Abstract
Objective
This systematic review and meta-analysis examines the effect of screening and brief intervention (SBI) on outpatient, emergency department (ED), and inpatient health care utilization outcomes. Much of the current literature speculates that SBI provides cost savings through reduced health care utilization, but no systematic review or meta-analysis examines this assertion.
Method
Publications were abstracted from online journal collections and targeted Web searches. The systematic review included any publications that examined the association between SBI and health care utilization. Each publication was rated independently by two study authors and assigned a consensus methodological score. The meta-analysis focused on those studies examined in the systematic review, but it excluded publications that had incomplete data, low methodological quality, or a cluster randomized design.
Results
Systematic review results suggest that SBI has little to no effect on inpatient or outpatient health care utilization, but it may have a small, negative effect on ED utilization. A random effects meta-analysis using the Hedges method confirms the ED result for SBI delivered across settings (SMD = −.06, I-squared = 13.9%) but does not achieve statistical significance (CI: −0.15, 0.03).
Conclusions
SBI may reduce overall health care costs, but more studies are needed. Current evidence is inconclusive for SBI delivered in ED and non-ED hospital settings. Future studies of SBI and health care utilization should report the estimated effects and variance, regardless of the effect size or statistical significance.
Keywords: Screening and brief intervention, health care utilization, systematic review, meta-analysis
Introduction
A number of systematic reviews and meta-analyses assess the effectiveness of screening and brief intervention (SBI) to reduce alcohol consumption among at-risk drinkers.1-12 Despite concerns about some studies' methodology,5,9 SBI is widely thought to reduce alcohol consumption. Beyond clinical outcomes, SBI is also considered to be cost-effective or cost-beneficial by many authors.11,13-16 Furthermore, many U.S. policy makers—such as the Substance Abuse and Mental Health Services Administration17—advocate for the widespread adoption of SBI, often stating that SBI will reduce health care utilization and therefore save money.
Several recent studies and reviews of the economic evaluation of SBI have been published,13-16 but to date there has been no systematic review and meta-analysis that assesses whether SBI reduces health care utilization. A recent review16 suggests SBI can be cost-effective in improving quality-adjusted life years (QALYs) when implemented in primary care settings. However, evidence of a cost-effective intervention does not necessarily imply reduced health care utilization or health care cost savings. This article presents a systematic review and meta-analysis of the effect of SBI on health care utilization to evaluate the gap between the literature and broad policy support for SBI.
Methods
Systematic Review
A systematic literature search and review was conducted using electronic databases, formal selection criteria, and multiple reviewers. A literature search was conducted using several databases: CINAHL, MEDLINE, PubMed, Cochrane, EBSCO, JSTOR, and PsycARTICLES. Search terms comprised combinations of brief intervention terminology (screening and brief intervention, alcohol brief intervention, brief intervention, SBI, BI, and alcohol) and health care outcomes (health, health care utilization, utilization, physician visit, emergency department visit, general practitioner visit, hospital stays, hospitalization, hospital readmission, cost, and cost-effectiveness). All identified publications' reference lists, including those from other systematic reviews or meta-analyses on SBI, were also used.
Searches were not limited by year of publication (dates ranged from 1962 to 2010), but publications unavailable in English were excluded. The primary inclusion criterion was a health care utilization outcome in an alcohol-focused publication. Publications were then reviewed using the following 3 criteria: (1) conducted a form of brief intervention, (2) involved a solely non-alcohol-dependent population, and (3) was an independent publication (e.g., not a review or meta-analysis). Publications targeting alcohol-dependent populations were excluded.
The relationship between SBI and health care utilization may depend on both the setting in which SBI is delivered (e.g., primary care vs. ED) and the type of health care utilization (e.g., inpatient stay vs. outpatient visit). Publications were thus categorized into medical settings based on where SBI was delivered: primary care, ED, and non-ED hospital. As noted by Kraemer15 and Kaner et al.,7 the quality and outcome of SBI delivered in each of these 3 settings differ greatly.
Health care utilization is classified into outpatient care, ED care, and inpatient care. The types of care assigned for study outcomes were based on the descriptions in each publication. Outpatient care includes visits to a primary care provider/general practitioner, nurse practitioner, or outpatient counselor. In many cases, the outpatient care category is a catch-all for services not otherwise classified, such as ambulatory hospital or laboratory.18 ED care includes any hospital ED or urgent or trauma care facility visit. Inpatient care includes any non-ED hospital stay or admission or inpatient treatment facility stay. Setting is not tied specifically to the type of outcome. For example, a study conducted in a primary care setting may examine inpatient care.
