Abstract
Acute aortic occlusion is a catastrophic event requiring early recognition and intervention. The patient was diagnosed type B aortic dissection. He became anuric on the sixth day of illness and the femoral artery pulse was not palpable. Therefore the patient was conveyed to our hospital. During transfer, his blood pressure was suddenly elevated and later he was in cardiopulmonary arrest. After cardiopulmonary resuscitation, the heart resumed beating in several minutes. Acute dynamic obstruction was regarded as a cause of the cardiac arrest. A thoracic endovascular aortic repair was performed urgently. His postoperative period was uneventful and the patient was discharged without problems.
Keywords: aortic occlusion, aortic dissection, TEVAR
Introduction
Basic treatment of the type B acute aortic dissection is conservative treatment using antihypertensive medications. However, invasive treatment is required when it is associated with rupture and organ ischemia. Acute aortic occlusion is a catastrophic event and the prognosis remains poor. It requires early recognition and intervention. Traditional causes of occlusion as saddle embolus and thrombosis are considered as the most frequent causes.
Thoracic endovascular aortic repair (TEVAR) is becoming increasingly popular due to reduced perioperative morbidity and mortality compared with open surgical repair.1) We are presenting a case of type B aortic dissection with dynamic obstruction caused cardiopulmonary arrest, in which a successful TEVAR was performed urgently.
Case Report
A 75 year-old male patient was admitted to the emergency department of another hospital for sudden intense back pain. Thoracic and abdominal computed tomography angiography (CTA) detected a tear at aortic isthmus just below the left subclavian artery (LSA) (Figs. 1A–1C). The patient was diagnosed with acute type B aortic dissection and treated using strict measures to control the blood pressure. The patient became anuric on the sixth day of illness and the femoral artery pulse was not palpable. CTA detected narrowing of the true lumen of the thoracic aorta due to dilatation of false lumen (Figs. 1D–1F). Therefore the patient was conveyed to our hospital. During transfer, his systolic blood pressure was suddenly elevated over 200 mmHg and later he was in cardiopulmonary arrest. After cardiopulmonary resuscitation, the heart resumed beating in several minutes. Then his femoral artery pulse was palpable. Acute thrombotic obstruction mediated by narrowing of the true lumen was regarded as a cause of the cardiac arrest. As the femoral artery was not palpated when the systolic blood pressure of the patients was 100 mmHg, we maintained systolic blood pressure in 60∼80 mmHg. Under general anesthesia, a TEVAR was performed emergently and was able to close primary entry (Fig. 2).
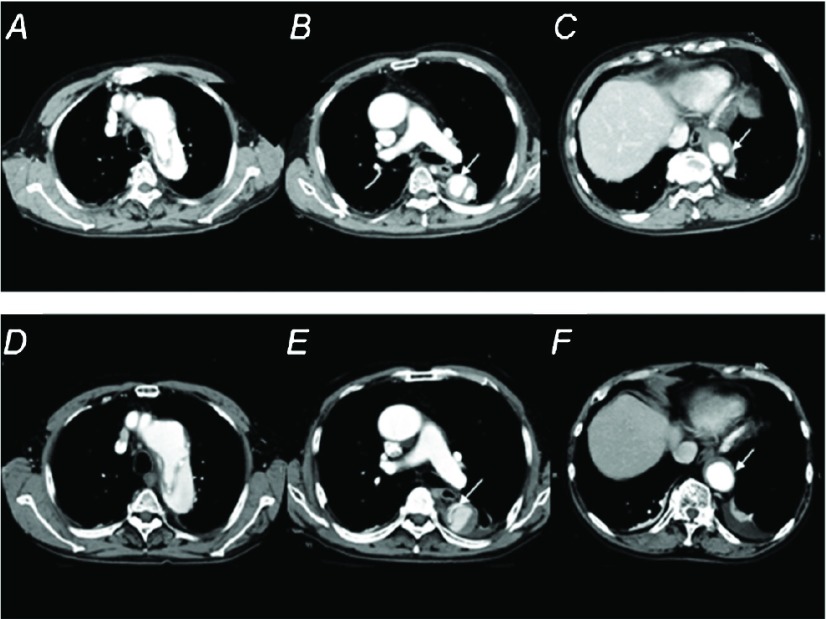
Fig. 1.
