Abstract
Context:
Hamstring acute muscle injuries are prevalent in several sports including AFL football (Australian Football League), sprinting and soccer, and are often associated with prolonged time away from sport.
Evidence Acquisition:
In response to this, research into prevention and management of hamstring injury has increased, but epidemiological data shows no decline in injury and re-injury rates, suggesting that rehabilitation programs and return to play (RTP) criteria have to be improved. There continues to be a lack of consensus regarding how to assess performance, recovery and readiness to RTP, following hamstring strain injury.
Results:
The aim of this paper was to propose rehabilitation protocol for hamstring muscle injuries based on current basic science and research knowledge regarding injury demographics and management options.
Conclusions:
Criteria-based (subjective and objective) progression through the rehabilitation program will be outlined along with exercises for each phase, from initial injury to RTP.
Keywords: Muscles, Wounds and Injuries, Rehabilitation, Skeletal
1. Context
Muscle injuries are among the most prevalent time-loss sports injuries and most are caused by over-strain or contusion (1). The thigh is the most common muscle site injured in soccer (2) and several other sports (3-6). Hamstring muscle injuries (HMIs) are the most prevalent muscle injury in soccer (2), Australian football (5), American football (4), and track and field (6). In soccer, a player suffers on average 0.6 muscle injuries per season, 92% located in lower limbs and 37% affecting hamstrings with a mean absence of 14.3 ± 14.9 days and a re-injury rate of 16% which causes a longer absence (2). In this study, HMIs refer to indirect over-strain; as direct hamstring muscle contusions are rare.
There is developing research into hamstrings injuries, investigating injury rates, risk factors, as well as prevention and rehabilitation programs (7, 8). Despite this research focus, hamstring injury and re-injury rates remain high in many sports (2, 8-11). A potential reason for high recurrence rates is failure of rehabilitation programs and poorly defined return to play (RTP) criteria (12).
Most recent rehabilitation protocols for HMIs incorporate goals to achieve in each phase, objective and subjective criteria to progress between phases (13), and combine different types of therapeutic exercises to not only work locally on the scar, but also look to improve capabilities like control of the lumbopelvic region (14). Most protocols lack consensus about key points like strength evaluation (how to evaluate it, positions, angles, the amount of strength and type necessary to progress between phases or for RTP) (12-14).
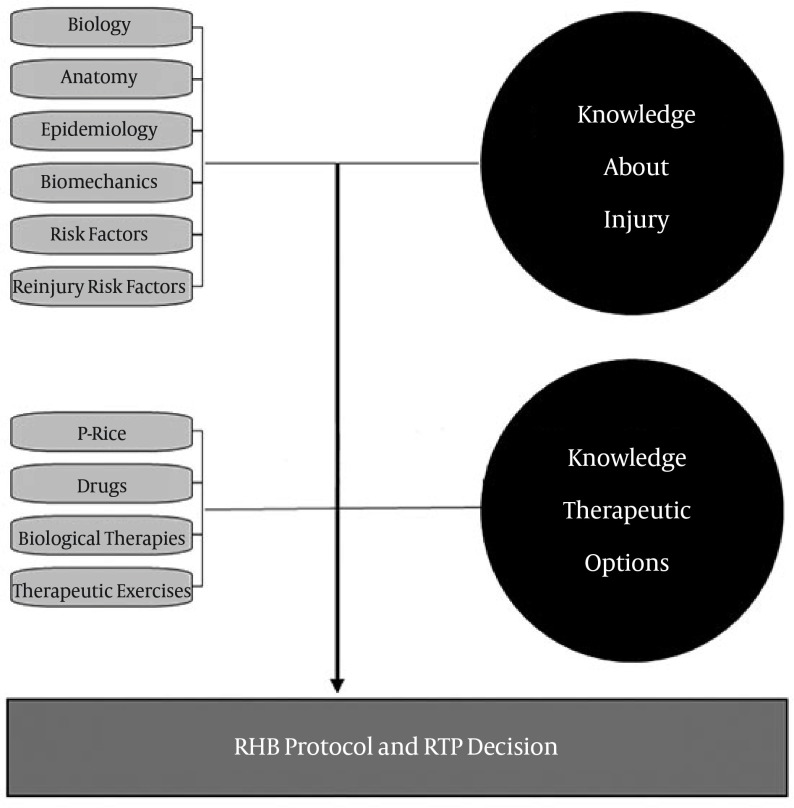
In our opinion a rehabilitation protocol should be based on the current available evidence (13). Knowledge about the injury including tissue healing, risk factors and rehabilitation, and clinical experience is valuable to bridge gaps in literature. The aim of this review is to describe an evidence-driven rehabilitation protocol for HMIs.
Figure 1. Rehabilitation Protocol Design Basis; RHB, Rehabilitation.
1.1. Muscle Injury Biology
Muscle healing is characterised by a reparative process (1) that involves formation of a scar (15). The scar tissue formation has been observed from 6 weeks (16) until 23 months (17) after the injury. Skeletal muscle healing is divided into three phases: destruction, repair and remodelling (18). The destruction phase involves myofibres rupture and necrosis, haematoma formation and initiation of an inflammatory reaction. The repair phase is characterised by phagocytosis, connective tissue production, and subsequently revascularisation. In the remodelling phase there is scar organisation, neo-myofibres maturation and the recovery of the functional capacities, with a new myotendinous junction (MTJ) between the repaired myofibres (17-19). The optimal healing process is characterised by stimulating regeneration and minimizing reparation, to minimise the size of the scar.
1.2. Hamstrings Anatomy and Function
The muscles most commonly injured in sport are the hamstrings, rectus femoris and medial head of the gastrocnemius, all primarily biarticular muscles with high proportion of fast-twitch fibers and complex architecture (2). The semimembranosus (SM), semitendinosus (ST), and biceps femoris long head (BFlh) are biarticular, whereas biceps femoris short head (BFsh) is mono-articular. Hamstrings cross over two joints to allow simultaneous knee flexion and hip extension. This biarticular anatomy sometimes means that the hamstring muscles are stressed heavily over two joints simultaneously, as in contracting eccentrically at the hip and knee while lengthened in terminal swing phase of running (20, 21). The different nerve supplies of the short (peroneal) and long (tibial) heads of biceps femoris suggests different function and it has been suggested that a lack of coordination during contraction is associated with HMIs (22). Anterior pelvic tilt (23), the proportion of type II fibers, and muscle architecture are other potential anatomical risk factors for sustaining HMIs. As with all musculoskeletal injuries, the aetiology of HMIs is multifactorial; related to function, anatomy and other factors including genes, hamstring strength, etc. and the co-existence of all previous referred factors are the reason to explain hamstrings high injury rate (9).
1.3. Injury Mechanism and Types
Muscle strain injuries are frequently located close to the MTJ (18), or around an intramuscular tendon (24). Hamstring injuries can be divided based on injury mechanism into sprinting or stretching injuries (25). The stretching type occur during movements with combined hip flexion and knee extension, in these cases injuries are most commonly located in the SM proximal MTJ or its free tendon, and the time loss is high (26). The sprinting type occur during running and are typically located on BFlh and the time loss is shorter than in the stretching type (25). Therefore, the mechanism and moment when the injury occurs will help us for the diagnosis. The moment when the injury occurs during running can be allocated in connection with the running phase. The running cycle is divided in the stance and the swing phase (27) and sprinting HMIs have been associated with both late swing (20, 28), and the early stance phase (29). Hamstrings are activated throughout the running cycle with peaks during the terminal swing and early stance (30, 31). During the terminal swing the biarticular hamstrings are lengthening and absorbing energy, producing their peak force, reaching peak strain and performing the highest negative work (21). Hamstring peak length does not vary significantly during running progression from submaximal to maximal velocity (27). On the other hand, force, power and work steadily increase with speed (20, 21, 31, 32).
1.4. Injury Risk Factors
The knowledge about the injury/reinjury risk factors will help in designing therapeutic or preventive programs for it. In the last two years several reviews and a meta-analyses investigating risk factors for HMIs have been published (9, 33-35), trying to increase the knowledge about this point.
