Abstract
Introduction
The goal of this project was to use the Consolidated Framework for Implementation Research (CFIR) as the theoretical foundation for developing a web-based clinical decision support system (CDSS) for primary care screening and care coordination by dental hygienists at chairside.
Methods
First, we appraised New York State education and scope of practice requirements for dental hygienists with input from health experts who constituted a Senior Advisory Board for the project, and reviewed current professional guidelines and best practices for tobacco use, hypertension and diabetes screening, and nutrition counseling at chairside. Second, we created algorithms for these four health issues (tobacco, hypertension, diabetes, and nutrition) using evidence-based guidelines endorsed by authoritative professional bodies. Third, an information technology specialist incorporated the algorithms into a tool using an iterative process to refine the CDSS, with input from dental hygienists, dentists, Senior Advisory Board members and research staff.
Results
An evidence-based CDSS for use by dental hygienists at chairside for tobacco use, hypertension and diabetes screening, and nutrition counseling was developed with the active participation of the individuals involved in the implementation process.
Conclusions
CDSS technology may potentially be leveraged to enhance primary care screening and coordination by dental hygienists at chairside, leading to improved patient care. Using the CFIR as a pragmatic structure for implementing this intervention across multiple settings, the developed CDSS is available for downloading and adaptation to diverse dental settings and other primary care sensitive conditions.
Keywords: dental hygienist, primary care, clinical decision support system, implementation science, health screening, care coordination
Graphical Abstract
Introduction
A considerable body of evidence has long existed concerning the links between general and oral health.1 The landmark 2007 guidance document, Report of the Independent Panel of Experts of The Scottsdale Project underscored the significance of oral health in promoting whole body health, and the importance of medical-dental collaboration in improving patient outcomes.2 Since tobacco use is a leading cause of oral pathology,3 there is compelling cause to involve dental providers in evidence-based cessation services. More than three decades ago, McCarthy made a plea for measurement of blood pressure at the initial physical evaluation of the adult dental patient, along with pulse, temperature, respiration, height, and weight.4 Strauss and colleagues have been pivotal in demonstrating that gingival crevicular blood collected at chairside can be used to screen for diabetes and monitor glycemic control during dental visits.5 Finally, in light of the demonstrated relationship between sugar-sweetened beverage (SSB) intake and caries risk, Marshall has argued that all dental practices should assess patients’ SSB intake and tailor dietary recommendations accordingly.6
The 2009 Health Information Technology for Economic and Clinical Health (HITECH) Act provides financial incentives for use of certified electronic health records (EHRs) by eligible providers, including dentists.7 This may potentially spur better coordination of patient care by the medical and dental professions, but evidence-based tools are needed to abet this desired outcome. We conducted formative research to explore dental hygienists’ and dentists’ perspectives regarding the integration of primary care activities into routine dental care, and assess the needs of dental hygienists and dentists regarding primary care coordination activities and use of information technology to obtain clinical information at chairside.8 Findings were that dental hygienists are well positioned to facilitate greater integration of oral and general health care, but that challenges exist, including the lack of evidence-based knowledge, coordination with dentists, and systems-level support.8
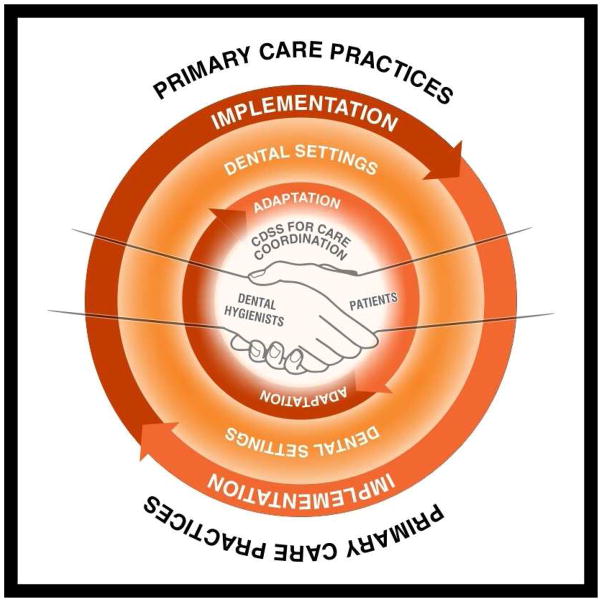
Using the Consolidated Framework for Implementation Research (CFIR) as our theoretical foundation,9 we built upon this formative research to approach the development of a web-based clinical decision support system (CDSS) for primary care screening and care coordination by dental hygienists at chairside (see Figure 1).
