Abstract
OBJECTIVES
We examined whether gender differences exist regarding stress, symptom distress, coping, adherence, and social support 5 years after heart transplantation.
BACKGROUND
Differences exist in health-related quality of life outcomes by gender after heart transplantation; women report poorer outcomes.
METHODS
Patients (n=210, female=42), were from a prospective, multi-site, study of health-related quality of life long-term after heart transplantation. Patients completed self-report instruments 5 years after heart transplantation (mean=4.98±0.17 years after transplant). Statistical analyses included two-sample t-tests, Chi-square or Fisher’s exact test, and multivariable modeling.
RESULTS
Women did not report more overall stress or symptom distress, but reported more difficulty adhering to the transplant regimen, yet more actual adherence than men. Women reported using more negative coping styles, but reported more satisfaction with social support.
CONCLUSIONS
Gender differences exist regarding appraisal of stress, coping styles, and coping resources long-term after heart transplantation. These differences may guide tailoring therapy regarding stress, poor coping, and lack of resources.
Keywords: stress and coping, heart transplant, gender
INTRODUCTION
Long-term survival after heart transplantation is similar for men and women.1 Other outcomes after heart transplantation differ by gender. We have previously reported that being female was related to worse functional ability both early and later after heart transplantation2, 3 and depression later after heart transplantation.4 Gender was not related to work status5 or overall satisfaction with health-related quality of life, although being female was related to less satisfaction with health and functioning long-term after transplant.6 Given differences in these outcomes by gender long-term after heart transplantation, we questioned whether factors that may influence these outcomes might also differ by gender.
Previous incidental findings of gender differences regarding stress, symptom distress, coping, and adherence7, 8, 9 supported our undertaking of a more rigorous examination of the influence of gender on these factors. Importantly, stress, symptom distress, coping, support, and adherence have been related to outcomes (e.g., quality of life, depression, physical function, and survival) after heart transplantation.1, 3, 4, 6, 10 Understanding whether gender affects stress related to heart transplantation, appraisal of transplant-related stress, and coping may provide guidance in tailoring long-term care after heart transplantation which may improve outcomes.
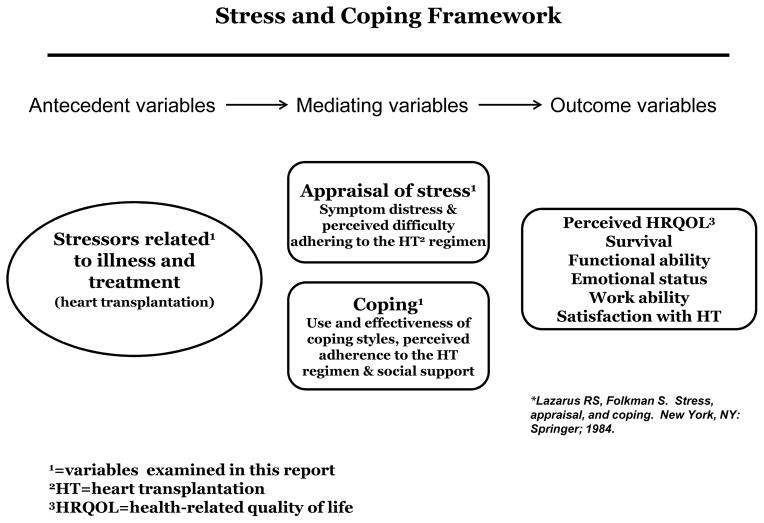
Using the Lazarus and Folkman Stress, Appraisal, and Coping framework,11 we examined whether gender differences exist regarding stress (e.g., stress related to illness and treatment [i.e., heart transplantation]), appraisal of stress (e.g., symptom distress, and perceived difficulty adhering to the heart transplant treatment regimen), and coping (e.g., use and effectiveness of coping styles, perceived adherence to the heart transplant regimen, and coping resources [e.g., social support]) at 5 years after heart transplantation, which are related to outcomes (Figure 1). This framework has appropriately guided our research, as per Lazarus and Folkman, outcomes, including quality of life, are affected by the stresses of living, evaluation of those stresses, and how individuals cope.11 We hypothesized that female heart transplant recipients would report more overall stress and symptom distress, use of more negative coping styles, more difficulty adhering to the transplant medical regimen, less adherence to the transplant regimen, and less satisfaction with social support than men.
Figure 1.
Stress and coping framework for patients who undergo heart transplantation
METHODS
Design
The study used a prospective, multi-site, longitudinal, observational design.
