast.2003.50003. [DOI] [PubMed] [Google Scholar]
- 36.Liu C.J., Kao J.H., Wang H.Y., Lai M.Y., Chen T.C., Chen P.J., Chen D.S. Origin of serum hepatitis B virus in acute exacerbation: Comparison with HBV in the liver and from other exacerbation. Hepatology. 2004;40:310–317. doi: 10.1002/hep.20331. [DOI] [PubMed] [Google Scholar]
- 37.Chang J., Block T.M., Guo J.T. The innate immune response to hepatitis B virus infection: Implications for pathogenesis and therapy. Antivir. Res. 2012;96:405–413. doi: 10.1016/j.antiviral.2012.10.001. [DOI] [PubMed] [Google Scholar]
- 38.Chang J.J., Lewin S.R. Immunopathogenesis of hepatitis B virus infection. Immunol. Cell Biol. 2007;85:16–23. doi: 10.1038/sj.icb.7100009. [DOI] [PubMed] [Google Scholar]
- 39.Mels G.C., Bellatl G., Leandro G., Brunetto M.R., Vican O., Borzlo M., Piantino P., Fornaclan G., Scudeller G., Angeh G., et al. Fluctuations in vlremla, amlnotransferases and IgM antibody to hepatitis B core antigen in chronic hepatitis B patients with disease exacerbations. Liver. 1994;14:175–181. doi: 10.1111/j.1600-0676.1994.tb00071.x. [DOI] [PubMed] [Google Scholar]
- 40.Liaw Y.F., Pao C.C., Chu C.M., Sheen I.S., Huang M.J. Changes of serum hepatitis B virus DNA in two types of clinical events preceding spontaneous hepatitis B e antigen seroconversion in chronic type B hepatitis. Hepatology. 1987;7:1–3. doi: 10.1002/hep.1840070102. [DOI] [PubMed] [Google Scholar]
- 41.Liaw Y.F., Pao C.C., Chu C.M. Changes of serum HBV DNA in relation to serum transaminase level during acute exacerbation in patients with chronic type B hepatitis. Liver. 1988;8:231–235. doi: 10.1111/j.1600-0676.1988.tb00998.x. [DOI] [PubMed] [Google Scholar]
- 42.Yang P.M., Su I.J., Lat M.Y., Huang G.T., Hsu H.C., Chen D.S., Sung J.L. Immunohistochemical studies on intrahepatic lymphocyte infiltrates in chronic type B hepatitis, with spectal emphasis on the activation status of the lymphocytes. Am. J. Gastroenterol. 1988;83:948–953. [PubMed] [Google Scholar]
- 43.Lowin B., Hahne M., Mattmann C., Tschopp J. Cytolybc T-cell cytotoxicty is medtated through perforin and Fas lytic pathways. Nature. 1994;370:650–652. doi: 10.1038/370650a0. [DOI] [PubMed] [Google Scholar]
- 44.Takehara T., Hayashi N., Katayama K., Kasahara A., Fusamoto H., Kamada T. Hepatitis B core antigen-specific interferon gamma production of peripheral blood mononuclear cells during acute exacerbation of chronic hepatitis B. Scand. J. Gastroenterol. 1992;27:727–731. doi: 10.3109/00365529209011173. [DOI] [PubMed] [Google Scholar]
- 45.Fukuda R., Ishimura N., Nguyen T.X., Chowdhury A., Ishihara S., Kohge N., Akagi S., Watanabe M., Fukumoto S. The expression of IL-2, IL-4 and interferon-gamma (IFN-γ) mRNA using liver biopsies at different phases of acute exacerbation of chronic hepatitis B. Clin. Exp. Immunol. 1995;100:446–451. doi: 10.1111/j.1365-2249.1995.tb03720.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zhang J.Y., Zhang Z., Lin F., Zou Z.S., Xu R.N., Jin L., Fu J.L., Shi F., Shi M., Wang H.F., et al. Interleukin-17-producing CD4+ T cells increase with severity of liver damage in patients with chronic hepatitis B. Hepatology. 2010;51:81–91. doi: 10.1002/hep.23273. [DOI] [PubMed] [Google Scholar]
- 47.Wu H.L., Kao J.H., Chen T.C., Wu W.H., Liu C.H., Su T.H., Yang H.C., Chen D.S., Chen P.J., Liu C.J. Serum cytokine/chemokine profiles in acute exacerbation of chronic hepatitis B: Clinical and mechanistic implications. J. Gastroenterol. Hepatol. 2014;29:1629–1636. doi: 10.1111/jgh.12606. [DOI] [PubMed] [Google Scholar]