Figure 1. The five major domains of the Consolidated Framework of Implementation Research (CFIR), displayed for the current study.
In this conceptual framework, the intervention is a clinical decision support system (CDSS) for primary care screening and care coordination at chairside that may be adapted for a variety of dental settings. Dental hygienists and their patients are the primary individuals involved, and successful implementation of this intervention may improve care coordination between dental settings and primary care practices, leading to improved patient care. Adapted from Northridge et al.8 and Damschroder et al.9
In essence, a web-based CDSS is an information technology-based system designed to provide expert support to improve clinical decision-making.10,11 For this project, the intervention is a CDSS designed specifically for dental hygienists to aid in primary care screening and coordination at chairside. That is, the CDSS is intended to combine the tenets of evidence-based medicine and dentistry, provider knowledge, existing research, and patient values and preferences into a tool to aid dental hygienists in selecting the appropriate course of action for each patient.12 Evidence-based clinical decision support tools have been previously used in dentistry not only to facilitate clinical decision-making around gingival recession, root exposure, caries, dental sealants, decay prevention, and topical fluoride guides, but also to enhance transfer of knowledge to patients at the point of care.13
In a systematic review of trials to identify CDSS features critical to their success, four features were identified as independent predictors of improved clinical practice: automatic provision of decision support as part of clinician workflow, provision of recommendations rather than just assessments, provision of decision support at the time and location of decision-making, and computer-based decision support.14 In addition to incorporating these features into our approach, we also worked closely with dental hygienists at every stage of the research process, to ensure that the developed CDSS would meet both their standards for clinical dental hygiene practice15 and workflow preferences.
Methods
Overview
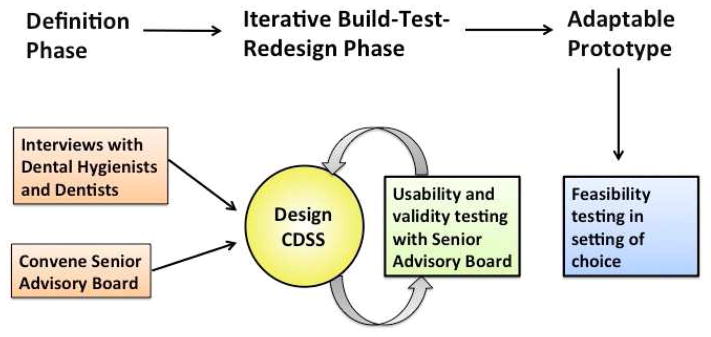
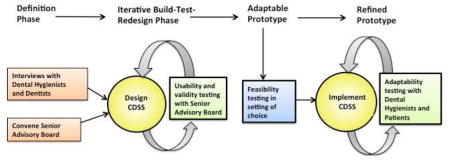
The sequence of developing the CDSS for use by dental hygienists at chairside is illustrated in Figure 2.
Figure 2. Sequence of developing the electronic clinical decision support system (CDSS) for primary care screening and coordination by dental hygienists at chairside.
The three-phase development process includes a definition phase, an iterative build-test-redesign phase, and a clinical testing phase with an adaptable prototype that remains to be conducted. Based upon Wyatt and Spiegelhalter.16
Toward ensuring the CDSS might be rigorously evaluated, used in clinical practice, and improve patient care, we elected to follow the recommendation to evaluate the CDSS in two stages: laboratory and field testing.16 In the former, the perspectives of both prospective users (dental hygienists) and experts (medical, dental, and information technology) responsible for implementation are valuable.16 In the definition phase, we relied on interviews with dental hygienists and dentists8 and members of our Senior Advisory Board to guide the design of the CDSS. In the following iterative build-test-redesign phase led by an information technology expert, intensive input was incorporated from dental hygienists, especially, but also dentists, Senior Advisory Board members and research staff.