A recent meta-analysis identified evidence that age, previous hamstring injury and increased quadriceps peak torque are associated with HMIs (35); about other risk factor including weight, flexibility (hamstrings, hip flexor, quadriceps), ankle ROM, proprioception, ethnicity, other strength measurements (hamstrings peak torque, H: H ratio), playing position, and psychological factors, may be associated but more research is required to confirm an association (35). There are also a considerable number of risk factors showing little correlation, including physical performance (anaerobic fitness, VO2 max., peak O2 uptake, CMJ, standing jump, running speed, maximal average power), anthropometric measures (BMI, height), strength (abdominal strength), dominant limb, slump test, mechanism of injury, player exposure, and more (35). Although not all are modifiable, potential risk factors need to be considered in designing rehabilitation and prevention programs.
1.5. Reinjury Risk Factors
Hamstring reinjury can be due to persisting risk factors, or because some maladaptation secondary to initial HMIs (33-36). Potential maladaptation associated with HMI recurrence includes scar tissue formation, reduced flexibility, strength deficits, selective hamstring atrophy and shifts in the torque-joint angle relationship (36). There is limited evidence supporting these suggestions. Previously injured hamstrings have been suggested to have a larger peak torque angle (i.e. in more knee flexion) (37), but prospective studies are needed to confirm this finding (38). After a HMIs, especially regarding BFlh, several long-lasting maladaptations have been described: a reduced BFlh muscle volume with BFsh hypertrophy 5 - 23 months after the injury (17, 19); eccentric strength deficits, decreased EMG activity (39, 40), and other strength and functional test deficiencies (41). The shift in knee flexion PT angle and the loss in eccentric strength might persist for months or years (42, 43), and it is not known why PT angle or eccentric strength deficits do not normalize after regular training and competing (36). These maladaptations suggest a disturbance in neuromuscular function after HMIs that may not reverse with current rehabilitation protocols or return to normal sport activity (17, 39, 40). Reduced hamstring activation can be a protective mechanism to for the injured muscle, which complicates the rehabilitation process (39).
2. Evidence Acquisition
2.1. Clinical Consideration in Rehabilitating and Therapeutic Options
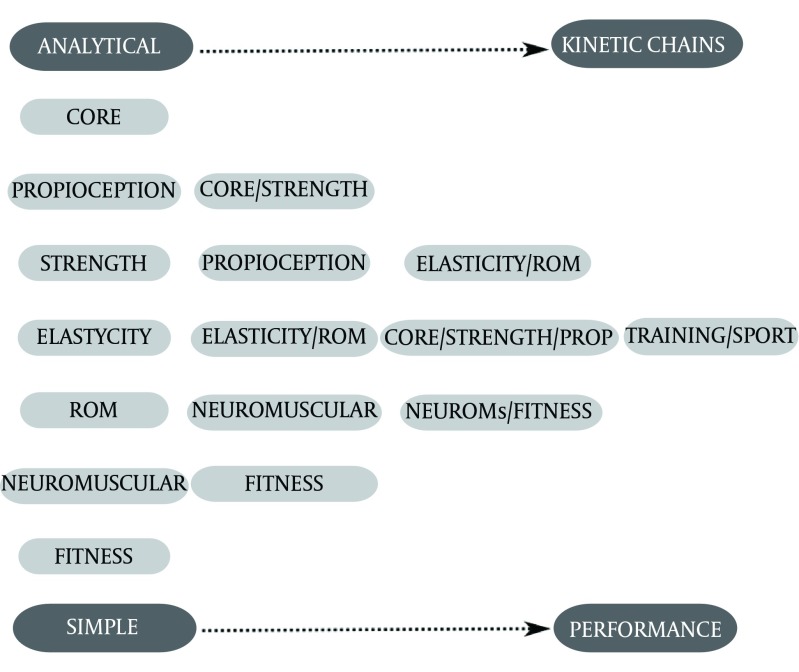
Several protocols have been published using stretching exercises (44), balance (45), eccentrics exercises (46, 47), or different combinations of exercises (12-14, 48). Despite the multifactorial aetiology of HMIs (9, 49, 50) rehabilitation programs generally focus on just one or few factors. Our purpose is to propose a multi-phase and criteria-based rehabilitation programme with clear objectives and progression criteria in each phase, as in previous rehabilitation protocols (13); but this program will include a core battery of exercises designed to address modifiable potential risk factors for HMIs (51, 52). Criteria to design the exercises are described, therefore, they can be tailored to individual ability and goals, and will be progressed from single joint, low demand to more complex and combined joint movements, until rehabilitation exercises reproduce sport movements and load demands.
Figure 2. Therapeutic Exercises Combination, And Progresion During Phases.
When designing the exercises for each phase it is necessary to follow the criteria described, but also taking into account hamstrings anatomy and function, injury mechanism, type of sport practised for the athlete etc. (53). Exercise parameters that need to be taken into account include contraction type and load, ROM, uni- versus bi-lateral, open versus closed kinetic chain and hip/knee dominant versus multi-joint movements exercise (54, 55). Regardless of the injury severity, progression between phases is based on achieving clear criteria (56), as previously illustrated (12), Table 1.
Table 1. Rehabilitation Protocol Purpose Describing the Criteria to Design the Exercises in Each Phase, the Goals and Test to Progress Between Phases, and RTP Criteria a.
| Acute Phase | Subacute Phase | Functional Phase | |
|---|---|---|---|
| Exercise design criteria | |||
| Proprioception | Start on a stable surface and progress to light instability (soft mat, dynadisk or similar). Knee flexion, start 0° and progress until 30°. Static movement and progress to low unstable dynamic. | Increase instability (bosu, balance board, rocker board or similar). Knee flexion, progress to 45°. Moderate reactive/strength movement. Active and wide movements. | Unstable surface. Knee flexion progress to 90°. Intense strength and reactive movements. |
| Core | Static exercises on stable surface in frontal, sagittal and transverse planes. | Dynamic exercises in frontal, sagittal and transverse planes from stable surface and progress to one unstable point; unstable elements progressing in instability (soft mat to fitball). | Dynamic exercises on two unstable points. Exercises in standing position reproducing functional movements (acceleration, deceleration, and dynamic stabilization). No limit. |
| Flexibility and rom | Stretch with ESH ≤ 45, avoiding pain. | Stretch with ESH ≤ 70, avoiding pain. | No limit. |
| Strength and power | ESH ≤ 45, avoiding pain. Isolated knee flexion or hip extension exercises, progress to combine both actions. When starting CKC exercises, first unipodal and progress to bipodal. In the corresponding ESH star with ISOM, progress to CONC and ECC and progress in muscle length avoiding pain or discomfort. | ESH ≤ 70 avoiding pain. In the corresponding ESH, progress in analytic movements length, velocity and load to the maximum effort; and increase combine movement demands. OKC and CKC uni and bipodal exercises. | No ESH limit. Progress in length, joint velocity, load and complexity. Horizontal strength application exercises. |
| Neuromuscular and fitness | ESH ≤ 45, avoiding pain. Start on a soft surface and progress to hard (to reduce eccentric contraction). Start walking on treadmill and progress until V max ≤ 8 km/h, 5% slope to decrease ESH | ESH ≤ 70 avoiding pain. Start on a soft surface and progress to hard. Run on treadmill, progress until 70% of athletes maximal speed, 3 % slope to decrease ESH | No ESH limit. On hard surface. Progress until maximal speed, start on flat and progress to negative slope |
| Goals and test to progress | No pain or discomfort during exercises. To find and maintain a neutral spine position in static (laying, standing or sitting) and during exercises. Isometric knee flexion strength, decubito prono knee flexion 45° and hip 0° > 50% of previous data or uninjured leg (dynamometer or similar). Isometric hip extension strength, decubito supine hip flexion 45° and Knee 0° > 50% of previous data or uninjured leg (dynamometer or similar). Full knee and hip isolated tested ROM | No pain or discomfort during exercises. Not tilting the pelvis or flattening the spine during exercises. Isometric knee flexion strength in decubito supino knee flexion 25° and hip flexion 45°, less than 10% asymmetry from previous data or uninjured leg (dynamometer or similar). Isometric hip extension strength in decubito supino knee 0° and hip flexion 70°, less than 10% asymmetry from previous data or uninjured leg (dynamometer or similar). Less than 10° asymmetry in in AKET Less than 10° asymmetry in the Active Hip Flexion Test. Modified Thomas test > 5 and symmetry below horizontal. Deep squat test (50). Single leg squat (51). Runner pose test (51). In-line lunge test (50). | No pain or discomfort during exercises. Correct spine control and strength transfer during exercises. Integrate strength, neuromuscular and proprioceptive work. Hip strength test in bipedestation knee 0° hip at maximum hip flexion achieved in contralateral leg, no asymmetry (dynamometer or similar). Isokinetic criteria: Differences higher than 20% should be avoided in absolute values. Normal isokinetic ratios No asymmetry in the Active Hip Flexion Test. No asymmetry in AKET |
| Criteria | |||
| Functional Test | A normal week training with the group, without pain, discomfort or "fears". Normal performance by GPS or similar (distances, speeds, accelerations), and HR data (training zones%, etc). | ||
| Athlete “psycho” | Full performance feelings and no fear/doubts from player or similar expression to describe a positive feeling from the subject. | ||
| Clinical Test | Free pain maximal eccentric knee extension in decubito prono hip 0° knee 90° and moves to 0°; and free pain maximal eccentric hip extension in decubito supine knee 0° hip 0° and moves to 70°. | ||
aAbbreviations: aKET, active knee extension test; CKC, close kinetic chain; CON, concentric; ECC, eccentric; ESH, elongation stress on hamstrings; HR, heart rate; ISOM, isometric; OKC, open kinetic chain; ROM, range of motion.
