Abstract
Background
There is a perception among surgeons that hospitals disproportionately transfer unfavorably insured patients for emergency surgical care. Emergency Medical Condition (EMC) designation mandates referral center acceptance of patients for whom transfer is requested. We sought to understand whether unfavorably insured patients are more likely to be designated as EMCs.
Materials and Methods
A retrospective cohort study was performed of patient transfers from a large network of acute care facilities to emergency surgery services at a tertiary referral center from 2009-2013. Insurance was categorized as favorable (commercial or Medicare) or unfavorable (Medicaid or uninsured). The primary outcome, transfer designation as EMC or non-EMC, was evaluated using multivariable logistic regression. A secondary analysis evaluated uninsured patients only.
Results
There were 1,295 patient transfers in the study period. Twenty percent had unfavorable insurance. Favorably insured patients were older with fewer non-white, more comorbidities, greater illness severity, and more likely transferred for care continuity. More unfavorably insured patients were designated as EMCs (90% vs 84%, p<0.01). In adjusted models, there was no association between unfavorable insurance and EMC transfer (OR 1.61, 0.98-2.69). Uninsured patients were more likely to be designated as EMCs (OR 2.27, 1.08-4.77)
Conclusions
The finding that uninsured patients were more likely to be designated as EMCs suggests non-clinical variation that may be mitigated by clearer definitions and increased inter-facility coordination to identify patients requiring transfer for emergency medical conditions.
Keywords: transfer, inter-hospital, insurance, emergency medical condition, uninsured, EMTALA
1. Introduction
Patient transfers between acute care hospitals comprise up to 30% of admissions to tertiary center acute care surgery services.[1] Transfers are typically performed to address a mismatch between patient needs and provider or facility capacities.[2] Recognition of the potential for patient selection by non-clinical factors such as ability to pay resulted in the creation of the Emergency Medical Treatment and Active Labor Act (EMTALA) in 1986, which mandated that capable facilities accept in transfer those patients presenting to an acute care facility emergency department whose needs exceed the capacity of the facility at which they are currently being treated.[3] Such patients are designated by referring providers as Emergency Medical Conditions (EMCs), and referral center acceptance is required by law.[4] There is currently no coordinated infrastructure to define patient needs and facility capacities for non-trauma emergency surgical patients. As a result, these need-capacity mismatches are determined by referring facility providers on a case-by-case basis rather than in a uniform fashion. This lack of standardization permits variability in selection of transfer patients on both clinical and non-clinical factors.
Existing literature suggests notable variation in transfer rates based on insurance status, but is limited in the ability to adjust for clinical factors such as severity of illness, and does not differentiate reasons for transfer.[5-14] Further, insurance status appears to be less influential in patient transfers from inpatient settings, to which EMTALA typically does not apply.[5] We suspect that EMC transfer designation is an important mechanism by which unfunded patients and those with unfavorable insurance are transferred at disproportionately higher rates as EMTALA-relevant cases. Therefore, we tested the hypothesis that unfavorably insured transfer patients are more likely to be designated as EMCs.
2. Materials and Methods
A retrospective cohort study was performed of patient transfers from a large referral network of acute care hospital emergency departments to Vanderbilt University Medical Center (VUMC) from January 1, 2009 through December 31, 2013. Adult patients admitted to the tertiary referral center's general surgery, thoracic surgery, urology, and vascular surgery services were included. Patients transferred from a non-acute care facility, including rehabilitation hospitals and long term acute care facilities, were excluded (2% of cohort). Because EMTALA does not apply to inpatient transfers, patients who were admitted to the referring facility prior to transfer were excluded. Those patients who were transferred to the referral center but not admitted were also excluded because it was not possible to determine whether the transfer was for care by one of the included surgical services. The study was approved by Vanderbilt University's Human Research Protection Program and Institutional Review Board.
Data were collected from the tertiary referral center's administrative records, patient electronic medical records, and referring facility documentation. All patients for whom transfer was requested were reviewed by VUMC's Access Center, which coordinates inter-hospital transfers for our facility. Information collected by VUMC Access Center from providers requesting transfer included patient insurance status, transfer diagnosis, reason for transfer, and whether the referring provider declared the transfer to be an Emergency Medical Condition (EMC) or non-EMC. Administrative records, including VUMC Access Center records, are maintained in the institution's Enterprise Data Warehouse (EDW), and include clinical and billing data for each patient encounter. Data obtained from referring facility records were abstracted via electronic medical records by a physician.
