Abstract
Objective
High achievement in school has been associated with increased risk of eating disorders, including anorexia nervosa (AN) and bulimia nervosa (BN), but causality of these relationships is unclear. We sought to examine the association between school achievement and AN or BN in a national cohort and to determine the possible contribution of familial confounding using a co-relative design.
Method
The national cohort study involved 1,800,643 persons born in Sweden during 1972-1990 who were still living in Sweden at age 16 years, followed up for AN and BN identified from inpatient and outpatient diagnoses through 2012. We used Cox regression to examine the association between school achievement and subsequent risk of AN or BN, and stratified Cox models to examine the gradient in this association across different strata of co-relative pairs (first cousins, half siblings, full siblings).
Results
School achievement was positively associated with risk of AN among females and males (hazard ratio per additional 1 standard deviation, females: 1.29; 95% CI, 1.25-1.33; males: 1.29; 95% CI, 1.10-1.52), and risk of BN among females but not males (females: 1.16; 95% CI, 1.11-1.20; males: 1.05; 95% CI, 0.84-1.31). In co-relative analyses, as the degree of shared genetic and environmental factors increased (e.g., from first-cousin to full-sibling pairs), the association between school achievement and AN or BN substantially decreased.
Conclusion
In this large national cohort study, high achievement in school was associated with increased risk of AN and BN, but this appeared to be explained by unmeasured familial (genetic and environmental) factors.
Keywords: achievement, anorexia nervosa, bulimia nervosa, eating disorders, schools
Introduction
Eating disorders are an important cause of morbidity and mortality in adolescents and young adults, especially among women.1-3 The lifetime prevalence of anorexia nervosa (AN) and bulimia nervosa (BN) in women has been reported to be up to 4% and 3%, respectively.4-6 Both AN and BN have a high risk of premature mortality even when specialized treatment is available.7,8 Young adults with AN or BN are reported to have more than a 6-fold and nearly 3-fold all-cause mortality, respectively, relative to healthy controls.7
Eating disorders are reported to be more common among individuals with high intelligence,9 perfectionism,10 high grades in school,11 or higher achievement in school than would be predicted by intelligence.12 However, causality of associations between school achievement and eating disorders is unclear. Previous studies have examined factors commonly associated with school achievement, such as parental education or socioeconomic status (SES), with conflicting results. Some11,13-16 but not all17-19 have reported associations between high parental education or SES and increased risk of eating disorders. A recent Swedish cohort study of 250,000 youth reported that high parental education was associated with eating disorders among females but not males.13 However, a Korean study reported that the association between SES and risk of eating disorders among girls was U-shaped, with increased risk among those with either lowest or highest SES.20
Confounding by familial factors potentially may explain the association between school achievement and eating disorders. To our knowledge, no studies have used family-based designs to examine the potential contribution of unmeasured familial factors. We conducted a national cohort study in Sweden to: (1) examine the association between school achievement and subsequent risk of AN or BN in a national cohort of 1.8 million native-borne Swedes, and (2) use a co-relative design to examine the gradient in this association across different strata of co-relative pairs (e.g., first cousins, half siblings, full siblings) to determine whether observed associations, if any, are explained by unmeasured shared familial (genetic or environmental) factors.
Method
Study Population and Data Sources
We identified 1,861,934 persons who were born in Sweden from 1972 to 1990 and were still living in Sweden at age 16 years. Of this total, 1,800,643 (96.7%) were registered in the National School Register and were included in this study. This study was approved by the Regional Ethical Review Board of Lund University in Sweden.
We linked data from multiple Swedish national registries using an anonymous version of the unique individual 10-digit personal ID number assigned at birth or immigration to all Swedish residents. Our database was created from the following sources: the Multi-Generation Register, providing information on family relationships; Swedish Hospital Discharge Register, containing all discharge diagnoses for Swedish inhabitants during 1964-2012; Swedish Outpatient Registry, containing all outpatient diagnoses nationwide during 2001-2012; Population and Housing Census, providing information on educational status for the biological parents in every fifth year between 1960 and 1985; and the National School Register, containing the school grade score (similar to a grade point average) for all students at the end of grade nine (usually age 16 years) during 1988-2012.