Figure 3. Exercise Progression Examples.
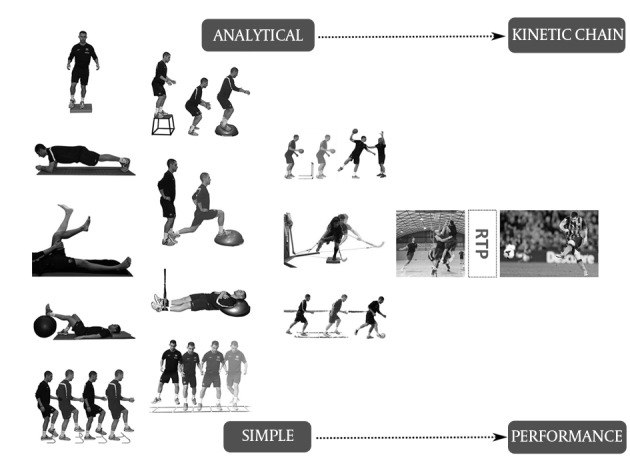
Acute phase in first column (five exercises), subacute phase in the second column (four exercises), and functional in the third column.
2.2. Protection-Rest, Ice, Compression and Elevation (P-RICE)
Immediately after the injury, compression (57), ice (58) and non-painful movements are encouraged (13, 18), because an early mobilization foments scar healing (collagen penetration and orientation through the scar tissue) (1). The rehabilitation program can be commenced when normal pain free gait is achieved (59).
2.3. Drugs and Biological Therapies
There is no clear evidence regarding the use of medications. (60), cooling (58), or Platelet Rich Plasma (61), but with limited impact on RTP or reinjury statistics. The use of NSAIDs did not modify the outcome for HMIs (60), and is not recommended because its inhibitory effect on satellite cell, macrophages, and protein formation (62). To date, there is no high-level evidence to support the widespread use of platelet-rich plasma (61).
2.4. Elongation Stress on Hamstrings
The concept of elongation stress on hamstrings (ESH) is recently introduced and aims to assess hamstring elongation during exercise and function. This is achieved by subtracting the knee flexion angle from the hip flexion angle (63). Larger positive ESH values are associated with greater hamstring tissue stress (54). Running cycle kinematics can be used to calculate the ESH during late swing or early stance hamstring injury. During running the hip ROM goes from 70° flexion to 45° extension, and from 30° - 130° knee flexion (27, 64).
The hamstrings PT angle is influenced by hip flexion, when hip flexion increase will cause an increase in the PT angle in all muscular contraction (63); and as the same authors recognise, this has to be taken into account when designing the exercises, because to perform strength exercises at long musculotendinous length with a high hip angle can be more efficient preventing injuries because of the shift of PT angle to longer muscle length (54).
Therefore, we can use the ESH as a criterion to objectively monitor hamstrings stretch progression during the rehabilitation and to determine the ROM to work during the different phases and exercises. There is no scientific data to determine ROM progression criteria or goals to achieve between phases. In previous published protocols the goals related to ROM are non-existing (47) or very variable (12-14, 46, 47, 65), Table 2.
Table 2. Range of Motion (ROM) and Strength Criteria for Progression Through Phases in Previous Rehabilitation Protocols Published in the Literaturea.
| Study/Goals | Acute Phase | Subacute/Regenerating Phase | Functional Phase |
|---|---|---|---|
| Clanton (65) | |||
| ROM | Normal gait | Pain free full AROM | Pain free for sports movements |
| STR | Generic recommendations | ||
| Heiderscheit (13) | |||
| ROM | Normal walking stride without pain | Full ROM without pain | |
| STR | Pain free ISOM sub-maximal (50% - 70%) prone knee flexion (67) MST | Full strength (5/5) pain free prone knee flexion (90°) MST | Full strength pain free MST prone knee flexion (90° - 15°). ISOK: Less than 5% bilateral deficit in the ratio ECC-H (30°/s): CONC-Q (240°/s). Bilateral symmetry in CONC knee flexion PT angle at 60°/s |
| Mendiguchia (12) | |||
| ROM | AKE test < 10% asymetry and < 20 MTT > 5 and symmetry below horizontal | ||
| STR | Prone knee flexed 15° < 10% asymmetry ISOM strength (DYN) | ISOK: PT angle < 28 during knee flexion 60°/s, asym. < 8 Hip extension strength, ISK hip extension 60°/s < 10 asym. | |
| Schmitt (46) | |||
| ROM | Normal walking pain free | Full ROM pain free | |
| STR | Pain free submaximal ISOM contraction (50% - 75%) during prone knee flexion (90°) MST | Strength (5/5) pain free, prone knee flexion (67) MST Asymetry < 20% compared against uninjured limb Pain free max ECC in a non-lengthened state | Full strength without pain in lengthened position. Bilateral symmetry in knee flexion PT angle |
| Askling (47) | |||
| ROM | Progression in load/speed/excursion based on the avoidance of the pain criterion | ||
| STR | Progression in load/speed/excursion based on the avoidance of the pain criterion | ||
| Silder (14) | |||
| ROM | Normal walk, same stride length and stance time on injured and non injured limbs (visually assessed) | Jog FW and BW (same stride length and stance time) on injured/non injured limbs (visually assessed) | |
| STR | A pain-free ISOM contraction at 90° of knee flexion with a MST judged to be at least 4/5 | Full strength (5/5 MST) prone at 90° of knee flexion (tibia in neutral/internally and externally rotated) | Full strength (5/5 MST) in various knee positions prone, hip 0° of flexion and knee flexed at 90° and 15°; (tibia in neutral/internally and externally rotated) |
a Abbreviations: AROM, active range of motion; ECC, eccentric; DYN, dynamometer; ISOM, isometric; MST, manual strength test; MTT, modified thomas test; ROM, range of motion; STR, strength.
Because hamstrings are a biarticular muscles, the ROM evaluation is more complex, to monitor hamstrings stretch progression with an objective and clear tool seems useful.
2.5. Neuromuscular Exercises, Propioception and Stretching
Two recent reviews conclude that neuromuscular training programmes with different exercises (stretching, strength, plyometrics, balance, agility, stretching, running, cutting and landing technique) can reduce the relative risk of lower limb injuries in sport (acute and overuse), and injury severity (66). There is also a reduction in HMIs risk with neuromuscular training (45, 68). In the same way, programs based on proprioception exercises have shown to be effective in injury prevention (69), and specifically muscle injuries (45). The ideal neuromuscular exercises are sports-specific, involve progressive complexity and challenge (e.g. from linear low demanding exercises to change of direction and explosive).