The primary exposure of patient insurance status was categorized as favorable or unfavorable using a previously published categorization scheme.[13, 12] Individuals insured by a commercial, Medicare, or federal (VA/Tricare) payer were defined as having favorable insurance. Unfavorable insurance included Medicaid and uninsured patients. Information on individual patient insurance status was ascertained from VUMC Access Center records, which reflected the insurance status reported by the referring provider. For transfers for which VUMC Access Center documentation of insurance status was not available (<1%), the insurance status documented in the referral center's billing records was used instead. The primary outcome measure was referring provider designation of the transfer as an EMC versus non-EMC transfer.
The analysis was performed at the level of the patient transfer. Transfers for patients with favorable insurance were compared to those with unfavorable insurance for the outcome of EMC designation, adjusting for relevant confounders. Patient comorbidity and severity of illness at the time of transfer were measured by calculating Elixhauser Comorbidity Scores and Acute Physiology Scores (APS) using previously published methods.[15, 16] Comorbidities were identified from the referral center's administrative records based on ICD-9 codes for the index admission. Acute Physiology Scores relied on the first set of laboratory tests and vital signs performed upon patient arrival to the referral center, as well as documentation of each patient's mental status on arrival according to the admitting service history and physical exam. Missing vital sign and basic laboratory values (3%) were coded as normal. Missing arterial blood gas values (76%) were also coded as normal, assuming that such tests would primarily be performed if there was clinical concern that they might be abnormal. This is consistent with assumptions made by the developers of the Acute Physiology Score in handling missing values.[16] Patients with unknown race were excluded in the primary analysis, but the effect of excluded patients was investigated in sensitivity analyses.
Descriptive statistics were used to compare patient and transfer characteristics by insurance status using chi-squared tests for categorical variables and student's t-test or Wilcoxon rank sum test for continuous variables, depending on their distributions. The unadjusted association between insurance status and transfer designation as EMC or non-EMC was evaluated using a chi-squared test. Other unadjusted bivariate comparisons between covariates and the primary outcome included chi-squared tests for categorical variables and simple logistic regression for continuous exposures. Referring hospitals were compared based on the volume of transfer patients each contributed to the sample divided into quartiles as very low volume (1-15 transfers/5 years), low (16-33), moderate (34-53), or high (54-149). A multivariable logistic regression model was created to estimate the association of insurance status with emergent transfer designation, adjusting for patient age, race, Elixhauser Comorbidity Score, Acute Physiology Score, admitting service, year of transfer request, reason for transfer, and whether each patient transfer was related to having undergone a prior procedure at the referral center.
In secondary analyses, patient insurance status was re-categorized as “uninsured” if the patient had no insurance and “insured” if the patient had any insurance, including Medicaid, and unadjusted and adjusted tests of association were performed. Finally, insurance types were included as separate variables in the model (Commercial, Medicare, Medicaid, and uninsured) and another adjusted model was created. Sensitivity analyses were performed for race and Acute Physiology Scores to assess the potential impact of missing data on the results. All models were adjusted to account for within subject correlation due to patients who had more than 1 eligible transfer during the study period (<7% of sample).
3. Results
The initial patient cohort included 2,221 patients who were admitted to an included surgical service at the tertiary referral center after transfer from another acute care hospital. Transfers for patients with admission at the referring hospital (888, 40%) and unknown race (38, 3%) were excluded, yielding a cohort of 1,295. The population was on average 56 ±17 years old, 53% male, 91% Caucasian. Eighty percent of the population had favorable insurance (Commercial 39%, Medicare 41%) while 20% had unfavorable insurance (Medicaid 9%, Uninsured 11%). Patients with favorable versus unfavorable insurance differed with respect to age, race, Elixhauser Comorbidity Scores, Acute Physiology Scores, reason for transfer, and whether a prior procedure has been performed at the referral center that was related to the transfer diagnosis (Table 1).