Exposure and Outcome Ascertainment
The school grade score was recorded on a scale from 1 (lowest) to 5 (overall mean was 3.2) during 1988-1997, and on a scale from 10 (lowest) to 320 (overall mean was 207) from 1998 onwards. For each year and by gender, we standardized the grade score into a Z-score with mean 0 and SD 1. This standardized variable, which we refer to as school achievement (SA), was our exposure of interest.
The study outcomes were AN and BN, which were identified using International Classification of Diseases (ICD) codes in the Swedish Hospital Discharge and Outpatient Registries, and were examined separately. AN was identified by ICD-9 code 307B and ICD-10 codes F50.0-F50.1 (DSM-IV/V code 307.1), and BN by ICD-9 code 307F and ICD-10 codes F50.2-F50.3 (DSM-IV/V code 307.51).
Education level among biological parents was examined as a potential confounder and was measured as the mean of the highest education level achieved by both parents. It was categorized into five groups (<9, 9, 10-11, 12, >12 years) and modeled as an ordinal variable. Individuals with missing data for one parent were assigned the education level of the other parent, and those with missing data for both parents (n=13,929) were assigned the lowest education level (or alternatively, exclusion of these individuals in a secondary analysis did not affect the results).
Statistical Analyses
Because our aim was to assess causality, we sought to ensure that our exposure of interest (SA) preceded our study outcomes (AN and BN). Therefore, in our main analyses, we removed prevalent (pre-existing) cases of AN or BN by excluding diagnoses that were made prior to registration of SA. This resulted in exclusion of 1,249/6,122 (20.4%) AN cases and 793/4,054 (19.6%) BN cases among females, and 110/311 (35.4%) AN cases and 577/648 (89.0%) BN cases among males. We also performed secondary analyses in which all prevalent cases were included.
We used Cox proportional hazards regression to compute hazard ratios (HRs) and 95% CIs for the association between SA and risk of AN or BN. Robust standard errors were used to adjust the 95% CIs for correlation within families. The Cox model time scale was follow-up time from SA registration until the first diagnosis of AN or BN, emigration, death, or the end of follow-up (December 31, 2012), whichever occurred first. In all models, we investigated the proportional hazards assumption by including an interaction term between SA and the natural logarithm of time.
In a second analysis, we compared results from the entire population with those from a co-relative design. Using the Swedish Multi-Generation Register, we identified all first-cousin, half-sibling, and full-sibling pairs. We performed stratified Cox regression analyses for all first-cousin, half-sibling, and full-sibling pairs that did not have the same SA score, and extrapolated analyses for monozygotic (MZ) twins, with a separate stratum for each relative pair. The co-relative design allows a comparison of rates of AN or BN in relatives with different levels of SA. The stratified Cox models compute HRs that are adjusted for the familial cluster, and therefore account for shared genetic and environmental factors. MZ twins, full siblings, half siblings, and first cousins share, respectively, 100%, 50%, 25%, and 12.5% of their genes identical by descent. We constructed a final model that includes all four types of relative relationships, in which the HR for each relative type is dependent on the degree of genetic resemblance. The logarithm of the HRs was assumed to be a linear function of the proportion of genes shared and the outcome of interest. This model can yield a more robust estimate of the association between SA and eating disorders among MZ twins, for whom data are sparse (e.g., the number of discordant pairs for AN and BN was 0 and 1, respectively, among MZ twin males, and 22 and 14, respectively, among MZ twin females). All statistical analyses were performed using SAS 9.3.
Results
In this cohort of 1,800,643 native-born Swedes, subsequent diagnosis of AN or BN was much more common among females (0.56% and 0.37%, respectively) than males (0.02% and 0.01%, respectively) (Table 1). Incidence rates (per 10,000 person-years) for AN were 3.93 in females and 0.15 in males, and for BN were 2.59 in females and 0.05 in males. The mean age at diagnosis was 20.7 years for AN and 23.5 years for BN, and was similar for females and males. Standardized across sexes, individuals who subsequently were diagnosed with AN or BN had SA scores that were 0.3 and 0.1 SDs higher, respectively, than the overall mean SA. The associations between SA and AN or BN are illustrated in more detail in Figures 1 and 2. Especially among females, higher SA was associated with an increased risk of AN and BN.