Although stretching is popular among athletes and often prescribed by health professionals there is no consensus regarding whether stretching reduces injury risk or improves performance (70). Reduced hamstring flexibility may, however be a potential risk factor for HMIs (35), and has been used to grade hamstrings injury severity (71). Hamstring strain rehabilitation programs based on stretching exercises (44), or increasing ROM (23), have reported positive outcomes.
2.6. Core Strengthening Exercises
Lumbo-pelvic muscles can influence hamstring function during running (20) by modifying pelvic tilt and therefore influencing hamstring length (72), changing maximal force generating capacity (73), performance (74), and in its treatment (14, 48). There is less anterior pelvic tilt in unilateral exercises which reduces ESH (54), and they also allow the clinician to train each side to a capacity when there is side-to-side asymmetry (75). When a higher elongation stress is tolerated, bilateral exercises can be introduced. A key focus of core strength exercise is achieving and maintaining neutral spine position in various positions including lying, sitting, standing and during athletic performance (76).
Proprioception criteria for progression are described (77); but has been difficult to find criteria to design core exercises, progression or test with good agreement in the literature. There are rehabilitation protocols for HMIs using core exercises with good results (14, 48), therefore this protocol purpose decided to follow their criteria, adding unstable supports to increase difficulty, and progressing in movementj demands and instability; the goal is to be able to perform high-level activities while still stabilizing the spine (76).
2.7. Strength
Hamstrings PT angle shifts to longer muscle length after eccentric training, and there is a greater shift in PT angle when more hamstring muscle elongation is achieved during loading (78). This shift in hamstring PT angle has also been reported after concentric exercises (79), but only when performed at longer lengths (78). Eccentric lengthening exercises have been shown to improve hamstring flexibility (80), reduce risk of injury (81) and are associated with positive outcomes in HMIs rehabilitation (47). We propose performing strength exercises at longer lengths in order to maximise the increase in PT angle. Eccentric biased strengthening is also important because there is greater reduction in eccentric compared with concentric knee flexor strength post fatigue
decreasing the functional hamstrings to quadriceps ratio in patients with normal ratios before fatigue (36). Eccentric loading can be performed at slower velocities, as this still protects against the very fast angular velocities (up to 1000°/s) during running (54). Starting with isometric and concentric loading is important for regaining bulk and strength and to support tissue healing initially.
Only general recommendations about the quantification and progression of strength exercises during the rehabilitation are found (1, 18); and the test and position used to evaluate it in previous protocols are variable, Table 2. In our method isometric, concentric and eccentric exercises will overlap during the protocol; with part of the strength work performed at long lengths (20, 21).
3. Results
3.1. Health and Performance Evaluation
RTP decisions should be based on specific criteria including tests to confirm functional recovery (56). Normalised strength values are considered essential for athletes’ RTP, and can be tested in several ways. Manual strength test has been widely used, but in athletes’ rehabilitation this scale cannot be used to detect subtle differences in strength (82).
Isometric strength tests are low cost, easily performed and have adequate reliability (83). There is no agreement in the literature about the relationship between isometric strength and dynamic sports performance (83). Another issue is joint angle used for testing varies in the literature (84). Isometric tests should be performed at the angle at which peak force is achieved in the performance of interest (12).
Isokinetic tests are reproducible, allow muscle group isolation and test dynamic strength (85). Evaluation is frequently performed in non-weight-bearing open-kinetic chain positions so may not correlate with functional performance (83). Hamstring isokinetic strength differences between injured and uninjured legs of around 5% - 10% are considered to demonstrate restored function before RTP (12, 86). Recent studies show no differences in isokinetic strength between athletes that have been reinjured and those that have not been reinjured (19, 87). In one of these studies, 67% of athletes RTP with at least one hamstring isokinetic variable in more than 10% deficit compared to the non-injured side, and the reinjury rate was 11.5% (87). Isokinetic tests do not detect some performance deficits (12, 39, 40). Especially important are the deficits in horizontal strength and its effects on running performance (88), in spite of the complexity for its evaluation (41).
Power should be included in RTP considerations because it reflects sports performance (83). The preferable method for power measurement is open to discussion (83). Isoinertial dynamometry is probably more appropriate than isokinetic testing to measure power because it better reproduces human movement and higher speeds can be achieved (83).
There are several functional tests that evaluate hamstring function (89). Due to the important role of hip angle in hamstring function, the ideal functional test would be capable of evaluating the performance of injured versus uninjured legs (26) in functional positions.
Hamstrings flexibility has to be assessed in relation to hip and knee movement. There are several tests in the literature like the active knee extension test (AKE), with good inter-tester reliability (67). The Knee ROM deficit in the AKE has been used to predict recovery time in elite athletes after a HMIs (71). The active hip flexion test will be used to isolate hip movement and to evaluate hamstrings flexibility (51). Hip flexor flexibility is measured with the modified Thomas test (90).
Several tests in the literature evaluate core endurance or strength (52, 91), including the dip test, runner pose test and the single leg squat test (52). These tests assess body segment alignment of the trunk, pelvis, and thigh in several planes using validated rating criteria (52). In addition the single leg squat test has also been used to identify people with low hip muscle strength (91), which has been related with an increased risk for lower limb injuries (92).
3.2. Return to Play Decision
Decisions about RTP are part of all injuries treatment, with health, legal, and economical implications but without standard criteria (93, 94). There is no consensus regarding HMIs RTP criteria in the literature (12, 14, 46, 47, 95). A questionnaire based study in professional soccer club doctors found that the criteria for RTP after a HMI were pain resolution, normal strength, subjective feeling of full recovery reported by the player, normal flexibility and achievement of a specific soccer test; with no consensus on how to assess muscle strength (95).
Normalisation of strength, flexibility, fitness, etc. does necessarily mean performance is also recovered. Based on our experience in elite athletes, we recommend that the athlete will have to accomplish a normal week of training with at least four sessions, without pain, discomfort or "fears" and apprehension (96). During this week, performance can be monitored for normalisation by GPS (88) and heart rate data; this performance monitoring should be extended to the competition after RTP. Obviously, before starting regular training, there will be a progression in exercise demands, physically and technically, and from individual to team training.
Fatigue has influence on muscle injuries because of its effect on functional hamstrings to quadriceps ratio (36). Cardiovascular fitness needs to be normalised before competition, heart rate data from training sessions, and data from on field fitness tests are helpful to achieve this.
The strength criteria for RTP are still open for discussion. Isokinetic strength normalisation seems not to be required for successful RTP, but its relation with re-injury risk is unknown (87). Indeed we need to define when strength normalisation is achieved (percentage discrepancy, in how many isokinetic variables), or which data do we have to use to check strength normalisation, absolute values or ratios, contralateral leg or previously collected data (97). A study in 1252 American football players shows that mean quadriceps strength in the dominant leg is 1.9% higher, therefore, to use ratios which are more stable can be a good option (97).
Due to the recent papers published about isokinetic strength deficit and reinjury (87), to recommend a percentage for asymmetry is difficult, but seems logical to avoid more than 20% asymmetry in absolute values and achieve normal ratios before progressing to power rehabilitation and sport. The authors feel that it is necessary to add a hip extension strength test, with isokinetic (98) or similar, 100% related to the contralateral leg data or previous test, in a functional position, Table 1.
In addition to the strength testing, we recommend two clinical tests to evaluate patient readiness to RTP: This will include maximal eccentric knee flexion and maximal eccentric hip extension test, assessing the athlete apprehension, pain or discomfort. A maximal eccentric strength test without apprehension or pain is commonly used for us as part of RTP decisions in our daily practice, Table 1.
Some of the main maladaptations after HMIs seem to be related with a neuromuscular inhibition indicated by decreased EMG activity (39), the mechanisms of this neuromuscular inhibition and its effects on HMIs reinjury rates or athletes performance after RTP are still unclear. Further research is needed to decide if EMG evaluations should be incorporated as RTP criteria, but to detect and follow EMG disturbances evolution in injured athletes would be the first step to understand if in some HMIs there is a neuromuscular deficit that is influencing prognosis and reinjury.
