Abstract
Objectives
To quantify absorption coefficients of specific fatty acids in preterm infants as a function of diet, formula (F) or breast milk (BM), and postnatal age; and, to identify the fatty acid structural characteristics that determine optimal fatty acid absorption.
Methods
Fatty acids from dietary and fecal samples were extracted and quantified by gas chromatography-mass spectroscopy. Fatty acid absorption coefficients (FA-CFAs) were calculated by comparing the total amount of fatty acids supplied by the diet to the amount quantified in the total fecal output over a 3-day period.
Results
18 infants (BM=8; F=10) were studied at 2 weeks of age and 20 infants (BM=10; F=10) were studied at 6 weeks of age. FA-CFAs decreased with increasing carbon length in formula-fed infants at 2 and 6 weeks. Results were similar, but less in magnitude in breast milk-fed infants at 2 weeks with no difference at 6 weeks.
Conclusions
Preterm infants fed formula demonstrated lower FA-CFAs as a function of increasing carbon length. This is consistent with limited pancreatic lipase production and with lipase being present in breast milk but not in formula. The fact that this pattern was seen in BM-fed infants at 2 weeks but not 6 weeks of age suggests that intestinal immaturity may also play a role in impaired fatty acid absorption. These data highlight principles that need to be considered to optimize delivery and absorption of dietary LCPUFAs in preterm infants.
Keywords: fatty acid, docosahexaenoic acid, arachidonic acid, term infant, preterm infant nutrition, breast milk, formula, stool, fat digestion, coefficient of fat absorption
INTRODUCTION
Long chain polyunsaturated fatty acids (LCPUFAs) are critical for fetal development with transfer of these immunonutrients occurring predominantly in the last trimester. Moderately to extremely preterm infants miss much of the last trimester; and, as a result, are unable to adequately store LCPUFAs and are completely reliant on the supplied diet to maintain circulating and tissue levels of fatty acids.
Preterm infants are initially provided parenteral nutrition, which is steadily decreased as enteral nutrition is slowly advanced. Thus, nutritional requirements must be adequately provided reliably intravenously and enterally. Both routes represent a challenge in fatty acid delivery. In the first postnatal week docosahexaenoic acid (DHA) and arachidonic acid (AA) levels rapidly fall when preterm infants are predominantly dependent on parenteral nutrition.1 This is largely due to the use of a soybean based lipid emulsion (IntraLipid®), which provides the essential precursor fatty acids linoleic and linolenic acid but no AA or DHA. The enteral phase of nutrition is complicated by immaturity of the intestine and pancreas.
Throughout the first year of life newborns exhibit exocrine pancreatic insufficiency. During early infancy, the pancreas produces proteases to digest proteins, but secrete inadequate amounts of amylase and lipase, enzymes required to digest and absorb carbohydrates and fats, respectively. Early exocrine pancreatic insufficiency is based on studies by Lebenthal and Lee where pancreatic enzyme activity and secretagogue responses were studied in term infants at birth, one month of age, and 2 years of age or older.2 Although trypsin levels were found to be similar across the age ranges, lipase and amylase activity was not detectable at birth and one month of age. While gastric lipase output in preterm neonates has been shown to be comparable to that of adults, and aids in digestion of fats at the sn-1 and -3 positions, it only accounts for upwards of 10% of total fat digestion.3,4 Lipase is found in human breast milk at high concentrations at all stages of lactation and is largely responsible for compensating for the transient pancreatic insufficiency seen in newborns.5 Therefore, breast milk-fed infants are provided with the enzymes necessary to digest and absorb fats. In contrast, infant formula does not contain these enzymes and would be predicted to lead to steatorrhea, with malabsorption of fats and critical fatty acids.
The objective of this study was to (1) quantify in very low birth weight preterm infants absorption coefficients of specific fatty acids as a function of diet and postnatal age and (2) identify the clinical and fatty acid structural characteristics that determined optimal fatty acid absorption.
METHODS
Population sample and Cohort selection
In this retrospective cohort study, infants were selected from a cohort of premature infants less than 33 weeks of gestation enrolled in the Infant Health Research Program at Beth Israel Deaconess Medical Center, Boston, an ongoing recruitment of premature infants with collection of discarded biological samples to evaluate the impact of nutrition on health and disease. Breast milk and fecal samples were collected when available. The Institutional Review Board approved the collection of discarded specimens as well as the analyses conducted for this study (protocol numbers: 2009P-000014 and 2009P-000193). Verbal informed consent was obtained from the parents of infants enrolled in this study. Infants were selected for this study if they were receiving full enteral feedings at two and six postnatal weeks of age, were exclusively breast milk-fed or formula-fed, and if a complete 3-day block of nutritional intake with dietary and fecal samples were collected and available for analysis. All data were anonymized and de-identified for study analysis.