Sample
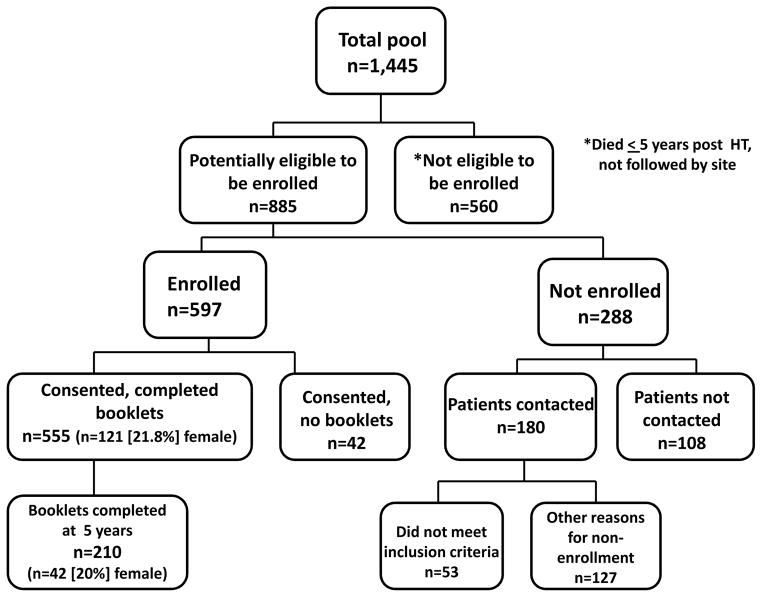
Patients for this secondary analysis were from a study of HRQOL outcomes at 5 – 10 years after heart transplantation. The study cohort was from a pool of 1,437 adult patients who were transplanted between July 1, 1990 and June 30, 1999 at 4 medical centers in the United States. Inclusion criteria were age ≥ 21 years, ability to read and write English, and physically able to participate. Of the 1,437 patients, 884 were potentially eligible to enroll in our study, 597 were enrolled, and 555 patients completed one or more booklets of questionnaires over time. Two hundred eighty-seven patients were not enrolled, and 127 of them chose not to participate. Reasons for non-enrollment are documented elsewhere.6 When consented patients (n=597) were compared to patients who did not consent (n=127), there were no statistically significant differences between groups for gender.6 Two hundred ten of the 555 patients were 5 years post heart transplantation and comprise the sample for this report (figure 2). Of the 210 patients, 42 (20%) were women, which is similar to the 22% of women who underwent heart transplantation during the era of data collection for our report, per the International Society of Heart and Lung Transplantation Registry.12
Figure 2.
Flow chart of study sample
Instruments
Self-report questionnaires used for this report were completed by paper and pencil at 5 years after heart transplantation. Questionnaires, aligned with our Stress and Coping Framework, measured the following constructs: (1) frequency and intensity of stress (Heart Transplant Stressor Scale13); (2) appraisal of stress (symptom frequency and distress (Heart Transplant Symptom Checklist14) and perceived difficulty with adherence to the medical regimen (Assessment of Problems with the Heart Transplant Regimen15); and (3) coping and coping resources (coping use and perceived effectiveness (Jalowiec Coping Scale16), perceived actual adherence with the medical regimen (Assessment of Problems with the Heart Transplant Regimen15), and satisfaction with social support (Social Support Index17).
Stress
We defined stress as “a relationship between the person and the environment that is appraised by the person as taxing or exceeding his or her resources and endangering his or her well-being”.11 The Heart Transplant Stressor Scale includes 81 items that measure stress related to physical, psychological, self-care, family, work/school/financial, and hospital/clinic dimensions. (0=not stressful at all to 3=very stressful).13 Psychometric support is adequate for this instrument. Homogeneity reliability is supported (Cronbach’s alpha coefficients = 0.95 for the entire scale and 0.78–0.90 for the dimensions).13 Validity was also acceptable.13
Appraisal of stress
Evaluation of stress included measures of symptom distress and difficulty adhering to the medical regimen. Symptom distress occurs in response to the perception of an abnormal physical, emotional, or cognitive state (e.g., cramps in feet, mood swings, and problems with memory).18 The Heart Transplant Symptom Checklist has 89 items measuring symptom frequency (yes/no) and symptom distress (0=not bothered at all to 3=very bothered for symptom distress).14 There are six subscales: cardiopulmonary, gastrointestinal, neuromuscular, genitourinary, dermatologic, and psychological). Cronbach’s alpha was acceptable (0.95 for the entire scale and range = 0.91 – 0.68 for five of the six subscales). The genitourinary subscale had a Chronbach’s alpha of only 0.46 which we potentially attribute to fewer items on the subscale.14 Content and construct validity were supported.14
Adherence is “the extent to which a person’s behavior, following the medical regimen, corresponds with the agreed recommendations of a healthcare provider”.19 Perceived difficulty with adherence to the transplant regimen is measured by the Assessment of Problems with the Heart Transplant Regimen instrument. Part A measures difficulty (1=no difficulty to 4=a lot of difficulty) regarding taking medications, lifestyle changes, and appointment keeping.15 Test-retest reliability was acceptable for this instrument.15 This instrument did not meet requirements for internal consistency reliability. Given the multiple distinct items in the instrument, related to the post transplant medical regimen, we did not expect this instrument to have adequate internal consistency reliability. Validity was acceptable, with support for both content and concurrent validity.15
Coping and coping resources
Coping is defined as “constantly changing cognitive and behavioral efforts to manage specific external and/or internal demands that are appraised as taxing or exceeding the resources of the person”.11 Coping use and effectiveness are measured by the 60-item Jalowiec Coping Scale (0=never used to 3=often used and 0=not helpful to 3=very helpful) which has 8 subscales (confrontive, evasive, optimistic, fatalistic, emotive, palliative, supportant and self-reliant).16 Two summary scores were calculated from subscale scores: (1) positive coping styles (confrontive, optimistic, self-reliant and supportant subscales) and (2) negative coping styles (fatalistic, evasive, and emotive subscales). This widely used instrument has alpha reliability coefficients of 0.75–0.86 for the total and subscale scores and acceptable validity.16
Perceived adherence to the transplant regimen, a behavioral effort to manage the demands of heart transplantation, is also measured by the Assessment of Problems with the Heart Transplant Regimen instrument. Part B measures actual adherence (1=all of the time to 4=hardly ever) for taking medications, lifestyle changes, and appointment keeping.15
Social support (a coping resource) is the degree of perceived satisfaction with support provided by others; thus, the individual appraises whether support is acceptable or satisfactory at times of need.20, 21 The Social Support Index has 15 items that include both tangible and emotional support. Patients respond to their level of satisfaction with support on a scale from 1=very satisfied to 4=very dissatisfied.17 Cronbach’s alpha reliability was supported for the total scale (0.84) and subscales (tangible support=0.78 and emotional support=0.69).17 Validity for this instrument was acceptable, as well.17
Medical records
Medical records data at 5 years after transplant were used for this report as well as data available to us from the Cardiac Transplant Research Database (CTRD), a large registry located at the University of Alabama, Birmingham. Clinical data from medical records and the CTRD included medical conditions diagnosed per cardiologist and associated tests (e.g., acute rejection, infection, renal disease, and endocrine disorders [e.g., diabetes mellitus]) and psychiatric conditions diagnosed per psychologist / psychiatrist (e.g., depression and anxiety). The co-principal investigator, a heart transplant clinician, reviewed small samples of medical records data from all sites to ensure accuracy of chart review.