The role of MRI to guide RTP clearance is at least limited, in a recent study the 89% of HMIs clinically recovered for RTP showed increased signal intensity on fluid-sensitive sequences on MRI, and one third of changes were suggestive of new fibrous tissue, the author therefore concluded that normal MRI is not necessary for the RTP (99); in addition another recent paper detected MRI abnormalities at RTP with posterior normalization (19), Table 1.
4. Conclusions
Resuming the main lines of the purpose, exercises in open and closed kinetic chain for hip extension and knee flexion, overlapping strength work (isometric, concentric and eccentric) in lengthening positions with a high hip angle, focusing on recovering eccentric strength in all degrees but especially when strain on hamstrings is higher (late degrees). Work specific hip extension to avoid horizontal strength deficits, and as soon as possible, to perform part of the strength work in standing with hip in functional position. We recommend putting the athlete on a secondary preventive program during the months after RTP.
We offer criteria to design the exercises, to progress between phases and for the RTP decision, which will be a useful tool in this key moment. The aim of these criteria is to objectify all physical variables involved in the RTP, making the decision less subjective or experience dependent. Even so, the RTP decision will be still predominantly experience-based. The recommendations reflect our current understanding, but should develop over time to come to a more evidence based decision process.
As we have recognized, several points are open to discussion; actually we send this purpose as an invitation to all people taking care of athletes’ health to join efforts, send suggestions for improvements and look to find the best rehabilitation strategy for HMIs. Both authors’ institutions have been working with this aim for the last years, trying to create networks to help this policy develop. Network collaboration is crucial if we want to improve the management of muscle injuries, since no scientific evidence is achieved on key points if samples are not enough; we can make mistakes as researchers; new ones, but should never repeat old mistakes.
Acknowledgments
Joaquim Chaler from FC Barcelona medical department and PM and R Department Egarsat. Terrassa, Barcelona, Spain. For his support about isokinetic and strength assessment.
Footnotes
Authors’ Contribution:The idea and design of the paper was from Xavier Valle and Gil Rodas. Xavier Valle did the review of the literature to incorporate the knowledge about the injury, therapeutic options and criteria to design the exercises, etc. Bruce Hamilton and Johannes L Tol. offer support in the idea design and creating process. Also both gave support about English grammar. Peter Malliaras and Nikos Malliaropoulos as experts in the field, reviewed the paper and offered suggestion to improve the paper. Peter Malliaras also offered support about English grammar. Jaume Jardi, Vicenc Rizo and Marcel Moreno, offered support in the exercise practical design protocol. All authors read and accepted the final draft.
Financial Disclosure:No competing interests “We have read and understood the Asian journal of sports medicine policy on declaration of interests and declare that we have no competing interests”.
References
- 1.Jarvinen TA, Jarvinen TL, Kaariainen M, Kalimo H, Jarvinen M. Muscle injuries: biology and treatment. Am J Sports Med. 2005;33(5):745–64. doi: 10.1177/0363546505274714. [DOI] [PubMed] [Google Scholar]
- 2.Ekstrand J, Hagglund M, Walden M. Epidemiology of muscle injuries in professional football (soccer). Am J Sports Med. 2011;39(6):1226–32. doi: 10.1177/0363546510395879. [DOI] [PubMed] [Google Scholar]
- 3.Borowski LA, Yard EE, Fields SK, Comstock RD. The epidemiology of US high school basketball injuries, 2005-2007. Am J Sports Med. 2008;36(12):2328–35. doi: 10.1177/0363546508322893. [DOI] [PubMed] [Google Scholar]
- 4.Feeley BT, Kennelly S, Barnes RP, Muller MS, Kelly BT, Rodeo SA, et al. Epidemiology of National Football League training camp injuries from 1998 to 2007. Am J Sports Med. 2008;36(8):1597–603. doi: 10.1177/0363546508316021. [DOI] [PubMed] [Google Scholar]
- 5.Orchard J, Seward H. Epidemiology of injuries in the Australian Football League, seasons 1997-2000. Br J Sports Med. 2002;36(1):39–44. doi: 10.1136/bjsm.36.1.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alonso JM, Junge A, Renstrom P, Engebretsen L, Mountjoy M, Dvorak J. Sports injuries surveillance during the 2007 IAAF World Athletics Championships. Clin J Sport Med. 2009;19(1):26–32. doi: 10.1097/JSM.0b013e318191c8e7. [DOI] [PubMed] [Google Scholar]
- 7.Schache AG, Dorn TW, Wrigley TV, Brown NA, Pandy MG. Stretch and activation of the human biarticular hamstrings across a range of running speeds. Eur J Appl Physiol. 2013;113(11):2813–28. doi: 10.1007/s00421-013-2713-9. [DOI] [PubMed] [Google Scholar]
- 8.Ekstrand J, Hagglund M, Walden M. Injury incidence and injury patterns in professional football: the UEFA injury study. Br J Sports Med. 2011;45(7):553–8. doi: 10.1136/bjsm.2009.060582. [DOI] [PubMed] [Google Scholar]
- 9.Opar DA, Williams MD, Shield AJ. Hamstring strain injuries: factors that lead to injury and re-injury. Sports Med. 2012;42(3):209–26. doi: 10.2165/11594800-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 10.Malliaropoulos N, Isinkaye T, Tsitas K, Maffulli N. Reinjury after acute posterior thigh muscle injuries in elite track and field athletes. Am J Sports Med. 2011;39(2):304–10. doi: 10.1177/0363546510382857. [DOI] [PubMed] [Google Scholar]
- 11.Verrall GM, Esterman A, Hewett TE. Analysis of the Three Most Prevalent Injuries in Australian Football Demonstrates a Season to Season Association Between Groin/Hip/Osteitis Pubis Injuries With ACL Knee Injuries. Asian J Sports Med. 2014;5(3):e25411. doi: 10.5812/asjsm.23072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mendiguchia J, Brughelli M. A return-to-sport algorithm for acute hamstring injuries. Phys Ther Sport. 2011;12(1):2–14. doi: 10.1016/j.ptsp.2010.07.003. [DOI] [PubMed] [Google Scholar]
- 13.Heiderscheit BC, Sherry MA, Silder A, Chumanov ES, Thelen DG. Hamstring strain injuries: recommendations for diagnosis, rehabilitation, and injury prevention. J Orthop Sports Phys Ther. 2010;40(2):67–81. doi: 10.2519/jospt.2010.3047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Silder A, Sherry MA, Sanfilippo J, Tuite MJ, Hetzel SJ, Heiderscheit BC. Clinical and morphological changes following 2 rehabilitation programs for acute hamstring strain injuries: a randomized clinical trial. J Orthop Sports Phys Ther. 2013;43(5):284–99. doi: 10.2519/jospt.2013.4452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Silder A, Thelen DG, Heiderscheit BC. Effects of prior hamstring strain injury on strength, flexibility, and running mechanics. Clin Biomech (Bristol, Avon). 2010;25(7):681–6. doi: 10.1016/j.clinbiomech.2010.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Connell DA, Schneider-Kolsky ME, Hoving JL, Malara F, Buchbinder R, Koulouris G, et al. Longitudinal study comparing sonographic and MRI assessments of acute and healing hamstring injuries. AJR Am J Roentgenol. 2004;183(4):975–84. doi: 10.2214/ajr.183.4.1830975. [DOI] [PubMed] [Google Scholar]