Table 1. Characteristics of Patient Transfers by Payer Status.
| Characteristic | Favorable Insurance N=1038 | Unfavorable Insurance N=257 | P-Value |
|---|---|---|---|
|
| |||
| Age (years, mean±SD) | 59±17 | 44±14 | <0.01 |
|
| |||
| Male Gender (N, %) | 547 (53) | 137 (53) | 0.86 |
|
| |||
| Non-White Race (N, %) | 82 (8) | 36 (14) | <0.01 |
|
| |||
| Elixhauser Comorbidity Score* (mean±SD) | 7.0±8.3 | 4.7±7.6 | <0.01 |
|
| |||
| Acute Physiology Score† (mean±SD) | 3.9±3.6 | 4.2±3.3 | 0.03 |
|
| |||
| Insurer (N, %) | |||
| Private/Commercial | 508 (49) | 0 (0) | <0.01 |
| Medicare | 530 (51) | 0 (0) | |
| Medicaid/State | 0 (0) | 118 (46) | |
| Uninsured/Self-pay | 0 (0) | 139 (54) | |
|
| |||
| Service (N, %) | |||
| General Surgery | 637 (61) | 157 (61) | 0.84 |
| Thoracic Surgery | 77 (7) | 23 (9) | |
| Vascular Surgery | 204 (20) | 47 (18) | |
| Urologic Surgery | 120 (12) | 30 (12) | |
|
| |||
| Year of Service (N, %) | |||
| 2009 | 216 (21) | 54 (21) | 0.28 |
| 2010 | 187 (18) | 54 (21) | |
| 2011 | 228 (22) | 41 (16) | |
| 2012 | 153 (15) | 42 (16) | |
| 2013 | 254 (24) | 66 (26) | |
|
| |||
| Reason for Transfer (N, %) | |||
| Higher Level of Care/Specialist | 585 (56) | 182 (71) | <0.01 |
| Continuity of Care | 397 (38) | 58 (23) | |
| Patient/Family Request | 43 (4) | 8 (3) | |
| Other | 13 (1) | 9 (4) | |
|
| |||
| Prior Related Procedure at Referral Center (N, %) | 322 (31) | 49 (19) | <0.01 |
|
| |||
| Referring Hospital Transfer Volume (N, %) | |||
| Very Low | 275 (26) | 54 (21) | 0.14 |
| Low | 250 (24) | 76 (30) | |
| Moderate | 270 (26) | 62 (24) | |
| High | 243 (23) | 65 (25) | |
Elixhauser Comorbidity Scores can range from -19 to + 89, with 0 being normal.
Acute Physiology Scores can range from 0 to 48, with 0 being normal.
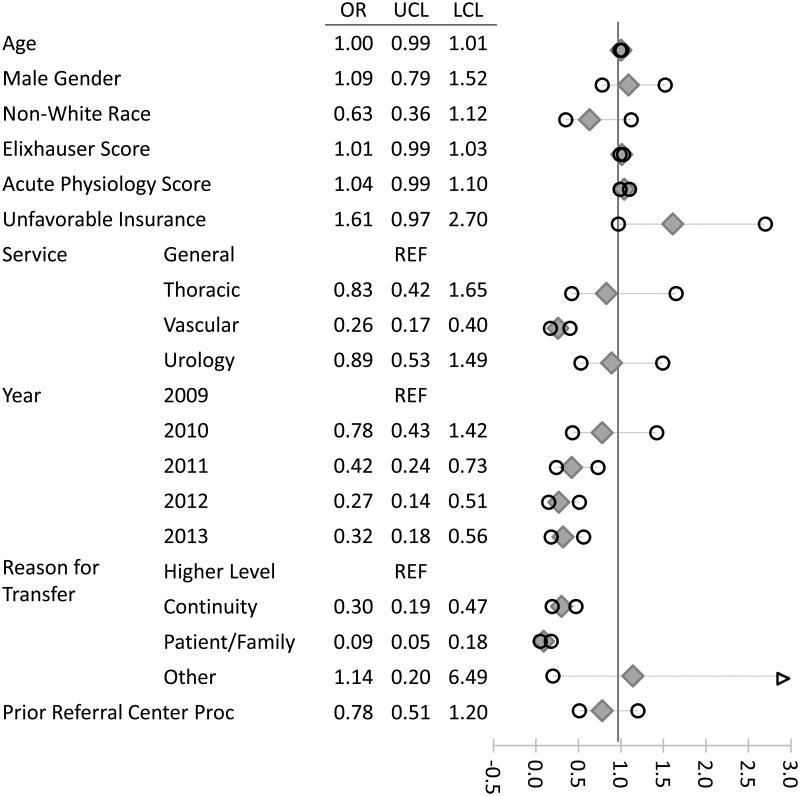
In unadjusted analyses, patients with unfavorable insurance were more likely to be designated by referring providers as EMC transfers (90% versus 84%, Unadjusted Odds Ratio (OR) 1.74, 95% Confidence Interval (CI) 1.12-2.72) (Table 2). After adjustment for relevant covariates, the observed association was not significant (Adjusted OR 1.61, 95% CI 0.98-2.69) (Table 3 and Figure 1). Transfers to the vascular surgery service, transfers performed in later years of the study, and transfers for continuity of care or patient/family request were less likely to be designated as EMC transfers. No factors were positively associated with emergent transfer designation in the adjusted model (Figure 1). Repeating the analysis with insurance status categorized as “uninsured” or “insured” demonstrated an association between lack of insurance and EMC transfer designation in both unadjusted (93% for uninsured versus 85% for insured, p<0.01) and adjusted analyses (OR 2.27, 95% CI 1.08-4.77) (Table 3). The additional model including each payer status as a separate category also demonstrated that uninsured patients, relative to commercially insured patients, were more likely to be designated as EMCs (OR 2.30, 95% CI 1.08-4.91), while there was no evidence of association between EMC designation and Medicare (OR 0.97, 95% CI 0.64-1.48) or Medicaid insurance (OR 1.16, 95% CI 0.60-2.22) (Table 3).