Procedures
Sites received Institutional Review Board approval prior to participation in our larger HRQOL study and the CTRD. Patients were consented either face-to-face at a clinic visit or while hospitalized or via mail. Patients who provided written informed consent completed booklets of questionnaires every 6 months from 5 to 10 years after heart transplantation. Research coordinators collected medical records data. Data used for this report were from patient completed self-report questionnaires and medical records at approximately 5 years (mean=4.98±0.17 years, median=4.99 years) after transplant, which for the cohort of patients in this study was from 7/1/95 – 6/30/99. Data were screened and cleaned and then sent to our Data Coordinating Center at the University of Alabama, Birmingham for data entry and analyses.
Statistical Analyses
Continuously distributed measurements are summarized using means and standard deviations and compared using two-sample t-tests. Categorical variables are shown as counts/percentages and group comparisons are based on the Chi-square or Fisher’s exact test.
To assess the hypothesized gender differences, multivariable models were created based on a simplified version of bagging,22 a widely employed machine learning ensemble method. This approach alleviates some of the most common shortcomings of automatic model building methods, such as instability, sensitivity to outliers or lack of reproducibility. For every factor (statistical outcome), a two-stage process was created: first, the original dataset was bootstrap resampled (with replacement) 1,000 times. Within each bootstrap sample, stepwise variable selection with 0.05 entry/exit criteria occurred, and gender was included, by default, in every model. The following predictors were entered into the model: gender, age, race group (white, non-white), marital status (married, non-married), heart disease etiology (idiopathic, ischemic, other), education (≤12 years (high school), >12 years), diabetes, orthopedic illness, gout, renal disease, cardiovascular disease, co-existing oncologic illness, gastrointestinal disease, co-existing psychological illness and coronary artery disease.
In stage two, the short list of predictors significant at a two-sided 5% level in at least 200 of the 1,000 resamples (20%) was compiled. Only these predictors were included in the final regression model created based solely on the original dataset. The 20% threshold choice is intended to produce a parsimonious and stable final model. Currently, there are no metric-driven guidelines for the choice of such thresholds, yet common choices in practice may range between 20% and 50%. All analyses were performed using SAS v9.3. Throughout, statistical significance was established at the two-sided 5% alpha level, and no adjustments for multiplicity were made.
RESULTS
Differences by gender were detected for demographic and clinical characteristics at 5 years after heart transplantation (Table 1). More female patients (n=42) were significantly younger, non-white, and not married than male patients (n=168). More women than men had dilated cardiomyopathy as the etiology of heart failure. Additionally, women had less concomitant renal disease, as compared to men.
Table 1.
Comparison of Demographic and Pre- and Post-operative Characteristics by Gender
| Variable | Women (N=42) | Men (N=169) | P-value |
|---|---|---|---|
| Demographic characteristics | |||
| Age of recipient at transplant (years) | 48.8 ± 12.0 | 57.1 ± 8.5 | <.001 |
| Race | 0.008 | ||
| White | 34 (81%) | 160 (95%) | |
| Black | 8 (19%) | 7 (4%) | |
| Asian | 0 (0%) | 2 (1%) | |
| Marital Status | <.001 | ||
| Divorced/separated | 9 (21%) | 17 (10%) | |
| Married | 24 (57%) | 139 (82%) | |
| Single | 7 (17%) | 5 (3%) | |
| Widowed | 2 (5%) | 8 (5%) | |
| Education | 0.85 | ||
| High school degree or less | 16 (38%) | 67 (40%) | |
| College degree or more | 26 (62%) | 102 (60%) | |
| Pre-operative characteristics | |||
| Heart Disease Etiology | <.001 | ||
| Idiopathic | 24 (57%) | 38 (22%) | |
| Ischemic | 9 (21%) | 116 (69%) | |
| Other | 9 (21%) | 15 (9%) | |
| Post-operative characteristics | |||
| Co-morbid conditions | |||
| Diabetes | 8 (20%) | 57 (34%) | 0.07 |
| Orthopedic Illness | 7 (17%) | 36 (22%) | 0.53 |
| Gout | 5 (12%) | 32 (19%) | 0.30 |
| Cardiovascular Disease | 8 (20%) | 31 (19%) | 0.89 |
| Oncologic Illness | 7 (17%) | 40 (24%) | 0.35 |
| GI Illness | 8 (20%) | 39 (23%) | 0.60 |
| Renal Illness | 5 (12%) | 74 (44%) | <.001 |
| Psychiatric Condition | 14 (34%) | 38 (23%) | 0.13 |
| Coronary Artery Disease | 10 (24%) | 65 (38%) | 0.08 |
| Coronary Heart Failure | 0 (.%) | 2 (100%) | . |
| Hypertension | 30 (73%) | 143 (86%) | 0.06 |
| Hyperlipidemia | 29 (71%) | 125 (75%) | 0.59 |
| Pulmonary Disease | 6 (15%) | 16 (10%) | 0.35 |
| Infection Co-Existing Illness | 3 (7%) | 14 (8%) | 0.82 |
| Total number of rejection episodes | 2.1 ± 1.9 | 1.6 ± 1.6 | 0.06 |
| Total number of infection episodes | 0.6 ± 1.0 | 0.8 ± 1.3 | 0.24 |
| At least on rejection episode | 35 (83%) | 119 (70%) | 0.09 |
| At least one infection episode | 14 (33%) | 78 (46%) | 0.13 |
| New York Heart Functional Class | 0.45 | ||
| I | 23 (55%) | 111 (65%) | |
| II | 17 (40%) | 54 (32%) | |
| III | 0 (0%) | 1 (1%) | |
| missing | 2 (5%) | 3 (2%) | |
Appraisal of Heart Transplant-related Stress
Appraisal of heart transplant-related stress is presented in Table 2. Regarding overall stress, as compared to men, women had borderline higher overall intensity of stress by 0.02 points on average. In addition, patients without a psychiatric condition (e.g., depression and anxiety) or diabetes experienced a lower overall intensity of stress.