- 17.Silder A, Heiderscheit BC, Thelen DG, Enright T, Tuite MJ. MR observations of long-term musculotendon remodeling following a hamstring strain injury. Skeletal Radiol. 2008;37(12):1101–9. doi: 10.1007/s00256-008-0546-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jarvinen TA, Jarvinen TL, Kaariainen M, Aarimaa V, Vaittinen S, Kalimo H, et al. Muscle injuries: optimising recovery. Best Pract Res Clin Rheumatol. 2007;21(2):317–31. doi: 10.1016/j.berh.2006.12.004. [DOI] [PubMed] [Google Scholar]
- 19.Sanfilippo JL, Silder A, Sherry MA, Tuite MJ, Heiderscheit BC. Hamstring strength and morphology progression after return to sport from injury. Med Sci Sports Exerc. 2013;45(3):448–54. doi: 10.1249/MSS.0b013e3182776eff. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chumanov ES, Heiderscheit BC, Thelen DG. The effect of speed and influence of individual muscles on hamstring mechanics during the swing phase of sprinting. J Biomech. 2007;40(16):3555–62. doi: 10.1016/j.jbiomech.2007.05.026. [DOI] [PubMed] [Google Scholar]
- 21.Schache AG, Dorn TW, Blanch PD, Brown NA, Pandy MG. Mechanics of the human hamstring muscles during sprinting. Med Sci Sports Exerc. 2012;44(4):647–58. doi: 10.1249/MSS.0b013e318236a3d2. [DOI] [PubMed] [Google Scholar]
- 22.Dahmane R, Djordjevic S, Smerdu V. Adaptive potential of human biceps femoris muscle demonstrated by histochemical, immunohistochemical and mechanomyographical methods. Med Biol Eng Comput. 2006;44(11):999–1006. doi: 10.1007/s11517-006-0114-5. [DOI] [PubMed] [Google Scholar]
- 23.Cibulka MT, Rose SJ, Delitto A, Sinacore DR. Hamstring muscle strain treated by mobilizing the sacroiliac joint. Phys Ther. 1986;66(8):1220–3. doi: 10.1093/ptj/66.8.1220. [DOI] [PubMed] [Google Scholar]
- 24.Garrett WJ, Rich FR, Nikolaou PK, Vogler JB 3rd. Computed tomography of hamstring muscle strains. Med Sci Sports Exerc. 1989;21(5):506–14. [PubMed] [Google Scholar]
- 25.Askling CM, Malliaropoulos N, Karlsson J. High-speed running type or stretching-type of hamstring injuries makes a difference to treatment and prognosis. Br J Sports Med. 2012;46(2):86–7. doi: 10.1136/bjsports-2011-090534. [DOI] [PubMed] [Google Scholar]
- 26.Askling C, Saartok T, Thorstensson A. Type of acute hamstring strain affects flexibility, strength, and time to return to pre-injury level. Br J Sports Med. 2006;40(1):40–4. doi: 10.1136/bjsm.2005.018879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Thelen DG, Chumanov ES, Hoerth DM, Best TM, Swanson SC, Li L, et al. Hamstring muscle kinematics during treadmill sprinting. Med Sci Sports Exerc. 2005;37(1):108–14. doi: 10.1249/01.mss.0000150078.79120.c8. [DOI] [PubMed] [Google Scholar]
- 28.Chumanov ES, Schache AG, Heiderscheit BC, Thelen DG. Hamstrings are most susceptible to injury during the late swing phase of sprinting. Br J Sports Med. 2012;46(2):90. doi: 10.1136/bjsports-2011-090176. [DOI] [PubMed] [Google Scholar]
- 29.Orchard JW. Hamstrings are most susceptible to injury during the early stance phase of sprinting. Br J Sports Med. 2012;46(2):88–9. doi: 10.1136/bjsports-2011-090127. [DOI] [PubMed] [Google Scholar]
- 30.Yu B, Queen RM, Abbey AN, Liu Y, Moorman CT, Garrett WE. Hamstring muscle kinematics and activation during overground sprinting. J Biomech. 2008;41(15):3121–6. doi: 10.1016/j.jbiomech.2008.09.005. [DOI] [PubMed] [Google Scholar]
- 31.Chumanov ES, Heiderscheit BC, Thelen DG. Hamstring musculotendon dynamics during stance and swing phases of high-speed running. Med Sci Sports Exerc. 2011;43(3):525–32. doi: 10.1249/MSS.0b013e3181f23fe8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Thelen DG, Chumanov ES, Best TM, Swanson SC, Heiderscheit BC. Simulation of biceps femoris musculotendon mechanics during the swing phase of sprinting. Med Sci Sports Exerc. 2005;37(11):1931–8. doi: 10.1249/01.mss.0000176674.42929.de. [DOI] [PubMed] [Google Scholar]
- 33.van Beijsterveldt AM, van de Port IG, Vereijken AJ, Backx FJ. Risk factors for hamstring injuries in male soccer players: a systematic review of prospective studies. Scand J Med Sci Sports. 2013;23(3):253–62. doi: 10.1111/j.1600-0838.2012.01487.x. [DOI] [PubMed] [Google Scholar]
- 34.de Visser HM, Reijman M, Heijboer MP, Bos PK. Risk factors of recurrent hamstring injuries: a systematic review. Br J Sports Med. 2012;46(2):124–30. doi: 10.1136/bjsports-2011-090317. [DOI] [PubMed] [Google Scholar]
- 35.Freckleton G, Pizzari T. Risk factors for hamstring muscle strain injury in sport: a systematic review and meta-analysis. Br J Sports Med. 2013;47(6):351–8. doi: 10.1136/bjsports-2011-090664. [DOI] [PubMed] [Google Scholar]
- 36.Fyfe JJ, Opar DA, Williams MD, Shield AJ. The role of neuromuscular inhibition in hamstring strain injury recurrence. J Electromyogr Kinesiol. 2013;23(3):523–30. doi: 10.1016/j.jelekin.2012.12.006. [DOI] [PubMed] [Google Scholar]
- 37.Proske U, Morgan DL, Brockett CL, Percival P. Identifying athletes at risk of hamstring strains and how to protect them. Clin Exp Pharmacol Physiol. 2004;31(8):546–50. doi: 10.1111/j.1440-1681.2004.04028.x. [DOI] [PubMed] [Google Scholar]
- 38.Yeung SS, Suen AM, Yeung EW. A prospective cohort study of hamstring injuries in competitive sprinters: preseason muscle imbalance as a possible risk factor. Br J Sports Med. 2009;43(8):589–94. doi: 10.1136/bjsm.2008.056283. [DOI] [PubMed] [Google Scholar]
- 39.Opar DA, Williams MD, Timmins RG, Dear NM, Shield AJ. Knee flexor strength and bicep femoris electromyographical activity is lower in previously strained hamstrings. J Electromyogr Kinesiol. 2013;23(3):696–703. doi: 10.1016/j.jelekin.2012.11.004. [DOI] [PubMed] [Google Scholar]
- 40.Sole G, Milosavljevic S, Nicholson HD, Sullivan SJ. Selective strength loss and decreased muscle activity in hamstring injury. J Orthop Sports Phys Ther. 2011;41(5):354–63. doi: 10.2519/jospt.2011.3268. [DOI] [PubMed] [Google Scholar]
- 41.Brughelli M, Cronin J, Mendiguchia J, Kinsella D, Nosaka K. Contralateral leg deficits in kinetic and kinematic variables during running in Australian rules football players with previous hamstring injuries. J Strength Cond Res. 2010;24(9):2539–44. doi: 10.1519/JSC.0b013e3181b603ef. [DOI] [PubMed] [Google Scholar]
- 42.Brockett CL, Morgan DL, Proske U. Predicting hamstring strain injury in elite athletes. Med Sci Sports Exerc. 2004;36(3):379–87. doi: 10.1249/01.mss.0000117165.75832.05. [DOI] [PubMed] [Google Scholar]
- 43.Lee MJ, Reid SL, Elliott BC, Lloyd DG. Running biomechanics and lower limb strength associated with prior hamstring injury. Med Sci Sports Exerc. 2009;41(10):1942–51. doi: 10.1249/MSS.0b013e3181a55200. [DOI] [PubMed] [Google Scholar]
