Abstract
The present study investigated whether an 8-day intensive treatment for panic disorder in adolescents conferred a corollary benefit of ameliorating symptoms of depression. Participants included 57 adolescents between the ages of 11 and 18 who were randomly assigned to an intensive panic treatment for adolescents with or without parental involvement. Paired samples t tests and hierarchical linear models (HLM) indicated that participants' total depression score and scores on depression subscales declined from baseline to the 3-month follow-up. Additional HLM analyses indicated that the interaction term between age and parent involvement was a significant moderator in the negative slope for adolescent depression, with younger participants benefitting more from treatment without parent involvement than older participants with regard to depression symptoms.
Keywords: Panic disorder, Adolescents, Depression, Cognitive-behavioral therapy, Family treatment
Introduction
Cognitive-behavioral therapy (CBT) has been shown to be an efficacious treatment for anxiety with a large effect size (Beidel et al. 2007; In-Albon and Schneider 2006; Kendall et al. 2008; Walkup et al. 2008). In addition to treatment-related reductions in anxiety, CBTs focused on treating adult anxiety disorders in general (Davis et al. 2010) and adult panic disorder (PD) specifically (Allen et al. 2010) have been found to ameliorate broader negative emotional symptoms, such as depression. Despite the tremendous impairment and interference associated with adolescent PD (Ollendick and Pincus 2008), regrettably few studies have examined such broadened effects of treatment for PD on depression in younger populations. In one rare exception, Pincus et al. (2010) found in a small sample (13 in the treatment group and 13 in the control group) that treatment for adolescent panic reduced symptoms of depression, but this study only examined the impact 6 weeks post-treatment, and there is little information on whether these benefits would be maintained.
Though CBT for childhood anxiety disorders is generally effective (Beidel and Alfano 2011; In-Albon and Schneider 2006; Kendall et al. 2008; Walkup et al. 2008), the presence of depression predicts poorer treatment response (Berman et al. 2000). Unfortunately, the rate of concurrent anxiety and depressive symptomatology is high, as is the rate of diagnoses of comorbid depression and anxiety (Garber and Weersing 2010; O'Neil et al. 2010). Adolescents with PD are even more likely to be diagnosed with comorbid depression compared with those suffering from other disorders (Kearney et al. 1997). Moreover, adolescents suffering from untreated PD are at increased risk for attempted suicide in later adolescence and adulthood (Boden et al. 2007), and reduced health-related quality of life more broadly (Comer et al. 2011). Effective treatments for adolescent PD that can also ameliorate symptoms of depression would, therefore, be particularly valuable.
Researchers have expected that educating parents in the process of treating their children's anxiety disorders may benefit their children's treatment process (Barmish and Kendall 2005). Studies have, therefore, increasingly included a family involvement component in child anxiety treatment (Barmish and Kendall 2005; Bögels and Siqueland 2006; Comer et al. 2012; Hughes et al. 2008; Kendall et al. 2008; Rapee 2012). While these reasons are compelling, there is mixed evidence regarding whether direct parental involvement actually confers additional benefits for their children (Drake and Ginsburg 2012; Ginsburg et al. 2004; Kendall et al. 2008; Silverman et al. 2009). A few studies have shown long-term positive benefits, particularly when parents show elevated symptoms of negative emotion and receive direct teaching of parental management of their own anxiety (Cobham et al. 2010; Creswell and Cartwright-Hatton 2007). Other investigations of individual versus family-based CBT for children with separation anxiety disorder, social phobia, or generalized anxiety disorder have indicated that treatment can confer secondary benefits on depression symptoms (Suveg et al. 2009). Some studies, however, have found little additional benefit to including family in cognitive behavioral therapy (FCBT) over child cognitive behavioral therapy (CCBT) alone—at least in studies with children above the age of 7 (In-Albon and Schneider 2006; Kendall et al. 2008; Silverman et al. 2009). Speculation concerning these null findings is varied. Some have suggested that most of these studies have had statistical power which was insufficient to detect these relatively small effect sizes (Creswell and Cartwright-Hatton 2007; Rapee 2012). It is also possible that moderating effects (such as age and gender) mask the superiority of one treatment over another for certain children under certain circumstances (Barmish and Kendall 2005; Creswell and Cartwright-Hatton 2007; Drake and Ginsburg 2012; Hudson et al. 2002; Rapee 2012). In particular, it has been suggested that FCBT may be inappropriate for adolescents, given their growing need for independence and autonomy (Barmish and Kendall 2005).
Previous studies assessing the benefit of a panic control treatment for adolescents indicated that an 11 week manualized treatment was efficacious in reducing panic as well as self-reported symptoms of general anxiety and depression (Pincus et al. 2010). Because participants in this original study expressed interest in the possibility of a shorter-term treatment, an intensive treatment program was developed. This short-term intensive panic treatment with in vivo exposures was administered to adolescent participants over eight consecutive days for 2–6 h each day. This intensive treatment for PD has been found to reduce the rate and severity of PD. Adolescents participating in this intensive treatment protocol reported a significant decline in their fear and avoidance ratings between the beginning and the conclusion of treatment. Additionally, their therapists reported a decline in their panic severity as measured by a seven- point PD Severity Scale (Gallo et al. 2014; Pincus et al. in preparation). This intensive protocol was also found to reduce the number of comorbid clinical disorders, especially specific phobias, generalized anxiety disorder, and social phobia (Gallo et al. 2012). Based on a clinical severity rating using diagnostic interviews, only four of these participants were clinically diagnosed with a mood disorder. Using this criterion, there was no significant change in the diagnostic status of the participants at the 6 week follow-up assessment. The Clinical Severity Ratings (CSRs; ranging from 0 to 8) for major depressive disorder (MDD) of these four participants were, however, reduced from an average of 4.75 to an average of 1.50. The authors of this study suggested that the full effects of CBT on depression may take longer than 6 weeks to emerge. Additionally, the study did not examine whether treatment reduced rates of subsyndromal depression and continuous depressive symptomatology across all the participants; rather, only the small handful of participants whose CSRs warranted a full diagnosis of MDD at baseline assessment were evaluated (Gallo et al. 2012; Pincus et al. in preparation).
The current study examined the extent to which this intensive treatment for PD addressed continuous depressive symptomatology as measured by the Children's Depression Inventory (Kovacs 1992) at a 3-month follow-up. We hypothesized that this intensive treatment would significantly reduce symptoms of depression. Additionally we examined the extent to which these effects were moderated by enhanced parental involvement in their adolescents' treatment. While a recent meta-analysis examining the relative benefit of including parents in child treatment has identified some potential long-term benefit of family participation in CBT (Manassis et al. 2014), the findings on parental involvement in their children's therapy have generally been inconclusive (Breinholst et al. 2012; Manassis et al. 2014). Additionally, we were unaware of any studies that included a full range adolescent ages (both older and younger) in treatment of PD, despite the fact that reviewers of such research have suggested that the age of the participant might moderate the effectiveness of parental involvement in therapy (Rapee et al. 2009). We were, therefore, cautious in making any specific hypotheses regarding the effects of parental involvement in their adolescents' therapy.