Data and sample collection
Infant data abstracted from the electronic medical record included gestational age, sex, birth weight, weight at entry into the study (at 2 weeks or 6 weeks postnatal age), and the clinical outcomes of bronchopulmonary dysplasia (BPD), sepsis, and necrotizing enterocolitis (NEC). BPD was defined as requiring oxygen at 36 weeks postnatal age. Sepsis was diagnosed has having a positive blood culture during any time point while in the neonatal intensive care unit. NEC was defined as having documented pneumatosis on an abdominal radiograph. In addition, complete nutritional information was collected from the electronic medical record and included diet, total number of feedings, and total volume of enteral diet per day. All breast milk samples represented mother’s own milk. Donor milk was not being used at the time of this study. A sample of breast milk was collected at the time of every feeding for three full days. At the end of each feeding, the bedside nurse placed the infusion tubing with residual breast milk in a 4°C refrigerator. After each 24 hour collection, the breast milk samples were pooled, aliquoted, and stored in a −80°C freezer until analysis. This was repeated for three consecutive days. Similarly, every diaper for each infant was collected for three complete days and stored in a 4°C refrigerator. After each 24 hour collection the fecal samples were pooled, weighed, aliquoted, and stored in a −80°C freezer until analysis.
Determination of fatty acids in breast milk and formula
100 μl of either breast milk or formula was added to 0.4 ml of phosphate buffered saline solution and 30 μg of heptadecanoic acid to serve as the internal standard. Fatty acids from breast milk and infant formula preparations were isolated and methylated using a modified Folch method as described previously.6 After the lipid extraction, the sample was quantified by gas chromatography-mass spectroscopy (GC-MS) using a Hewlett-Packard Series II 5890 chromatograph coupled to a HP-5971 mass spectrometer equipped with a Supelcowax SP-10 capillary column.
Determination of fatty acids in fecal samples
Portions of the frozen fecal samples, weighing between 50 – 100 mg were thawed on ice and weight recorded. While vortexing, 0.5 ml of phosphate buffered saline was slowly added to the stool. The sample was then vortexed for an additional minute. The entire preparation was extracted as described above for breast milk and formula specimens. In order to correct for the true mass of the fecal sample, taking into consideration the varying water content of each infant’s sample, a separate aliquot of frozen stool (50–100mg) was thawed, weighed, and then dried in 95°C oven for approximately 40 hours. The sample was then re-weighed and from these weight differences a wet/dry ratio was calculated. This ratio was applied to the recorded weight of the sample used for the fatty acid extraction and subsequent GC-MS quantification in order to express each fatty acid on an nmol fatty acid per gram dry weight of stool basis.
GC-MS FAME identification and quantification
Peak identification was based upon comparison of both retention time and mass spectra of the unknown peak to that of known standards within the GC-MS database library. FAME mass was determined by comparing areas of unknown FAMEs to that of a fixed concentration of 17:0 internal standard. Response factors were determined for each individual FAME to correct for GC-MS total ion chromatograph discrepancies in quantification. These factors were determined through the use of a GLC reference standard which contained known masses of FAMEs ranging from C8–C24. The response ratio of each FAME is corrected to a fixed amount ratio for each FAME relative to 17:0.
Calculation of coefficient of fat absorption and coefficient of fatty acid absorption
The coefficient of total fat absorption (CFA) was calculated as follows: [(Total fat intake − Total fat output)/Total fat intake] × 100 = % absorption. The coefficient of absorption of individual fatty acids (FA-CFA) was similarly calculated with the specific fatty acid replacing total fat.
Statistical Analysis
Continuous variables with normal distribution are expressed as mean ± standard deviation (SD). CFA values were expressed as a percentage. The Wilcoxon ranksum test assuming nonparametric data was used to compare each specific fatty acid CFA value between the breast milk-fed and formula-fed groups. Multiple fatty acid CFA comparisons across carbon length between the two groups were performed using the Kruskal-Wallis nonparametric test. All analyses were performed using STATA statistical software, version 13 (StataCorp) and GraphPad Prism version 6.00 for Windows, GraphPad Software (San Diego, CA, www.graphpad.com).
Results
Clinical characteristics
At two weeks postnatal age, 18 premature infants (BM=8; Formula=10) on full enteral feedings were studied (Table 1). Males comprised one-half of each cohort. No significant differences were noted in gestational age, birth weight, and weight at time of study. At 6 weeks postnatal age, 20 premature infants (BM=10; Formula=10) were studied. As in the earlier time point, no differences between the groups were observed for gestational age, birth weight, and weight at time of study. In addition, no differences were noted in the clinical outcomes. No infant in either group or time period was identified as having NEC. In week 2, 1 infant had BPD in the breast milk fed group and 1 infant had BPD in the formula fed group. In week 6, 2 infants had BPD in the breast milk fed group and 3 infants BPD in the formula fed group. No infant had sepsis at 2 weeks, and none had sepsis in the formula group at 6 weeks. Two infants had sepsis in the breast milk fed group at 6 weeks.
Table 1.