- 44.Malliaropoulos N, Papalexandris S, Papalada A, Papacostas E. The role of stretching in rehabilitation of hamstring injuries: 80 athletes follow-up. Med Sci Sports Exerc. 2004;36(5):756–9. doi: 10.1249/01.mss.0000126393.20025.5e. [DOI] [PubMed] [Google Scholar]
- 45.Kraemer R, Knobloch K. A soccer-specific balance training program for hamstring muscle and patellar and achilles tendon injuries: an intervention study in premier league female soccer. Am J Sports Med. 2009;37(7):1384–93. doi: 10.1177/0363546509333012. [DOI] [PubMed] [Google Scholar]
- 46.Schmitt B, Tim T, McHugh M. Hamstring injury rehabilitation and prevention of reinjury using lengthened state eccentric training: a new concept. Int J Sports Phys Ther. 2012;7(3):333–41. [PMC free article] [PubMed] [Google Scholar]
- 47.Askling CM, Tengvar M, Thorstensson A. Acute hamstring injuries in Swedish elite football: a prospective randomised controlled clinical trial comparing two rehabilitation protocols. Br J Sports Med. 2013;47(15):953–9. doi: 10.1136/bjsports-2013-092165. [DOI] [PubMed] [Google Scholar]
- 48.Sherry MA, Best TM. A comparison of 2 rehabilitation programs in the treatment of acute hamstring strains. J Orthop Sports Phys Ther. 2004;34(3):116–25. doi: 10.2519/jospt.2004.34.3.116. [DOI] [PubMed] [Google Scholar]
- 49.Brooks JH, Fuller CW, Kemp SP, Reddin DB. Incidence, risk, and prevention of hamstring muscle injuries in professional rugby union. Am J Sports Med. 2006;34(8):1297–306. doi: 10.1177/0363546505286022. [DOI] [PubMed] [Google Scholar]
- 50.Henderson G, Barnes CA, Portas MD. Factors associated with increased propensity for hamstring injury in English Premier League soccer players. J Sci Med Sport. 2010;13(4):397–402. doi: 10.1016/j.jsams.2009.08.003. [DOI] [PubMed] [Google Scholar]
- 51.Frohm A, Heijne A, Kowalski J, Svensson P, Myklebust G. A nine-test screening battery for athletes: a reliability study. Scand J Med Sci Sports. 2012;22(3):306–15. doi: 10.1111/j.1600-0838.2010.01267.x. [DOI] [PubMed] [Google Scholar]
- 52.Perrott MA, Pizzari T, Opar M, Cook J. Development of clinical rating criteria for tests of lumbopelvic stability. Rehabil Res Pract. 2012;2012:803637. doi: 10.1155/2012/803637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kubota J, Ono T, Araki M, Torii S, Okuwaki T, Fukubayashi T. Non-uniform changes in magnetic resonance measurements of the semitendinosus muscle following intensive eccentric exercise. Eur J Appl Physiol. 2007;101(6):713–20. doi: 10.1007/s00421-007-0549-x. [DOI] [PubMed] [Google Scholar]
- 54.Guex K, Millet GP. Conceptual framework for strengthening exercises to prevent hamstring strains. Sports Med. 2013;43(12):1207–15. doi: 10.1007/s40279-013-0097-y. [DOI] [PubMed] [Google Scholar]
- 55.Malliaropoulos N, Mendiguchia J, Pehlivanidis H, Papadopoulou S, Valle X, Malliaras P, et al. Hamstring exercises for track and field athletes: injury and exercise biomechanics, and possible implications for exercise selection and primary prevention. Br J Sports Med. 2012;46(12):846–51. doi: 10.1136/bjsports-2011-090474. [DOI] [PubMed] [Google Scholar]
- 56.Thorborg K. Why hamstring eccentrics are hamstring essentials. Br J Sports Med. 2012;46(7):463–5. doi: 10.1136/bjsports-2011-090962. [DOI] [PubMed] [Google Scholar]
- 57.Kwak HS, Lee KB, Han YM. Ruptures of the medial head of the gastrocnemius ("tennis leg"): clinical outcome and compression effect. Clin Imaging. 2006;30(1):48–53. doi: 10.1016/j.clinimag.2005.07.004. [DOI] [PubMed] [Google Scholar]
- 58.Bleakley CM, Glasgow P, Webb MJ. Cooling an acute muscle injury: can basic scientific theory translate into the clinical setting? Br J Sports Med. 2012;46(4):296–8. doi: 10.1136/bjsm.2011.086116. [DOI] [PubMed] [Google Scholar]
- 59.Kerkhoffs GM, van Es N, Wieldraaijer T, Sierevelt IN, Ekstrand J, van Dijk CN. Diagnosis and prognosis of acute hamstring injuries in athletes. Knee Surg Sports Traumatol Arthrosc. 2013;21(2):500–9. doi: 10.1007/s00167-012-2055-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Robinson M, Hamilton B. Medical interventions in the management of hamstring muscle injury. Eur J Sport Sci. 2014;14(7):743–51. doi: 10.1080/17461391.2013.878756. [DOI] [PubMed] [Google Scholar]
- 61.Andia I, Sanchez M, Maffulli N. Platelet rich plasma therapies for sports muscle injuries: any evidence behind clinical practice? Expert Opin Biol Ther. 2011;11(4):509–18. doi: 10.1517/14712598.2011.554813. [DOI] [PubMed] [Google Scholar]
- 62.Ziltener JL, Leal S, Fournier PE. Non-steroidal anti-inflammatory drugs for athletes: an update. Ann Phys Rehabil Med. 2010;53(4):278–82. doi: 10.1016/j.rehab.2010.03.001. 282-8. [DOI] [PubMed] [Google Scholar]
- 63.Guex K, Gojanovic B, Millet GP. Influence of hip-flexion angle on hamstrings isokinetic activity in sprinters. J Athl Train. 2012;47(4):390–5. doi: 10.4085/1062-6050-47.4.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Caekenberghe IV, Segers V, Aerts P, Willems P, De Clercq D. Joint kinematics and kinetics of overground accelerated running versus running on an accelerated treadmill. J R Soc Interface. 2013;10(84):20130222. doi: 10.1098/rsif.2013.0222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Clanton TO, Coupe KJ. Hamstring strains in athletes: diagnosis and treatment. J Am Acad Orthop Surg. 1998;6(4):237–48. doi: 10.5435/00124635-199807000-00005. [DOI] [PubMed] [Google Scholar]
- 66.Hubscher M, Refshauge KM. Neuromuscular training strategies for preventing lower limb injuries: what's new and what are the practical implications of what we already know? Br J Sports Med. 2013;47(15):939–40. doi: 10.1136/bjsports-2012-091253. [DOI] [PubMed] [Google Scholar]
- 67.Reurink G, Goudswaard GJ, Oomen HG, Moen MH, Tol JL, Verhaar JA, et al. Reliability of the active and passive knee extension test in acute hamstring injuries. Am J Sports Med. 2013;41(8):1757–61. doi: 10.1177/0363546513490650. [DOI] [PubMed] [Google Scholar]
- 68.Cameron ML, Adams RD, Maher CG, Misson D. Effect of the HamSprint Drills training programme on lower limb neuromuscular control in Australian football players. J Sci Med Sport. 2009;12(1):24–30. doi: 10.1016/j.jsams.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 69.Eils E, Schroter R, Schroder M, Gerss J, Rosenbaum D. Multistation proprioceptive exercise program prevents ankle injuries in basketball. Med Sci Sports Exerc. 2010;42(11):2098–105. doi: 10.1249/MSS.0b013e3181e03667. [DOI] [PubMed] [Google Scholar]
- 70.Fourchet F, Materne O, Horobeanu C, Hudacek T, Buchheit M. Reliability of a novel procedure to monitor the flexibility of lower limb muscle groups in highly-trained adolescent athletes. Phys Ther Sport. 2013;14(1):28–34. doi: 10.1016/j.ptsp.2012.02.004. [DOI] [PubMed] [Google Scholar]
- 71.Malliaropoulos N, Papacostas E, Kiritsi O, Papalada A, Gougoulias N, Maffulli N. Posterior thigh muscle injuries in elite track and field athletes. Am J Sports Med. 2010;38(9):1813–9. doi: 10.1177/0363546510366423. [DOI] [PubMed] [Google Scholar]