Table 2. Patient Transfer Characteristics by Emergency Medical Condition Designation.
| Characteristic | Non-EMC N=189 | EMC N=1,106 | Unadjusted Odds (95% CI) |
|---|---|---|---|
|
| |||
| Age (years, mean, SD) | 57±17 | 56±17 | 1.00 (0.99-1.01) |
|
| |||
| Male Gender (N, %) | 98 (52) | 586 (53) | 1.05 (0.77-1.43) |
|
| |||
| Non-White Race (N, %) | 20 (11) | 98 (9) | 0.82 (0.49-1.37) |
|
| |||
| Elixhauser Comorbidity Score (mean±SD) | 6.0±7.5 | 6.6±8.3 | 1.01 (0.99-1.03) |
|
| |||
| Acute Physiology Score (mean±SD) | 3.4±2.7 | 4.1±3.6 | 1.06 (1.01-1.11) |
|
| |||
| Unfavorable Insurance (N, %) | 25 (13) | 232 (21) | 1.74 (1.12-2.72) |
|
| |||
| Service (N, %) | |||
| General Surgery | 99 (52) | 695 (63) | REF |
| Thoracic Surgery | 11 (6) | 89 (8) | 1.15 (0.60-2.23) |
| Vascular Surgery | 59 (31) | 192 (17) | 0.46 (0.32-0.66) |
| Urologic Surgery | 20 (11) | 130 (12) | 0.93 (0.55-1.55) |
|
| |||
| Year of Service (N, %) | |||
| 2009 | 25 (13) | 245 (22) | REF |
| 2010 | 28 (15) | 213 (19) | 0.78 (0.44-1.37) |
| 2011 | 49 (26) | 220 (20) | 0.46 (0.27-0.77) |
| 2012 | 34 (18) | 161 (15) | 0.48 (0.28-0.84) |
| 2013 | 53 (28) | 267 (24) | 0.51 (0.31-0.85) |
|
| |||
| Reason for Transfer (N, %) | |||
| Higher Level of Care/Specialist | 78 (41) | 689 (62) | REF |
| Continuity of Care | 87 (46) | 368 (33) | 0.48 (0.34-0.67) |
| Patient/Family Request | 22 (12) | 29 (3) | 0.15 (0.08-0.27) |
| Other | 2 (1) | 20 (2) | 1.13 (0.26-4.93) |
|
| |||
| Prior Related Procedure at Referral Center (N, %) | 66 (34) | 305 (28) | 0.71 (0.51-0.98) |
|
| |||
| Referring Hospital Transfer Volume (N, %) | |||
| Very Low | 45 (24) | 284 (26) | REF |
| Low | 45 (24) | 281 (25) | 0.99 (0.63-1.54) |
| Moderate | 53 (28) | 279 (25) | 0.83 (0.54-1.28) |
| High | 46 (24) | 262 (24) | 0.90 (0.58-1.41) |
Table 3. Comparison of Multivariable Logistic Regression Models by Method of Payer Status Categorization.
| Model* | Adjusted Odds of EMC† Designation | 95% Confidence Interval | |
|---|---|---|---|
|
| |||
| Model 1 | |||
| Favorable Insurance | REF | REF | |
| Unfavorable Insurance | 1.61 | 0.98-2.69 | |
|
| |||
| Model 2 | |||
| Insured | REF | REF | |
| Uninsured | 2.27 | 1.084.77 | |
|
| |||
| Model 3 | |||
| Commercial | REF | REF | |
| Medicare | 0.97 | 0.64-1.48 | |
| Medicaid | 1.16 | 0.60-2.22 | |
| Uninsured | 2.30 | 1.08-4.91 | |
All models similarly adjusted for patient age, gender, race, Elixhauser Comorbidity Score, Acute Physiology Score, year, surgical service, reason for transfer, and any prior related procedure at the referral center
EMC = Emergency Medical Condition
Figure 1.