Table 2.
Multivariable Models for Appraisal of Heart Transplant-related Stress. Dependent Variables (Outcomes) are “Difficulty with Adherence to the HT Regimen” and “Intensity of Overall Stress”. Independent Variables are Listed for Each Outcome and No Additional Variables Were Controlled For.
| Factor | Variable | Estimate | 95% CI | P-value |
|---|---|---|---|---|
| Difficulty with Adherence to the HT Regimen | ||||
| Women | 0.05 | (0.01, 0.08) | 0.01 | |
| Age (years) | −0.001 | (−0.003, 0.001) | 0.035 | |
| No Renal Disease | 0.03 | (0.001, 0.05) | 0.048 | |
| Idiopathic Etiology | −0.005 | (−0.05, 0.04) | 0.80 | |
| Ischemic Etiology | 0.02 | (−0.02, 0.06) | 0.27 | |
| Non-White | −0.03 | (−0.08, 0.01) | 0.14 | |
| High School Degree or less | −0.02 | (−0.04, 0.01) | 0.23 | |
|
| ||||
| Intensity of Overall Stress | ||||
| Women | 0.02 | (0.001, 0.05) | 0.052 | |
| Age | −0.001 | (−0.002, 0.001) | 0.16 | |
| No Psychiatric Condition | −0.05 | (−0.07, −0.03) | <.0001 | |
| No Diabetes | −0.02 | (−0.04, −0.001) | 0.036 | |
| No CAD | −0.01 | (−0.03, 0.01) | 0.14 | |
Women reported significantly more difficulty adhering to the heart transplant regimen than men by an average of 0.05 points (Table 2). Additionally, younger patients indicated that they had more difficulty adhering to the heart transplant regimen than older patients. No differences were detected between groups for symptom distress (data not shown).
Coping Styles and Resources
In terms of coping styles (Table 3), women demonstrated significantly higher scores on the Overall Negative Use subscale than men (mean difference 0.1 points). In addition, women displayed a trend for significantly higher scores on the Overall Positive Use subscale as compared to men, with a mean difference of 0.08 points. Participants with no documented psychiatric condition had lower scores on the Overall Negative use subscale.
Table 3.
Multivariable Models for Use of Coping Styles. Dependent Variables (Outcomes) are “Overall Positive Use of Coping Styles”, “Overall Negative Use of Coping Styles” and “Actual Adherence to the Heart Transplant (HT) Regimen”. Independent Variables are Listed for Each Outcome and No Additional Variables Were Controlled For.
| Factor | Variable | Estimate | 95% CI | P-value |
|---|---|---|---|---|
| Overall Positive Use of Coping Styles | ||||
| Women | 0.08 | (−0.003, 0.17) | 0.06 | |
| No Cardiovascular Illness | −0.07 | (−0.15, 0.02) | 0.13 | |
| No Oncologic Illness | −0.06 | (−0.14, 0.03) | 0.17 | |
|
| ||||
| Overall Negative Use of Coping Styles | ||||
| Women | 0.10 | (0.03, 0.16) | 0.005 | |
| Age (years) | −0.002 | (−0.005, 0.001) | 0.13 | |
| No Psychiatric Condition | −0.10 | (−0.15, −0.04) | 0.001 | |
| Idiopathic Etiology | −0.002 | (−0.08, 0.08) | 0.96 | |
| Ischemic Etiology | 0.08 | (−0.005, 0.16) | 0.07 | |
| No Cardiovascular Illness | −0.04 | (−0.10, 0.02) | 0.19 | |
|
|
|
|||
| Actual Adherence to the HT Regimen | ||||
| Women | 0.05 | (0.02, 0.08) | 0.005 | |
| Age (years) | −0.003 | (−0.004, −0.001) | <.0001 | |
| Idiopathic Etiology | 0.05 | (0.01, 0.09) | 0.028 | |
| Ischemic Etiology | 0.06 | (0.02, 0.11) | 0.003 | |
| No Psychiatric Condition | −0.02 | (−0.05, 0.004) | 0.09 | |
| No Orthopedic Illness | −0.02 | (−0.05, 0.01) | 0.22 | |
| No Diabetes | −0.02 | (−0.04, 0.01) | 0.26 | |
Self-report of actual adherence to the heart transplant regimen was significantly higher among women, as compared to men (Table 3), by 0.05 points on average. Similar to difficulty with adherence, younger patients also reported lower adherence than older patients.