The literature search and review was conducted by a study author. Two other authors conducted targeted, random sample screenings to ensure quality and accuracy. Several publications in this review use the same study for source data: Project TrEAT,19-24 Project GOAL,25,26 the Radcliffe Study (Radcliffe Hospital, Oxford, United Kingdom),27,28 and the St. Mary's Hospital study (St. Mary's Hospital, London, United Kingdom).29,30 So that the results of this analysis are not disproportionately influenced by any 1 study, the analyses include only those publications from any 1 study with the most comprehensive set of outcomes, the longest follow-up period, and/or exclusive target populations. For Project TrEAT, 3 of 6 publications were included: Fleming et al.,21 Grossberg et al.,23 and Manwell et al.22 Fleming et al.21 is the most comprehensive set of main findings. Grossberg et al.23 and Manwell et al.22 represent specific sub-analyses on young adults and women, respectively. Barrett et al.30 was selected for the St. Mary's study over Crawford et al.29 for a more comprehensive analysis. Mundt et al.26 was selected to represent Project GOAL because that publication had the longest follow-up period of the available project publications. For the Radcliffe Study, Anderson and Scott28 and Scott and Anderson27 were selected because those publications used mutually exclusive male and female cohorts.
A qualitative methodological score was assigned to each publication in the meta-analysis. The method followed was that of Miller et al.,31 as described in Vasilaki et al.,10 Miller and Willbourne,32 and Bien et al.,3 using a 12-item assessment of methodological quality and design. Summary scores range from 0 to 17, with 14 out of 17 indicating an excellent methodological quality.32 Each article was scored independently by 2 of the contributing authors. Any disagreement on scoring was resolved by the authors to obtain a consensus score.
Meta-Analysis
Data for the meta-analysis were abstracted from each publication by 1 author and reviewed by another author for accuracy. For publications that did not contain the necessary statistical components for the health care outcomes (sample size, effect size, variance measure), the corresponding author was contacted. Authors of publications published before 1995 were not contacted because of the anticipated infeasibility of retrieving the data or estimates. If the corresponding author could not provide the requested information, the publication was excluded from the meta-analysis. If the corresponding author provided data files instead of summary statistics, Stata 11 was used to calculate continuous effect sizes and standard deviations.
A random-effects specification with the Hedges method was used for the meta-analysis using the “metan” command in Stata 11. A random-effects model was selected because publications vary substantially in setting, form, and quality of the intervention and in the definition of the health care utilization outcomes. Publications were excluded from the final meta-analysis if data were not available, the publication was of poor methodological quality, or the publication used a cluster randomized design. The publications with cluster randomized designs did not provide enough information to include clustering effects in the meta-analysis appropriately.
The standardized mean difference (SMD) and associated 95% confidence interval were assessed for each publication and pooled for all publications. An SMD of 0.20 or less is considered small.33 The I-squared statistic is included to interpret the heterogeneity around the pooled SMD. Heterogeneity is categorized into 3 levels: low (I2 = ∼20%), moderate (I2 = ∼50%), and high (I2 = ∼70%). Higher levels of heterogeneity indicate greater variability across publications, in which case the pooled SMD may not be representative of the publications in the analysis. Given the aforementioned variation in setting, form, and quality of the intervention, moderate to high heterogeneity should be expected. This analysis examined 1 publication per study (the “main findings” publication). An alternative analysis included additional publications on Project TrEAT and the St. Mary's study.
Forest plots for the meta-analysis are presented separately by type of care. Although it is preferred to also present forest plots separately by setting, there were insufficient publications to review each setting separately.
Results
Systematic Review
For the systematic review, 216 publications were identified and abstracted for further review. Of these, 56 contained a health care utilization outcome and met the basic inclusion criteria; 29 publications met the full list of inclusion criteria and were selected for review. Table 1 describes the key characteristics of the publications by type of care and setting. Within setting, publications are presented by country, author, and year. Twenty-one publications were conducted in a primary care setting,18-28,34-43 Four were conducted in an ED setting,29,30,44,45 and 4 were conducted in a hospital setting other than an ED.46-49 Seventeen of the 29 publications were set in the United States, 6 in the United Kingdom, 2 in Australia and Sweden, and 1 in Canada and Switzerland. Table 1 also presents the qualitative methodological scoring of each publication. Scores ranged from 5 to 16; the mean score was 13.17, and the median was 13.