Method
Participants
Participants in the study were 57 adolescents (34 girls and 23 boys) aged 11.83–17.83 (M = 15.42, SD = 1.70) who completed an intensive treatment for PD (Pincus et al. in preparation). Adolescents were recruited to this study both locally (through referrals to an outpatient, university-based research clinic specializing in child anxiety treatment) and nationally (through referrals from mental health and health professionals around the country as well as referrals from a panic informational website for teenagers designed specifically for this study) to participate in a treatment study examining the efficacy of an 8-day intensive treatment program for adolescents with PD, with or without agoraphobia. Local and nationwide recruitment efforts included community talks at local high schools, hospitals, and clinics and through advertising in internet and print media around the country. Some participants were referred to the study through their pediatricians, social workers, or from other psychologists.
These 57 participants completed the intensive treatment and were a subset of 63 participants who volunteered for the treatment trial. Of the original 63 participants, four participants dropped out after randomization but before treatment began. Reasons that participants dropped before the treatment began included being initially assigned to a waitlist period of 6 weeks (n = 3) or dropping out after randomization because they were not from the local area (n = 1). Two individuals dropped after beginning the treatment (one individual from the group with direct parental involvement dropped after Day 3 of the treatment, and another individual from the individual treatment group dropped after Day 1). Assignment to direct parental involvement in therapy did not predict the likelihood that adolescents would complete the intensive therapy protocol, χ2 (1, N = 63) = .81, n.s; 87.1 % (27/31) participants whose parents were not directly involved with therapy completed the protocol and 93.8 % (30/32) participants whose parents were directly involved with the therapy protocol completed the protocol.
All participants were informed of the potential risks and benefits of participation and given a complete overview of the study. Adolescent participants were enrolled in the study if they provided informed assent (including assent to have their parents potentially involved with their therapy sessions) and at least one parent or caregiver also provided signed informed study consent. Additionally, participants were only enrolled in the study if at least one parent or guardian was available and willing to participate directly in the therapy sessions. The majority of adolescents completing treatment reported that they were of Caucasian descent (86 %). Over half of those participating reported their annual family income which ranged from $25,000 to $500,000; the median reported income was $95,000 (M = 112,419, SD = 92,104). Forty-three participants reported whether or not they were currently taking any psychotropic medications; of these, 60.5 % reported use of at least one medication, and 39.5 % reported no use of such medication.
All adolescents had a primary diagnosis of PD with or without agoraphobia (PDA) as determined by the Anxiety Disorders Interview Schedule—Child and Parent Versions (ADIS-IV-C/P; Silverman and Albano 1997), a structured diagnostic parent and child interview. Based on a composite of the parent and adolescent report, this PDA diagnosis was assigned when the clinician-assigned clinical severity rating (CSR) was four or greater. As reported elsewhere, the majority of participants in this study examining the impact of intensive therapy on PDA met the criteria for at least one other comorbid disorder, but very few of them met the criteria for MDD (Gallo et al. 2012). Participants also included mothers (n = 53) and fathers (n = 44) of the 57 adolescents. Both parents completed self-report measures and were included in the parent ADIS-IV-C/P interview whenever possible and both parents were invited to participate in treatment; however, at least one parent or caregiver was required to participate in the parental involvement condition. Exclusion criteria included any positive diagnosis of pervasive developmental disorder, schizophrenia, organic brain syndrome, intellectual disability, or current suicidal ideation; parental refusal to accept treatment conditions or random assignment; unavailability of the parent or caregiver with whom the adolescent was living to bring the adolescent in for treatment; or adolescent or parental refusal to accept the stabilization of medication prior to their initial diagnostic assessment for 1 month for any benzodiazepines and three-months for SSRIs or tricyclic medication. These procedures were approved by the Institutional Review Board at Boston University's Charles River Campus.
Procedures
Eligible participants completed an intensive format of the Riding the Wave treatment protocol for adolescent panic (Pincus et al. 2008) with in vivo exposures, a 20 h, 6-day CBT that spanned a consecutive 8-day period. Therapists for the present study were either MA level doctoral students in clinical psychology or Ph.D. level psychologists. Approximately 13 therapists administered the protocol and all had background training and expertise in treatment of PD in youth. Therapist training included reading the therapist manual, which provided information on how to present the information in each session, and shadowing one senior therapist as he or she treated one intensive panic case. Adolescents completed Adolescent Intensive Panic treatment without parental involvement (AIP; n = 27) or Adolescent Intensive Panic treatment with parental involvement (AIP + FAM; n = 30). Participants in both treatment protocols received psychoeducation regarding the nature of anxiety, including information on the physiology of anxiety and panic and skills to engage in cognitive restructuring regarding anxiety-provoking stimuli. In both conditions, adolescent participants received homework assignments and self-study reading materials to complete each evening. All participants learned about interoceptive conditioning and were guided by the therapist to engage in a series of a interoceptive exposures through which participants learned that the physiological sensations associated with panic are not life threatening or dangerous and that these sensations diminish over time (see Angelosante et al. 2009 for more details regarding protocol implementation). Participants were also taught about the concept of situational exposures, and they developed a personalized “Fear and Avoidance Hierarchy,” (FAH), which consisted of a list of avoided situations due to panic. Using the situations adolescents had listed on their FAHs, therapists helped teens enter previously avoided situations and guided them toward reaching the most avoided situation as quickly as possible. Participants receiving AIP participated in sessions with only the therapist present, except the penultimate 2 days of therapy in which they completed exposures independently. The final session included a treatment review with the adolescent and a plan for continuing practice after the conclusion of formal treatment.
Participants assigned to AIP + FAM followed a similar protocol; however, at least one parent or guardian was included in all phases of the treatment. Parents in AIP + FAM condition were educated about the nature of PD and taught ways in which they might effectively “coach” their children to engage in exposures. The AIP + FAM condition was conducted similarly to the AIP without FAM condition, except that parents were included in specific portions of all sessions so that they could learn panic-reduction skills to help their adolescents. Specifically, parents were included in the last 30 min of Sessions 1–3 to teach them the specific anxiety-related skills the adolescents had learned. Adolescents were asked to summarize the session content for their parents; this also helped the therapist to know that the adolescent learned the material. Parents were also provided with their own psychoeducational handouts, on behavioral principles for parenting anxious youth, on limit setting, and on what to do when a child is experiencing a panic attack. During the last 30 min of Session 3, the session on interoceptive exposures, parents were asked to conduct several symptom induction exercises with their adolescent. Parents were also asked to complete homework assignments that paralleled the assignments that the teen was completing. Additionally, therapists taught parents how to effectively conduct a panic exposure practice, and parents were instructed how to initiate such exposures with their adolescent without becoming overly intrusive or overly involved. Parents were also taught behavioral concepts such as differential reinforcement of anxious versus brave behaviors, and were taught to support adolescents' successes and encourage adolescents' continued progress without inadvertently reinforcing anxious or avoidant behavior. During Sessions 4 and 5, adolescents conducted situational exposures with therapist accompaniment and for the following 2 days, the adolescent conducted exposures without therapist guidance but with parent as “coach” for some of the exposures. During the final session of treatment, the therapist met with the adolescent and parent to review adolescents' progress and to discuss plans for future exposure practices. Thus, in this AIP + FAM condition, therapists treated the adolescent individually while engaging parents or caregiver(s) as trained “coaches.”