The field testing stage of the CDSS remains to be completed. This will involve designing a study to test, in an unbiased manner, whether the CDSS is used in clinical practice, and if it is used, how it affects the structure, process and outcome of dental care encounters.16 It will also involve creating an interface between the CDSS and electronic health record (EHR) systems used in clinical practice.
CDSS development
The overall goal of this study was to develop a CDSS for dental hygienists to guide primary care screening and care coordination at chairside, beginning with New York University College of Dentistry practice settings. Hence, it was important to ensure that current New York State education and scope of practice requirements for dental hygienists were followed.15,17 Based upon a public health understanding of prevention as the cornerstone of overall health and well-being, we elected to focus on tobacco use, hypertension and diabetes screening, and nutrition counseling. Dental hygienists are involved in all of these content areas, as they: counsel and coordinate tobacco cessation programs; take and record blood pressure; screen for systemic diseases and conditions, including diabetes; and educate patients on the importance of good nutrition for maintaining optimal oral health.15
In addition to soliciting the expert opinions of and adapting the CDSS resources developed by our Senior Advisory Board members,18–20 we appraised the existing medical and dental literature and consulted our dental hygiene colleagues to create dental hygiene specific evidence-based algorithms and language for the CDSS based upon best practices at the New York University College of Dentistry. Built into the CDSS is evidence-based guidance for the interpretation of the results for each patient, and suggested language to use in discussing the results and any needed referrals with the patient. The core of the authoritative guidance for each of the four content areas is provided next.
Tobacco
The tobacco use algorithm is based upon the US Public Health Service guide titled, Treating Tobacco Use and Dependence Clinical Practice Guideline,21 which was previously adapted for use in dental care settings.18 The major revision from the algorithm for dentists which uses the Ask, Advise, Assess, Assist, Arrange model is that the algorithm for dental hygienists uses the Ask, Advise, Refer model.22 Specifically, dental hygienists are guided to ask patients about tobacco use, advise patients to quit, and refer patients to the the New York State Smokers’ Quitline,23 as indicated.
Hypertension
The hypertension screening algorithm is based upon the Eighth Joint National Committee (JNC 8) recommendations for diagnosing and managing hypertension.24 The blood pressure categories for normal, prehypertension, stage 1 hypertension, and stage 2 hypertension remain unchanged from the earlier JNC 7 recommendations, which stressed that all health care providers, including dentists and members of the dental team, need to be involved in detection and management of this important public health problem.25 The major change from JNC 7 to JNC 8 is age-specific guidance, namely, there is strong evidence to support treating hypertensive persons aged 60 years or older to a blood pressure goal of less than 150/90 mm Hg and hypertensive persons aged 30–59 years to a diastolic goal of less than 90 mm Hg.24 The critical role of the dental hygienist is to measure and record every patient’s systolic and diastolic blood pressure at chairside before any dental procedure, and repeat these measurements in five minutes after obtaining any high reading. Decisions regarding next steps, e.g., avoid elective dental care and refer patient to the New York University Nursing Faculty Practice if there is no medical home, are then discussed with the patient.
Diabetes
The diabetes screening algorithm is based upon the Standards of Care recommendations developed by the American Diabetes Association.26 In essence, patients who are overweight or obese and all patients older than age 45 years who have not been tested for diabetes should be referred to a primary care provider. Moreover, oral symptoms of diabetes ought to be noted by dental hygienists upon examination. Specifically, periodontal changes are the first clinical manifestation of diabetes, and patients with long-standing, poorly controlled diabetes are at risk of developing oral candidiasis.27
Nutrition
The nutrition counseling algorithm is based upon the Diet Assessment of Caries Risk tool developed at the University of Iowa toward assisting oral health care professionals to efficiently assess dietary contributors to caries risk.6 A multidisciplinary group of faculty devised a Nutrition Caries Risk Assessment algorithm based upon this tool that is now in place at the New York University College of Dentistry (available upon request from the authors). The Academy of Nutrition and Dietetics supports the integration of oral health with nutrition services, education, and research, and recommends collaboration between dietetics practitioners and oral care professionals.28 The emphasis in the nutrition counseling algorithm developed for dental hygienists for use with their patients is that they link the development of carious lesions to the consumption of sugar sweetened beverages and snacks.