Table 1. Characteristics of Reviewed Studies.
| Author (Year) |
Country | Popu- lation |
Follow-Up Period |
Sample Size (Total/Int/Con) |
Study Design |
QMS | Outpatient Measure |
Direction | Significant Effect? |
ED Measure |
Direction | Significant Effect? |
Inpatient Measure |
Direction | Significant Effect? |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Primary Care Setting | |||||||||||||||
| Wutzke et al,.200234 | Australia | General | 10 year | 554/410/144 | RCT | 13 | Outpatient visits | Increase | No sig. effect | NA | NA | Use of health care facilities | Increase | No sig. effect | |
| Israel et al., 199635 | Canada | General | 12 | 73/38/35 | RCT | 15 | GP visits | Decrease | Sig. effect | NA | NA | NA | NA | - | |
| Kristenson et al., 198336 | Sweden | General | 24, 60 | 414/219/195 | Mixed QE/ RCT | 10 | NA | NA | NA | NA | Hospital days | Decrease | Not tested | ||
| Tomson et al. 199837 | Sweden | General | 36 | 75/30/45 | RCT | 13 | Consultations (mean) | No change | No sig. effect | NA | NA | Admission rate (%) | Increase | No | |
| Heather et al., 198738 | UK | General | 6 | 91/59/32 | RCT | 14 | GP consultations | Increase | No sig. effect | NA | NA | NA | NA | ||
| Lock et al., 200639 | UK | General | 12 | 127/67/60 | Cluster RCT | 11 | GP visits (mean), NP visits (mean) | Decrease | No sig. effect | ED visits (mean) | Decrease | No sig. effect | Hospital inpatient care | Increase | No |
| Anderson and Scott, 199228 | UK | Male | 12 | 154/80/74 | RCT | 13 | Consultation Rate (mean) | Increase | No sig. effect | NA | NA | Episode Rate (mean) | Increase | No sig. effect | |
| Fleming et al., 200440 | US | Diabetic, hyperten-sive, other medical | 12 | 13570/65 | RCT | 16 | NA | NA | ED visit in last 12 months, urgent care visit in last 12 months | Not given | No sig. effect | Hospitali-zation in last 12 months | Not given | No sig. effect | |
| Fleming et al., 199719 | US | General | 6, 12 | 774/392/382 | RCT | 16 | NA | NA | ED visits in last 6 months | Decrease | No sig. effect | Hospital days | Decrease | No sig. effect | |
| Senft et al., 199741 | US | General | 12 | 514/260/254 | RCT | 15 | Outpatient visits (mean) | Increase | No sig. effect | NA | NA | Hospitali-zation rate | Increase | No sig. effect | |
| Fleming et al., 200020 | US | General | 6, 12 | 774/392/382 | RCT | 16 | NA | NA | ED visits in last 6 months | Decrease | No sig. effect | Hospital days | Decrease | Sig. effect | |
| Fleming et al., 200221 | US | General | 48 | 774/392/382 | RCT | 16 | NA | NA | ED visits in last 6 months | Decrease | Sig. effect | Hospital days | Decrease | Sig. effect | |
| Freeborn et al., 200042 | US | General | 24 | 514/260/254 | RCT | 15 | Outpatient visits (mean, if any) | Decrease | No sig. effect | NA | NA | Mean Hospital days (if any) | Decrease | No sig. effect | |
| Mundt et al., 200624 | US | General | 12 | 774/392/382 | RCT | 16 | NA | NA | Total no. ED visits | Decrease | Not tested | Total no. days hospitalized | Decrease | Not tested | |
| Bray et al., 200718 | US | General | 12 | 3628/1945/1683 | Cluster RCT | 12 | Outpatient visits (mean), | Mixed | No sig. effect | ED visits (mean) | Mixed | No sig. effect | Inpatient days (mean), ADM days (mean) | Mixed | No sig. effect |
| Fleming et al., 199925 | US | Older Adults | 6, 12 | 158/87/71 | RCT | 15 | NA | NA | ED visits in last 6 months | Not given | No sig. effect | Hospital days | Not given | No sig. effect | |
| Mundt et al., 200526 | US | Older Adults | 24 | 158/87/71 | RCT | 15 | NA | NA | ED visits in last 6 months | Not given | No sig. effect | Hospital days | Not given | No sig. effect | |
| Copeland et al., 200343 | US | Veteran | 9, 18 | 205/100/105 | RCT | 12 | Total outpatient stops (mean) | Increase | sig. effect | NA | NA | Total inpatient stops (mean) | Increase | No sig. effect | |
| Scott and Anderson, 199027 | US | Women | 12 | 72/33/39 | RCT | 12 | Consultation rate (mean) | Decrease | No sig. effect | NA | NA | Episode Rate (mean) | Decrease | No sig. effect | |