Clinical Characteristics
| Age, Weeks | ||||
|---|---|---|---|---|
| 2 | 6 | |||
| BM (n=8) |
Formula (n=10) |
BM (n=10) |
Formula (n=10) |
|
| Characteristic | ||||
| Gender, male, n (%) | 4 (50) | 5 (50) | 6 (60) | 4 (40) |
| Gestational Age, week (mean ±SD) | 30.3 ± 2.1 | 29.8 ± 2.6 | 28.0 ± 2.5 | 28.0 ± 2.4 |
| Birth weight, grams (mean ±SD) | 1358 ± 233 | 1402 ± 488 | 1104 ± 300 | 1053 ± 425 |
| Weight at time of study, grams (mean ±SD) | 1373 ± 245 | 1440 ± 532 | 1815 ± 480 | 1777 ± 666 |
BM = Breast Milk
Dietary intakes, fecal output, and fat-balance data in preterm infants fed breast milk or formula
Dietary intake, fecal output, total fat intake, total fat output, and coefficient of total fat absorption (CFA) were not statistically different between breast milk-fed and formula-fed infants at 2 weeks postnatal age (Table 2). At 6 weeks, formula-fed infants’ demonstrated greater total fat intake and fat output. Despite this, there was no difference in the total CFA between the two groups.
Table 2.
Dietary intakes, fecal output, and fat-balance data in preterm infants fed breast milk or formula
| 2 Weeks | p | 6 Weeks | p | |||
|---|---|---|---|---|---|---|
| Breast Milk (n=8) |
Formula (n=10) |
Breast Milk (n=10) |
Formula (n=10) |
|||
| Dietary intake (mL/kg/d) | 130 ± 38 | 144 ± 21 | 0.4 | 145 ± 15 | 149 ± 5 | 0.5 |
| Fecal output (g/kg/d) | 2.9 ± 1.6 | 4.4 ± 2.4 | 0.2 | 2.9 ± 2.0 | 4.3 ± 2.5 | 0.2 |
| Fat intake (nmol × 105/kg/d) | 181 ± 38 | 184 ± 43 | 0.8 | 127 ± 27.4 | 193 ± 32.9 | 0.0001 |
| Fat output (nmol × 105/kg/d) | 5.6 ± 3.5 | 7.0 ± 4.2 | 0.5 | 2.6 ± 2.8 | 6.9 ± 4.9 | 0.03 |
| Coefficient of total fat absorption (CFA, %) | 97.2 (96.0–98.1) | 96.0 (94.9–98.3) | 0.5 | 98.7 (97.2–99.1) | 96.2 (95.0–98.3) | 0.2 |
CFA of specific fatty acids (FA-CFAs)
Although the total CFA was not different between breast milk-fed and formula-fed infants at both 2 and 6 weeks of age, the coefficient of specific fatty acid absorptions for some of the individual fatty acids did reveal differences between groups across both time periods (Table 3). The absorption coefficient for the essential fatty acids, linoleic acid and alpha-linolenic acid, did not differ significantly between the two groups during either time period. For both groups and both time periods, the absorption of these two essential fatty acids were greater than 95%. With respect to the critical fatty acid DHA, there was a difference in the absorption between formula-fed and breast milk-fed infants, with formula-fed infants less efficient at 2 and 6 weeks (83.4 vs. 96.2% and 74.9 vs. 97.4%, respectively).
Table 3.
Summary of absorption coefficients for all fatty acids
| 2 Weeks | 6 Weeks | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Breast Milk | Formula | Breast Milk | Formula | ||||||
| Saturated | |||||||||
| 12:0 | Lauric acid | 99.5 (98.3–99.7) | 98.9 (98.6–99.2) | 0.37 | 99.5 (97.8–99.8) | 97.4 (96.2–99.2) | 0.11 | ||
| 14:0 | Myristic acid | 98.2 (95.3–98.9) | 94.4 (93.7–95.7) | 0.03 | 98.5 (94.7–98.9) | 94.0 (90.2–96.9) | 0.04 | ||
| 15:0 | Pentadecanoic acid | 96.4 (94.1–98.1) | 92.8 (86.5–94.5) | 0.03 | 98.3 (95.6–98.9) | 91.9 (83.1–94.9) | 0.01 | ||
| 16:0 | Palmitic acid | 96.2 (93.1–97.3) | 87.9 (85.9–93.3) | 0.006 | 97.5 (95.3–98.3) | 93.5 (87.2–94.6) | 0.005 | ||
| 18:0 | Stearic acid | 91.3 (88.2–93.6) | 66.4 (50.9–84.5) | 0.003 | 96.8 (89.3–97.3) | 76.8 (71.1–90.3) | 0.003 | ||
| 20:0 | Arachidic acid | 88.5 (84.5–90.4) | 73.3 (65.6–81.3) | 0.01 | 91.7 (85.8–95.6) | 84.3 (74.7–87.0) | 0.03 | ||