- 48.Dunn C., Brunetto M., Reynolds G., Christophides T., Kennedy P.T., Lampertico P., Das A., Lopes A.R., Borrow P., Williams K., et al. Cytokines induced during chronic hepatitis B virus infection promote a pathway for NK cell-mediated liver damage. J. Exp. Med. 2007;204:667–680. doi: 10.1084/jem.20061287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tan A.T., Koh S., Goh W., Zhe H.Y., Gehring A.J., Lim S.G., Bertoletti A. A longitudinal analysis of innate and adaptive immune profile during hepatic flares in chronic hepatitis B. J. Hepatol. 2010;52:330–339. doi: 10.1016/j.jhep.2009.12.015. [DOI] [PubMed] [Google Scholar]
- 50.Wenjin Z., Chuanhui P., Yunle W., Lateef S.A., Shusen Z. Longitudinal fluctuations in PD1 and PD-L1 expression in association with changes in anti-viral immune response in chronic hepatitis B. BMC Gastroenterol. 2012;12:109. doi: 10.1186/1471-230X-12-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chen Z., Cheng Y., Xu Y., Liao J., Zhang X., Hu Y., Zhang Q., Wang J., Zhang Z., Shen F., et al. Expression profiles and function of Toll-like receptors 2 and 4 in peripheral blood mononuclear cells of chronic hepatitis B patients. Clin. Immunol. 2008;128:400–408. doi: 10.1016/j.clim.2008.04.006. [DOI] [PubMed] [Google Scholar]
- 52.Wang K., Liu H., He Y., Chen T., Yang Y., Niu Y., Chen H., Chen Y., Liu J., Ye F., et al. Correlation of TLR1–10 expression in peripheral blood mononuclear cells with chronic hepatitis B and chronic hepatitis B-related liver failure. Hum. Immunol. 2010;71:950–956. doi: 10.1016/j.humimm.2010.07.013. [DOI] [PubMed] [Google Scholar]
- 53.Bañares R., Catalina M.V., Vaquero J. Molecular adsorbent recirculating system and bioartificial devices for liver failure. Clin. Liver Dis. 2014;18:945–956. doi: 10.1016/j.cld.2014.07.011. [DOI] [PubMed] [Google Scholar]
- 54.Polson J., Lee W.M. AASLD position paper: The management of acute liver failure. Hepatology. 2005;41:1179–1197. doi: 10.1002/hep.20703. [DOI] [PubMed] [Google Scholar]
- 55.Hassanein T.I., Schade R.R., Hepburn I.S. Acute-on-chronic liver failure: Extracorporeal liver assist devices. Curr. Opin. Crit. Care. 2011;17:195–203. doi: 10.1097/MCC.0b013e328344b3aa. [DOI] [PubMed] [Google Scholar]
- 56.Kribben A., Gerken G., Haag S., Herget-Rosenthal S., Treichel U., Betz C., Sarrazin C., Hoste E., van vlierberghe H., Escorsell A., et al. HELIOS Study Group. Effects of fractionated plasma separation and adsorption on survival in patients with acute-on-chronic liver failure. Gastroenterology. 2012;142:782–789. doi: 10.1053/j.gastro.2011.12.056. [DOI] [PubMed] [Google Scholar]
- 57.Bañares R., Nevens F., Larsen F.S., Jalan R., Albillos A., Dollinger M., Saliba F., Sauerbruch T., Klammt S., Ockenga J., et al. Extracorporeal albumin dialysis with the molecular adsorbent recirculating system in acute-on-chronic liver failure: The RELIEF trial. Hepatology. 2013;57:1153–1162. doi: 10.1002/hep.26185. [DOI] [PubMed] [Google Scholar]
- 58.Chan H.L., Tsang S.W., Hui Y., Leung N.W., Chan F.K., Sung J.J. The role of lamivudine and predictors of mortality in severe flare-up of chronic hepatitis B with jaundice. J. Viral. Hepat. 2002;9:424–428. doi: 10.1046/j.1365-2893.2002.00385.x. [DOI] [PubMed] [Google Scholar]
- 59.Tsubota A., Arase Y., Suzuki Y., Sezaki H., Hosaka T., Akuta N., Someya T., Kobayashi M., Saitoh S., Ikeda K., et al. Lamivudine monotherapy for spontaneous severe acute exacerbation of chronic hepatitis B. J. Gastroenterol. Hepatol. 2005;20:426–432. doi: 10.1111/j.1440-1746.2004.03534.x. [DOI] [PubMed] [Google Scholar]