| Manwell et al., 200022 | US | Women | 48 | 205/103/102 | RCT | 16 | NA | NA | ED visits in last 6 months | Decrease | No sig. effect | Hospital days | Decrease | No sig. effect | |
| Grossberg et al., 200423 | US | Young Adults | 48 | 226/114/112 | RCT | 16 | NA | NA | ED visits | Decrease | Sig. effect | Hospital days | Decrease | No sig. effect | |
| ED Setting | |||||||||||||||
| Daeppen et al., 200744 | Switzer-land | Injured | 12 | 770/236/534 | RCT | 12 | Medical consultations (mean) | Increase | No sig. effect | NA | NA | Hospital days (mean) | Increase | No sig. effect | |
| Crawford et al., 200429 | UK | General | 12 | 377/182/195 | RCT | 13 | NA | NA | ED visits (mean) | Decrease | Sig. effect | NA | NA | - | |
| Barrett et al., 200630 | UK | General | 12 | 290/131/159 | RCT | 13 | Outpatient hospital visit (mean), GP contacts (mean) | Increase | Not tested | ED visits (mean), | Decrease | Not tested | Inpatient days (mean) | Decrease | Not tested |
| Gentilello et al., 199945 | US | General | 12 | 409/194/215 | RCT | 14 | NA | NA | - | Risk of repeat injury requiring ED visit (%) | Decrease | Sig. effect | NA | NA | - |
| Non-ED Hospital Setting | |||||||||||||||
| Shourie et al., 200646 | Australia | Overnight Surgery Patients | 6 | 106/45/61 | QE | 8 | GP visits | No change | No sig. effect | NA | NA | Hospital readmission rate (%) | No change | No sig. effect | |
| Watson et al., 199947 | UK | General | 12 | 102/71/31 | QE | 7 | GP visits | Not given | No sig. effect | NA | NA | Hospital visits | Not given | No sig. effect | |
| Saitz et al., 200748 | US | Inpatient | 12 | 287/141/146 | RCT | 13 | NA | NA | ED visits | Not given | No sig. effect | Hospital days | Not given | No sig. effect | |
| Storer, 200349 | US | Military | 12 | 444/206/238 | Obser-vation | 5 | NA | NA | - | NA | NA | Hospital days (mean), hospital readmission rate (%) | Not given, Decrease | Not tested, sig. effect | |
Note: Int = intervention, Con = control, ADM = alcohol, drug, or mental health, ED = emergency department, GP = general practitioner, NP = nurse practitioner, RCT = randomized control trial, QE = quasi-experimental
Table 2 summarizes the findings by type of care and setting. In the primary care setting, 11 of the 21 publications measured outpatient care. The evidence appears to be evenly split between decreased and increased utilization, suggesting no real effect. One publication35 found a statistically significant decrease in outpatient utilization, and 3 others27,39,42 reported decreases that were not statistically significant. One publication43 found a statistically significant increase in outpatient utilization, and 4 reported increases that were not statistically significant.28,34,38,41 Tomson et al.37 found no differences at follow-up.
Table 2. Summary of Health Care Utilization Outcomes Identified in the Systematic Review.
| Primary Care Setting | ED Setting | Non-ED Hospital Setting | |
|---|---|---|---|
| Outpatient utilization measured | 11 of 21 | 2 of 4 | 2 of 4 |
| Significant decrease | 1 | - | - |
| Non-significant decrease | 3 | - | - |
| Significant increase | 1 | - | - |
| Non-significant increase | 4 | 2 | - |
| No effect or mixed effect | 2 | - | 2 |
| ED utilization measured | 11 of 21 | 3 of 4 | 1 of 4 |
| Significant decrease | 2 | 2 | - |
| Non-significant decrease | 5 | 1 | - |
| Significant increase | - | - | - |
| Non-significant increase | - | - | - |
| No effect or mixed effect | 4 | - | 1 |
| Inpatient utilization measured | 19 of 21 | 2 of 4 | 4 of 4 |
| Significant decrease | 2 | - | 1 |
| Non-significant decrease | 7 | 1 | - |
| Significant increases | - | - | - |
| Non-significant increases | 6 | 1 | - |
| No effect or mixed effect | 4 | - | 3 |
Note: ED = emergency department
For ED care, the evidence in the primary care setting indicates a statistically insignificant decrease in ED utilization (11 of 21 possible). Two TrEAT publications21,23 reported a statistically significant decrease. The remaining Project TrEAT publications19,20,22,24 and 1 independent publication39 reported decreases that were statistically insignificant.