| 22:0 | Behenic acid | 85.4 (82.3–89.1) | 61.8 (45.1–73.2) | 0.01 | 93.1 (87.0–97.1) | 75.6 (71.0–83.5) | 0.005 | ||
| n-6 | |||||||||
| 18:2n-6 | Linoleic acid | 98.3 (94.9–99.3) | 96.3 (94.3–97.6) | 0.29 | 99.1 (97.6–99.5) | 95.1 (93.8–99.0) | 0.11 | ||
| 18:3n-6 | Gamma-linolenic acid | 99.0 (96.4–99.9) | 97.8 (95.3–99.3) | 0.42 | 99.9 (99.6–100) | 94.4 (88.8–99.0) | 0.09 | ||
| 20:2n-6 | Eicosadienoic acid | 93.5 (85.6–94.8) | 80.5 (55.2–87.0) | 0.03 | 97.4 (91.0–98.2) | 81.3 (42.5–93.9) | 0.003 | ||
| 20:3n-6 | Dihomo-gamma-linolenic acid | 95.4 (90.8–98.2) | 90.9 (78.2–94.9) | 0.29 | 98.1 (95.5–98.8) | 81.4 (75.3–94.8) | 0.007 | ||
| 20:4n-6 | Arachidonic acid | 96.2 (90.5–98.6) | 91.0 (80.0–94.6) | 0.13 | 85.8 (70.2–93.3) | 87.9 (72.9–96.3) | 0.65 | ||
| 22:4n-6 | Adrenic acid | 92.9 (87.5–95.8) | 77.6 (69.9–98.0) | 0.15 | 97.7 (92.7–98.7) | 89.3 (40.7–100.0) | 0.65 | ||
| n-3 | |||||||||
| 18:3n-3 | α-Linolenic acid | 98.8 (95.5–99.7) | 97.7 (95.8–98.3) | 0.29 | 99.5 (98.1–99.6) | 95.3 (88.8–99.3) | 0.08 | ||
| 22:6n-3 | Docosahexaenoic acid | 95.8 (92.8–97.9) | 84.2 (66.9–92.4) | 0.01 | 98.2 (89.1–98.6) | 74.9 (35.6–85.8) | 0.003 | ||
| n-9 | |||||||||
| 16:1n-9 | Palmitoleic acid | 97.9 (95.1–99.2) | 93.2 (88.7–95.5) | 0.02 | 99.3 (97.2–99.6) | 91.2 (86.7–97.6) | 0.02 | ||
| 18:1n-9 | Oleic acid | 96.7 (92.8–98.3) | 95.9 (94.5–96.5) | 0.53 | 98.5 (97.1–98.6) | 96.8 (91.8–98.8) | 0.26 | ||
| 20:1n-9 | Eicosenoic | 90.7 (80.4–92.3) | 84.3 (80.8–89.8) | 0.21 | 96.6 (86.3–97.4) | 76.9 (73.2–93.8) | 0.01 | ||
| Total Saturated vs. Unsaturated | |||||||||
| Saturated | 95.0 (92.9–96.3) | 84.2 (81.1–89.7) | 0.005 | 97.1 (94.5–98.4) | 91.3 (82.8–91.8) | 0.005 | |||
| Unsaturated | 96.1 (90.9–97.5) | 89.9 (75.9–92.4) | 0.06 | 97.3 (91.4–98.3) | 87.3 (73.7–91.9) | 0.06 | |||
| Carbon Length | |||||||||
| 12 | 99.5 (98.3–99.7) | 98.9 (98.6–99.2) | 0.37 | 99.5 (97.8–99.8) | 97.4 (96.2–99.2) | 0.11 | |||
| 14 | 98.2 (95.3–98.9) | 94.4 (93.7–95.7) | 0.03 | 98.5 (94.7–98.9) | 94.0 (90.2–96.9) | 0.04 | |||
| 15 | 96.4 (94.1–98.1) | 92.8 (86.5–94.5) | 0.03 | 98.3 (95.6–98.9) | 91.9 (83.1–94.9) | 0.01 | |||
| 16 | 97.1 (94.0–98.2) | 90.6 (84.1–94.2) | 0.008 | 98.4 (96.2–98.9) | 92.7 (86.8–95.6) | 0.01 | |||
| 18 | 97.0 (93.0–98.0) | 87.6 (86.1–95.8) | 0.01 | 98.4 (96.1–99.0) | 91.5 (83.0–93.9) | 0.02 | |||
| 20 | 93.3 (85.4–94.6) | 84.2 (74.8–88.5) | 0.04 | 93.8 (86.0–96.5) | 82.5 (58.6–92.8) | 0.08 | |||
| 22 | 90.8 (86.1–94.3) | 71.5 (58.7–85.5) | 0.01 | 96.4 (90.1–98.1) | 75.7 (61.1–82.7) | 0.003 | |||
| Number of Double Bonds | |||||||||
| 0 | 95.0 (92.9–96.3) | 84.2 (81.1–89.7) | 0.005 | 97.1 (94.5–98.4) | 91.3 (82.8–91.8) | 0.005 | |||
| 1 | 95.3 (89.3–96.4) | 91.1 (86.1–93.9) | 0.16 | 98.0 (93.9–98.7) | 87.8 (84.0–96.7) | 0.02 | |||
| 2 | 95.9 (89.6–97.0) | 88.5 (74.8–92.0) | 0.08 | 98.0 (94.3–98.9) | 87.8 (65.8–96.4) | 0.007 | |||
| 3 | 97.8 (94.0–99.2) | 95.6 (89.8–97.4) | 0.25 | 99.1 (97.6–99.5) | 89.2 (85.7–97.7) | 0.04 | |||
| 4 | 94.9 (88.8–97.1) | 82.5 (75.1–90.0) | 0.06 | 91.9 (81.1–96.0) | 83.3 (68.5–94.2) | 0.36 | |||
| 6 | 95.8 (92.8–97.9) | 84.2 (66.9–92.4) | 0.01 | 98.2 (89.1–98.6) | 74.9 (35.6–85.8) | 0.003 | |||
For saturated fatty acids with the exception of C12:0, there was a significant decrease in fatty acid absorption of C14:0, C16:0, C18:0, C20:0, and C22:0 at both 2 and 6 weeks in formula-fed compared to breast milk-fed infants. Comparing all saturated fatty acids to all unsaturated fatty acids, this significant difference was only seen with the former class of fatty acids (Figure 1, Panel A).