CDSS programming
The CDSS tool was programmed as a web application using a variety of open source technologies, toward ensuring that the tool was available on as many devices as possible, e.g., smart phones, tablet computers, chairside terminals. Dental hygienists are thus able to access the tool using whatever electronic devices are on-hand at chairside in various dental settings, such as dental clinics and offices.
From a technological standpoint, the CDSS is comprised of a combination of HTML, CSS and JavaScript to handle front-end interaction and PHP to power the back-end scripting which enables the algorithmic guidance provided through the application. The CDSS runs in a LAMP environment (Linux, Apache, MySQL and PHP) hosted by New York University.
The software development methodology used to create the application was an iterative process with aspects of agile development, including frequent version releases and close interaction with the research team and their expert consultants over a period of six months. The CDSS may be adapted to encompass a variety of dental setting workflows and expanded to assess other primary care conditions, such as asking about and recording patient receipt of recommended immunizations by age group.
Results and Discussion
Structured multi-step algorithms were created to provide decision support to dental hygienists at the time and location of decision-making.14 Care was taken to ensure that the algorithms were consistent with current New York State education and scope of practice requirements for dental hygienists15,17 and that they provided recommendations rather than just assessments.14
Once the algorithms were initially created, they were refined and improved upon by engaged dental hygienists, dentists, Senior Advisory Board members and research staff, and then modified in the web-based application by the dental informatics programmer (see Figure 2). The algorithms provide step-by-step guidance for dental hygienists for use in interacting with each patient, and prompt dental hygienists toward different evidence-based decisions depending on the answers provided by their patients and the clinical assessments they conduct and record. At this stage, the developed CDSS includes algorithms for tobacco use, hypertension and diabetes screening, and nutrition counseling.
While these algorithms were created using evidence-based guidelines endorsed by authoritative professional bodies, they were adapted to incorporate dental hygiene best practices and clinical workflow at the New York University College of Dentistry. Thus, dental hygienists are prompted to refer patients who currently use tobacco to the New York State Smokers’ Quitline23 and patients who do not currently have a primary care provider to the New York University Nursing Faculty Practice. Beyond recording important primary care information and prompting dental hygienists to initiate recommended referrals, the CDSS also provides language to assist dental hygienists in communicating essential health information to their patients (see the Appendix for screen shots of the suggested language for dental hygienists to use in communicating recommendations to patients).
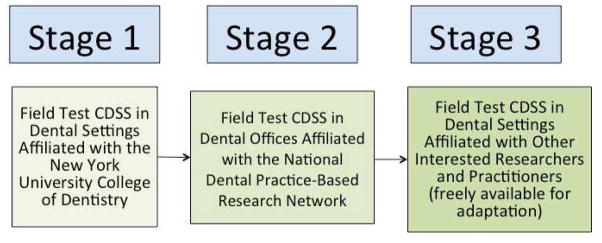
An adaptable prototype of the developed CDSS is available at http://www.nyu.edu/dental/ctsi/. We are currently collaborating with our dental hygiene, dental, medical, and information technology partners to feasibility test this CDSS in a variety of dental settings, and writing proposals to obtain funding for a rigorous evaluation of its impact on the structure, process and outcomes of dental care encounters.16 A staged approach is envisioned. First, we plan to work with dental settings affiliated with the New York University College of Dentistry, to include dental clinics and faculty practices. Second, we hope to collaborate with the National Dental Practice-Based Research Network at the University of Alabama at Birmingham School of Dentistry to conduct implementation studies in a variety of private dental practices. Finally, since the CDSS is available for downloading free of charge to readers of this journal, we are enthusiastic about engaging with other dental researchers and practitioners to adapt this tool to their own dental settings (see Figure 7).
Figure 7. Staged approach to the field testing.
The various stages envisioned to implement and evaluate the adaptable electronic clinical decision support system in diverse dental settings.