- 72.Telhan G, Franz JR, Dicharry J, Wilder RP, Riley PO, Kerrigan DC. Lower limb joint kinetics during moderately sloped running. J Athl Train. 2010;45(1):16–21. doi: 10.4085/1062-6050-45.1.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Rockey AM. The Relationship Between Anterior Pelvic Tilt, Hamstring Extensibility and Hamstring Strength. University of North Carolina at Greensboro: ProQuest; 2008. [Google Scholar]
- 74.Shinkle J, Nesser TW, Demchak TJ, McMannus DM. Effect of core strength on the measure of power in the extremities. J Strength Cond Res. 2012;26(2):373–80. doi: 10.1519/JSC.0b013e31822600e5. [DOI] [PubMed] [Google Scholar]
- 75.Zakas A. Bilateral isokinetic peak torque of quadriceps and hamstring muscles in professional soccer players with dominance on one or both two sides. J Sports Med Phys Fitness. 2006;46(1):28–35. [PubMed] [Google Scholar]
- 76.Barr KP, Griggs M, Cadby T. Lumbar stabilization: a review of core concepts and current literature, part 2. Am J Phys Med Rehabil. 2007;86(1):72–80. doi: 10.1097/01.phm.0000250566.44629.a0. [DOI] [PubMed] [Google Scholar]
- 77.Kloos AD, Heiss GD. Exercise for Impaired Balance. In: Kisner C, Colby LA, editors. Therapeutic exercise. 5 ed. Philadelphia: FA Davis; 2007. pp. 251–70. [Google Scholar]
- 78.Guex K, Degache F, Gremion G, Millet GP. Effect of hip flexion angle on hamstring optimum length after a single set of concentric contractions. J Sports Sci. 2013;31(14):1545–52. doi: 10.1080/02640414.2013.786186. [DOI] [PubMed] [Google Scholar]
- 79.Blazevich AJ, Cannavan D, Coleman DR, Horne S. Influence of concentric and eccentric resistance training on architectural adaptation in human quadriceps muscles. J Appl Physiol (1985). 2007;103(5):1565–75. doi: 10.1152/japplphysiol.00578.2007. [DOI] [PubMed] [Google Scholar]
- 80.O'Sullivan K, McAuliffe S, Deburca N. The effects of eccentric training on lower limb flexibility: a systematic review. Br J Sports Med. 2012;46(12):838–45. doi: 10.1136/bjsports-2011-090835. [DOI] [PubMed] [Google Scholar]
- 81.Hibbert O, Cheong K, Grant A, Beers A, Moizumi T. A systematic review of the effectiveness of eccentric strength training in the prevention of hamstring muscle strains in otherwise healthy individuals. N Am J Sports Phys Ther. 2008;3(2):67–81. [PMC free article] [PubMed] [Google Scholar]
- 82.Whiteley R, Jacobsen P, Prior S, Skazalski C, Otten R, Johnson A. Correlation of isokinetic and novel hand-held dynamometry measures of knee flexion and extension strength testing. J Sci Med Sport. 2012;15(5):444–50. doi: 10.1016/j.jsams.2012.01.003. [DOI] [PubMed] [Google Scholar]
- 83.Pigozzi F, Giombini A, Macaluso A. Do current methods of strength testing for the return to sport after injuries really address functional performance? Am J Phys Med Rehabil. 2012;91(5):458–60. doi: 10.1097/PHM.0b013e31824663ec. [DOI] [PubMed] [Google Scholar]
- 84.Bosco C. Methods of functional testing during rehabilitation exercises. Rehabilitation of Sports Injuries.: Springer; 2001. pp. 11–22. [Google Scholar]
- 85.Pincivero DM, Lephart SM, Karunakara RA. Reliability and precision of isokinetic strength and muscular endurance for the quadriceps and hamstrings. Int J Sports Med. 1997;18(2):113–7. doi: 10.1055/s-2007-972605. [DOI] [PubMed] [Google Scholar]
- 86.Croisier JL, Forthomme B, Namurois MH, Vanderthommen M, Crielaard JM. Hamstring muscle strain recurrence and strength performance disorders. Am J Sports Med. 2002;30(2):199–203. doi: 10.1177/03635465020300020901. [DOI] [PubMed] [Google Scholar]
- 87.Tol JL, Hamilton B, Eirale C, Muxart P, Jacobsen P, Whiteley R. At return to play following hamstring injury the majority of professional football players have residual isokinetic deficits. Br J Sports Med. 2014;48(18):1364–9. doi: 10.1136/bjsports-2013-093016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Mendiguchia J, Samozino P, Martinez-Ruiz E, Brughelli M, Schmikli S, Morin JB, et al. Progression of mechanical properties during on-field sprint running after returning to sports from a hamstring muscle injury in soccer players. Int J Sports Med. 2014;35(8):690–5. doi: 10.1055/s-0033-1363192. [DOI] [PubMed] [Google Scholar]
- 89.Freckleton G, Cook J, Pizzari T. The predictive validity of a single leg bridge test for hamstring injuries in Australian Rules Football Players. Br J Sports Med. 2014;48(8):713–7. doi: 10.1136/bjsports-2013-092356. [DOI] [PubMed] [Google Scholar]
- 90.Harvey D. Assessment of the flexibility of elite athletes using the modified Thomas test. Br J Sports Med. 1998;32(1):68–70. doi: 10.1136/bjsm.32.1.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Crossley KM, Zhang WJ, Schache AG, Bryant A, Cowan SM. Performance on the single-leg squat task indicates hip abductor muscle function. Am J Sports Med. 2011;39(4):866–73. doi: 10.1177/0363546510395456. [DOI] [PubMed] [Google Scholar]
- 92.Leetun DT, Ireland ML, Willson JD, Ballantyne BT, Davis IM. Core stability measures as risk factors for lower extremity injury in athletes. Med Sci Sports Exerc. 2004;36(6):926–34. doi: 10.1249/01.mss.0000128145.75199.c3. [DOI] [PubMed] [Google Scholar]
- 93.Creighton DW, Shrier I, Shultz R, Meeuwisse WH, Matheson GO. Return-to-play in sport: a decision-based model. Clin J Sport Med. 2010;20(5):379–85. doi: 10.1097/JSM.0b013e3181f3c0fe. [DOI] [PubMed] [Google Scholar]
- 94.Benito del Pozo L, Ayan Perez C, Revuelta Benzanilla G, Maestro Fernandez A, Fernández Villa T, Martin Sanchez V. Influencia del estatus profesional de los jugadores de fútbol en la frecuencia y gravedad de las lesiones: estudio piloto comparativo. Apunts. Medicina de l'Esport. 2014;49(181):20–4. [Google Scholar]
- 95.Delvaux F, Rochcongar P, Bruyere O, Bourlet G, Daniel C, Diverse P, et al. Return-to-play criteria after hamstring injury: actual medicine practice in professional soccer teams. J Sports Sci Med. 2014;13(3):721–3. [PMC free article] [PubMed] [Google Scholar]
- 96.Ardern CL, Taylor NF, Feller JA, Webster KE. A systematic review of the psychological factors associated with returning to sport following injury. Br J Sports Med. 2013;47(17):1120–6. doi: 10.1136/bjsports-2012-091203. [DOI] [PubMed] [Google Scholar]
- 97.Zvijac JE, Toriscelli TA, Merrick WS, Papp DF, Kiebzak GM. Isokinetic concentric quadriceps and hamstring normative data for elite collegiate American football players participating in the NFL Scouting Combine. J Strength Cond Res. 2014;28(4):875–83. doi: 10.1519/JSC.0b013e3182a20f19. [DOI] [PubMed] [Google Scholar]
- 98.Sugiura Y, Saito T, Sakuraba K, Sakuma K, Suzuki E. Strength deficits identified with concentric action of the hip extensors and eccentric action of the hamstrings predispose to hamstring injury in elite sprinters. J Orthop Sports Phys Ther. 2008;38(8):457–64. doi: 10.2519/jospt.2008.2575. [DOI] [PubMed] [Google Scholar]
- 99.Reurink G, Goudswaard GJ, Tol JL, Almusa E, Moen MH, Weir A, et al. MRI observations at return to play of clinically recovered hamstring injuries. Br J Sports Med. 2014;48(18):1370–6. doi: 10.1136/bjsports-2013-092450. [DOI] [PMC free article] [PubMed] [Google Scholar]