Figure 1.
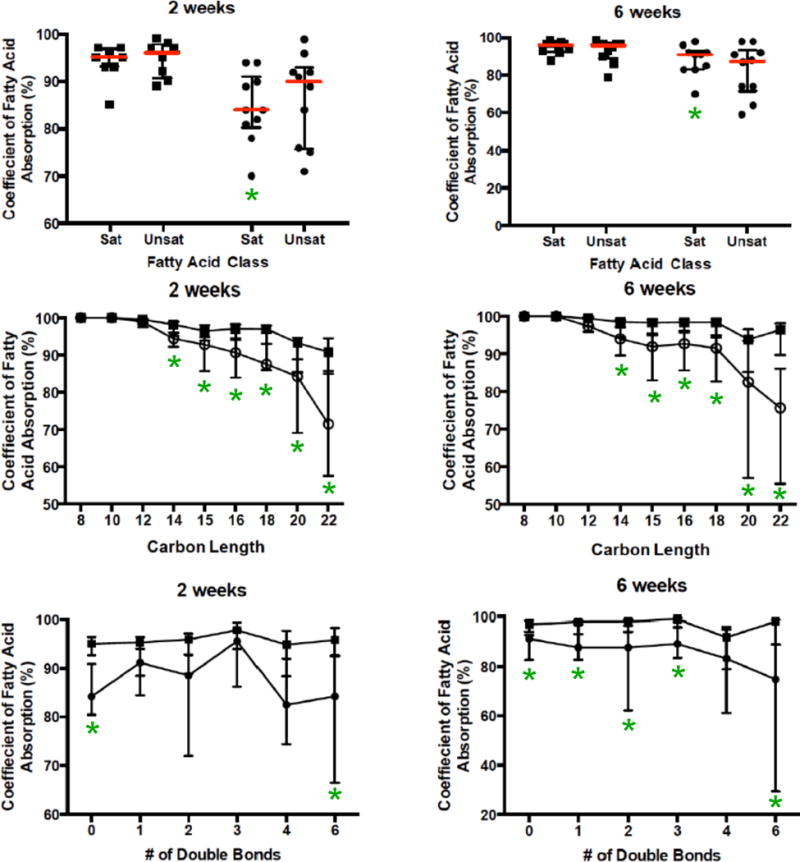
Absorption coefficients by fatty acid structural characteristics: saturated (Sat) vs. unsaturated (Unsat) (Panel A – BM square, formula circle), carbon length (Panel B – BM square, formula open circle), number of double bonds (Panel C – BM square, formula circle). BM= breast milk. * = p <0.05 formula vs. BM.
For n-6 fatty acids, only 20:2n-6 showed a statistically significant decrease in fatty acid absorption comparing formula-fed infants with those breast milk-fed. For n-3 fatty acids, DHA was on the only one showing lower values in formula-fed compared to breast milk-fed infants. For n-9 fatty acids, there was a small but statistically significant decrease in 16:1n-9.
To assess whether these differences could be the result of increasing carbon length, results were graphed as a function of carbon length (Figure 1, Panel B). With increasing carbon length beyond C12, there was a slight decrease in fatty acid absorption in breast milk-fed infants at both 2 weeks and 6 weeks. The magnitude of this decrease in fatty acid absorption was much greater in formula-fed infants at both time points. There was no clear relationship to number of double bonds (Figure 1, Panel C) or in omega class.
Discussion
Compared to breast milk-fed preterm infants, formula-fed preterm infants have impaired absorption of saturated fatty acids and fatty acids of all classes with carbon lengths of 14 or more. Of particular importance is the reduced absorption of DHA. These differences in absorption coefficients are evident through at least 6 weeks postnatal age. The fact that differences in fatty acid absorption coefficients were present between the two groups although there were no differences in total fat absorption highlights the importance of evaluating absorption coefficients for individual fatty acids to further understand the biological limitations in supplying adequate amounts of these important nutrients through enteral feedings.