In moving forward, we are mindful of the obstacles we may well face in implementing this evidence-based tool, including the need to close the gap between academics and dental practitioners.29 Thus, we will use the theory and methods of implementation science to guide us each step of the way.9
Conclusions
A CDSS for primary care screening and care coordination by dental hygienists at chairside holds the potential to spur better coordination of patient care by the medical and dental professions. Because the setting where dental hygienists work is critical in influencing provider adherence to evidence-based guidelines,30 we plan to collaborate closely with our dental and medical colleagues to rigorously evaluate this tool in a variety of dental settings and share our findings in an ongoing way with the broader community of dental and medical practitioners.
Supplementary Material
Figure 3. Developed algorithm for counseling for tobacco use by dental hygienists at chairside.
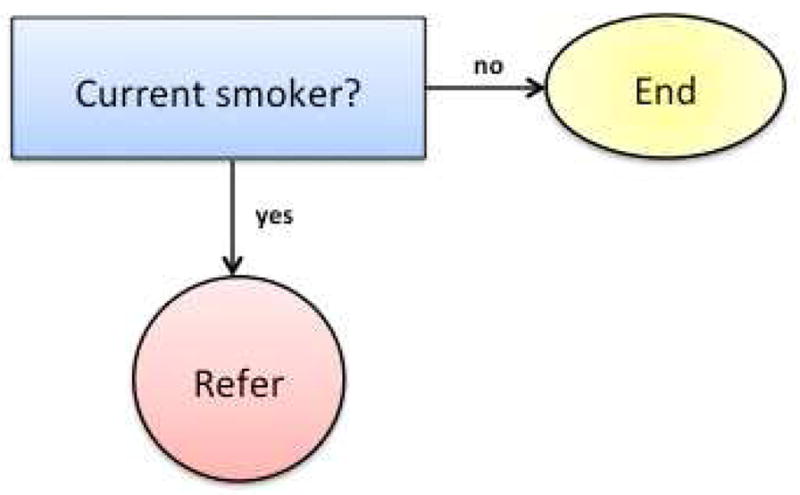
The tobacco use algorithm is based upon the US Public Health Service guide titled, Treating Tobacco Use and Dependence Clinical Practice Guideline,21 and adapted for dental hygienists using the Ask, Advise, Refer model.22
Figure 4. Developed algorithm for hypertension screening by dental hygienists at chairside.
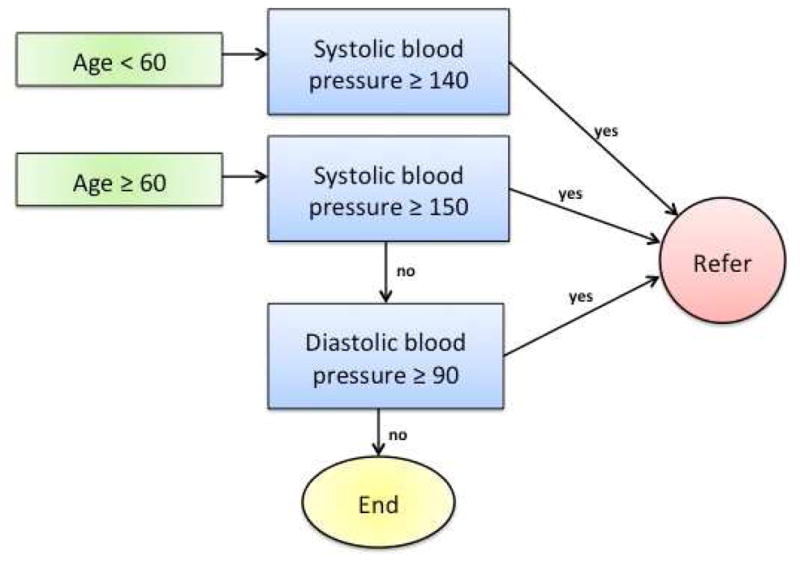
The hypertension screening algorithm is based upon the Eighth Joint National Committee (JNC 8) recommendations for diagnosing and managing hypertension,24 and adapted for dental hygienists to include referral to a primary care provider.
Figure 5. Developed algorithm for diabetes screening by dental hygienists at chairside.