Preoperative CTA images on the first day (A, B, C) and six day (D, E, F) of the illness at the level of the thoracic cavity. White arrows indicate the true lumen. (A, D) aortic arch, (B, E) bifurcation of trachea, (C, F) diaphragm. CTA on the six day of illness was detected narrowed true lumen accompanied by expanded the false lumen compared with the first day. CTA: computed tomography angiography
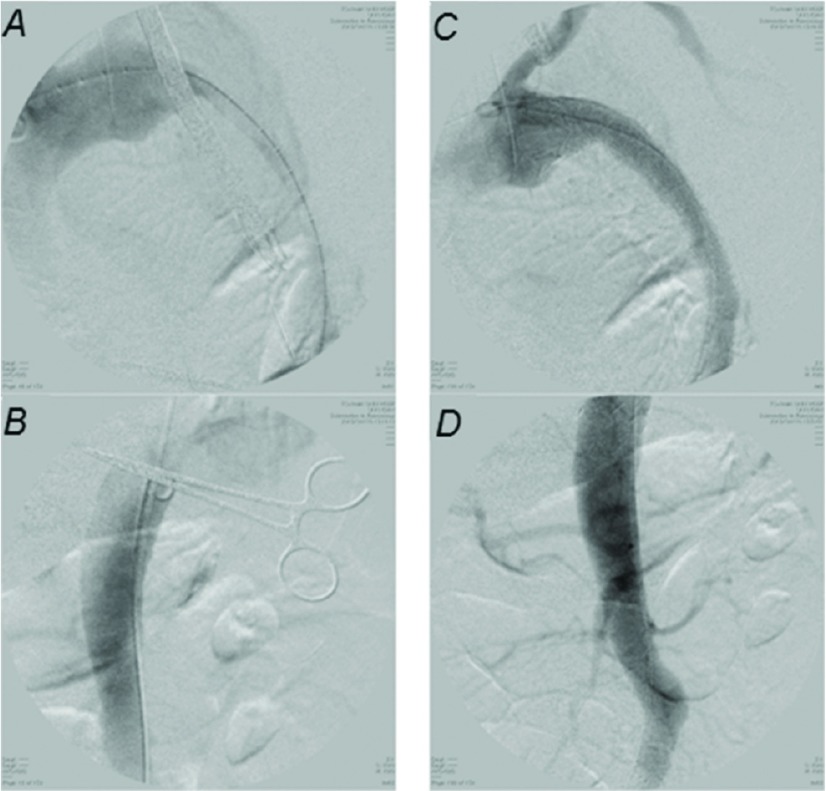
Fig. 2.
Intraoperative digital subtraction angiography (DSA) images. (A) pre-deployment image of the thoracic aorta. There was little blood flow in the true lumen. (B) pre-deployment image of the abdominal aorta at the Th 11 level. (C) post-deployment image of the thoracic aorta. (D) post-deployment image of the abdominal aorta.
After the operation, there were no ischemic symptoms of the cerebral, abdominal organs, bilateral legs, or arms. His postoperative period was uneventful and the patient was discharged from the hospital on the 14th day. Six month after TEVAR, postoperative CT showed no migration of the stent-graft (Fig. 3).