Adjusted odds of Emergency Medical Condition (EMC) designation for patient transfers to a tertiary referral center emergency surgical service from 2009-2013. OR=odds ratio, LCL=lower confidence limit, UCL=upper confidence limit
Inclusion of patients with unknown race did not alter the results of the multivariable logistic regression model. Replacement of patient transfers of unknown race in either the “white” or “nonwhite” categories also did not impact observed associations in the adjusted model. Finally, models excluding Acute Physiology Scores, but still including Elixhauser Comorbidity Scores for risk adjustment, did not alter the findings.
4. Discussion
In risk-adjusted analyses of patient transfers from acute care facilities to a tertiary referral center for acute surgical care, uninsured patients were more likely to be designated as Emergency Medical Condition transfers for which tertiary center acceptance was compulsory. Findings for patients insured by Medicaid were not significant. In the absence of clear guidelines for appropriateness of EMC designation, this suggests the influence of a non-clinical factor, patient payer, in the EMC designation of patient transfers.
This finding may elucidate a mechanism by which insurance-related disparities in transfer patient selection and processes have been observed in other populations. Most prior work addresses differences in payer mix for patients who are transferred from versus admitted to the facilities at which they initially present. An assessment of payer mix among patient transfers for medical and surgical disease categories with highest rates of transfer using the National Emergency Department Sample (NEDS) demonstrated that uninsured patients and those insured by Medicaid were more likely to be transferred than patients insured by private payers or Medicare. Of note, these estimates were adjusted for comorbidity burden of the population, but not for acute illness severity.[8] A similar study specific to major trauma patients who initially presented to non-trauma emergency departments found that after adjustment for mechanism of injury and injury severity score, uninsured patients were more likely to be transferred to a trauma center whereas insured patients were more likely to be admitted to the non-trauma center.[6] This finding among trauma transfers was corroborated by evaluations of payer mix among head-injured patients using the National Trauma Data Bank (NTDB) and regional studies of trauma patients.[14, 17] Associations between transfer and less favorable insurance have also been demonstrated in general patient populations using the National Hospital Ambulatory Medical Care Survey (NHAMCS) and in patients with vascular emergencies.[18, 7] We are aware of a single study that found no difference in payer mix among transferred trauma patients relative to non-transferred patients using the general NTDB population.[19]
Other studies address payer mix variation among referral centers that receive patients in transfer relative to patients who are directly admitted to those facilities, and have yielded varying results. In general, more transfer patients have favorable payers than unfavorable payers, which reflects the distribution of health insurance in the general population.[13, 20] However, the underlying demographics of each referral center's proximate population may influence whether transferred patients worsen or improve an individual hospital's payer mix. While in some cases accepting transfer patients results in a greater proportion of patients without insurance or with Medicaid,[9, 10] in other cases inter-hospital transfer does not alter or even improves a facility's payer mix.[11, 21, 22]
To our knowledge, this study is the first to evaluate the association of insurance status with EMC transfer designation. We tested the hypothesis that EMC transfer designation is a mechanism by which patients with unfavorable insurance are transferred at disproportionately higher rates. Our finding that uninsured patients were more likely to be designated as EMCs in a risk-adjusted model supports this; however, we did not observe a significant association between Medicaid insurance and EMC designation.