Report of overall satisfaction with support (Table 4) was significantly higher among women (mean difference 0.04 points) than men. In addition, women also reported significantly higher levels of satisfaction with support, both on the emotional scale (mean difference 0.09), as well as for tangible support (mean difference 0.06).
Table 4.
Multivariable Models for Coping Resources. Dependent Variables (Outcomes) are “Overall Satisfaction with Social Support”, “Satisfaction with Emotional Support” and “Satisfaction with Tangible Support”. Independent Variables are Listed for Each Outcome and No Additional Variables Were Controlled For.
| Factor | Variable | Estimate | 95% CI | P-value |
|---|---|---|---|---|
| Overall Satisfaction with Social Support | ||||
| Women | 0.04 | (0.004, 0.08) | 0.032 | |
| Married | −0.02 | (−0.06, 0.02) | 0.26 | |
|
| ||||
| Satisfaction with Emotional Support | ||||
| Women | 0.09 | (0.03, 0.14) | 0.004 | |
| Idiopathic Etiology | −0.07 | (−0.15, 0.004) | 0.06 | |
| Ischemic Etiology | −0.04 | (−0.12, 0.03) | 0.24 | |
|
| ||||
| Satisfaction with Tangible Support | ||||
| Women | 0.06 | (0.01, 0.10) | 0.008 | |
| No Oncologic Illness | 0.03 | (−0.01, 0.06) | 0.17 | |
| Idiopathic Etiology | 0.003 | (−0.05, 0.06) | 0.93 | |
| Ischemic Etiology | 0.03 | (−0.02, 0.08) | 0.26 | |
| No Cardiovascular Illness | 0.02 | (−0.02, 0.06) | 0.26 | |
| High School Degree or less | −0.02 | (−0.05, 0.02) | 0.35 | |
DISCUSSION
We conclude that appraisal of stress related to heart transplantation, coping styles, and coping resources differ between men and women at 5 years after heart transplantation. Our hypotheses were partially supported. Regarding appraisal of heart transplant-related stress, women did not report more overall stress (although there was a strong trend) or symptom distress, but did report more difficulty adhering to the transplant regimen than men. For coping styles and resources, women indicated that they used more negative coping styles, but also reported more satisfaction with social support and more adherence to the transplant regimen than men.
We have previously reported that overall intensity of stress is moderate at 5 years after heart transplantation.7 While frequency of stress was not related to gender, intensity of stress was related to gender at 5 years after transplant, with female patients experiencing more intense stress.7 Our current findings suggested only a strong trend for the experience of more intense stress as indicated by women, compared to men. In contradistinction, a study of liver transplant recipients (34–61 months post transplant) revealed that women experienced more psychological distress than men and that gender was significantly associated with overall psychosocial adjustment, which did not improve with the passage of time.23 The authors suggested that women may need more psychological intervention after liver transplantation. Given that we reported moderate levels of stress intensity at 5 and 10 years after heart transplantation in our previous report,7 despite the lack of differences in stress intensity by gender in this report, monitoring and possible intervention regarding stress may be useful.
Our finding of no self- reported differences in symptom distress between women and men later after heart transplantation is supported by our previous findings that examined variables associated with symptom distress at both 5 and 10 years after transplant.8 Of note, when we examined differences in symptom distress earlier (i.e., 1 year) after heart transplantation, women endorsed significantly worse symptom distress than men overall and for three of six subscales: cardiopulmonary, gastrointestinal, and dermatologic.24 Reports from other cohorts earlier after heart (median =3 years post transplant) and lung (mean=1.5±0.7 years post transplant) transplant also demonstrated differences in overall symptom distress for men and women, as well as distress regarding dermatologic / cosmetic symptoms (e.g., bruising, excessive hair growth, etc).25, 26 While a review of symptom occurrence and distress after solid organ transplant revealed that symptom distress was consistently related to gender, with more distress endorsed by women, the authors could not draw conclusions regarding the impact of time since transplant.27 Our findings of no differences in report of symptom distress between men and women long-term after transplant may be explained by lower doses of immunosuppression and therefore potentially reduced medication side effects. Given that our previous findings8 demonstrated symptom distress, at a moderate level of intensity, long-term after heart transplantation, it may none-the-less be useful to develop and test interventions that address symptom burden.
Our finding that women indicated they had more difficulty adhering to the medical regimen, yet reported higher levels of adherence than men deserves comment, as the effect of adherence on outcomes is substantial. An overview of adherence to the medical regimen after thoracic organ transplantation revealed that nonadherence to all aspects of the medical regimen is related to negative clinical outcomes.28 In a study of 218 solid organ transplant recipients (liver, kidney, heart, and lung) who were 84 ± 5 months from transplant, Germani et al.,29 reported that men were less adherent than women to lifestyle recommendations, yet both men and women had similar levels of adherence to medication taking, including both immunosuppressants and non-immunosuppressants. In a study of adherence during the first year after heart transplantation, Dew et al.30 reported no influence of gender on compliance with multiple areas of the post transplant regimen, but did find that compliance in most areas worsened over time. A later report by Dew et al.31 on adherence during the first two years after lung transplantation described better self-care adherence by men than women. Finally, a report from a consensus conference on nonadherence noted that a meta-analysis of risk factors for poor adherence to the medical regimen in other chronic illness populations has typically revealed females being more adherent than males, which is consistent with our findings.32, 33
Findings regarding differences by gender to adherence with components of a prescribed medical regimen are somewhat contradictory. Additional research is needed. Yet, our report and other articles in the literature raise important concerns regarding differences in adherence to the medical regimen by demographic characteristics and the inference that time since transplant may influence adherence. Thus, careful monitoring and intervention, as needed, are recommended across time after heart transplantation.