- 60.Yu W., Zhao C., Shen C., Wang Y., Lu H., Fan J. The efficacy and safety of Nucleos(t)ide analogues in patients with spontaneous acute exacerbation of chronic hepatitis B: A systematic review and meta-analysis. PLoS ONE. 2013;8:e65952. doi: 10.1371/journal.pone.0065952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Chen J., Han J.H., Liu C., Yu R.H., Li F.Z., Li Q.F., Gong G.Z. Short-term entecavir therapy of chronic severe hepatitis B. Hepatobiliary Pancreat. Dis. Int. 2009;8:261–266. [PubMed] [Google Scholar]
- 62.Chen T., He Y., Liu X., Yan Z., Wang K., Liu H., Zhang S., Zhao Y. Nucleoside analogues improve the short-term and long-term prognosis of patients with hepatitis B virus-related acute-on-chronic liver failure. Clin. Exp. Med. 2012;12:159–164. doi: 10.1007/s10238-011-0160-7. [DOI] [PubMed] [Google Scholar]
- 63.Ma K., Guo W., Han M., Chen G., Chen T., Wu Z., Yang D., Huang J., Huang Y., Zhao X., et al. Entecavir treatment prevents disease progression in hepatitis B virus-related acute-on-chronic liver failure: Establishment of a novel logistical regression model. Hepatol. Int. 2012;6:735–743. doi: 10.1007/s12072-012-9344-9. [DOI] [PubMed] [Google Scholar]
- 64.Zhang X., Liu L., Zhang M., Gao S., Du Y., An Y., Chen S. The efficacy and safety of entecavir in patients with chronic hepatitis B-associated liver failure: A meta-analysis. Ann. Hepatol. 2015;14:150–160. [PubMed] [Google Scholar]
- 65.Yu S., Jianqin H., Wei W., Jianrong H., Yida Y., Jifang S., Liang Y., Zhi C., Hongyu J. The efficacy and safety of ucleos(t)ide analogues in the treatment of HBV-related acute-on-chronic liver failure: A meta-analysis. Ann. Hepatol. 2013;12:364–372. [PubMed] [Google Scholar]
- 66.Lange C.M., Bojunga J., Hofmann W.P., Wunder K., Mihm U., Zeuzem S., Sarrazin C. Severe lactic acidosis during treatment of chronic hepatitis B with entecavir in patients with impaired liver function. Hepatology. 2009;50:2001–2006. doi: 10.1002/hep.23346. [DOI] [PubMed] [Google Scholar]
- 67.Marzano A., Marengo A., Marietti M., Rizzetto M. Lactic acidosis during Entecavir treatment in decompensated hepatitis B virus-related cirrhosis. Dig. Liver Dis. 2011;43:1027–1028. doi: 10.1016/j.dld.2011.06.013. [DOI] [PubMed] [Google Scholar]
- 68.Shouval D. The pros and cons of lamivudine vs. entecavir in decompensated or severe acute exacerbation of chronic hepatitis B) J. Hepatol. 2014;60:1108–1109. doi: 10.1016/j.jhep.2014.03.004. [DOI] [PubMed] [Google Scholar]
- 69.Garg H., Sarin S.K., Kumar M., Garg V., Sharma B.C., Kumar A. Tenofovir improves the outcome in patients with spontaneous reactivation of hepatitis B presenting as acute-on-chronic liver failure. Hepatology. 2011;53:774–780. doi: 10.1002/hep.24109. [DOI] [PubMed] [Google Scholar]
- 70.Cui Y.L., Yan F., Wang Y.B., Song X.Q., Liu L., Lei X.Z., Zheng M.H., Tang H., Feng P. Nucleoside analogue can improve the long-term prognosis of patients with hepatitis B virus infection-associated acute on chronic liver failure. Dig. Dis. Sci. 2010;55:2373–2380. doi: 10.1007/s10620-010-1257-7. [DOI] [PubMed] [Google Scholar]
- 71.Lai J., Yan Y., Mai L., Zheng Y.B., Gan W.Q., Ke W.M. Short-term entecavir vs. lamivudine therapy for HBeAg-negative patients with acute-on-chronic hepatitis B liver failure. Hepatobiliary Pancreat. Dis. Int. 2013;12:154–159. doi: 10.1016/S1499-3872(13)60025-9. [DOI] [PubMed] [Google Scholar]