The first 3 days of treatment (Sessions 1–3) lasted 2 h each. Days 4 and 5 of treatment lasted approximately 6 h each. Days 6 and 7 of treatment were days in which the adolescent (in the AIP group) or the adolescent and parent (in the AIP + FAM group) conducted exposures without the therapist. The adolescents in the AIP + FAM group also conducted some of these exposures entirely on their own. The final day of treatment (Day 8) lasted 2 h. A complete review of the structure of sessions and details about parent involvement is described in Angelosante et al. 2009. Participants' levels of anxiety and depression were assessed before treatment began (pretreatment). They were assessed again 6 weeks after the conclusion of the intensive treatment protocol (post-treatment) and then 3 months later (3 month follow-up).
Measures
Children's Depression
To assess symptoms of adolescent depression, participants completed the Children's Depression Inventory (CDI; Kovacs 1992). The CDI is a 27 item measure which yields a total score as well as scores on five subscales: negative mood, interpersonal problems, ineffectiveness, anhedonia, and negative self-esteem. The scale is appropriate for respondents aged 7–17. Scores range from 0 to 54, with higher scores indicating greater depression severity. Previous research supports the use of the CDI as a continuous measure of depressive symptoms in samples of anxious youth (Comer and Kendall 2005). Kovacs (1992) has suggested that, among a clinically referred sample, a score of 12 or 13 represents a reasonable clinical cutoff for depression. Table 1 lists participants' total CDI scores and average scores for each of the subscales across the three assessments, pretreatment, post-treatment and the 3 month follow-up assessment.
Table 1. Descriptive statistics and ns for study variables across three assessment periods.
| Pretreatment M (SD) n = 53 | Post-treatment M (SD) n = 38 | 3 month follow-up M (SD) n = 33 | |
|---|---|---|---|
| Child depression inventory (total) | 12.67 (7.54) | 10.47 (8.36) | 9.51 (8.29) |
| CDI negative mood score | 3.38 (2.15) | 2.95 (3.03) | 2.52 (2.69) |
| CDI interpersonal problems score | .89 (1.05) | .63 (.97) | .58 (1.00) |
| CDI ineffectiveness score | 2.11 (2.03) | 1.87 (1.74) | 1.72 (1.85) |
| CDI anhedonia score | 4.33 (2.73) | 3.63 (2.97) | 3.36 (2.55) |
| CDI negative self-esteem score | 1.96 (1.56) | 1.39 (1.41) | 1.33 (1.61) |
Child Anxiety Disorder Diagnosis and Severity
Clinical severity ratings (CSRs) for the principal diagnosis of PD were assigned based on parent and child interview using the ADIS-IV-C/P (Silverman and Albano 1997). The ADIS-IV-C/P assesses internalizing disorders and common behavioral disorders following parameters set out by the DSM-IV. Study team training involved didactic training, viewing live interviews, completing two interviews in collaboration with a trained interviewer, and then conducting interviews independently. In order to be certified to conduct interviews independently, interviewers were required to complete three interviews and generate diagnostic profiles which matched diagnostic profiles generated by a trained observer. Overall, the site inter-rater agreement on primary diagnosis (κ = .87) and clinical severity (r = .62) was high. Based on information from the combined parent and child interviews, a CSR of 0–8 was assigned, with 0 indicating that the participant shows an absence of any symptoms associated with the diagnosis, and eight indicating that symptoms associated with the diagnosis are very severe, the individual is experiencing intense distress, and the diagnosis is highly interfering with normal functioning. CSR scores of 3 and below reflect subclinical manifestations of disorder.
Data Analysis
To investigate the extent to which intensive treatment for adolescent panic also addressed child depressive symptoms, we analyzed the data in several steps. For each outcome, we evaluated whether participants' depression scores showed significant change between the baseline and 3 month follow-up assessments in two steps. First, we assessed whether participants' level of depression scores at the 3 month follow-up assessment differed significantly from their baseline score by conducting a series of paired samples t-tests. We then evaluated the overall slope of change across the 3 assessments (pretreatment, post-treatment, and 3 month follow-up) by fitting hierarchical linear models (HLM; Bryk et al. 1996). The full maximum likelihood estimation offered through HLM makes it possible to address challenges often presented when data analysis includes missing data, under the missing at random (MAR) assumption (Schafer and Graham 2002), which is common in the analysis of clinical trial data. For each model, two sets of equations were fit simultaneously; Level 1 equations represented the repeated measures of each participant, and Level 2 equations represented individual differences for the overall sample (Atkins 2005). The equations predicting a participant's score at a particular assessment was:
Level 1 equation:
| (1) |
In these equations, each outcome measure was modeled for the individual participant (j) across each of the three assessments (i) as a functioning of the intercept for that individual (b0j) as well as their slope over time (b1j). For the combined sample of participants, the Level 2 basic equations were:
Level 2 equations:
| (2) |
| (3) |
After examining whether baseline scores significantly differed from scores at the 3 month follow-up, we performed additional HLM analyses to examine the extent to which parent involvement in treatment moderated change across the three assessments by including potential moderators in the Level 2 equations and examining whether the slope of change differed by parent involvement in treatment (i.e., AIP vs. AIP + FAM), age of participant, or an interaction between the two.
Results
Similarity Between Groups
Post-randomization
We examined whether participants assigned to the parent involvement group (AIP + FAM) differed significantly from participants assigned to the individual group (AIP) prior to the beginning of treatment through a series of Analyses of Variance (ANOVAs) and Chi Squares. Participants did not differ in their age, pretreatment CDI levels, or PD CSRs F(1, 51–55) = .02–2.13, n.s. Gender was also similarly distributed across the three groups χ2 (1, N = 57) = .36, n.s. Of the 57 participants, 38 mothers and 37 fathers reported their education levels, and parental education did not differ between the two groups χ2 (1, Ns = 38; 37) = .90; .26, n.s. Reported family income was also similar between the parent involvement and individual therapy groups, F(1, 29) = .47, n.s. Parents' age did, however, differ between the two groups. The average age of mothers in the parental involvement group was 44.91 (SD = 5.29) and the average age for mothers whose adolescents were in the individual therapy group was 48.81 (SD = 6.22), F(1, 47) = 5.50, p < .05. Differences in paternal ages were marginally significant, the average for the parental involvement group was 47.87 (SD = 5.88) and the average age of fathers whose adolescents were in the individual therapy group was 51.00 (SD = 6.89), F(1, 46) = 2.84, p < .10. Because there were differences in the ages of parents between the two groups, we examined whether parental age was correlated with the change in adolescents' CDI scores between their pretreatment assessments and their 3 month follow-up scores. To accomplish this, we calculated the difference between 3 month and pretreatment CDI scores and examined the correlations between this change and mothers' and fathers' ages. In both cases, the correlations were non-significant r = −.04 and −.09, n.s. Because the difference of age was rather small, and parents in both groups were at similar points in their life courses (all groups were middle aged), and because parental age was not associated with change in CDI, we proceeded with analysis between the two groups.