Table 1. Descriptive Statistics for Population Born in Sweden From 1972 to 1990 and Registered for School Achievement.
| Females (n=878,365) | Males (n=922,278) | |||
|---|---|---|---|---|
|
| ||||
| AN | BN | AN | BN | |
| Cumulative prevalencea, % | 0.56 | 0.37 | 0.02 | 0.01 |
| Person-years | 12,375,125 | 12,600,612 | 13,362,872 | 13,360,740 |
| Incidence rateb | 3.93 | 2.59 | 0.15 | 0.05 |
| Mean age at diagnosis (SD) | 20.8 (4.6) | 23.6 (4.8) | 20.6 (4.2) | 23.4 (5.4) |
| Mean school achievement (SD)c | 0.26 (1.0) | 0.16 (1.0) | 0.26 (1.0) | 0.07 (0.9) |
Note: AN = anorexia nervosa, BN = bulimia nervosa.
Number of cases divided by number of individuals included in the study.
Cases per 10,000 person-years.
Grade score standardized by year and gender into Z-score with population mean 0 and SD 1.
Figure 1.

Anorexia prevalence (y axis: females, blue line, and males, red line) by school achievement (x axis). Note: dashed lines represent the upper 95% confidence limit; dotted lines represent the lower 95% confidence limit. Std = standard deviation.
Figure 2.
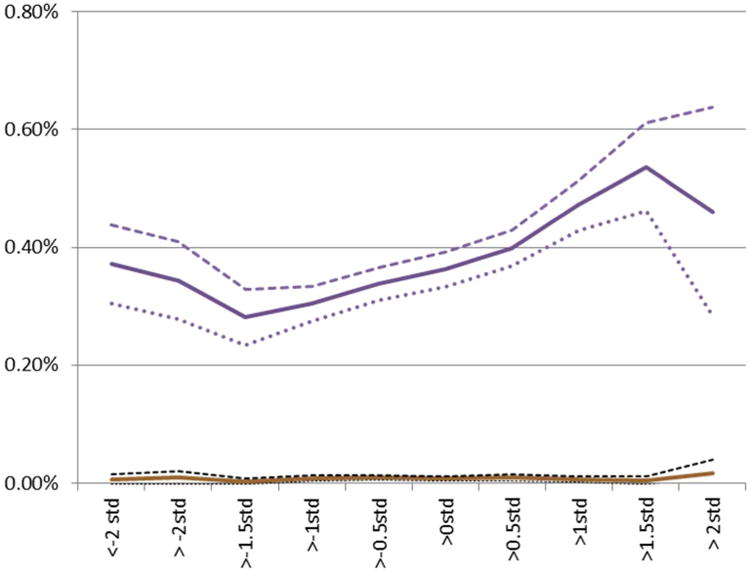
Bulimia prevalence (y axis: females, blue line, and males, red line) by school achievement (x axis). Note: dashed lines represent the upper 95% confidence limit; dotted lines represent the lower 95% confidence limit. Std = standard deviation.
The first gender-stratified Cox model included only SA as a predictor variable (Table 2, Model A). The association between SA and AN was similar between sexes (HR 1.29 for both), indicating that each additional 1 SD of SA was associated with a 29% increased risk of AN. Model B was additionally adjusted for parental education. In females (but not males), high parental education was associated with an increased risk of AN, and the HR for association between SA and AN was substantially attenuated (HR 1.19). In Model C, year of birth was positively associated with risk of AN (i.e., higher risk among later births), but adjustment for it had no effect on the association between SA and AN. Finally, we tested the proportional hazards assumption that the HR for the association between SA and AN was constant over time (Model D). This test suggested that the effect of SA was slightly stronger closer to the graduation year and waned over time, especially among males.