- 72.Liu C., Ye J., Jia H., Zhang M., Han H., Chen F., Chen C. Entecavir and lamivudine therapy for severe acute chronic hepatitis B. Exp. Ther. Med. 2013;5:545–548. doi: 10.3892/etm.2012.850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Zhang Y., Hu X.Y., Zhong S., Yang F., Zhou T.Y., Chen G., Wang Y.Y., Luo J.X. Entecavir vs. lamivudine therapy for naïve patients with spontaneous reactivation of hepatitis B presenting as acute-on-chronic liver failure. World J. Gastroenterol. 2014;28:4745–4752. doi: 10.3748/wjg.v20.i16.4745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Chen C.H., Lin C.L., Hu T.H., Hung C.H., Tseng P.L., Wang J.H., Chang J.Y., Lu S.N., Chien R.N., Lee C.M. Entecavir vs. lamivudine in chronic hepatitis B patients with severe acute exacerbation and hepatic decompensation. J. Hepatol. 2014;60:1127–1134. doi: 10.1016/j.jhep.2014.02.013. [DOI] [PubMed] [Google Scholar]
- 75.Wong V.W., Wong G.L., Yiu K.K., Chim A.M., Chu S.H., Chan H.Y., Sung J.J., Chan H.L. Entecavir treatment in patients with severe acute exacerbation of chronic hepatitis B. J. Hepatol. 2011;54:236–242. doi: 10.1016/j.jhep.2010.06.043. [DOI] [PubMed] [Google Scholar]
- 76.Tsai W.L., Chiang P.H., Chan H.H., Lin H.S., Lai K.H., Cheng J.S., Chen W.C., Tsay F.W., Yu H.C., Hsu P.I. Early entecavir treatment for chronic hepatitis B with severe acute exacerbation. Antimicrob. Agents Chemother. 2014;58:1918–1921. doi: 10.1128/AAC.02400-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ye X.G., Su Q.M. Effects of entecavir and lamivudine for hepatitis, B decompensated cirrhosis: Meta-analysis. World J. Gastroenterol. 2013;19:6665–6678. doi: 10.3748/wjg.v19.i39.6665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Liaw Y.F. Management of YMDD mutations during lamivudine therapy in patients with chronic hepatitis B. J. Gastroenterol. Hepatol. 2002;17:S333–S337. doi: 10.1046/j.1440-1746.17.s3.23.x. [DOI] [PubMed] [Google Scholar]
- 79.Liaw Y.F. The current management of HBV drug resistance. J. Clin. Virol. 2005;34:S143–S146. doi: 10.1016/S1386-6532(05)80025-3. [DOI] [PubMed] [Google Scholar]
- 80.Wong V.W., Wong G.L., Tsang S.W., Hui A.Y., Chim A.M., Yiu K.K., Chan H.Y., Chan F.K., Sung J.J., Chan H.L. Long-term follow-up of lamivudine treatment in patients with severe acute exacerbation of hepatitis B e antigen (HBeAg)-positive chronic hepatitis B. Antivir. Ther. 2008;13:571–579. [PubMed] [Google Scholar]
- 81.Lok A.S., McMahon B.J. Chronic hepatitis B: Update 2009. Hepatology. 2009;50:661–662. doi: 10.1002/hep.23190. [DOI] [PubMed] [Google Scholar]
- 82.European Association For The Study Of The Liver EASL clinical practice guidelines: Management of chronic hepatitis B virus infection. J. Hepatol. 2012;57:167–185. doi: 10.1016/j.jhep.2012.02.010. [DOI] [PubMed] [Google Scholar]
- 83.Hung C.H., Hu T.H., Lu S.N., Lee C.M., Chen C.H., Kee K.M., Wang J.H., Tsai M.C., Kuo Y.H., Chang K.C., et al. Tenofovir vs. Entecavir in treatment of chronic hepatitis B virus with severe acute exacerbation. Antimicrob. Agents Chemother. 2015;59:3168–3173. doi: 10.1128/AAC.00261-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Lai C.L., Dienstag J., Schiff E., Leung N.W., Atkins M., Hunt C., Brown N., Woessner M., Boehme R., Condreay L. Prevalence and clinical correlates of YMDD variants during lamivudine therapy for patients with chronic hepatitis B. Clin. Infect. Dis. 2003;36:687–696. doi: 10.1086/368083. [DOI] [PubMed] [Google Scholar]
