Abstract
Gastroduodenal artery (GDA) aneurysm is a rare but potentially fatal vascular disease, with chronic pancreatitis being reported as the commonest aetiological factor. Its main complication is rupture, which is not uncommon and carries high risk of mortality. Clinical suspicion and advanced imaging tools should be employed in a timely fashion to make a diagnosis before this ominous event. We report a case of successfully treated GDA aneurysm who presented with minor bleeding episodes before suffering a major bleed and briefly discuss this pathology in light of the existing literature.
Keywords: gastroduodenal artery aneurysm, visceral artery aneurysm, coil embolization
Introduction
The term visceral artery aneurysm (VAA) has been used to refer to any intra-abdominal aneurysm excluding those of the aortoiliac axis. Generally, VAAs are rare clinical entities, with a reported incidence of 0.01%–0.2% though an incidence of 10% has been reported among chronic pancreatitis patients.1) However, they could be potentially lethal owing to the 25% risk of rupture; which consequently has a mortality rate of 70%.2,3) Gastro duodenal artery (GDA) aneurysm is among the rarest VAAs; accounting only for 1.5% of the total, second in its rarity only to inferior mesenteric artery aneurysm.4) Despite its rarity, it represents an important subcategory of VAAs on account of having up to 75% risk of rupture;5) with gastrointestinal bleeding being the presenting feature in up to 52% of cases.6) In this article we add a GDA aneurysm case to the existing literature and briefly discuss its aetiology, pathology, presentation and management.
Case Scenario
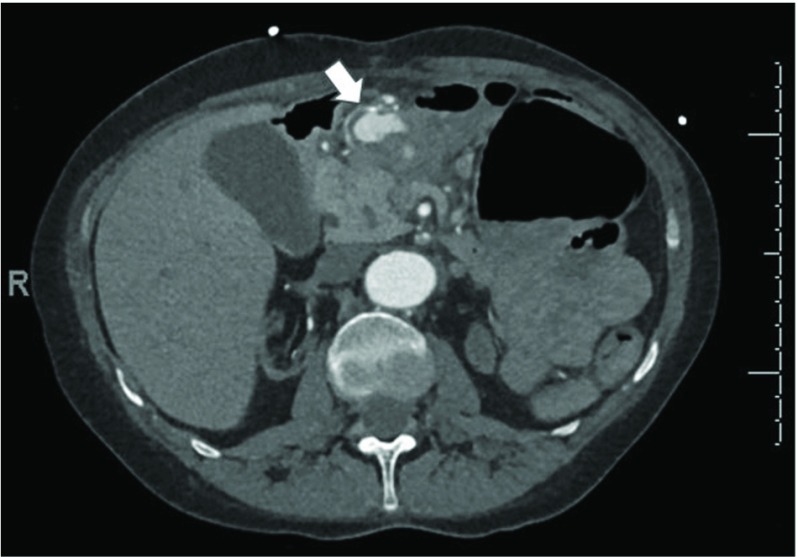
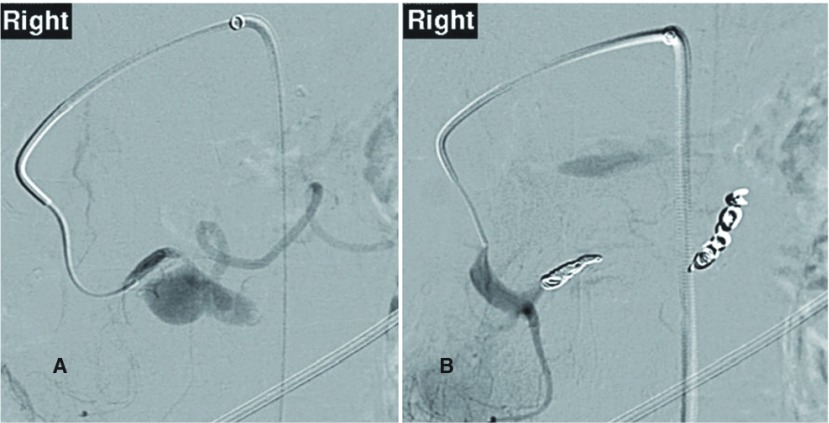
A 45 year old female presented to a smaller referral centre with one week history of intermittent severe upper abdominal pain, melena and a feeling of light headedness. Abdominal examination was unremarkable. Vital signs and blood picture showed mild haemorrhagic hypovolemia with blood pressure (BP) at 100/82, pulse at 115 beats/min (B/M) and haemoglobin (Hb) at 64 with normal mean corpuscular volume (MCV). Her past history entailed severe blunt abdominal trauma for which she sustained pancreatic head and body laceration with main pancreatic duct injury and significant intra-abdominal haemorrhage. Significant medical conditions were end stage renal disease (ESRD) for 22 years, secondary to trauma related ischemic cortical necrosis. She was first on haemodialysis for two years, then she had a cadaveric renal transplant surgery which subsequently gradually developed chronic rejection that eventually caused her to be put back on haemodialysis 18 years after the transplant surgery, till the presenting time. She also had other co-morbidities in the form of hypertension, and dyslipidaemia. Past surgeries included traumatic pancreatico-jejunostomy/distal pancreatectomy and splenectomy and failed renal transplant. On admission, she was transfused 2 red blood cells (RBCs) units and then proceeded to osophagogastroduodenoscopy (OGD) which showed only mild gastritis and duodenitis without ulcers or bleeding stigmata. Shortly after that, she developed severe epigastric pain and reported an episode of bleeding per rectum causing her to develop moderate degree haemorrhagic shock with BP dropping to 69/40 and Hb to 59. She received 300 ml saline and 2 RBC units and then transferred to our hospital. On admission, her pain was settled, her vital signs had improved and her Hb was 77. Her coagulation profile was normal with international normalized ratio (INR) at 1.1 and platelet count at 193. She then vomited about 50 ml of fresh blood, passed a bloody motion and developed clinically mild hypovolemia with her Hb at 66; for which she received one unit of RBC. Few hours later, she developed severe epigastric pain, attack of haematemesis and another bloody motion causing her consciousness to deteriorate, pulse raised to 135 B/M, systolic BP dropped to 64 and Hb to 58; for which she received a 200 ml saline bolus plus 1 unit RBC. Given the presence of haematemesis and severity of gastro-intestinal (GI) bleeding, an upper, rather than lower, GI source was suggested thus precluding colonoscopy as a diagnostic procedure. After she had been stabilized, a triphasic computerized tomography (CT) scan of the abdomen and pelvis was done and showed a 4 cm × 3 cm × 4 cm partly calcified aneurysm of the GDA with loss of continuity and fat stranding on its medial aspect; however a definite communication with the gastrointestinal tract could not be delineated (Fig. 1). In addition, CT showed absence of the tail and distal pancreatic body with coarse pancreatic calcifications. Transfemoral catheter embolization of the GDA aneurysm was performed emergently through multiple coils placed in the GDA going back to its origin (Fig. 2). The patient was then admitted to the high dependency unit for close monitoring, where her condition showed gradual continuous improvement. After 2 days, she was discharged back to the referring hospital.
Fig. 1.
Contrast enhanced CT abdomen showing partially calcified aneurysm of the GDA (arrow). CT: computerized tomography; GDA: gastroduodenal artery
Fig. 2.
Celiac angiography showing: (A) GDA aneurysm (pre embolization), (B) Non enhancement of the GDA (post coil embolization). GDA: gastroduodenal artery
Discussion
Since first reported by Starlinger7) in 1930, there have been several dozens of GDA aneurysm reports at prolonged but decreasing intervals; obviously due to improved imaging techniques and increased tendency to report such cases. In 2013, Habib et al. have identified 74 GDA aneurysm cases in English and Japanese literature between the years 1956–2011.6) We have identified additional 18 cases including ours in the English literature in the years 2012–2015. Depending on the morphology and aetiology, GDA aneurysms may be classified into false or true aneurysms, with the former being more common. Pancreatitis and atherosclerosis are the commonest aetiological factors associated with GDA aneurysm formation. Leakage of proteolytic enzymes in the setting of pancreatitis can result in destruction of the vessel wall with subsequent false aneurysm formation. Weakening of the arterial wall secondary to atherosclerosis is the usual pathogenetic event for true aneurysms. However, some authors proposed that atherosclerotic celiac trunk stenosis may cause retrograde flow of blood through superior mesenteric then pancreaticoduodenal arteries with consequent building of pressure in the GDA and aneurysm formation.8) Other rarer causes include congenital absence of celiac axis, peptic ulcer, iatrogenic injury during pancreatic head biopsy and tuberculous infection. In our case, it is likely that aneurysm formation was related to pancreatic insult possibly related to her old pancreatic surgery. Also contributing to pathogenesis may have been her atherosclerotic process which is predisposed to by elevated blood pressure and deranged lipid profile. Pathogenesis of her GI bleeding is most probably related to intermittent erosion and breakdown of the aneurysm wall through the duodenal wall, secondary to pressure necrosis caused by the expanding calcified aneurysm. Although ESRD is known to be a procoagulant state, patients are known to be at a higher bleeding risk secondary to the coexisting uremic platelet dysfunction. Clinically, unruptured GDAs may be asymptomatic or may cause upper abdominal pain, obstructive jaundice or anemia from chronic gastrointestinal blood loss. Ruptured GDAs may bleed into the gastro-intestinal tract (GIT) causing haematemesis, melena, haemobilia or pseudo haemobilia or into the peritoneum causing haemorrhagic shock or severe abdominal pain. Very rarely, GDA may rupture into superior mesenteric vein and present with bleeding esophageal varices.9) Currently, with the availability and feasibility of highly sensitive imaging modalities, more GDA aneurysms are being detected incidentally in asymptomatic individuals undergoing abdominal imaging for another reason. A diagnostic challenge, however, may arise in the acute situation since OGD which is the gold standard investigation for evaluating a patient with GIT haemorrhage may not pick a GDA aneurysm as the