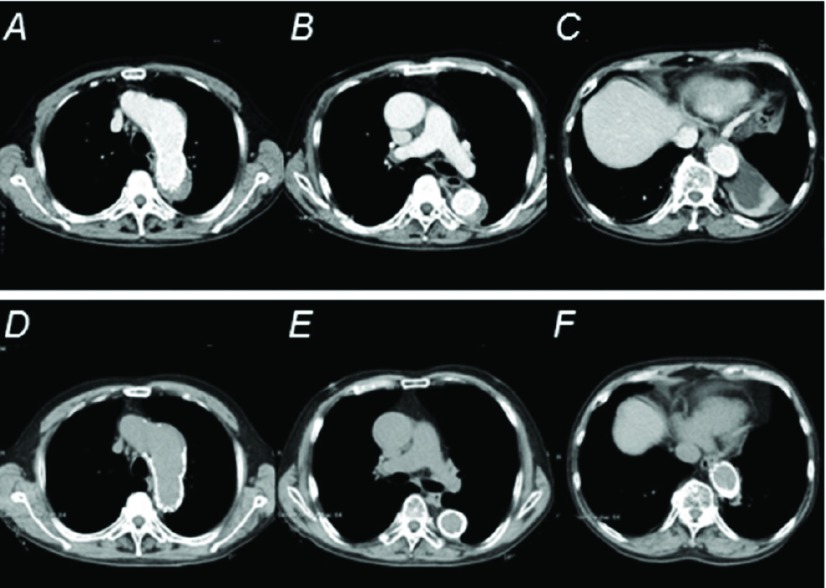
Fig. 3.
Postoperative CTA and CT images at the discharge (A, B, C) and six month (D, E, F) after discharge at the level of the thoracic cavity. (A, D) aortic arch, (B, E) bifurcation of trachea, (C, F) diaphragm. CTA on the six month after discharge was detected the remodeling of Thoracoabdominal aorta. CTA: computed tomography angiography
Discussion
Cases of complicated type B dissection associated with explosion and lower limbs ischemia, organ ischemia, refractory pain in an acute phase is extremely serious clinical condition. In 15% to 20% of these cases, it was often candidates for the surgical treatment or interventional therapy, with a mortality rate up to 20% on day 2 and 25% to 50% at 1 month.2)
However, the involvement of the conventional thoracotomy, abdominal operation was so invasive procedure, and conservative treatment mainly composed of the management of the blood pressure with the antihypertensive agent has been chosen in case without these symptoms. Nevertheless, it is said that the mortality in 1 year from conservative treatment generally reaches approximately 10%.3) And the reported long-term survival rate with medical therapy is approximately 60% to 80% at 4 to 5 years and approximately 40% to 45% at 10 years.4–6) Therefore, in the uncomplicated type B aortic dissection, there is an opinion saying that TEVAR should be performed for the case that is more likely to cause the aorta-related adverse event of the remote phase including the dissecting aortic aneurysm positively.7)
The literature about TEVAR as the surgical treatment means for aortic dissection is already present much. Therefore TEVAR is becoming increasingly popular due to reduced perioperative morbidity and mortality compared with open surgical repair.1)
Dynamic obstruction is caused by occlusion of the suppressed true lumen of the aorta by the pressurized false lumen, and static obstruction is caused by dissection into branch vessel ostia with distal vessel occlusion. Dynamic obstruction occurs while a large quantity of blood flow greatly flows into the false lumen from an opened primary entry when there is little blood flow to flow out from re-entry, or there is few it. Conventional surgical treatments of this obstruction such as laparotomy or transcatheter fenestration, true lumen stenting are some effect of treatment, and has been performed spread widely.8) However, there are some problems that the ischemia may not be improved only by fenestration in transcatheter fenestration and that the expansion power of the self-dilated stent may not be opposed to pressure to depend on false lumen. Thus, it is an extremely useful therapy that TEVAR closes the entry by little involvement, and can expand a true lumen and the branch artery which became constricted. Nienaber et al. performed a randomized controlled trial to compare conservative treatment and the stent graft treatment for the type B aortic dissection case of for a sub-acute phase without complications or the chronic stage in The Investigation of Stent Grafts in Aortic Dissection trial (INSTEAD trial). They reported that the 2-year survival rate of both, an aorta-related adverse event incidence did not have a significant difference. Furthermore, they reported recently for the remote phase in this trial when there were significantly few aorta-related adverse events in TEVAR group.9) Significance of the TEVAR group may be found by the progress of the device more in future.