The finding that uninsured patients were more likely to be designated as EMC transfers could have increasingly important implications for tertiary referral centers. Prior work suggests that transfer patients pose greater financial risk to accepting hospitals.[23] Recent changes in payer mix and planned reductions in federal subsidization of many referral centers under the Patient Protection and Affordable Care Act (PPACA) could increase the financial liability of some referral centers. The PPACA included planned reductions, now scheduled for 2017, in disproportionate share payments to hospitals that provide high volumes of uncompensated care with the expectation that patients who previously received uncompensated care would become insured through Medicaid or a commercial payer through the health insurance exchange. The fiscal impact is expected to be greatest in those states that elected not to expand Medicaid, which are projected to receive diminished funding for uncompensated care despite little to no change in the proportion of uninsured patients for whom care is provided.[24]
If transfer differentially selects unfavorably insured patients, tertiary referral hospitals may face greater financial risk in an already strained healthcare system. It is also understandable that smaller referring hospitals, with operating margins that can be very narrow, may be unable to care for unfavorably or uninsured patients even if these hospitals have clinical support and capabilities to do so. This tension between referring and accepting facilities needs to be addressed to prevent fragmented and suboptimal patient care. Patient selection for transfer might be improved through mutually-developed standards that remain sensitive to individual situations.
The adjusted model also illustrates a temporal decline in EMC designations during the three most recent years of the study relative to the first two years. The reason for this is unclear, but could reflect improved relationships between centers requesting transfer and the tertiary referral center of study. An affiliated network of hospitals was formed during the study period, which may be associated with increased inter-hospital coordination and mutually beneficial transfer arrangements. If this trend is widespread, it could mitigate projected financial hardships to referral centers while improving inter-facility transitions for patients.
This study reflects the experience of a single referral network in the Southeast, which may not be generalizable to other regions. The racial distribution of this population is not representative of the general population. Additionally, the payer mix represented in this cohort includes fewer patients with commercial insurance and more patients covered by Medicare than national averages, which reflects the higher mean age of the population. The proportion of patients with no insurance is lower than national averages (9% versus 15%).[20] Insurance status was defined based on the requesting provider's report to the referral hospital Vanderbilt Access Center, which was perceived as most relevant given the same entity designated the transfer as EMC or non-EMC. It is not known whether referring facilities or individual referring providers were aware of patient payer status when making transfer designations. If referring facilities were not aware of payer status, this suggests that the observed increase in EMC-designations for uninsured patients may be attributed to other unmeasured variables that correlate with payer status.
Another limitation is our inability to capture all laboratory and vital sign values comprising each patient's Acute Physiology Score, which reflects severity of illness. The majority of missing data were arterial blood gas values. Under the assumptions that data are missing because the test was not performed, and that it would only be performed for critically ill patients, we coded these values as normal to calculate the composite scores. However, we acknowledge that data could be missing for other unknown reasons, which could skew the results.
The categorization scheme for favorably versus unfavorably insured patients was based on prior work. We recognize that from the standpoint of financial incentives, profit margins are greatest for privately insured patients, followed by Medicare, then Medicaid. Knowing that under the PPACA, more uninsured patients are becoming insured by Medicaid, we believed our conclusions would have greater relevance if these two categories were combined in the primary analysis.
Patients who were transferred but not admitted to our referral center are not captured in this cohort. Based on our institution's records, this occurs in approximately 10% of transfers. Given the high volume of transfers to the study institution (approximately 8000 per year) and variation in how service-specific documentation is catalogued in the electronic medical record, we were not able to determine what proportion of this non-admitted population was transferred for care by an included surgical service, but we suspect rates are lower for surgical services than non-surgical services based on clinical experience. We do not expect such patients to be different from admitted patients with respect to payer status; however it is certainly possible that insurance-related disparities exist at the level of the receiving facility emergency department in selecting which transfer patients are admitted to the tertiary center and which are discharged from the emergency department.
Similarly, we are unable to comment on how transfer diagnoses from referring facility providers compared with final diagnoses made at the referral center or on the clinical appropriateness of Emergency Medical Condition designation. The relationship between insurance status and EMC designation could be further evaluated in a prospective fashion using pre-defined criteria for emergent conditions and real-time collection of insurance data from referral center billing records.
5. Conclusions
Uninsured surgical patients were more likely to be designated as EMCs by transferring facilities, for which tertiary referral center acceptance was mandatory under EMTALA. No effect was observed for patients insured by Medicaid. This non-clinical variation may impact referral center finances and transfer patient care, and may be improved through collaboratively-defined transfer indications and improved coordination between centers requesting and receiving patients in transfer for acute surgical care.
Acknowledgments
The authors would like to thank Drs. William Nealon, MD and Richard Pierce, MD, PhD for their thoughtful review and feedback on the manuscript.