Total fat absorption and carbon length
Our study rigorously examined fatty acid composition by GC-MS in 3-day stool collections with results consistent with a progressive decrease in the coefficient of fatty acid absorption with increasing carbon length. This is in agreement with the known kinetics of pancreatic lipase with increasing chain length.7 Furthermore, differences observed between breast milk-fed and formula-fed infants are unlikely to be explained by differences in the sn position of LCPUFAs in breast milk compared to formula as the standard oils used to supplement formulas have, in contrast to breast milk, triglycerides with two versus one LCPUFA esterified per triglyceride molecule, LCPUFAs in all three sn positions, versus predominantly the sn-2 and sn-3 positions, and a greater proportion of LCPUFAs of the total fatty acid pool in the sn-2 position compared to that found in breast milk.8 Thus, the data represented are consistent with limited pancreatic lipase production by the preterm infant with lipase being present in breast milk but not in formula. This would extend the results by Lee and Lebenthal demonstrating that in healthy term infants, significant pancreatic lipase and amylase production by the newborn does not increase until after 6 months of age,2 with these two enzymes being present in breast milk as a compensatory process.
Similar to our study, Moya et al demonstrated that total fat absorption in preterm infants fed formula was 91 to 95% and Carnielle et al showed that the coefficient of total fat absorption was not statistically different between preterm infants fed breast milk compared to those fed formula supplemented with LCPUFAs (82.3% vs. 75.6%, respectively); of note, the CFA values from the latter study were lower than the values in our study.9,10 Moya et al demonstrated absorption rates of C8:0, C10:0 and C12:0 as well as linoleic and alpha-linolenic acid greater than 94% in formula-fed infants.9 Jensen et al also found absorption rates of 99% for fatty acids with carbon lengths up to 12 in infants supplemented with medium chain or long-chain fatty acid formulas. Additionally, and in concordance with our findings, Jensen noted in infants fed formulas with long-chain fatty acids declining fatty acid absorption rates with increasing carbon lengths.11
Docosahexaenoic acid (DHA) and Arachidonic acid (AA)
In our preterm cohort, AA absorption rates did not significantly differ between breast milk-fed and formula-fed infants. In contrast, DHA absorption was significantly lower in formula-fed compared to breast milk-fed infants at both 2 and 6 weeks postnatal age. Moya et al also demonstrated absorption rates below 90% for DHA and AA, (74.4% and 75.2%, respectively); however, there was no breast milk-fed control group.9 Although Boehm et al compared formula-fed infants to breast milk-fed infants, he found that absorption rates were similar for AA (70.6 vs. 73.0%, respectively) and DHA (69.0 vs. 73.0%, respectively).12 Carnielli et al did not find differences between preterm infants fed formula versus breast milk-fed infants in the absorption of AA; however, DHA was better absorbed from phospholipid derived LCPUFA enriched formulas compared to breast milk or triglyceride derived PUFA enriched formula (88.7 vs. 79.2 vs. 80.4%, respectively).10 Although we show low absorption rates of DHA in formula-fed infants, we also found higher rates in breast milk-fed infants compared to these studies cited and thus unlike these studies, demonstrating a difference between breast milk-fed and formula-fed infants. Although Carnielli also found a difference, this was only a function of how the DHA was supplied in the formula with no difference seen between breast milk-fed and standard formula.
It should be emphasized that the finding of coefficient of fatty acid absorption for AA and DHA <90% and in particular 74.7% for DHA at 6 weeks in formula-fed preterm infants is below what was seen in breast milk-fed infants and signifies a clinically meaningful abnormal result. Although there are no defined normal values for coefficient of fatty acid absorption, normal coefficient of fat absorption (CFA) values are >90%. In patients with chronic pancreatitis with exocrine pancreatic insufficiency and cystic fibrosis, the CFA is <85%.13 Thus coefficient of fatty acid absorption values of >90% seen in breast milk-fed infants parallel normal CFA values. Hence, the lower values, especially for DHA in formula-fed infants, likely represent suboptimal lipolysis and is similar to the CFA seen in exocrine pancreatic patients. Whether these changes are at least in part reflective of decreased absorption from the intestine in preterm infants is unknown but is not unexpected given the prematurity of the gut in these very low birth weight preterm infants.