- 85.Lok A.S., Lai C.L., Leung N., Yao G.B., Cui Z.Y., Schiff E.R., Dienstag J.L., Heathcote E.J., Little N.R., Griffiths D.A., et al. Long-term safety of lamivudine treatment in patients with chronic hepatitis B. Gastroenterology. 2003;125:1714–1722. doi: 10.1053/j.gastro.2003.09.033. [DOI] [PubMed] [Google Scholar]
- 86.Allen M.I., Deslauriers M., Andrews C.W., Tipples G.A., Walters K.A., Tyrrell D.L., Brown N., Condreay L.D. Identification and characterization of mutations in hepatitis B virus resistant to lamivudine. Hepatology. 1998;27:1670–1677. doi: 10.1002/hep.510270628. [DOI] [PubMed] [Google Scholar]
- 87.Stuyver L.J., Locarnini S.A., Lok A., Richman D.D., Carman W.F., Disentag J.L., Schinazi R.F. Nomenclature for antiviral-resistant human hepatitis B virus mutations in the polymerase region. Hepatology. 2001;33:751–757. doi: 10.1053/jhep.2001.22166. [DOI] [PubMed] [Google Scholar]
- 88.Akuta N., Tsubota A., Suzuki F., Suzuki Y., Hosaka T., Someya T., Kobayashi M., Saitoh S., Arase Y., Ikeda K., et al. Long-term prognosis by lamivudine monotherapy for severe acute exacerbation in chronic hepatitis B infection: Emergence of YMDD motif mutant and risk of breakthrough hepatitis—An open-cohort study. J. Hepatol. 2003;38:91–97. doi: 10.1016/S0168-8278(02)00335-5. [DOI] [PubMed] [Google Scholar]
- 89.Zhang J.M., Yao X., Wang Y.X., Liu F., Ma Z.M., Weng X.H., Wen Y.M. High replicative full-length lamivudine-resistant hepatitis B virus isolated during acute exacerbations. J. Med. Virol. 2005;77:203–208. doi: 10.1002/jmv.20453. [DOI] [PubMed] [Google Scholar]
- 90.Tenney D.J., Levine S.M., Rose R.E., Walsh A.W., Weinheimer S.P., Discotto L., Plym M., Pokornowski K., Yu C.F., Angus P., et al. Clinical emergence of entecavir resistant hepatitis B virus requires additional substitutions in virus already resistant to Lamivudine. Antimicrob. Agents Chemother. 2004;48:3498–3507. doi: 10.1128/AAC.48.9.3498-3507.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Sheldon J., Camino N., Rodes B., Bartholomeusz A., Kuiper M., Tacke F., Núñez M., Mauss S., Lutz T., Klausen G., et al. Selection of hepatitis B virus polymerase mutations in HIV-coinfected patients treated with tenofovir. Antivir. Ther. 2005;10:727–734. [PubMed] [Google Scholar]
- 92.Fung J., Lai C.L., Seto W.K., Yuen M.F. Nucleoside/nucleotide analogues in the treatment of chronic hepatitis B. J. Antimicrob. Chemother. 2011;66:2715–2725. doi: 10.1093/jac/dkr388. [DOI] [PubMed] [Google Scholar]
- 93.Yeh C.T. Development of HBV S gene mutants in chronic hepatitis B patients receiving nucleotide/nucleoside analogue therapy. Antivir. Ther. 2010;15:471–475. doi: 10.3851/IMP1552. [DOI] [PubMed] [Google Scholar]
- 94.Delaney W., 4th, Yang H., Westland C.E., Das K., Arnold E., Gibbs C.S., Miller M.D., Xiong S. The hepatitis B virus polymerase mutation rtV173L is selected during lamivudine therapy and enhances viral replication in vitro. J. Virol. 2003;77:11833–11841. doi: 10.1128/JVI.77.21.11833-11841.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Torresi J., Earnest-Silveira L., Civitico G., Walters T.E., Lewin S.R., Fyfe J., Locarnini S.A., Manns M., Trautwein C., Bock T.C. Restoration of replication phenotype of lamivudine-resistant hepatitis B virus mutants by compensatory changes in the “fingers” subdomain of the viral polymerase selected as a consequence of mutations in the overlapping S gene. Virology. 2002;299:88–99. doi: 10.1006/viro.2002.1448. [DOI] [PubMed] [Google Scholar]