Table 2. Hazard Ratios (HR) and 95% CIs for Association Between School Achievement (SA; Modeled as a Continuous Z-score) and Risk of Anorexia Nervosa.
| Females | Males | ||
|---|---|---|---|
|
| |||
| HR (95% CI) | HR (95% CI) | ||
| Model A | Z-score (SA) | 1.29 (1.25, 1.33) | 1.29 (1.10, 1.52) |
| Model B | Z-score (SA) | 1.19 (1.14, 1.23) | 1.32 (1.11, 1.58) |
| Parental education | 1.18 (1.15, 1.21) | 1.04 (0.91, 1.20) | |
| Model C | Z-score (SA) | 1.19 (1.14, 1.24) | 1.34 (1.11, 1.61) |
| Parental education | 1.17 (1.14, 1.20) | 1.03 (0.89, 1.19) | |
| Year of birth | 1.10 (1.10, 1.11) | 1.11 (1.07, 1.14) | |
| Model D | Z-score (SA) | 1.29 (1.23, 1.36) | 1.58 (1.23, 2.03) |
| Parental education | 1.16 (1.14, 1.20) | 1.02 (0.89, 1.18) | |
| Year of birth | 1.10 (1.10, 1.11) | 1.11 (1.07, 1.14) | |
| Log(time) * Z-score | 0.92 (0.90, 0.95) | 0.84 (0.73, 0.96) | |
SA was associated with a modestly increased risk of BN among females (HR 1.16; Table 3, Model A). There were few BN cases among males (n=71), resulting in wide confidence intervals. As a result, we did not perform further analyses of BN among males. In Model B, high parental education was associated with an increased risk of BN among females, and adjustment for parental education resulted in attenuation of the association between SA and BN (HR 1.08). In Model C, year of birth was positively associated with risk of BN, but adjustment for it had no effect on the association between SA and BN. Finally, a test of the proportional hazards assumption indicated that the HR for association between SA and BN was constant over time.
Table 3. Hazard Ratios (HR) and 95% CIs for Association Between School Achievement (SA; Modeled as a Continuous Z-score) and Risk of Bulimia Nervosa.
| Females | Males | ||
|---|---|---|---|
|
| |||
| HR (95% CI) | HR (95% CI) | ||
| Model A | Z-score (SA) | 1.16 (1.11, 1.20) | 1.05 (0.84, 1.31) |
| Model B | Z-score (SA) | 1.08 (1.03, 1.12) | -- |
| Parental education | 1.14 (1.11, 1.18) | -- | |
| Model C | Z-score (SA) | 1.08 (1.04, 1.13) | -- |
| Parental education | 1.13 (1.10, 1.17) | -- | |
| Year of birth | 1.09 (1.08, 1.10) | -- | |
We performed co-relative analyses to assess the possible contribution of unmeasured familial confounding to the associations between SA and AN or BN. As the degree of shared genetic and environmental factors increased (e.g., from first-cousin to full-sibling pairs), the association between SA and AN in males decreased (HR among full siblings = 1.18) (Figure 3). Among MZ twin pairs, the extrapolated HR was very close to 1, suggesting complete familial confounding of the association between SA and AN in males. Among females, the association between SA and AN followed the same pattern (Figure 4). As the degree of shared genetic and environmental factors increased, the HR decreased toward unity, also suggesting complete familial confounding. Note that among females, the HRs did not decrease in the first-cousin or half-sibling analyses (in which we control for 12.5% and 25%, respectively, of their genes which are identical by descent, and a relatively small degree of shared environment), whereas in the analysis of full siblings (in which we control for 50% of shared genes and a large degree of shared environment), the HR decreased to unity. This may suggest that genetic factors play a less important role than shared environment in the association between SA and AN among females. A similar pattern was seen for the association between SA and BN among females (see Figure S1, available online), with the HR decreasing toward unity as the degree of shared genetic and environmental factors increased, suggesting complete familial confounding.
Figure 3.