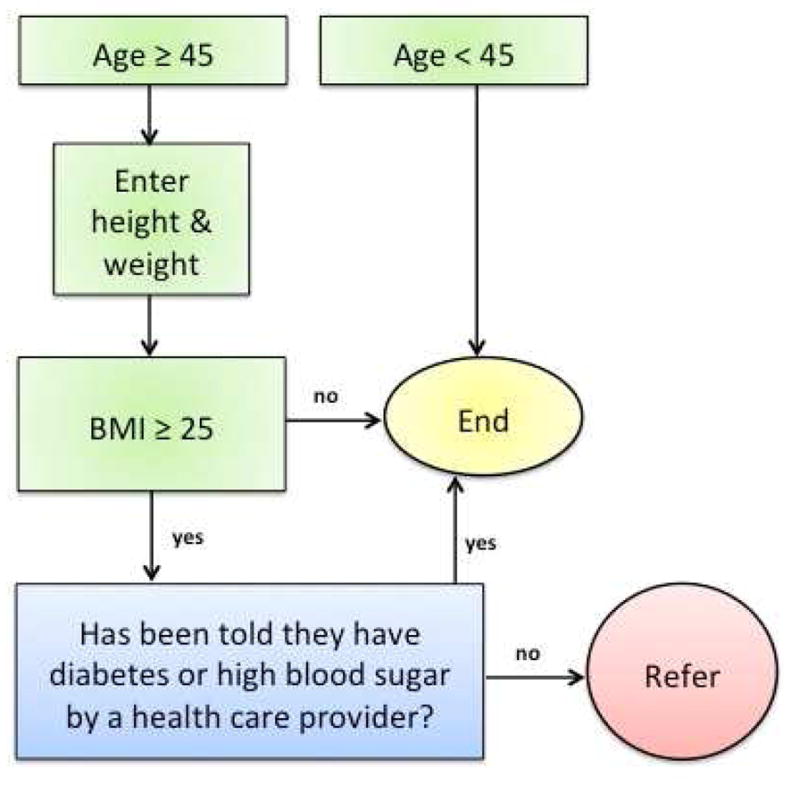
The diabetes screening algorithm is based upon the Standards of Care recommendations developed by the American Diabetes Association,26 and adapted for dental hygienists to include referral to a primary care provider.
Figure 6. Developed algorithm for sugar sweetened food and beverages intake and caries risk for use by dental hygienists at chairside.
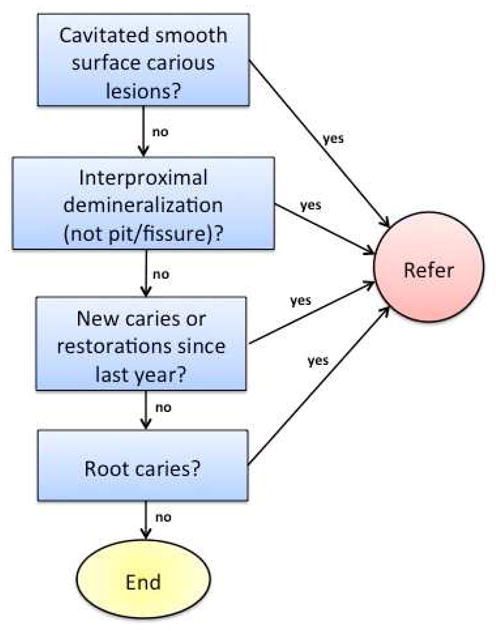
The nutrition counseling algorithm is based upon the Diet Assessment of Caries Risk tool developed at the University of Iowa toward assisting oral health care professionals to efficiently assess dietary contributors to caries risk,6 notably sugar sweetened food and beverages.
Acknowledgments
The authors would like to thank the members of our Senior Advisory Board and dental colleagues who do not appear as co-authors on this paper for their generosity in sharing their professional insights and evidence-based resources with us, especially: Michael Glick, DMD, Emilie Godfrey, MS, RD, Sheila M. Strauss, PhD, and Miriam R. Robbins, DDS, MS. We are encouraged by the dedication of the following dental hygiene faculty at the New York University College of Dentistry who do not appear as co-authors yet supported us in ensuring that this tool is in keeping with best dental hygiene practices: Judith Kreismann, RDH, BS, MA and Cheryl E. Westphal Thiele, RDH, EdD. The authors were supported in the research, analysis, and writing of this paper by the National Center for Advancing Translational Sciences of the US National Institutes of Health for the project titled, Primary Care Screening by Dental Hygienists at Chairside: Developing and Evaluating an Electronic Tool (grant UL1TR000038) and by the National Institute for Dental and Craniofacial Research and the Office of Behavioral and Social Sciences Research of the US National Institutes of Health for the project titled, Integrating Social and Systems Science Approaches to Promote Oral Health Equity (grant R01-DE023072).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Stefanie L. Russell, Email: stefanie.russell@nyu.edu.