Additionally, per our Stress, Appraisal, and Coping framework, difficulty with adherence to the medical regimen reflects appraisal of stress, which is distinct from actual adherence. While reports in the literature focus primarily on actual adherence, studying difficulty with adherence, as well as actual adherence, can highlight components of the medical regimen that are appraised as taxing and provide clinicians with an opportunity to assist patients to overcome these difficulties. For example, Zikmund-Fisher et al.34 reported a significant correlation between having problems with taking anti-hypertensive medications and willingness to consider intensification of blood pressure medications in response to an elevated blood pressure. They concluded that paying attention to medication related “issues” can enhance adherence to the medication regimen and downstream outcomes.
More frequent use of negative coping styles as reported by women, as compared to men, long-term after heart transplantation was previously described by our team, using two sample t-tests.7 Our current examination of coping use by gender, using more rigorous statistical methods, supports our earlier findings. This finding may have important clinical implications after transplant. For example, more use of fatalistic coping and high avoidance coping has been found to be related to poor adherence early after heart transplantation.15, 30 Our finding that women indicate that they use more negative coping styles than men long term after heart transplantation reinforces the ongoing need for psychosocial monitoring. Whether or not coping styles can be changed is unclear.35
Contrary to our hypotheses, women reported being more satisfied with overall social support and experienced higher levels of support (tangible and emotional support) later after transplant than men. Support is an important determinant of outcomes after thoracic organ transplantation. More support is related to better health-related quality of life,36 while poor family caregiver support is related to an increased risk of depression and psychological distress.37, 38 Poor support has also been found to be related to immunosuppressant nonadherence after solid organ transplantation.39 Reports of relationships of social support by gender with outcomes (e.g., survival and health-related quality of life) have also been reported in other populations of chronic illness patients, including those with diabetes,40 heart failure,41 and end-stage renal disease.42 Monitoring satisfaction with support and actual support for both men and women long-term after transplant may guide development of interventions for those at risk for poor support and potentially poor outcomes.
Our study was limited by survivorship bias. However, our inclusion of four sites across the U.S. enhanced representativeness of our target population. Also, self-report was the only measure of adherence, a measurement method which tends to overestimate actual adherence, and we only examined overall adherence and difficulty with adherence, rather than adherence to components of the medical regimen. Lastly, while these data are old, heart transplant clinical practice has not changed much over time. Immunosuppression today is similar to medications used when our data were collected, except the use of tacrolimus and mycophenolate mofetil has increased, while the use of cyclosporine and azathioprine has decreased. Also, more ventricular assist devices are being implanted as a bridge to heart transplantation. Since our data were collected long-term after transplant, increased use of these devices should not affect our findings. Finally, patients must still adapt to having received a heart transplant and care for themselves long-term after surgery.
CONCLUSIONS
We conclude that men and women differ on appraisal of stress related to heart transplantation, coping styles, and coping resources long-term after heart transplantation. These differences may guide monitoring and tailoring therapy when stress, symptom burden, poor coping, difficulty with adherence to the medical regimen, and lack of resources are identified later after heart transplantation. We are currently conducting a pilot trial to test an intervention focused on enhancing adherence and maximizing support for an especially vulnerable, high-risk cohort of young adults who receive heart transplantation as children and transition to adult care. Still more research is needed to test interventions (e.g., psychological interventions [related to high stress and poor coping], and behavioral and support-focused interventions [related to adherence with the medical regimen and support] in vulnerable subgroups of patients, after heart transplantation, other solid organ transplantation, and other chronic illnesses (e.g., congenital heart disease).
Acknowledgments
This study was funded by National Institute of Nursing Research Grant R01 NR005200, a grant-in-aid from the College of Nursing, Rush University, intramural funding from the Rush Heart Institute, Rush University Medical Center, Chicago, IL; and intramural funding from Northwestern University, Department of Surgery, Division of Cardiac Surgery.
Footnotes
None of the authors has a financial relationship with a commercial entity that has an interest in the subject of the presented manuscript or other conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Kathleen L Grady, Department of Surgery, Division of Cardiac Surgery, Northwestern University, Chicago, IL.
Adin-Cristian Andrei, Department of Surgery, Division of Cardiac Surgery, Northwestern University, Chicago, IL.
Zhi Li, Department of Surgery, Division of Cardiac Surgery, Northwestern University, Chicago, IL.
Bruce Rybarczyk, Department of Psychology, Virginia Commonwealth University, Richmond, VA.
Connie White-Williams, Department of Nursing, University of Alabama Medical Center, Birmingham, AL.
Robert Gordon, Department of Medicine, Division of Cardiology, Northwestern University, Chicago, IL.
Edwin C. McGee, Jr., Department of Surgery, Division of Cardiac Surgery, Northwestern University, Chicago, IL.