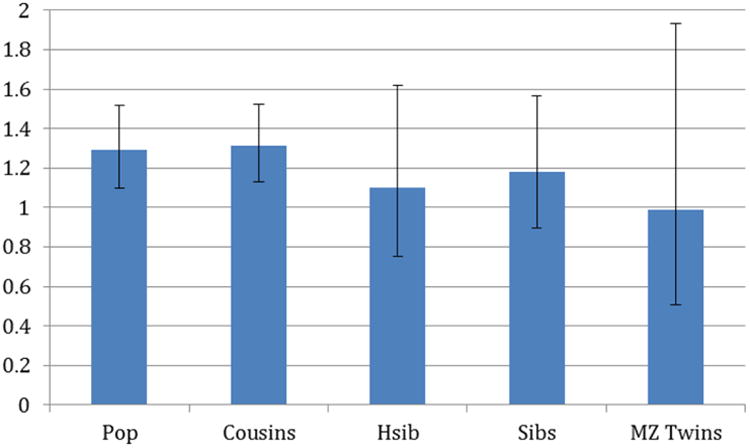
Hazard ratios and 95% CIs for association between school achievement and anorexia in males in the general population (Pop), first cousins, half siblings (Hsib), full siblings, and monozygotic (MZ) twins.
Figure 4.
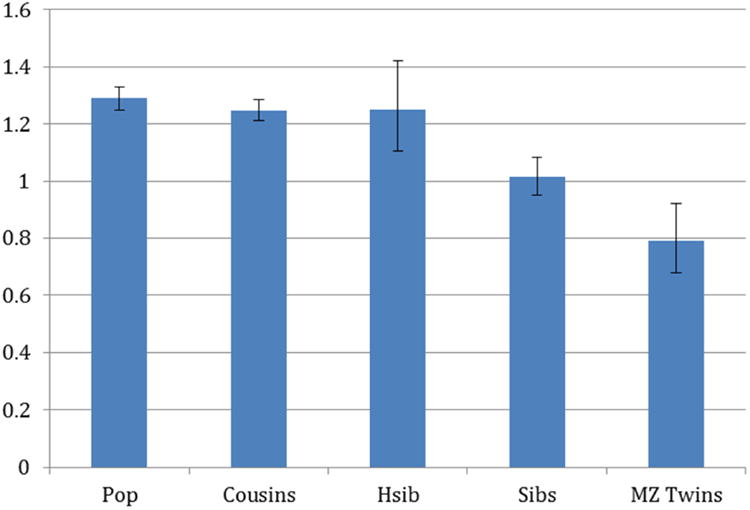
Hazard ratios and 95% CIs for association between school achievement and anorexia in females in the general population (Pop), first cousins, half siblings (Hsib), full siblings, and monozygotic (MZ) twins.
Secondary Analyses
In secondary analyses that included prevalent (pre-existing) cases, the prevalence of AN was increased to 0.70% for females and 0.03% for males, and the prevalence of BN was increased to 0.46% for females and 0.07% for males. The mean age at AN diagnosis decreased to 19.4 (SD 5.0) for females and 18.0 (SD 4.9) for males, and the mean age at BN diagnosis decreased to 19.5 (SD 10.0) for females and 3.6 (SD 7.6) for males (based on only 648 cases among males). In co-relative analyses, as the degree of shared genetic and environmental factors increased, risk estimates were substantially attenuated toward unity for all outcomes except AN among males, for which the risk estimate remained modestly elevated. However, this finding should be interpreted cautiously considering that the exposure (SA) may not have preceded the outcome (AN), and hence the basic criteria for causality may not be met. Overall, these secondary analyses suggested that exclusion of prevalent cases in our main analyses had no substantial effect on our overall findings.
Discussion
To our knowledge, this national cohort study is the largest to date to examine the association between school achievement and eating disorders, and the first to use a co-relative design to assess causality of this association. We found that high achievement in school was associated with an increased risk of AN and BN among females, and AN among males. However, using co-relative analyses, we found that these associations appear to be non-causal and are explained entirely by unmeasured familial confounders. As the degree of shared genetic and environmental factors increased (e.g., from first-cousin to full-sibling pairs), the association between school achievement and AN or BN decreased substantially and was absent in extrapolated risk estimates for monozygotic twin pairs, suggesting complete familial confounding.