Dr. Kummerow's salary is supported by the Office of Academic Affiliations (OAA), Department of Veterans Affairs, VA National Quality Scholars Program. She used facilities at VA Tennessee Valley Healthcare System, Nashville Tennessee. The funding organization was not involved in study design, data collection, analysis, or interpretation, writing of the manuscript, or the decision to submit the article for publication.
This study used Vanderbilt University REDCap, which is supported by grant UL1 TR000445 from NCATS/NIH.
Footnotes
Drs. Kummerow, Hayes, Ehrenfeld, Holzman, Sharp, and Kripalani, and Mrs. Phillips have no conflicts of interest to disclose. Dr. Poulose received research support from Bard-Davol and is a consultant to Ariste Medical.
Author contributions: Conception and design – All authors
Acquisition and interpretation of data – Kummerow Broman, Phillips, Hayes, Ehrenfeld, Poulose
Drafting of the manuscript – Kummerow Broman, Poulose
Critical revision of the manuscript for important intellectual content – All authors
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Kristy Kummerow Broman, Email: kristy.l.kummerow@vanderbilt.edu.
Sharon Phillips, Email: sharon.phillips@vanderbilt.edu.
Rachel M. Hayes, Email: rachel.m.hayes@vanderbilt.edu.
Jesse M. Ehrenfeld, Email: jesse.ehrenfeld@vanderbilt.edu.
Michael D. Holzman, Email: mike.holzman@vanderbilt.edu.
Kenneth Sharp, Email: ken.sharp@vanderbilt.edu.
Sunil Kripalani, Email: sunil.kripalani@vanderbilt.edu.
Benjamin K. Poulose, Email: Benjamin.poulose@vanderbilt.edu.
References
- 1.Santry HP, Janjua S, Chang Y, Petrovick L, Velmahos GC. Interhospital transfers of acute care surgery patients: should care for nontraumatic surgical emergencies be regionalized? World Journal of Surgery. 2011;35(12):2660–7. doi: 10.1007/s00268-011-1292-3. [DOI] [PubMed] [Google Scholar]
- 2.Iwashyna TJ. The incomplete infrastructure for interhospital patient transfer. Critical Care Medicine. 2012;40(8):2470–8. doi: 10.1097/CCM.0b013e318254516f. [DOI] [PubMed] [Google Scholar]
- 3.Testa PA, Gang M. Triage, EMTALA, consultations, and prehospital medical control. Emergency Medicine Clinics of North America. 2009;27(4):627–40. viii–ix. doi: 10.1016/j.emc.2009.07.011. [DOI] [PubMed] [Google Scholar]
- 4.Bitterman RA. Transferring and Accepting Patients under EMTALA. In: Aghababian R, editor. Essentials of Emergency Medicine. Third. Burlington, MA: Jones and Bartlett; 2010. [Google Scholar]
- 5.Hanmer J, Lu X, Rosenthal GE, Cram P. Insurance status and the transfer of hospitalized patients: an observational study. Annals of Internal Medicine. 2014;160(2):81–90. doi: 10.7326/M12-1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Delgado MK, Yokell MA, Staudenmayer KL, Spain DA, Hernandez-Boussard T, Wang NE. Factors associated with the disposition of severely injured patients initially seen at non-trauma center emergency departments: disparities by insurance status. JAMA Surgery. 2014;149(5):422–30. doi: 10.1001/jamasurg.2013.4398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mell MW, Wang NE, Morrison DE, Hernandez-Boussard T. Interfacility transfer and mortality for patients with ruptured abdominal aortic aneurysm. Journal of Vascular Surgery. 2014;60(3):553–7. doi: 10.1016/j.jvs.2014.02.061. [DOI] [PubMed] [Google Scholar]
- 8.Kindermann DR, Mutter RL, Cartwright-Smith L, Rosenbaum S, Pines JM. Admit or transfer? The role of insurance in high-transfer-rate medical conditions in the emergency department. Annals of Emergency Medicine. 2014;63(5):561–71 e8. doi: 10.1016/j.annemergmed.2013.11.019. [DOI] [PubMed] [Google Scholar]
- 9.Kamath AF, Austin DC, Derman PB, Israelite CL. Transfer of hip arthroplasty patients leads to increased cost and resource utilization in the receiving hospital. The Journal of Arthroplasty. 2013;28(9):1687–92. doi: 10.1016/j.arth.2013.07.009. [DOI] [PubMed] [Google Scholar]