Implications of exocrine pancreatic effects on AA and DHA levels in preterm infants
Proper central nervous system and retinal development requires adequate LCPUFA intake, especially DHA and AA. In recognition of the importance of these two fatty acids on infant development, the FDA recommends that infant formulas be supplemented with DHA as well as AA. However, this recommendation is potentially ineffective due to the fact that formula lacks lipase, thereby limiting the ability of formula-fed newborns to digest these LCPUFAs. Although not examined in the present study, the pasteurization of donor breast milk inactivates endogenous bile salt stimulated lipase and thus would mimic the results seen in formula-fed infants.14 Taken together, the maldigestion as shown by our current data and the likely downstream malabsorption of DHA and AA in preterm infants leading to low systemic levels would be predicted to be exacerbated by a shorter gestation period resulting in decreased placental transfer of these two LCPUFAs, leaving preterm newborns with less stored AA and DHA at birth compared to term infants. In fact our group has shown that DHA and AA blood levels fall rapidly within the first postnatal week in preterm infants as a result of the current parenteral nutrition used.1 Thus the absorption of AA and especially DHA by the subsequent administration of enteral formula is likely to be further complicated by lower levels of bile salts in preterm infants as well as a lack of intestinal maturation affecting fatty acid absorption across the enterocyte.15,16 As a result, strategies to maintain DHA and AA levels need to take into account modifications to both parenteral as well as enteral administration of LCPUFAs with the latter addressing both lipolysis and intestinal absorption.
There are limitations to our study. First, this was a retrospective study and the preterm infants were selected for this study if they were receiving full enteral feedings at two and six postnatal weeks of age, were exclusively breast milk-fed or formula-fed, and if a complete 3-day block of nutritional intake with dietary and fecal samples was collected and available for analysis. Thus the study relied on previously collected samples that were obtained from the infusion tubing after completion of the feeding. This may have over represented the fat content in the diet and as a result the absorption coefficients. This, however, likely does not change the conclusions of the study. The data on breast milk fed infants is in agreement with prior reported literature; and, for the formula fed infants, residual fat from the tubing suggests that our absorption coefficients may represent the best-case scenario, which further magnifies the CFA differences between breast milk fed and formula fed infants. Second, although all fecal samples were extracted from the diapers, given the fact that the study was retrospective, no carmine red dye was used as a marker. Although it is possible that this may result in some variability between days of collection, the changing of diets after reaching full enteral feedings was minimal and thus unlikely to result in substantial error, which is supported by the similarities in our observations with other investigators.
Strengths of this study, which add to the current literature, include absorption coefficient data for total fat and specific fatty acids in a cohort of very preterm infants; analysis at two different postnatal ages highlighting the persistent, developmental significance of pancreatic insufficiency during early infancy; and, evaluation in a contemporary cohort of very preterm infants receiving formula with standard LCPUFA supplementation (not receiving experimental formulations) with comparisons to breast milk-fed preterm infants which represent optimal conditions.
Conclusion
Preterm infants fed formula demonstrated lower coefficient of fatty acid absorption as a function of increasing carbon length. This is consistent with limited pancreatic lipase production by the preterm infant and with lipase being present in breast milk but not in formula-fed infants. This is unlikely to be explained by sn-position of LCPUFAs in breast milk versus formula-fed infants. These data highlight principles that need to be considered to optimize delivery and absorption of dietary LCPUFAs in preterm infants. Although, the amount of fatty acids needed to approximate fetal accretion have been defined, which is more than is currently provided, this value does not take into account the exocrine pancreatic insufficiency of infancy.
What is known about this subject?
In term infants, the exocrine pancreas produces proteases; but only limited amounts of lipase and amylase.
Breast milk contains enzymes, including lipase, to aid digestion.
Prior literature is mixed on the ability of preterm infants to efficiently digest triglycerides and absorb fatty acids.
What are the new findings and/or what is the impact on clinical practice?
Formula-fed preterm infants have impaired absorption for saturated fatty acids and fatty acids with increasing carbon length, including docosahexaenoic acid (DHA).
Impaired fatty acid absorption is evident through at least six weeks postnatal age.
Supplementing formula with additional amounts of DHA and arachidonic acid to achieve the needs of preterm infants is unlikely to be an effective strategy without optimizing lipolysis.
Acknowledgments
We gratefully acknowledge the nursing staff of our NICU as well as the parents of our preterm infants who were critical is ensuring successful completion of this study.
Funding: CRM supported by the Program for Faculty Development and Diversity of Harvard Catalyst, Harvard Clinical and Translational Science Center, National Center for Research Resources (award UL1 RR 025758 and financial contributions from Harvard University and its affiliated academic health care centers), 1R01DK104346-01, the Charles H. Hood Foundation, the Alden Trust, the Gerber Foundation, and the generous philanthropic donors to the Infant Health Research Program at Beth Israel Deaconess Medical Center. The content is solely the responsibility of the authors and does not necessarily represent the official views of Harvard Catalyst, Harvard University and its affiliated academic health care centers, the National Center for Research Resources, or the National Institutes of Health.
Abbreviations
- AA
Arachidonic acid
- BM
Breast milk
- CFA
coefficient of fat absorption
- DHA
Docosahexaenoic acid
- F
Formula
- FA-CFA
Fatty acid specific coefficient of fat absorption
- GC-MS
Gas chromatography-mass spectroscopy
- LCPUFAs
long chain polyunsaturated fatty acids
Footnotes
Role of the Sponsors: None of the funding bodies had any role in the study design or conduct; data collection, management, analysis or interpretation; or preparation, review, or approval of the manuscript.
Disclosures
None of the authors has any financial issue or conflict of interest to disclose.
- Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; AND
- Drafting the work or revising it critically for important intellectual content; AND
- Final approval of the version to be published; AND
- Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- 1.Martin CR, Dasilva DA, Cluette-Brown JE, et al. Decreased Postnatal Docosahexaenoic and Arachidonic Acid Blood Levels in Premature Infants are Associated with Neonatal Morbidities. J Pediatr. 2011;159:743–9 e2. doi: 10.1016/j.jpeds.2011.04.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lebenthal E, Lee PC. Development of functional responses in human exocrine pancreas. Pediatrics. 1980;66:556–60. [PubMed] [Google Scholar]
- 3.Armand M, Hamosh M, Mehta NR, et al. Effect of human milk or formula on gastric function and fat digestion in the premature infant. Pediatr Res. 1996;40:429–37. doi: 10.1203/00006450-199609000-00011. [DOI] [PubMed] [Google Scholar]
- 4.Hamosh M, Mehta NR, Fink CS, Coleman J, Hamosh P. Fat absorption in premature infants: medium-chain triglycerides and long-chain triglycerides are absorbed from formula at similar rates. J Pediatr Gastroenterol Nutr. 1991;13:143–9. [PubMed] [Google Scholar]
- 5.Hernell O, Gebre-Medhin M, Olivecrona T. Breast milk composition in Ethiopian and Swedish mothers. IV. Milk lipases. Am J Clin Nutr. 1977;30:508–11. doi: 10.1093/ajcn/30.4.508. [DOI] [PubMed] [Google Scholar]
- 6.Freedman SD, Blanco PG, Zaman MM, et al. Association of cystic fibrosis with abnormalities in fatty acid metabolism. N Engl J Med. 2004;350:560–9. doi: 10.1056/NEJMoa021218. [DOI] [PubMed] [Google Scholar]
- 7.Akanbi TO, Sinclair AJ, Barrow CJ. Pancreatic lipase selectively hydrolyses DPA over EPA and DHA due to location of double bonds in the fatty acid rather than regioselectivity. Food chemistry. 2014;160:61–6. doi: 10.1016/j.foodchem.2014.03.092. [DOI] [PubMed] [Google Scholar]
- 8.Food Standards Australia New Zealand. (Technical Report Series NO. 22).DHASCO and ARASCO oils as sources of long-chain ployunsaturated fatty acids in Infant formula: A Safety Assessment. 2003
- 9.Moya M, Cortes E, Juste M, De Dios JG, Vera A. Fatty acid absorption in preterms on formulas with and without long-chain polyunsaturated fatty acids and in terms on formulas without these added. Eur J Clin Nutr. 2001;55:755–62. doi: 10.1038/sj.ejcn.1601219. [DOI] [PubMed] [Google Scholar]
- 10.Carnielli VP, Verlato G, Pederzini F, et al. Intestinal absorption of long-chain polyunsaturated fatty acids in preterm infants fed breast milk or formula. Am J Clin Nutr. 1998;67:97–103. doi: 10.1093/ajcn/67.1.97. [DOI] [PubMed] [Google Scholar]
- 11.Jensen C, Buist NR, Wilson T. Absorption of individual fatty acids from long chain or medium chain triglycerides in very small infants. Am J Clin Nutr. 1986;43:745–51. doi: 10.1093/ajcn/43.5.745. [DOI] [PubMed] [Google Scholar]
- 12.Boehm G, Muller H, Kohn G, Moro G, Minoli I, Bohles HJ. Docosahexaenoic and arachidonic acid absorption in preterm infants fed LCP-free or LCP-supplemented formula in comparison to infants fed fortified breast milk. Ann Nutr Metab. 1997;41:235–41. doi: 10.1159/000177998. [DOI] [PubMed] [Google Scholar]
- 13.Borowitz D, Konstan MW, O’Rourke A, Cohen M, Hendeles L, Murray FT. Coefficients of fat and nitrogen absorption in healthy subjects and individuals with cystic fibrosis. The journal of pediatric pharmacology and therapeutics : JPPT : the official journal of PPAG. 2007;12:47–52. doi: 10.5863/1551-6776-12.1.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Henderson TR, Fay TN, Hamosh M. Effect of pasteurization on long chain polyunsaturated fatty acid levels and enzyme activities of human milk. J Pediatr. 1998;132:876–8. doi: 10.1016/s0022-3476(98)70323-3. [DOI] [PubMed] [Google Scholar]
- 15.Verkade HJ, Hoving EB, Muskiet FA, et al. Fat absorption in neonates: comparison of long-chain-fatty-acid and triglyceride compositions of formula, feces, and blood. Am J Clin Nutr. 1991;53:643–51. doi: 10.1093/ajcn/53.3.643. [DOI] [PubMed] [Google Scholar]
- 16.Watkins JB, Szczepanik P, Gould JB, Klein P, Lester R. Bile salt metabolism in the human premature infant. Preliminary observations of pool size and synthesis rate following prenatal administration of dexamethasone and phenobarbital. Gastroenterology. 1975;69:706–13. [PubMed] [Google Scholar]