We also found that high parental education, which has both genetic and environmental determinants, was associated with a modestly increased risk of AN and BN among females but not males. This is consistent with a smaller Swedish study that reported an association between high parental education and eating disorders among females but not males,13 whereas another Swedish study reported a modest association with AN among males.15 The present study suggests that parental education only partly explains the observed associations between school achievement and eating disorders among females. Other unmeasured familial factors may contribute to this association, such as familial values, role modeling, or personality traits. Some evidence has suggested that perfectionistic character traits may be important factors underlying both higher school achievement as well as disordered eating behaviors aimed at achieving the “ideal” weight. Perfectionism has been reported to be a precursor to AN and other eating disorders,10,21,22 to persist after long-term recovery from AN,23 and to be more common in relatives of women with eating disorders.24 Perfectionism also may explain why persons with eating disorders, on average, have higher achievement in school. AN, for example, has been associated not only with higher IQ,9 but with higher school performance than would be predicted by IQ.12 The association between school performance and eating disorders may be caused by perfectionism acting in different behavioral domains, including both school and eating behaviors. The underlying mechanisms by which perfectionism may lead to eating disorders are not well-established but may involve maladaptive attempts to attain social status or rank, for which body weight is perceived as a quantifiable marker.25
A Swedish twin study estimated that the genetic heritability of narrowly defined AN is 56%, with the remaining variance attributable to shared environment (5%) and unique environment (38%).26 A similar level of genetic heritability (50-60%) has been estimated for BN.6,27 However, confidence intervals for these estimates were wide due to the rarity of these conditions, and the estimated genetic heritability of broadly defined AN was lower (31%).26 Pooled twin studies to augment statistical power would be useful for estimating heritability more precisely for these conditions. In our co-relative analyses, we found that the association between school achievement and AN among females was attenuated very little among cousins or half siblings compared with the association in the general population, whereas it was much more attenuated among full siblings. This pattern suggests the possibility that shared environment may make a relatively larger contribution to this association than genetic factors.
The present study had certain limitations. It was based solely on medical records and therefore included only individuals who presented for treatment. As a result, the identified cases were not entirely representative of the eating disorder population, many of whom choose not to seek or receive treatment. On the other hand, among those who seek treatment, differential access by socioeconomic status is less of a problem in Sweden than in other countries such as the US because of the Swedish universal health care system. In addition, although we provide evidence that the link between school achievement and eating disorders is non-causal, we lacked data on other psychosocial characteristics that may plausibly explain this association. School achievement is likely to encompass many underlying factors such as perfectionism, obsessionality, familial values, and role modeling, which we were unable to assess directly.
This study also has several important strengths. It is the largest and most comprehensive study to date of school performance and subsequent development of eating disorders. It is the first to use a co-relative design to assess for confounding by unmeasured familial factors, by comparing the association between school performance and eating disorders among co-relative pairs with varying levels of shared genetic and environmental factors. The use of nationwide outpatient and inpatient diagnoses allowed more complete ascertainment of eating disorders than in many previous studies. Prospective ascertainment of the exposure and outcomes for nearly all Swedish-born adolescents and young adults prevented selection or self-reporting biases that potentially compromise survey-based studies. We also had highly complete data on parental education which enabled us to examine its influence on the link between school achievement and eating disorders.
In summary, this large national cohort study found that high achievement in school is associated with an increased risk of eating disorders in adolescence and young adulthood. However, using a co-relative design, we found that this relationship appears to be non-causal and is explained by shared familial (genetic and/or environmental) factors.
Supplementary Material
Figure S1. Hazard ratios and 95% CIs for association between school achievement and bulimia in females in the general population (Pop), first cousins, half siblings (Hsib), full siblings, and monozygotic (MZ) twins.
Acknowledgments
This work was supported by grants from the National Institute of Drug Abuse at the National Institutes of Health (R01 DA030005); the Swedish Research Council; and ALF project grant, Region Skåne/Lund University, Sweden. The funding agencies had no role in the design and conduct of the study; in the collection, analysis, and interpretation of the data; or in the preparation, review, or approval of the manuscript.
Dr. Ohlsson served as the statistical expert for this research.
Footnotes
This article is discussed in an editorial by Dr. Daniel Le Grange on page xx.
Supplemental material cited in this article is available online.
Disclosure: Drs. J. Sundquist, Ohlsson, Winkleby, K. Sundquist, and Crump report no biomedical financial interests or potential conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Dr. Jan Sundquist, Lund University, Center for Primary Health Care Research, Malmö, Sweden.
Dr. Henrik Ohlsson, Lund University, Center for Primary Health Care Research, Malmö, Sweden.