Ariel Port Greenblatt, Email: ap140@nyu.edu.
Danni Gomes, Email: dmg9@nyu.edu.
Shirley Birenz, Email: ssb254@nyu.edu.
Cynthia A. Golembeski, Email: cgolembeski@fortunesociety.org.
Donna Shelley, Email: donna.shelley@nyumc.org.
Matthew McGuirk, Email: matt.mcguirk@yale.edu.
Elise Eisenberg, Email: elise.eisenberg@nyu.edu.
Mary E. Northridge, Email: men6@nyu.edu.
References
- 1.Oral health in America: a report of the surgeon general. Rockville, MD: US Department of Health and Human Services, National Institute of Dental and Craniofacial Research; 2000. [Google Scholar]
- 2.Hein C, Cobb C, Iacopino A. [Accessed May 25, 2015];Report of the independent panel of experts of the Scottsdale Project. 2007 Available at: http://downloads.pennnet.com/pnet/gr/scottsdaleproject.pdf.
- 3.Fiore M. Treating tobacco use and dependence: 2008 update. Rockville, MD: US Department of Health and Human Services, Public Health Service; 2008. Tobacco Use and Dependence Guideline Panel. [Google Scholar]
- 4.McCarthy FM. Vital signs--the six-minute warnings. J Am Dent Assoc. 1980;100(5):682–691. doi: 10.14219/jada.archive.1980.0210. [DOI] [PubMed] [Google Scholar]
- 5.Strauss SM, Rosedale MT, Pesce MA, Rindskopf DM, Kaur N, Juterbock CM, Wolff MS, Malaspina D, Danoff A. The potential for glycemic control monitoring and screening for diabetes at dental visits. Am J Public Health. 2015;105(4):796–801. doi: 10.2105/AJPH.2014.302357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marshall TA. Chairside diet assessment of caries risk. J Am Dent Assoc. 2009;140:670–674. doi: 10.14219/jada.archive.2009.0252. [DOI] [PubMed] [Google Scholar]
- 7.Kalenderian E, Walji M, Ramoni RB. “Meaningful use” of HER in dental school clinics: how to benefit from the U.S. HITECH Act’s financial and quality improvement incentives. J Dent Educ. 2013;77(4):401–415. [PubMed] [Google Scholar]
- 8.Northridge ME, Birenz S, Gomes G, Golembeski CA, Greenblatt AP, Shelley D, Russell SL. Views of dental providers on primary care coordination at chairside. J Dent Hyg. in review. [PMC free article] [PubMed] [Google Scholar]
- 9.Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4:50. doi: 10.1186/1748-5908-4-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Haynes RB, Wilczynski NL Computerized Clinical Decision Support System (CCDSS) Systematic Review Team. Effects of computerized clinical decision support systems on practitioner performance and patient outcomes: methods of a decision-maker-researcher partnership systematic review. Implement Sci. 2010;5:12. doi: 10.1186/1748-5908-5-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mendonca EA. Clinical decision support systems: perspectives in dentistry. J Dent Educ. 2004;68:589–597. [PubMed] [Google Scholar]
- 12.Brignardello-Petersen R, Carrasco-Labra A, Glick M, Guyatt GH, Azarpazhooh A. A practical approach to evidence-based dentistry: understanding and applying the principles of EBD. J Am Dent Assoc. 2014;145:1105–1107. doi: 10.14219/jada.2014.102. [DOI] [PubMed] [Google Scholar]
- 13.Merijohn GK, Bader JD, Frantsve-Hawley J, Aravamudhan K. Clinical decision support chairside tools for evidence-based dental practice. J Evid Base Dent Pract. 2008;8:119–132. doi: 10.1016/j.jebdp.2008.05.016. [DOI] [PubMed] [Google Scholar]
- 14.Kawamoto K, Houlihan CA, Balas EA, Lobach DF. Improving clinical practice using clinical decision support systems: a systematic review of trials to identify features critical to success. BMJ. 2005;330:765. doi: 10.1136/bmj.38398.500764.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.American Dental Hygienists’ Association (ADHA) Standards for Clinical Dental Hygiene Practice. Chicago, IL: ADHA; 2008. [Google Scholar]
- 16.Wyatt J, Spiegelhalter D. Evaluating medical expert systems: what to test and how? Med Inform. 1990;15:205–217. doi: 10.3109/14639239009025268. [DOI] [PubMed] [Google Scholar]
- 17.New York State Education Department (NYSED). Office of the Professions. Dental Professions. [Accessed June 12, 2015];Regulations of the Commissioner. Available at: http://www.op.nysed.gov/prof/dent/part61.htm.