Missing Data
Of the 57 participants who completed the 8-day, intensive treatment, 33 returned for the 3-month follow-up assessment. To examine the differences between the group of 24 participants who did not return for this assessment and the 33 who did return, we conducted a series of One Way Analyses of Variance (ANOVAs) using their status of whether or not they returned for the 3 month assessment as a between subjects variable. These analyses indicated that the group who returned for assessment did not differ significantly from the group who finished treatment but did not return in their pretreatment CDI and CSR scores, the ages of their parents, or the level of family income F(1, 29–55) = .05–.50, n.s.
Changes in Adolescent Depression between Pretreatment and 3 Month Follow-up
Paired Samples t Tests
The mean baseline CDI for the sample fell within the 12–13 clinical cutoff range (Kovacs 1992; Matthey and Petrovski 2002), suggesting elevated symptoms of depression on average among the sample. Paired samples t tests supported the hypothesis that adolescents' depression scores would decline significantly from pretreatment to the 3 month follow-up (see Table 2). Analysis of CDI sub-scale scores indicated that the treatment was particularly effective for improving adolescents' negative mood, interpersonal problems, and negative self-esteem.
Table 2. t tests and HLM slopes indicating change in symptoms of depression across the 3 month assessment.
| Pretreatment measurement M (SD) | Paired difference Pretreatment to 3 month follow-up M (SD) | Pretreatment to 3 month follow-up | HLM slopes (SE) | HLM slope | |
|---|---|---|---|---|---|
| CDI total depression score | 12.86 (8.50) | 3.67 (7.70) | t(31) = 2.69* | −1.84 (.62) | t(122) = −2.98** |
| CDI negative mood score | 3.38 (2.25) | 1.00 (2.60) | t(31) = 2.17* | −.48 (.21) | t(122) = −2.26* |
| CDI interpersonal problems score | .91 (1.15) | .31 (.86) | t(31) = 2.06* | −.18 (.07) | t(122) = −2.59* |
| CDI ineffectiveness score | 2.16 (2.27) | .47 (1.70) | t(31) = 1.56 | −.22 (.13) | t(122) = −1.68+ |
| CDI anhedonia score | 4.26 (2.88) | .95 (3.02) | t(31) = 1.78+ | −.51 (.24) | t(122) = −2.17* |
| CDI negative self-esteem score | 2.16 (1.74) | .94 (1.34) | t(31) = 3.95*** | −.44 (.11) | t(122) = −4.02*** |
N = 33–57 individuals, SE = Robust standard errors for slopes
p<.10;
p< .05;
p < .01;
p < .001.
Hierarchical Linear Models
Using HLM multilevel analyses, we modeled the slope for adolescents' change in total depression and scores on each of the subscales across all three assessment points (pretreatment; post-treatment, and the 3 month follow-up). These models supported the findings from the t tests; slopes for the total depression score, negative mood, interpersonal problems, anhedonia, and negative self-esteem all showed a significant linear decline from baseline to the 3 month follow-up assessments (see Table 2 for HLM slopes and associated t tests). As can be seen in Table 2, HLM slopes show significant declines for the total depression, negative mood, interpersonal problems, anhedonia, and negative self-esteem scores. Findings from the paired-samples t-tests are largely consistent with these findings, but the significant HLM negative slope for anhedonia corresponds to a marginally significant paired-samples t test difference for that outcome. This can be explained by the way in which HLM models are fit to the data across the three assessments. Hierarchical Linear Modeling relies on the Maximum Likelihood estimation, and therefore, all of the available data can be used to fit the model (Schafer and Graham 2002), whereas the paired samples t test relies only on complete cases between the pretreatment and the 3 month follow-up assessments.
Moderation of Effects by Parent Involvement Group or Age of Adolescent
To examine whether parent involvement in therapy or the interaction between parent involvement and the age of the child impacted the decline of depression scores, follow-up HLM analyses included AIP versus AIP + FAM as a predictor in the Level 2 equations according to the following:
Level 2
| (4) |
| (5) |
Treatment assignment did not significantly moderate the rate of adolescent depression change for any of the CDI subscales across the three assessments (pretreatment, post-treatment, and the 3 month follow-up), suggesting that there were no main effects on youth depression for including parents in therapy and neither treatment protocol conferred better outcomes on adolescent depression t(120) = −.05–.1.02, n.s.
We also examined whether parent involvement in treatment interacted with the age of the participant to predict better depression outcomes for younger versus older adolescents. Models were fit according to the following Level 2 equations:
Level 2
| (6) |
| (7) |
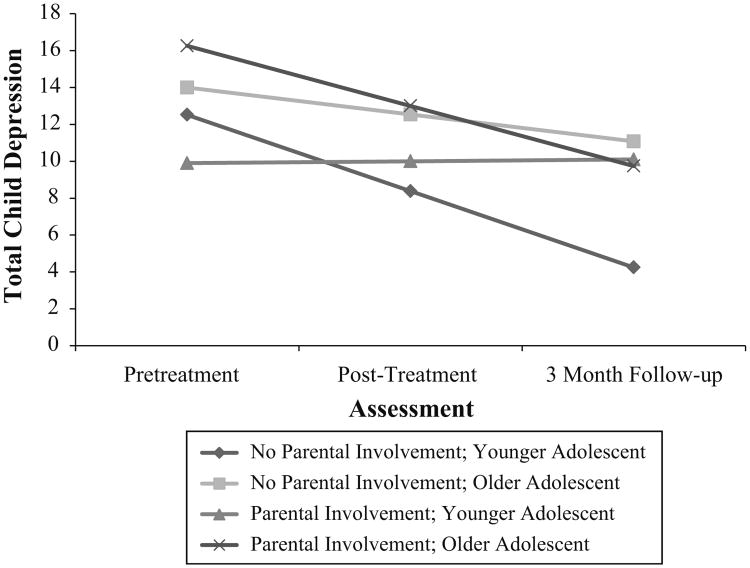
As portrayed in Fig. 1, the interaction term between age and parent involvement was a significant moderator in the negative slope for adolescent depression, with younger participants benefitting more from individual treatment than older participants with regard to depression symptoms, t(1,116) = −2.39, p < .05.
Fig. 1.