For inpatient care, the evidence in the primary care setting (19 of 21 possible) suggests no real effect, with little consensus on the direction or magnitude of any potential effect. Two Project TrEAT publications reported statistically significant decreases,20,21 and 7 other publications reported decreases that were statistically insignificant; 4 use TrEAT data,19,22-24 and 3 are independent.27,36,42 Six publications28,34,37,39,41,43 reported increases in inpatient utilization that were statistically insignificant.
Across all 3 types of care in the primary care setting, several publications reported mixed results or no effect. Bray et al.18 reported mixed, insignificant results. Project GOAL25,26 and 1 independent publication40 indicated no differences.
Findings for health care utilization in the ED and non-ED hospital settings were inconclusive largely due to an insufficient number of publications. There were no statistically significant findings for outpatient care in the ED setting; 2 publications30,44 found an insignificant increase in outpatient care. Both St. Mary's study publications found reduced ED care; Crawford et al.29 was statistically significant, but Barrett et al.30 was statistically insignificant. For inpatient care, there was 1 statistically significant decrease,45 1 statistically insignificant decrease,30 and 1 statistically insignificant increase.44
In the non-ED hospital setting, 1 statistically significant decrease was found for inpatient care.49 Three other publications found mixed or no effects for outpatient and ED care.46-48
Meta-Analysis
The following publications were excluded from the meta-analysis because complete data were not available: Israel et al.,35 Fleming et al.,40 Kristenson et al.,36 Tomson et al.,37 and Freeborn et al.46 Several publications were also excluded because another publication used the same data source but provided more relevant estimates, usually with a longer follow-up or objective data: Fleming et al.,19,20,25,40 Mundt,24 and Senft and Polen.41 Two publications were excluded because they used a cluster randomized design.18,39 All but 3 publications46,47,49 were of sufficiently high quality to include in the meta-analysis.
Figure 1a suggests a small, insignificant positive effect of SBI on outpatient care (SMD = 0.13). The I-squared of 53.4% indicates that more than half of the variance in effect size is accounted for by between-publication differences, and the null hypothesis of homogeneity is rejected. Thus, no conclusion can be drawn about the direction or magnitude of the overall effect. Finally, there were no differences between the results of this specification and the alternative specification that included additional Project TrEAT and St. Mary's publications.
Figure 1. Meta-analytic results for outpatient and ED care.
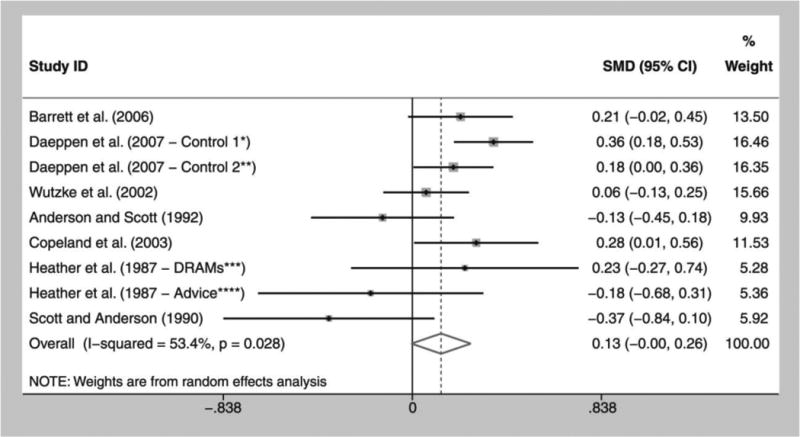
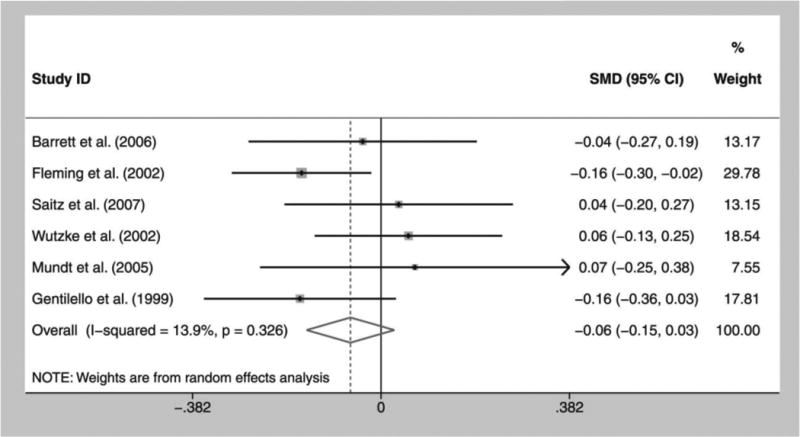
Figure 1a. Outpatient care forest plot
Figure 1b. Emergency department care forest plot
Figure 1a and 1b Legend: *Control 1: Intervention vs. control with assessment
**Control 2: Intervention vs. control without assessment
***Drinking reasonably and moderately with self-control (DRAMs): DRAMs scheme vs. control
****Advice: Simple advice vs. control
Caption: Effect sizes are Hedges d (i.e., within-group effect sizes) with random effects. Error bars represent 95% confidence intervals. The I-squared statistic measures heterogeneity across estimates.