- 18.Montini T, Schenkel AB, Shelley DR. Feasibility of a computerized clinical decision support system for treating tobacco use in dental clinics. J Dent Educ. 2013;77:458–462. [PubMed] [Google Scholar]
- 19.Glick M. Medical Support System. [Accessed June 12, 2015];ICE Health Systems in partnership with ADEC, LLC. 2012 Available at: http://icemedicalsupport.com/
- 20.Shelley D, Tseng TY, Matthews AG, Wu D, Ferrari P, Cohen A, Millery M, Ogedegbe O, Farrell L, Kopal H. Technology-driven intervention to improve hypertension outcomes in community health centers. Am J Manag Care. 2011;17(12 Spec No):SP103–110. [PubMed] [Google Scholar]
- 21.Fiore M. Treating tobacco use and dependence: 2008 update. Rockville, MD: US Department of Health and Human Services, Public Health Service; 2008. Tobacco Use and Dependence Guideline Panel. [Google Scholar]
- 22.New York University Manhattan Tobacco Cessation Program. [Accessed June 12, 2015];Treating Tobacco Use and Dependence: A Toolkit for Providers. Available at: http://www.med.nyu.edu/sites/default/files/pophealth/MTCPdentaltoolkit.pdf.
- 23.New York State Department of Health Tobacco Control Program. [Accessed June 12, 2015];New York State Smokers’ Quitline. Available at: http://www.nysmokefree.com/
- 24.James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8) JAMA. 2014;311:507–520. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- 25.Herman WW, Konzelman JL, Jr, Prisant LM Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. New national guidelines on hypertension: a summary for dentistry. J Am Dent Assoc. 2004;135:576–584. doi: 10.14219/jada.archive.2004.0244. quiz 653–574. [DOI] [PubMed] [Google Scholar]
- 26.American Diabetes Association. Standards of medical care in diabetes--2014. Diabetes Care. 2014;37(Suppl 1):S14–80. doi: 10.2337/dc14-S014. [DOI] [PubMed] [Google Scholar]
- 27.Lamster IB, Lalla E, Borgnakke WS, Taylor GW. The relationship between oral health and diabetes mellitus. J Am Dent Assoc. 2008;139(Suppl):19S–24S. doi: 10.14219/jada.archive.2008.0363. [DOI] [PubMed] [Google Scholar]
- 28.Touger-Decker R, Mobley C Academy of Nutrition and Dietetics. Position of the Academy of Nutrition and Dietetics: oral health and nutrition. J Acad Nutr Diet. 2013;113:693–701. doi: 10.1016/j.jand.2013.03.001. [DOI] [PubMed] [Google Scholar]
- 29.Hannes K, Norre D, Goedhuys J, Naert I, Aertgeerts B. Obstacles to implementing evidence-based dentistry: a focus group-based study. J Dent Educ. 2008;72:736–744. [PubMed] [Google Scholar]
- 30.Hung DY, Leidig R, Shelley DR. What’s in a setting? Influence of organizational culture on provider adherence to clinical guidelines for treating tobacco use. Health Care Manage Rev. 2014;39:154–163. doi: 10.1097/HMR.0b013e3182914d11. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.