bleeding source; as was the case in our report. Hence; a high index of suspicion should always be kept. Ultrasound, either endoscopic or transabdominal, appears to be a useful and cost effective diagnostic tool with its sensitivity depending however on operator expertise. An abdominal CT or visceral angiography would be the appropriate next steps with the latter often being the investigation of choice due to its higher sensitivity (100% vs. 76%) and the potential to be therapeutic.10) Once diagnosed, a GDA must be definitively treated even if small or asymptomatic; on account of its potential to rupture; a drastic event which seems to be unrelated to size. The optimal management approach depends on the mode of presentation and hemodynamic status of the patient. In asymptomatic patient or in the “bleeding but stable” patient, an endovascular approach through coil embolization or stent grafting offers the best chance for the patient due to its overall low morbidity and mortality.11) Thrombin injection—under EUS guidance—has also been described for management of pancreatic pseudo aneurysms.12) Failed intervention or unstable patient requires emergency laparotomy, exclusion of the aneurysm by vessel ligation or aneurysm resection with or without vascular reconstruction through end to end anastmosis.
Conclusions
Given their rarity, GDA aneurysms may be difficult to be clinically thought of as a cause of upper GIT bleeding. Lack of definite convincing pathology on OGD should significantly raise suspicion. Recurrent minor attacks of upper GIT bleeding may precede a major one. Exhaustive efforts should be made at the former stage before a life threatening situation arises. Transcatheter angiographic coil embolization is a feasible, safe and effective treatment for those patients as long as the patient is haemodynamically stable.
Disclosure statement
All authors have no conflict of interest.
References
- Røkke O, Søndenaa K, Amundsen S, et al. The diagnosis and management of splanchnic artery aneurysms. Scand J Gastroenterol 1996; 31: 737-43. [DOI] [PubMed] [Google Scholar]
- Panayiotopoulos YP, Assadourian R, Taylor PR. Aneurysms of the visceral and renal arteries. Ann R Coll Surg Engl 1996; 78: 412-9. [PMC free article] [PubMed] [Google Scholar]
- Gehlen JM, Heeren PA, Verhagen PF, et al. Visceral artery aneurysms. Vasc Endovascular Surg 2011; 45: 681-7. [DOI] [PubMed] [Google Scholar]
- Edogawa S, Shibuya T, Kurose K, et al. Inferior mesenteric artery aneurysm: case report and literature review. Ann Vasc Dis 2013; 6: 98-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris K, Chalhoub M, Koirala A. Gastroduodenal artery aneurysm rupture in hospitalized patients: An overlooked diagnosis. World J Gastrointest Surg 2010; 2: 291-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Habib N, Hassan S, Abdou R, et al. Gastroduodenal artery aneurysm, diagnosis, clinical presentation and management: a concise review. Ann Surg Innov Res 2013; 7: 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starlinger F. Aneurysma spurium traumaticum der Art. gastroduodenalis. Zentralbi Chir 1930; 57: 1034-6. [Google Scholar]
- Kueper MA, Ludescher B, Koenigsrainer I, et al. Successful coil embolization of a ruptured gastroduodenal artery aneurysm. Vasc Endovascular Surg 2007; 41: 568-71. [DOI] [PubMed] [Google Scholar]
- Suzuki T, Ishida H, Komatsuda T, et al. Pseudoaneurysm of the gastroduodenal artery ruptured into the superior mesenteric vein in a patient with chronic pancreatitis. J Clin Ultrasound 2003; 31: 278-82. [DOI] [PubMed] [Google Scholar]
- Ghasura A, Patel K, Prajapati B, et al. Gastroduodenal artery pseudoaneurysm due to pancreatitis. J of Evolution of Med and Dent Sci 2014; 3: 4036-41. [Google Scholar]
- Cordova AC, Sumpio BE. Visceral artery aneurysms and pseudoaneurysms—should they all be managed by endovascular techniques?. Ann Vasc Dis 2013; 6: 687-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roach H, Roberts SA, Salter R, et al. Endoscopic ultrasound-guided thrombin injection for the treatment of pancreatic pseudoaneurysm. Endoscopy 2005; 37: 876-8. [DOI] [PubMed] [Google Scholar]