In this case, it was the acute type B aortic dissection in which complications were not associated with, and conservative treatment with the antihypertensive therapy was chosen. However, on the sixth day of illness, it was judged that emergency surgery was necessary because of anuria and femoral artery pulseless. Therefore the patient was conveyed to our hospital. During transfer, his systolic blood pressure was suddenly elevated and later he was in cardiopulmonary arrest. After cardiopulmonary resuscitation, the heart resumed beating in several minutes. There were no rupture of aorta, the evidence of cardiac tamponade by computed tomography after the heartbeat resumption. Acute thrombotic obstruction mediated by narrowing of the true lumen was regarded as a cause of the cardiac arrest. The Japanese Circulation Society (JCS) guidelines classify TEVAR as a Class I recommendation for cases of complicated acute type B dissection. For the acute type B aortic dissection with fatal complications, it is becoming the first choice.10) In this case, because it is high-risk to be performed open surgical repair after a revival, and because there was no static obstruction, we chose TEVAR as first choice. His postoperative period was uneventful and the patient was discharged without problems. We regard TEVAR as a very useful therapy in the acute type B aortic dissection.
Conclusion
We performed TEVAR successfully for a case of type B aortic dissection with dynamic obstruction followed by cardiopulmonary arrest. Endovascular treatment is considered an effective method for patients who cannot tolerate the surgery using artificial heart-lung machine.
Disclosure Statement
All authors have no conflict of interest.
References
- Murad MH, Rizvi AZ, Malgor R, et al. Comparative effectiveness of the treatments for thoracic aortic transection [corrected]. J Vasc Surg 2011; 53: 193-9. e1-21. [DOI] [PubMed] [Google Scholar]
- Hagan PG, Nienaber CA, Isselbacher EM, et al. The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease. JAMA 2000; 283: 897-903. [DOI] [PubMed] [Google Scholar]
- Suzuki T, Mehta RH, Ince H, et al. Clinical profiles and outcomes of acute type B aortic dissection in the current era: lessons from the International Registry of Aortic Dissection (IRAD). Circulation 2003; 108 Suppl 1: II312-7. [DOI] [PubMed] [Google Scholar]
- Umaña JP, Lai DT, Mitchell RS, et al. Is medical therapy still the optimal treatment strategy for patients with acute type B aortic dissections. J Thorac Cardiovasc Surg 2002; 124: 896-910. [DOI] [PubMed] [Google Scholar]
- Bernard Y, Zimmermann H, Chocron S, et al. False lumen patency as a predictor of late outcome in aortic dissection. Am J Cardiol 2001; 87: 1378-82. [DOI] [PubMed] [Google Scholar]
- Estrera AL, Miller CC, Safi HJ, et al. Outcomes of medical management of acute type B aortic dissection. Circulation 2006; 114: I384-9. [DOI] [PubMed] [Google Scholar]
- Nienaber CA, Rousseau H, Eggebrecht H, et al. Randomized comparison of strategies for type B aortic dissection: the INvestigation of STEnt Grafts in Aortic Dissection (INSTEAD) trial. Circulation 2009; 120: 2519-28. [DOI] [PubMed] [Google Scholar]
- Patel HJ, Williams DM, Meerkov M, et al. Long-term results of percutaneous management of malperfusion in acute type B aortic dissection: implications for thoracic aortic endovascular repair. J Thorac Cardiovasc Surg 2009; 138: 300-8. [DOI] [PubMed] [Google Scholar]
- Nienaber CA, Kische S, Rousseau H, et al. Endovascular repair of type B aortic dissection: long-term results of the randomized investigation of stent grafts in aortic dissection trial. Circ Cardiovasc Interv 2013; 6: 407-16. [DOI] [PubMed] [Google Scholar]
- Usui A. TEVAR for type B aortic dissection in Japan. Gen Thorac Cardiovasc Surg 2014; 62: 282-9. [DOI] [PubMed] [Google Scholar]