References
- 1.Farmer S, Grady KL, Wang E, McGee E, Cotts W, McCarthy P. Demographic, psychosocial, and behavioral factors associated with survival after heart transplant. Ann Thorac Surg. 2013 Mar;95(3):876–883. doi: 10.1016/j.athoracsur.2012.11.041. [DOI] [PubMed] [Google Scholar]
- 2.Jalowiec A, Grady K, White-Williams C. Functional status 1 year after a heart transplant. J Cardiopulm Rehab. 2007;7(1):24–32. doi: 10.1097/01.hcr.0000265029.25392.6e. [DOI] [PubMed] [Google Scholar]
- 3.Grady KL, Naftel DC, Young JB, Pelegrin D, Czerr J, Higgins R, Heroux A, McLeod M, Rybarczyk B, Kobashigawa J, Chair J, White-Williams C, Myers S, Kirklin J. Patterns and predictors of physical functional disability at 5–10 years after heart transplantation. J Heart Lung Transplant. 2007;26:1182–1191. doi: 10.1016/j.healun.2007.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rybarczyk B, Grady K, Naftel D, Kirklin J, White-Williams C, Kobashigawa J, Chait J, Young J, Pelegrin D, Czerr J, McLeod M, Rissinger J, Higgins R, Heroux A. Emotional adjustment five years after heart transplant: A multi-site study. Rehab Psychol. 2007;52:206–214. [Google Scholar]
- 5.White-Williams C, Grady KL, Wang E, et al. Factors associated with work status at 5 and 10 years after heart transplantation. Clin Transplant. 2011 Nov-Dec;25(6):E599–605. doi: 10.1111/j.1399-0012.2011.01507.x. [DOI] [PubMed] [Google Scholar]
- 6.Grady K, Naftel D, Kobashigawa J, Chait J, Young J, Pelegrin D, Czerr J, Heroux A, Higgins R, Rybarczyk B, McLeod M, White-Williams C, Kirklin J. Patterns and predictors of quality of life at 5 – 10 years after heart transplantation. J Heart Lung Transplant. 2007;26:535–543. doi: 10.1016/j.healun.2007.01.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grady KL, Wang E, White-Williams C, Naftel DC, Myers S, Kirklin J, Young JB, Pelegrin D, Kobashigawa J, Rybarczyk B, Higgins R, Heroux A. Factors associated with stress and coping at 5 and 10 years after heart transplantation. J Heart Lung Transplant. 2013 Apr;32(4):437–446. doi: 10.1016/j.healun.2012.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grady K, Wang E, Higgins R, Heroux A, Rybarczyk B, Young JB, Pelegrin D, Czerr J, Kobashigawa J, Chait J, Naftel DC, White-Williams C, Myers S, Kirklin J. Symptom frequency and distress from 5 to 10 years after heart transplantation. J Heart Lung Transplant. 2009;28:759–768. doi: 10.1016/j.healun.2009.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bellg AJ, Grady KL, Naftel DC, et al. Patient adherence at 5 to 6 years after heart transplantation. J Heart Lung Transplant. 2003;22:S127. doi: 10.1016/j.healun.2004.08.012. [DOI] [PubMed] [Google Scholar]
- 10.Grady K, Jalowiec A, White-Williams C. Predictors of Quality of Life in Patients at 1 Year After Heart Transplantation. The Journal of Heart and Lung Transplantation. 1999;18(3):202–210. doi: 10.1016/s1053-2498(98)00048-5. [DOI] [PubMed] [Google Scholar]
- 11.Lazarus RS, Folkman S. Stress, appraisal, and coping. New York, NY: Springer; 1984. [Google Scholar]
- 12.Lund L, Edwards L, Kucheryavaya A, et al. The Registry of the International Society for Heart and Lung Transplantation: 31st official adult heart transplant report-2014. J Heart Lung Transplant. 2014;33(10):996–1008. doi: 10.1016/j.healun.2014.08.003. [DOI] [PubMed] [Google Scholar]
- 13.Jalowiec A, Grady K, White-Williams C. Stressors in patients awaiting a heart transplant. Behav Med. 1994;19:145–154. doi: 10.1080/08964289.1994.9935185. [DOI] [PubMed] [Google Scholar]
- 14.Jalowiec A, Grady K, White-Williams C, Fazekas S, Laff M, Davidson-Bell V, Florczak K, Kracht E, Wilson G. Symptom distress 3 months after heart transplant. J Heart Lung Transplant. 1997;16:604–614. [PubMed] [Google Scholar]
- 15.Grady K, Jalowiec A, White-Williams C. Patient compliance at 1 year and 2 years after heart transplantation. J Heart Lung Transplant. 1998;17(4):383–394. [PubMed] [Google Scholar]
- 16.Jalowiec A. The Jalowiec Coping Scale. In: Strickland OL, Dilorio C, editors. Measurement of Nursing Outcomes, 2nd edition. Volume 3:Self-care and coping. New York, NY: Springer; 2003. pp. 71–87. [Google Scholar]
- 17.Grady K, Jalowiec A, White-Williams C, Pifarre R, Costanzo MR, Kirklin JK, Bourge RC. Predictors of quality of life in advanced heart failure patients awaiting transplantation. J Heart Lung Transplant. 1995;14:2–10. [PubMed] [Google Scholar]
- 18.Wilson I, Cleary P. Linking clinical variables with health-related quality of life: A conceptual model of patient outcomes. J Am Med Assoc. 1995;273:59–65. [PubMed] [Google Scholar]
- 19.Sabate E. World Health Organization. Adherence to long-term therapies. Evidence for action. 2003:211. [Google Scholar]
- 20.House J, Kahn R. Measure and concepts of social support. In: Cohen S, Syme S, editors. Social Support and Health. New York, NY: Academic Press, Inc; 1985. pp. 83–105. [Google Scholar]
- 21.Cohen S, Gottlieg B, Underwood L. Social relationships and health. In: Cohen S, Underwood L, Gottlieg B, editors. Measuring and intervening in social support. New York, NY: Oxford University Press; 2000. pp. 3–25. [Google Scholar]