Dr. Marilyn A. Winkleby, Stanford University, Stanford Prevention Research Center, Stanford, CA.
Dr. Kristina Sundquist, Lund University, Center for Primary Health Care Research, Malmö, Sweden.
Dr. Casey Crump, Stanford University.
References
- 1.Mitchell JE, Crow S. Medical complications of anorexia nervosa and bulimia nervosa. Curr Opin Psychiatry. 2006;19:438–43. doi: 10.1097/01.yco.0000228768.79097.3e. [DOI] [PubMed] [Google Scholar]
- 2.Arcelus J, Mitchell AJ, Wales J, Nielsen S. Mortality rates in patients with anorexia nervosa and other eating disorders. A meta-analysis of 36 studies. Arch Gen Psychiatry. 2011;68:724–31. doi: 10.1001/archgenpsychiatry.2011.74. [DOI] [PubMed] [Google Scholar]
- 3.Klump KL, Bulik CM, Kaye WH, Treasure J, Tyson E. Academy for eating disorders position paper: eating disorders are serious mental illnesses. Int J Eat Disord. 2009;42:97–103. doi: 10.1002/eat.20589. [DOI] [PubMed] [Google Scholar]
- 4.Smink FR, van Hoeken D, Hoek HW. Epidemiology, course, and outcome of eating disorders. Curr Opin Psychiatry. 2013;26:543–548. doi: 10.1097/YCO.0b013e328365a24f. [DOI] [PubMed] [Google Scholar]
- 5.Swanson SA, Crow SJ, Le Grange D, Swendsen J, Merikangas KR. Prevalence and correlates of eating disorders in adolescents. Results from the national comorbidity survey replication adolescent supplement. Arch Gen Psychiatry. 2011;68:714–23. doi: 10.1001/archgenpsychiatry.2011.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kendler KS, MacLean C, Neale M, Kessler R, Heath A, Eaves L. The genetic epidemiology of bulimia nervosa. Am J Psychiatry. 1991;148:1627–37. doi: 10.1176/ajp.148.12.1627. [DOI] [PubMed] [Google Scholar]
- 7.Suokas JT, Suvisaari JM, Gissler M, et al. Mortality in eating disorders: a follow-up study of adult eating disorder patients treated in tertiary care, 1995-2010. Psychiatry Res. 2013;210:1101–6. doi: 10.1016/j.psychres.2013.07.042. [DOI] [PubMed] [Google Scholar]
- 8.Crow SJ, Peterson CB, Swanson SA, et al. Increased mortality in bulimia nervosa and other eating disorders. American J Psychiatry. 2009;166:1342–6. doi: 10.1176/appi.ajp.2009.09020247. [DOI] [PubMed] [Google Scholar]
- 9.Lopez C, Stahl D, Tchanturia K. Estimated intelligence quotient in anorexia nervosa: a systematic review and meta-analysis of the literature. Ann Gen Psychiatry. 2010;9:40. doi: 10.1186/1744-859X-9-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Forbush K, Heatherton TF, Keel PK. Relationships between perfectionism and specific disordered eating behaviors. Int J Eat Disord. 2007;40:37–41. doi: 10.1002/eat.20310. [DOI] [PubMed] [Google Scholar]
- 11.Ahren-Moonga J, Silverwood R, Klinteberg BA, Koupil I. Association of higher parental and grandparental education and higher school grades with risk of hospitalization for eating disorders in females: the Uppsala birth cohort multigenerational study. Am J Epidemiol. 2009;170:566–75. doi: 10.1093/aje/kwp166. [DOI] [PubMed] [Google Scholar]
- 12.Dura JR, Bornstein RA. Differences between IQ and school achievement in anorexia nervosa. J Clin Psychol. 1989;45:433–5. doi: 10.1002/1097-4679(198905)45:3<433::aid-jclp2270450313>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 13.Ahren JC, Chiesa F, Koupil I, Magnusson C, Dalman C, Goodman A. We are family--parents, siblings, and eating disorders in a prospective total-population study of 250,000 Swedish males and females. Int J Eat Disord. 2013;46:693–700. doi: 10.1002/eat.22146. [DOI] [PubMed] [Google Scholar]