Adolescent age and parental involvement in treatment predicting total depression. Parental involvement reference group was coded as 0. Younger adolescents, a continuous variable, are represented in the graph as 13 years of age and older adolescents are represented as 17 years of age. Coefficients for the overall slope for time was −12.85, SE = 7.75, t(116) = −1.68, p < .10; the parental involvement coefficient was 23.87, SE = 9.72, t(116) = 2.46, p < .05; coefficient for age was .67, SE = .46, t(116) = 1.44, n.s. The age and family involvement interaction coefficient was −1.51, SE = .63, t(1,116) = −2.39, p < .05
To further examine the extent to which parental involvement affected adolescents' responses to treatment, we split the treatment completers into two age groups with a median age split of 15.42 years of age. We next calculated the change scores on the CDI by subtracting the final total CDI scores at the 3 month assessment from participants' pretreatment CDI scores. Two-way ANOVAs using participants' age grouping and parental involvement in therapy as between subjects variables confirmed the findings from the HLM analyses, indicating that there was a significant interaction effect between adolescent age and parental involvement, F(1,28) = 4.67, p < .05, η2 = .14. Among the older adolescents, the CDI scores of the nine participants whose parents were directly involved with therapy declined an average of 5.82 (SD = 8.33) points, and the seven participants whose parents were not directly involved with therapy declined an average of 2.86 (SD = 5.76) points. Among the younger adolescents, the CDI scores of the 12 participants whose parents were directly involved in therapy declined an average of .50 (SD = 6.01) points, and the decline of the CDI scores of the four participants whose parents were not directly involved in therapy was an average of 9.75 (SD = 11.15) points.
We investigated whether this decline in CDI scores among these 33 participants was attributable to some other feature of treatment or pretreatment differences between the groups. To examine whether the use of psychotropic medications was responsible for adolescents' improvement, we performed a one-way ANOVA, using use of psychotropic medication as a between subjects variable and decline in CDI scores as an outcome; this analysis indicated that use of medications did not predict this change over time F(1,26) = .91, n.s. We also performed analyses on group-level differences in 3 month levels of PD to investigate whether differences in the CSRs of the principal diagnosis were connected to the accompanying differences in adolescent depression at the 3 month follow-up assessment. The interaction between parental involvement and adolescent age predicting the CSR scores was not significant, F(1, 29) = .00, n.s. Adolescents in all four groups had an average CSR score in the subclinical range between an average of 1.43 (the average of older adolescents whose parents had not directly participated in therapy) and 2.41 (younger adolescents whose parents had directly participated in therapy). Moreover, adolescents in the four groups did not differ in their pretreatment CSR or CDI levels. The interaction between parental involvement group and adolescent age group at the pretreatment CSR assessment was not significant F(1, 29) = .28, n.s., and neither was the interaction term for the pretreatment CDI levels F(1, 28) = 1.26, n.s., indicating that these groups did not differ in their levels of panic or depression before treatment began.
To determine whether participation in the 3 month follow-up assessment differed for adolescents whose parents had participated directly in therapy compared to those who had not, we performed Chi Squares tests. Direct parental involvement in treatment marginally predicted differences in the likelihood for participants to return for this 3 month follow-up assessment. Of the 57 participants who completed therapy, 70.0 % (21/30) from the parental involvement group returned for the 3 month assessment compared with 44.4 % (12/27) from the adolescent-only, individual therapy group χ2 (1, N = 57) = 3.81, p = .051.
Discussion
The first goal of this study was to examine whether intensive treatment for PD also reduces symptoms of depression among adolescent participants. Overall, we found that the impact of short-term, intensive treatment for adolescent PD extends beyond the reduction of adolescent PDA symptoms and diagnosis (see Gallo et al. 2014; Pincus et al. in preparation) and that such treatment can more broadly ameliorate symptoms of depression. Both AIP and AIP + FAM alleviated adolescents' overall symptoms of depression, especially in the areas of negative mood, interpersonal problems, anhedonia, and negative self-esteem. The current study provides further support to a growing body of work suggesting that CBT provides broadened benefits beyond anxiety in the treatment of anxiety disorders (Davis et al. 2010; Ehrenreich-May and Bilek 2012; Gallo et al. 2012). It also supports previous studies which have found that treatment for PD reduces symptoms of depression (Pincus et al. 2010). Identifying that short-term intensive treatment for adolescent PD can also reduce symptoms of depression is particularly important, given that adolescents with PDA are more likely to meet criteria for comorbid depression (Kearney et al. 1997) and therefore are at greater risk for other emotional and health-related problems (Hirschfeld 1996; Kovacs and Devlin 1998).
The mechanisms whereby this intensive treatment conferred additional benefits on depressive symptoms for adolescents may be similar to those proposed in the treatment of adults. Research on the high comorbidity between depression and anxiety suggests that negative affect is common to both, with PD containing an additional element of anxious arousal (Mineka et al. 1998). It is possible that in addition to helping treated adolescents control their panic symptoms, the present treatment more broadly helped participants improve their overall abilities to regulate negative affect (Allen et al. 2010; Garber and Weersing 2010; Trosper et al. 2012). Depression and anxiety both involve negative and maladaptive cognitions and ruminations (Garber and Weersing 2010). Skills learned during the course of this intensive CBT for panic, including cognitive restructuring, monitoring of internal states, and exposure to feared experiences, may have generalized to combat other emotional difficulties like depressive cognitive activity (Allen et al. 2010; Ehrenreich-May and Bilek 2012). Additionally, adolescents with PD are less likely to engage in normative activities outside the home (Kearney et al. 1997). Returning participants' to normal adolescent activities as a consequence of successful PD treatment may also provide for behavioral activation, itself an effective treatment for depression (Chu et al. 2009; Ehrenreich-May and Bilek 2012). Alternatively, the “cause” of the depressive symptoms may have been the PD itself and alleviating this root cause also alleviated participants' depressive symptoms (Allen et al. 2010).
Importantly, findings from this study also extend the current understanding of possible moderating effects of parent involvement in the treatment of PD, which has received less attention in this regard than the treatment of other anxiety disorders, such as specific phobias (Ollendick et al. 2010), obsessive compulsive disorder (Waters et al. 2001), and social anxiety disorder (Spence et al. 2000). This paper also heeded the calls to examine the circumstances under which direct parent involvement in therapy was beneficial to their children's progress. More specifically, we considered the moderating effects of age when examining enhanced parent involvement in anxiety treatment for children and adolescents (Creswell and Cartwright-Hatton 2007; Hudson et al. 2002; Rapee 2012). While we found that there were no main effects indicating a benefit or detriment to parent's involvement in therapy, we did find that younger adolescents benefitted more when their parents were not involved directly in therapy. This is perhaps unsurprising, given the nature of the relationships that parents have with their younger adolescents, who are just beginning to face independence and perhaps have an increasing need for autonomy (Eccles et al. 1991; Hudson et al. 2002; Steinberg and Silk 2002). Indeed, the transition to adolescence that occurs around the age of 13 is marked by disequilibrium in the parent–child relationship as a response to many factors including the onset of puberty and an increased set of expectations placed on the adolescent from forces both within and outside of the family. As children move through their adolescence, many theoretical models suggest that the parent–child relationship establishes a new equilibrium (Steinberg and Silk 2002), and generally, the number of conflicts between adolescents and their parents increase dramatically as children enter adolescence but falls again as children progress through adolescence (Granic et al. 2003). These findings are consistent with those of previous research which has also suggested that the inclusion of parents in treatment with younger adolescents may not provide specific benefits to adolescents. For example, anxiety in younger children (aged 7 through 10) was better addressed by FCBT compared with CCBT, but young adolescents (aged 11–14) showed little difference in their response based on parental involvement (Barrett et al. 1996; Rapee et al. 2009). As children transition to adolescence, issue of autonomy and independence become prominent in the parent–child relationship, and this may be a developmental period in which parents are generally less well-positioned to help their children benefit from CBT.