- 10.Eberlin KR, Hartzell TL, Kuo P, Winograd J, Day C. Patients transferred for emergency upper extremity evaluation: does insurance status matter? Plastic and Reconstructive Surgery. 2013;131(3):593–600. doi: 10.1097/PRS.0b013e31827c6e82. [DOI] [PubMed] [Google Scholar]
- 11.Nahm NJ, Patterson BM, Vallier HA. The impact of injury severity and transfer status on reimbursement for care of femur fractures. The Journal of Trauma and Acute Care Surgery. 2012;73(4):957–65. doi: 10.1097/TA.0b013e31825a7723. [DOI] [PubMed] [Google Scholar]
- 12.Kao DP, Martin MH, Das AK, Ruoss SJ. Consequences of federal patient transfer regulations: effect of the 2003 EMTALA revision on a tertiary referral center and evidence of possible misuse. Archives of Internal Medicine. 2012;172(11):891–2. doi: 10.1001/archinternmed.2012.1290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Green A, Showstack J, Rennie D, Goldman L. The relationship of insurance status, hospital ownership, and teaching status with interhospital transfers in California in 2000. Academic Medicine: Journal of the Association of American Medical Colleges. 2005;80(8):774–9. doi: 10.1097/00001888-200508000-00015. [DOI] [PubMed] [Google Scholar]
- 14.Nathens AB, Maier RV, Copass MK, Jurkovich GJ. Payer status: the unspoken triage criterion. The Journal of Trauma. 2001;50(5):776–83. doi: 10.1097/00005373-200105000-00002. [DOI] [PubMed] [Google Scholar]
- 15.van Walraven C, Austin PC, Jennings A, Quan H, Forster AJ. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Medical Care. 2009;47(6):626–33. doi: 10.1097/MLR.0b013e31819432e5. [DOI] [PubMed] [Google Scholar]
- 16.Knaus WA, Zimmerman JE, Wagner DP, Draper EA, Lawrence DE. APACHE-acute physiology and chronic health evaluation: a physiologically based classification system. Critical Care Medicine. 1981;9(8):591–7. doi: 10.1097/00003246-198108000-00008. [DOI] [PubMed] [Google Scholar]
- 17.Babu MA, Nahed BV, Demoya MA, Curry WT. Is trauma transfer influenced by factors other than medical need? An examination of insurance status and transfer in patients with mild head injury. Neurosurgery. 2011;69(3):659–67. doi: 10.1227/NEU.0b013e31821bc667. discussion 67. [DOI] [PubMed] [Google Scholar]
- 18.Nacht J, Macht M, Ginde AA. Interhospital transfers from U.S. emergency departments: implications for resource utilization, patient safety, and regionalization. Academic Emergency Medicine: Official Journal of the Society for Academic Emergency Medicine. 2013;20(9):888–93. doi: 10.1111/acem.12209. [DOI] [PubMed] [Google Scholar]
- 19.Parks J, Gentilello LM, Shafi S. Financial triage in transfer of trauma patients: a myth or a reality? American Journal of Surgery. 2009;198(3):e35–8. doi: 10.1016/j.amjsurg.2009.01.012. [DOI] [PubMed] [Google Scholar]
- 20.American Community Survey. [Accessed December 20, 2014 2014];Health Insurance Coverage Status. 2013 http://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_13_1YR_S2701&prodType=table.
- 21.Melkun ET, Ford C, Brundage SI, Spain DA, Chang J. Demographic and Financial Analysis of EMTALA Hand Patient Transfers. Hand. 2010;5(1):72–6. doi: 10.1007/s11552-009-9214-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Spain DA, Bellino M, Kopelman A, Chang J, Park J, Gregg DL, et al. Requests for 692 transfers to an academic level I trauma center: implications of the emergency medical treatment and active labor act. The Journal of Trauma. 2007;62(1):63–7. doi: 10.1097/TA.0b013e31802d9716. discussion 7-8. [DOI] [PubMed] [Google Scholar]
- 23.Pietz K, Byrne MM, Daw C, Petersen LA. The effect of referral and transfer patients on hospital funding in a capitated health care delivery system. Medical Care. 2007;45(10):951–8. doi: 10.1097/MLR.0b013e31812f4f48. [DOI] [PubMed] [Google Scholar]
- 24.Graves JA. Medicaid expansion opt-outs and uncompensated care. The New England Journal of Medicine. 2012;367(25):2365–7. doi: 10.1056/NEJMp1209450. [DOI] [PubMed] [Google Scholar]