- 14.Ahren JC, Chiesa F, Af Klinteberg B, Koupil I. Psychosocial determinants and family background in anorexia nervosa--results from the Stockholm Birth Cohort Study. Int J Eat Disord. 2012;45:362–9. doi: 10.1002/eat.20953. [DOI] [PubMed] [Google Scholar]
- 15.Goodman A, Heshmati A, Koupil I. Family history of education predicts eating disorders across multiple generations among 2 million Swedish males and females. PloS one. 2014;9:e106475. doi: 10.1371/journal.pone.0106475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lindberg L, Hjern A. Risk factors for anorexia nervosa: a national cohort study. Int J Eat Disord. 2003;34:397–408. doi: 10.1002/eat.10221. [DOI] [PubMed] [Google Scholar]
- 17.Rastam M, Gillberg C, Garton M. Anorexia nervosa in a Swedish urban region. A population-based study. British J Psychiatry. 1989;155:642–6. doi: 10.1192/s0007125000018134. [DOI] [PubMed] [Google Scholar]
- 18.Rastam M, Gillberg C. The family background in anorexia nervosa: a population-based study. J Am Acad Child Adolesc Psychiatry. 1991;30:283–9. doi: 10.1097/00004583-199103000-00018. [DOI] [PubMed] [Google Scholar]
- 19.Gard MC, Freeman CP. The dismantling of a myth: a review of eating disorders and socioeconomic status. Int J Eat Disord. 1996;20:1–12. doi: 10.1002/(SICI)1098-108X(199607)20:1<1::AID-EAT1>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- 20.Lee HJ, Park S, Kim CI, et al. The association between disturbed eating behavior and socioeconomic status: the Online Korean Adolescent Panel Survey (OnKAPS) PloS one. 2013;8:e57880. doi: 10.1371/journal.pone.0057880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fairburn CG, Cooper Z, Doll HA, Welch SL. Risk factors for anorexia nervosa: three integrated case-control comparisons. Arch Gen Psychiatry. 1999;56:468–76. doi: 10.1001/archpsyc.56.5.468. [DOI] [PubMed] [Google Scholar]
- 22.Halmi KA, Sunday SR, Strober M, et al. Perfectionism in anorexia nervosa: variation by clinical subtype, obsessionality, and pathological eating behavior. Am J Psychiatry. 2000;157:1799–1805. doi: 10.1176/appi.ajp.157.11.1799. [DOI] [PubMed] [Google Scholar]
- 23.Lilenfeld LR, Stein D, Bulik CM, et al. Personality traits among currently eating disordered, recovered and never ill first-degree female relatives of bulimic and control women. Psychol Med. 2000;30:1399–1410. doi: 10.1017/s0033291799002792. [DOI] [PubMed] [Google Scholar]
- 24.Woodside DB, Bulik CM, Halmi KA, et al. Personality, perfectionism, and attitudes toward eating in parents of individuals with eating disorders. Int J Eat Disord. 2002;31:290–9. doi: 10.1002/eat.10032. [DOI] [PubMed] [Google Scholar]
- 25.Bardone-Cone AM, Wonderlich SA, Frost RO, et al. Perfectionism and eating disorders: current status and future directions. Clin Psychol Rev. 2007;27:384–405. doi: 10.1016/j.cpr.2006.12.005. [DOI] [PubMed] [Google Scholar]
- 26.Bulik CM, Sullivan PF, Tozzi F, Furberg H, Lichtenstein P, Pedersen NL. Prevalence, heritability, and prospective risk factors for anorexia nervosa. Arch Gen Psychiatry. 2006;63:305–12. doi: 10.1001/archpsyc.63.3.305. [DOI] [PubMed] [Google Scholar]
- 27.Bulik CM, Thornton LM, Root TL, Pisetsky EM, Lichtenstein P, Pedersen NL. Understanding the relation between anorexia nervosa and bulimia nervosa in a Swedish national twin sample. Biol Psychiatry. 2010;67:71–7. doi: 10.1016/j.biopsych.2009.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Hazard ratios and 95% CIs for association between school achievement and bulimia in females in the general population (Pop), first cousins, half siblings (Hsib), full siblings, and monozygotic (MZ) twins.