This study also extends the age range of participants through later adolescence, thus filling an important gap in the literature, including parents in the therapy of their children at an older age than in many studies which have largely focused on children up to age 13 (Ginsburg et al. 2004). Our findings suggest that older adolescents respond similarly to CCBT and FCBT. Older adolescents, perhaps having reached a new equilibrium in their relationships with parents (Granic et al. 2003; Steinberg and Silk 2002), may be able to benefit from their support in therapy. While younger adolescents may have benefitted more from the increased autonomy afforded to them when their parents were not involved directly in their therapy, older adolescents may have benefitted from a more gradual “transfer of control,” whereby therapeutic ownership is gradually transferred from the therapist to the child, or in the case of family-based treatment, from the therapist to the parent to the child (Barmish and Kendall 2005; Manassis et al. 2014; Ginsburg et al. 1995). In this protocol, parents were also taught both about the importance of differential contingency reinforcement and ways to avoid unintentionally reinforcing harmful behaviors, often referred to as contingency management in FCBT (Manassis et al. 2014). More research is required to identify the specific mechanisms which may be responsible for any benefit older adolescents might have experienced due to their parents' involvement in treatment, as it could be that parents learned differential reinforcement; it could be that parents learned not to facilitate avoidance; or it could be that the education parents received about panic was what helped them to encourage their child to approach new situations.
Direct parental involvement in therapy may, however, lead to more consistency in adolescent interactions with the therapist. Indeed, while young adolescents seem to benefit more when their parents did not participate in therapy, all adolescents were also less likely to return for the 3 month assessment when their parents had not directly participated in the therapy itself. The higher rate of attrition among participants whose parents had not been involved in treatment limits the clinical interpretation of these data. Though the results from the HLM models fit age as a continuous measurement and indicated that younger adolescents showed more benefit when parents were not involved in therapy, the median-age split between younger and older adolescents performed to examine group-level differences with the two way ANOVAs left only four participants in the younger adolescent-no parental involvement group. This small number of participants necessarily limits the conclusions that can be drawn from this data. Future studies should include a larger number of participants and also examine whether parents who are not directly involved in therapy could be effectively encouraged to provide consistency in their adolescents' participation in therapy and its follow-up assessments. Several other limitations merit consideration. The study included a relatively homogenous sample, and only a few participants met full diagnostic criteria for MDD. The present work also relied on child self-reports. Future work in this area would benefit from inclusion of multimodal assessments, including structured individual and family behavioral observations and physiological data.
Findings from the current study have several important implications. Because of the risk of depression associated with PD among adolescents (Kearney et al. 1997), identifying short-term treatments which also ameliorate symptoms of depression are particularly beneficial. Given that less than half of the adolescents who suffer from debilitating mental health disorders receive mental health services (Merikangas et al. 2011), there is a critical need to identify effective short-term treatments with the potential to reach increasingly wider ranges of affected adolescents. The present study adds to a growing literature suggesting that intensive treatment formats, which can improve treatment options for affected populations in geographic regions lacking local evidence-based treatment, are effective in reducing rates and symptoms of primary diagnoses and secondary concerns (e.g., Ollendick et al. 2010; Santucci et al. 2009). These findings highlight the generalized impact that intensive treatments for adolescent PD can have on symptoms of depression and underscore the critical need to broaden access to effective care for affected families.
Contributor Information
Christina L. Hardway, Email: hardwayc@merrimack.edu, Department of Psychology, Merrimack College, 315 Turnpike Street, North Andover, MA 01845, USA.
Donna B. Pincus, Departmentof Psychological and Brain Sciences, Center for Anxiety and Related Disorders, Boston University, Boston, MA, USA
Kaitlin P. Gallo, The Child Study Center at NYU LangoneMedical Center, New York University, New York, NY, USA
Jonathan S. Comer, Center for Children and Families, Florida International University, Miami, FL, USA
References
- Allen LB, White KS, Barlow DH, Shear M, Gorman JM, Woods SW. Cognitive-behavior therapy (CBT) for panic disorder: Relationship of anxiety and depression comorbidity with treatment outcome. Journal of Psychopathology and Behavioral Assessment. 2010;32:185–192. doi: 10.1007/s10862-009-9151-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angelosante AG, Pincus DB, Whitton SW, Cheron D, Pian J. Implementation of an intensive treatment protocol for adolescents with panic disorder and agorophobia. Cognitive and Behavioral Practice. 2009;16:345–357. doi: 10.1016/j.cbpra.2009.03.002. [DOI] [Google Scholar]
- Atkins DC. Using multilevel models to analyze couple and family treatment data: Basic and advanced issues. Journal of Family Psychology. 2005;19:98–110. doi: 10.1037/0893-3200.19.1.98. [DOI] [PubMed] [Google Scholar]
- Barmish AJ, Kendall PC. Should parents be co-clients in cognitive-behavioral therapy for anxious youth? Journal of Clinical Child and Adolescent Psychology. 2005;34:569–581. doi: 10.1207/s15374424jccp3403_12. [DOI] [PubMed] [Google Scholar]
- Barrett PM, Dadds MR, Rapee RM. Family treatment of childhood anxiety: A controlled trial. Journal of Consulting and Clinical Psychology. 1996;64:333–342. doi: 10.1037/0022-006X.64.2.333. [DOI] [PubMed] [Google Scholar]
- Beidel DC, Alfano CA. Child anxiety disorders: A guide to research and treatment. 2nd. New York: Routledge; 2011. [Google Scholar]