- 96.Villet S., Pichoud C., Villeneuve J.P., Trépo C., Zoulim F. Selection of a multiple drug-resistant hepatitis B virus strain in a liver-transplanted patient. Gastroenterology. 2006;131:1253–1261. doi: 10.1053/j.gastro.2006.08.013. [DOI] [PubMed] [Google Scholar]
- 97.Hsu C., Yeh C., Chang M.L., Liaw Y.F. Identification of a hepatitis B virus S gene mutant in lamivudine-treated patients experiencing HBsAg seroclearance. Gastroenterology. 2007;132:543–550. doi: 10.1053/j.gastro.2006.12.001. [DOI] [PubMed] [Google Scholar]
- 98.Yeh C.T., Chien R.N., Chu C.M., Liaw Y.F. Clearance of the original hepatitis B virus YMDD-motif mutants with emergence of distinct lamivudine-resistant mutants during prolonged lamivudine therapy. Hepatology. 2000;31:1318–1326. doi: 10.1053/jhep.2000.7296. [DOI] [PubMed] [Google Scholar]
- 99.Sheldon J., Soriano V. Hepatitis B virus escape mutants induced by antiviral therapy. J. Antimicrob. Chemother. 2008;61:766–768. doi: 10.1093/jac/dkn014. [DOI] [PubMed] [Google Scholar]
- 100.Sloan R.D., Ijaz S., Moore P.L., Harrison T.J., Teo C.G., Tedder R.S. Antiviral resistance mutations potentiate hepatitis B virus immune evasion through disruption of its surface antigen a determinant. Antivir. Ther. 2008;13:439–447. [PubMed] [Google Scholar]
- 101.Bock C.T., Tillmann H.L., Torresi J., Klempnauer J., Locarnini S., Manns M.P., Trautwein C. Selection of hepatitis B virus polymerase mutants with enhanced replication by lamivudine treatment after liver transplantation. Gastroenterology. 2002;122:264–273. doi: 10.1053/gast.2002.31015. [DOI] [PubMed] [Google Scholar]
- 102.Dai C.Y., Chuang W.L., Hou N.J., Lee L.P., Hsieh M.Y., Lin Z.Y., Chen S.C., Huang J.F., Hsieh M.Y., Wang L.Y., et al. Early mortality in Taiwanese lamivudine-treated patients with chronic hepatitis B-related decompensation: Evaluation of the model for end-stage liver disease and index scoring systems as prognostic predictors. Clin. Ther. 2006;28:2081–2092. doi: 10.1016/j.clinthera.2006.12.016. [DOI] [PubMed] [Google Scholar]
- 103.Yan Y., Mai L., Zheng Y.B., Zhang S.Q., Xu W.X., Gao Z.L., Ke W.M. What MELD score mandates use of entecavir for ACLF-HBV BeAg-negative patients? World J. Gastroenterol. 2012;18:4604–4609. doi: 10.3748/wjg.v18.i33.4604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Wu F.L., Shi K.Q., Chen Y.P., Braddock M., Zou H., Zheng M.H. Scoring systems predict the prognosis of acute-on-chronic hepatitis B liver failure: An evidence-based review. Expert Rev. Gastroenterol. Hepatol. 2014;8:623–632. doi: 10.1586/17474124.2014.906899. [DOI] [PubMed] [Google Scholar]
- 105.He W.P., Hu J.H., Zhao J., Tong J.J., Ding J.B., Lin F., Wang H.F. Comparison of four prognostic models and a new Logistic regression model to predict short-term prognosis of acute-on-chronic hepatitis B liver failure. Chin. Med. J. Engl. 2012;125:2272–2278. [PubMed] [Google Scholar]
- 106.Sarin S.K., Kedarisetty C.K., Abbas Z., Amarapurkar D., Bihari C., Chan A.C., APASL ACLF Working Party Acute-on-chronic liver failure: Consensus recommendations of the Asian Pacific Association for the Study of the Liver (APASL) 2014. Hepatol. Int. 2014;8:453–471. doi: 10.1007/s12072-014-9580-2. [DOI] [PubMed] [Google Scholar]
- 107.Hsu Y.C., Wu C.Y., Chang C.Y., Tai C.M., Tseng C.H., Perng D.S., Mo L.R., Lin J.T. Pretreatment viral DNA stratifies mortality risk in patients receiving antiviral therapy for severe acute exacerbation of chronic hepatitis B. Antivir. Ther. 2013;18:221–228. doi: 10.3851/IMP2435. [DOI] [PubMed] [Google Scholar]