- 22.Breiman L. Bagging predictors. Machine Learning. 1996;24(2):123–140. [Google Scholar]
- 23.Blanche J, Sureda B, Flavia M, et al. Psychosocial adjustment to orthotopic liver transplantation in 266 recipients. Liver Transplant. 2004;10(2):228–234. doi: 10.1002/lt.20076. [DOI] [PubMed] [Google Scholar]
- 24.Jalowiec A, Grady KL, White-Williams C. Gender and age differences in symptom distress and functional disability at 1 year after heart transplant surgery. Heart Lung. 2011;40(1):21–30. doi: 10.1016/j.hrtlng.2010.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lanuza DM, McCabe M, Norton-Rosko M, Corliss J, Garrity E. Symptom experiences of lung transplant recipients: Comparisons across gender, pretransplant diagnosis, and type of transplant. Heart Lung. 1999;28:429–437. doi: 10.1016/s0147-9563(99)70032-4. [DOI] [PubMed] [Google Scholar]
- 26.Moons P, De Geest S, Abraham I, Van Cleemput J, Vanhaecke J. Symptom experience associated with maintenance immunosuppression after heart transplantation: Patients’ appraisal of side effects. Heart Lung. 1998;27:315–325. doi: 10.1016/s0147-9563(98)90052-8. [DOI] [PubMed] [Google Scholar]
- 27.Kugler C, Geyer S, Gottlieb J, Simon A, Haverich A, Dracup K. Symptom experience after solid organ transplantation. J Psychosom Res. 2009;66:101–110. doi: 10.1016/j.jpsychores.2008.07.017. [DOI] [PubMed] [Google Scholar]
- 28.De Geest S, Dobbels F, Fluri C, Paris W, Troosters T. Adherence to the therapeutic regimen in heart, lung, and heart-lung transplant recipients. J Cardiovasc Nurs. 2005;20(55):S88–S98. doi: 10.1097/00005082-200509001-00010. [DOI] [PubMed] [Google Scholar]
- 29.Germani G, Lazzaro S, Gnoato F, et al. Nonadherent behaviors after solid organ transplantation. Transplant Proceed. 2011;43:318–323. doi: 10.1016/j.transproceed.2010.09.103. [DOI] [PubMed] [Google Scholar]
- 30.Dew MA, Roth L, Thompson M, Kormos R, Griffith B. Medical compliance and its predictors in the first year after heart transplantation. J Heart Lung Transplant. 1996;15:631–645. [PubMed] [Google Scholar]
- 31.Dew MA, DiMartini A, De Vito Dabbs A, Zomak R, et al. Adherence to the medical regimen during the first two years after lung transplantation. Transplant. 2008;85:193–202. doi: 10.1097/TP.0b013e318160135f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fine RN, Becker Y, De Geest S, et al. Nonadherence consensus conference summary report. Am J Transplant. 2009;9:35–41. doi: 10.1111/j.1600-6143.2008.02495.x. [DOI] [PubMed] [Google Scholar]
- 33.Urquhart J, Vrijens B. New findings about patient adherence to prescribed drug dosing regimens: An introduction to pharmionics. Euro J Hosp Pharm. 2005;11:103–106. [Google Scholar]
- 34.Zikmund-Fisher B, Hofer T, Klamerus M, Kerr E. First things first: Difficulty with current medications is associated with patient willingness to add new ones. Patient. 2009;2(4):221–231. doi: 10.2165/11313850-000000000-00000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.De Ridder D, Schreurs K. Developing interventions for chronically ill patients: Is coping a helpful concept? Clin Psychol Rev. 2001;21:205–240. doi: 10.1016/s0272-7358(99)00046-x. [DOI] [PubMed] [Google Scholar]
- 36.White-Williams C, Grady K, Myers S, Naftel D, Wang E, Bourge R, Rybaczyk B. The relationships among satisfaction with social support, quality of life, and survival 5 to 10 years after heart transplantation. J Cardiovasc Nurs. 2013;28(5):407–416. doi: 10.1097/JCN.0b013e3182532672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dew MA, Myaskovsky L, Switzer GE, DiMartini AF, Schulberg HC, Kormos RL. Profiles and predictors of the course of psychological distress across four years after heart transplantation. Psychol Med. 2005;35(8):1215–1227. doi: 10.1017/s0033291705004563. [DOI] [PubMed] [Google Scholar]
- 38.Dew MA, DiMartini A, DeVito Dabbs A, et al. Onset and risk factors for anxiety and depression during the first 2 years after lung transplantation. Gen Hosp Psychol. 2012;34:127–138. doi: 10.1016/j.genhosppsych.2011.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dew MA, DiMartini A, De Vito Dabbs A, et al. Rates and risk factors for nonadherence to the medical regimen after adult solid organ transplantation. Transplant. 2007;83:858–873. doi: 10.1097/01.tp.0000258599.65257.a6. [DOI] [PubMed] [Google Scholar]
- 40.Misra R, Lager J. Ethnic and gender differences in psychosocial factors, glycemic control, and quality of life among adult type 2 diabetes patients. J Diab Complic. 2009;23:54–64. doi: 10.1016/j.jdiacomp.2007.11.003. [DOI] [PubMed] [Google Scholar]
- 41.Arestedt K, Saveman BI, Johaansson P, Blomqvist K. Social support and its association with health-related quality of life among older patients with chronic heart failure. Euro J Cardiovasc Nurs. 2013;12(1):69–77. doi: 10.1177/1474515111432997. [DOI] [PubMed] [Google Scholar]
- 42.Lew S, Patel S. Psychosocial and quality of life issues in women with end-stage renal disease. Adv Chron Kid Dis. 2007;14(4):358–363. doi: 10.1053/j.ackd.2007.07.003. [DOI] [PubMed] [Google Scholar]