- Beidel DC, Turner SM, Sallee FR, Ammerman RT, Crosby LA, Pathak S. SET-C versus fluoxetine in the treatment of childhood social phobia. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46:1622–1632. doi: 10.1097/chi.0b013e318154bb57. [DOI] [PubMed] [Google Scholar]
- Berman SL, Weems CF, Silverman WK, Kurtines WM. Predictors of outcome in exposure-based cognitive and behavioral treatments for phobic and anxiety disorders in children. Behavior Therapy. 2000;31:713–731. doi: 10.1016/S0005-7894(00)80040-4. [DOI] [Google Scholar]
- Boden JM, Fergusson DM, Horwood L. Anxiety disorders and suicidal behaviours in adolescence and young adulthood: Findings from a longitudinal study. Psychological Medicine: A Journal of Research in Psychiatry and the Allied Sciences. 2007;37:431–440. doi: 10.1017/S0033291706009147. [DOI] [PubMed] [Google Scholar]
- Bo¨gels SM, Siqueland L. Family cognitive behavioral therapy for children and adolescents with clinical anxiety disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45:134–141. doi: 10.1097/01.chi.0000190467.01072.ee. [DOI] [PubMed] [Google Scholar]
- Breinholst S, Esbjørn BH, Reinholdt-Dunne M, Stallard P. CBT for the treatment of child anxiety disorders: A review of why parental involvement has not enhanced outcomes. Journal of Anxiety Disorders. 2012;26:416–424. doi: 10.1016/j.janxdis.2011.12.014. [DOI] [PubMed] [Google Scholar]
- Bryk AS, Raudenbush SW, Congdon RT. Hierarchical linear and nonlinear modeling with the HLM/2L and HLM/3L programs. Chicago: Scientific Software International; 1996. [Google Scholar]
- Chu BC, Colognori D, Weissman AS, Bannon K. An initial description and pilot of group behavioral activation therapy for anxious and depressed youth. Cognitive and Behavioral Practice. 2009;16:408–419. doi: 10.1016/j.cbpra.2009.04.003. [DOI] [Google Scholar]
- Cobham VE, Dadds MR, Spence SH, McDermott B. Parental anxiety in the treatment of childhood anxiety: A different story three years later. Journal of Clinical Child and Adolescent Psychology. 2010;39:410–420. doi: 10.1080/15374411003691719. [DOI] [PubMed] [Google Scholar]
- Comer JS, Blanco C, Hasin DS, Liu SM, Grant BF, Turner JB, Olfson M. Health-related quality of life across the anxiety disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Journal of Clinical Psychiatry. 2011;72:43–50. doi: 10.4088/JCP.09m05094blu. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comer JS, Kendall PC. High-end specificity of the children's depression inventory in a sample of anxiety-disordered youth. Depression and Anxiety. 2005;22:11–19. doi: 10.1002/da.20059. [DOI] [PubMed] [Google Scholar]
- Comer JS, Puliafico AC, Aschenbrand SG, McKnight K, Robin JA, Goldfine ME, Albano A. A pilot feasibility evaluation of the CALM program for anxiety disorders in early childhood. Journal of Anxiety Disorders. 2012;26:40–49. doi: 10.1016/j.janxdis.2011.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creswell C, Cartwright-Hatton S. Family treatment of child anxiety: Outcomes, limitations and future directions. Clinical Child and Family Psychology Review. 2007;10:232–252. doi: 10.1007/s10567-007-0019-3. [DOI] [PubMed] [Google Scholar]
- Davis L, Barlow DH, Smith L. Comorbidity and the treatment of principal anxiety disorders in a naturalistic sample. Behavior Therapy. 2010;41:296–305. doi: 10.1016/j.beth.2009.09.002. [DOI] [PubMed] [Google Scholar]
- Drake KL, Ginsburg GS. Family factors in the development, treatment, and prevention of childhood anxiety disorders. Clinical Child and Family Psychology Review. 2012;15:144–162. doi: 10.1007/s10567-011-0109-0. [DOI] [PubMed] [Google Scholar]
- Eccles JS, Buchanan CM, Flanagan C, Fuligni A, Midgley C, Yee D. Control versus autonomy during early adolescence. Journal of Social Issues. 1991;47:53–68. doi: 10.1111/j.1540-4560.1991.tb01834.x. [DOI] [Google Scholar]
- Ehrenreich-May J, Bilek EL. The development of a transdiagnostic, cognitive behavioral group intervention for childhood anxiety disorders and co-occurring depression symptoms. Cognitive and Behavioral Practice. 2012;19:41–55. doi: 10.1016/j.cbpra.2011.02.003. [DOI] [Google Scholar]
- Gallo KP, Chan PT, Buzzella BA, Whitton SW, Pincus DB. The impact of an 8-day intensive treatment for adolescent panic disorder and agoraphobia on comorbid diagnoses. Behavior Therapy. 2012;43:153–159. doi: 10.1016/j.beth.2011.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallo KP, Cooper-Vince CE, Hardway CL, Pincus DB, Comer JS. Trajectories of change across outcomes in intensive treatment for adolescent panic disorder and agoraphobia. Journal of Clinical Child and Adolescent Psychology. 2014;43:742–750. doi: 10.1080/15374416.2013.794701. [DOI] [PubMed] [Google Scholar]
- Garber J, Weersing V. Comorbidity of anxiety and depression in youth: Implications for treatment and prevention. Clinical Psychology: Science and Practice. 2010;17:293–306. doi: 10.1111/j.1468-2850.2010.01221.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginsburg GS, Silverman WK, Kurtines WK. Family involvement in treating children with phobic and anxiety disorders: A look ahead. Clinical Psychology Review. 1995;15:457–473. doi: 10.1016/0272-7358(95)00026-. [DOI] [Google Scholar]
- Ginsburg GS, Siqueland L, Masia-Warner C, Hedtke KA. Anxiety disorders in children: Family matters. Cognitive and Behavioral Practice. 2004;11:28–43. doi: 10.1016/S1077-7229(04)80005-1. [DOI] [Google Scholar]
- Granic I, Dishion TJ, Hollenstein T. The family ecology of adolescence: A dynamic systems perspective on normative development. In: Adams GR, Berzonsky MD, editors. Blackwell handbook of adolescence. Malden: Blackwell Publishing; 2003. pp. 60–91. [Google Scholar]
- Hirschfeld RA. Panic disorder: Diagnosis, epidemiology, and clinical course. Journal of Clinical Psychiatry. 1996;57:3–8. [PubMed] [Google Scholar]
- Hudson JL, Kendall PC, Coles ME, Robin JA, Webb A. The other side of the coin: Using intervention research in child anxiety disorders to inform developmental psychopathology. Development and Psychopathology. 2002;14:819–841. doi: 10.1017/S095457940200408X. [DOI] [PubMed] [Google Scholar]
- Hughes AA, Hedtke KA, Kendall PC. Family functioning in families of children with anxiety disorders. Journal of Family Psychology. 2008;22:325–328. doi: 10.1037/0893-3200.22.2.325. [DOI] [PubMed] [Google Scholar]
- In-Albon T, Schneider S. Psychotherapy of childhood anxiety disorders: A meta-analysis. Psychotherapy and Psychosomatics. 2006;76:15–24. doi: 10.1159/000096361. [DOI] [PubMed] [Google Scholar]
- Kearney CA, Albano AM, Eisen AR, Allan WD, Barlow DH. The phenomenology of panic disorder in youngsters: An empirical study of a clinical sample. Journal of Anxiety Disorders. 1997;11:49–62. doi: 10.1016/s0887-6185(96)00034-5. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Hudson JL, Gosch E, Flannery-Schroeder E, Suveg C. Cognitive-behavioral therapy for anxiety disordered youth: A randomized clinical trial evaluating child and family modalities. Journal of Consulting and Clinical Psychology. 2008;76:282–297. doi: 10.1037/0022-006X.76.2.282. [DOI] [PubMed] [Google Scholar]
- Kovacs M. Children's depression inventory. New York: Multi-Health Systems; 1992. [Google Scholar]
- Kovacs M, Devlin B. Internalizing disorders in childhood. Journal of Child Psychology and Psychiatry. 1998;39(1):47–63. doi: 10.1017/S0021963097001765. [DOI] [PubMed] [Google Scholar]
- Manassis K, Lee T, Bennett K, Zhao X, Mendlowitz S, Duda S, Wood JJ. Types of parental involvement in CBT with anxious youth: A preliminary meta-analysis. Journal of Consulting and Clinical Psychology. 2014 doi: 10.1037/a0036969. [DOI] [PubMed] [Google Scholar]
- Matthey S, Petrovski P. The Children's depression inventory: Error in cutoff scores for screening purposes. Psychological Assessment. 2002;14:146–149. doi: 10.1037/1040-3590.14.2.146. [DOI] [PubMed] [Google Scholar]
- Merikangas K, He J, Burstein M, Swendsen J, Avenevoli S, Case B, Olfson M. Service utilization for lifetime mental disorders in U.S. adolescents: Results of the National Comorbidity Survey-Adolescent Supplement (NCSA) Journal of the American Academy of Child and Adolescent Psychiatry. 2011;50:32–45. doi: 10.1016/j.jaac.2010.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mineka S, Watson D, Clark L. Comorbidity of anxiety and unipolar mood disorders. Annual Review of Psychology. 1998;49:377–412. doi: 10.1146/annurev.psych.49.1.377. [DOI] [PubMed] [Google Scholar]
- O'Neil KA, Podell JL, Benjamin CL, Kendall PC. Comorbid depressive disorders in anxiety-disordered youth: Demographic, clinical, and family characteristics. Child Psychiatry and Human Development. 2010;41:330–341. doi: 10.1007/s10578-009-0170-9. [DOI] [PubMed] [Google Scholar]
- Ollendick TH, Öst L, Reuterskiöld L, Costa N. Comorbidity in youth with specific phobias: Impact of comorbidity on treatment outcome and the impact of treatment on comorbid disorders. Behaviour Research and Therapy. 2010;48:827–831. doi: 10.1016/j.brat.2010.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ollendick TH, Pincus D. Panic disorder in adolescents. In: Steele RG, Elkin T, Roberts MC, editors. Handbook of evidence-based therapies for children and adolescents: Bridging science and practice. New York: Springer Science + Business Media; 2008. pp. 83–102. [DOI] [Google Scholar]
- Pincus DB, Ehrenreich JT, Mattis SG. Mastery of anxiety and panic for adolescents: Riding the wave, therapist guide. New York: Oxford University Press; 2008. [Google Scholar]
- Pincus DB, May J, Whitton SW, Mattis SG, Barlow DH. Cognitive-behavioral treatment of panic disorder in adolescence. Journal of Clinical Child and Adolescent Psychology. 2010;39:638–649. doi: 10.1080/15374416.2010.501288. [DOI] [PubMed] [Google Scholar]
- Pincus DB, Whitton S, Gallo KP, Weiner CL, Chow C, Barlow DH, Hardway CL. Intensive treatment of adolescent panic disorder: Results of a randomized controlled trial in preparation. [Google Scholar]
- Rapee RM. Family factors in the development and management of anxiety disorders. Clinical Child and Family Psychology Review. 2012;15:69–80. doi: 10.1007/s10567-011-0106-3. [DOI] [PubMed] [Google Scholar]
- Rapee RM, Schniering CA, Hudson JL. Anxiety disorders during childhood and adolescence: Origins and treatment. Annual Review of Clinical Psychology. 2009;53:11–341. doi: 10.1146/annurev.clinpsy.032408.153628. [DOI] [PubMed] [Google Scholar]
- Santucci LC, Ehrenreich JT, Trosper SE, Bennett SM, Pincus DB. Development and preliminary evaluation of a one-week summer treatment program for separation anxiety disorder. Cognitive and Behavioral Practice. 2009;16:317–331. doi: 10.1016/j.cbpra.2008.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schafer JL, Graham JW. Missing data: Our view of the state of the art. Psychological Methods. 2002;7:147–177. doi: 10.1037/1082-989X.7.2.147. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Albano AM. The anxiety disorders interview schedule for children for DSM-IV child and parent versions. San Antonio: Psychological Corporation; 1997. [Google Scholar]
- Silverman WK, Kurtines WM, Jaccard J, Pina AA. Directionality of change in youth anxiety treatment involving parents: An initial examination. Journal of Consulting and Clinical Psychology. 2009;77:474–485. doi: 10.1037/a0015761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spence SH, Donovan C, Brechman-Toussaint M. The treatment of childhood social phobia: The effectiveness of a social skills training-based, cognitive-behavioural intervention, with and without parental involvement. Journal of Child Psychology and Psychiatry. 2000;41:713–726. doi: 10.1111/1469-7610.00659. [DOI] [PubMed] [Google Scholar]
- Steinberg L, Silk JS. Parenting adolescents. In: Bornstein MH, editor. Handbook of parenting. Vol. 1. Children and parenting Mahwah: Lawrence Erlbaum; 2002. pp. 103–133. [Google Scholar]
- Suveg C, Hudson JL, Brewer G, Flannery-Schroeder E, Gosch E, Kendall PC. Cognitive-behavioral therapy for anxiety-disordered youth: Secondary outcomes from a randomized clinical trial evaluating child and family modalities. Journal of Anxiety Disorders. 2009;23:341–349. doi: 10.1016/j.janxdis.2009.01.003. [DOI] [PubMed] [Google Scholar]
- Trosper SE, Whitton SW, Brown TA, Pincus DB. Understanding the latent structure of the emotional disorders in children and adolescents. Journal of Abnormal Child Psychology. 2012;40:621–632. doi: 10.1007/s10802-011-9582-7. [DOI] [PubMed] [Google Scholar]
- Walkup JT, Albano A, Piacentini J, Birmaher B, Compton SN, Sherrill JT, Kendall PC. Cognitive behavioral therapy, sertraline, or a combination in childhood anxiety. The New England Journal of Medicine. 2008;359:2753–2766. doi: 10.1056/NEJMoa0804633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waters TL, Barrett PM, March JS. Cognitive-behavioral family treatment of childhood obsessive-compulsive disorder: Preliminary findings. American Journal of Psychotherapy. 2001;55:372–387. doi: 10.1176/appi.psychotherapy.2001.55.3.372. [DOI] [PubMed] [Google Scholar]