Figure 1b suggests a small, statistically insignificant negative effect (SMD = −0.06) for ED care. There is also low heterogeneity (I-squared = 13.9%), and the null hypothesis of homogeneity for ED utilization is not rejected, allowing for greater confidence in this result. Compared with this specification, the effect size of the alternative analysis for ED utilization increased (SMD = −0.10) and attained statistical significance. ED utilization may or may not be significantly reduced; it appears that the 2 Project TrEAT publications and additional publications from the St. Mary's study, especially Grossberg et al.,23 are weighted heavily in the analysis and shift the confidence intervals for the ED effect size. In any case, the effect sizes do not eclipse 0.10 and must be considered marginal.
Results of the inpatient care analysis (not shown) indicated very little overall effect (SMD = 0.02, 95% CI: –0.12, 0.15). Moderate to high heterogeneity (I-squared = 69.7%, P = 0.001) prevented further interpretation of the pooled SMD.
Discussion
Systematic Review
The systematic review suggests that SBI has little to no effect on inpatient or outpatient health care utilization but may reduce ED utilization. Most publications reporting effects of SBI on health care utilization were conducted in primary care settings. Among these publications, most results were statistically insignificant for outpatient and inpatient health care utilization. Furthermore, although both statistically significant increases and decreases were reported, results were approximately evenly distributed between positive and negative effects, suggesting there is no effect. In contrast, a more consistent sign pattern was indicated for changes in ED utilization associated with SBI provided in a primary care setting. Seven of 11 publications reported decreases in health care utilization (but only 1 of the 7 was statistically significant).
Relatively few publications examined changes in health care utilization associated with SBI delivered in ED or non-ED hospital settings. The systematic review found evidence that SBI delivered in an ED setting may reduce ED utilization. All 3 publications examining ED utilization reported decreases in utilization, and 2 reported statistically significant decreases. Across all types of health care utilization, SBI delivered in non-ED hospital settings appears to have no effect on health care utilization.
Another finding of the systematic review is the inconsistent and incomplete reporting by many publications on health care utilization outcomes. For example, 25% of publications from the primary care setting reported no effect of SBI on inpatient health care utilization but provided no information on the direction, magnitude, or variance of the estimate. Although this information might seem irrelevant for small and statistically insignificant effects, it is critically important for systematic reviews and meta-analyses because it helps establish cross-publications trends that might indicate small yet meaningful effects. The absence of such information is an unfortunate casualty of space limits and reduces the ability to perform rigorous meta-analyses.
Meta-Analysis
The results of the meta-analysis support the inferences from the systematic review. For all publications, a small and statistically insignificant decrease was found for ED care. However, when multiple publications from the same underlying study (e.g., TrEAT) were included in the analysis, the ED care finding was statistically significant. Furthermore, the ED utilization analysis had minimal heterogeneity, suggesting that the average effect adequately represents the literature. Thus, although the analysis does not demonstrate a particularly robust effect, it supports a tentative conclusion of a small decrease in ED care. This result is consistent with a decrease in the likelihood of accidents and injuries resulting from reduced alcohol consumption.
No significant effect was found for outpatient or inpatient health care utilization, and the inpatient effect size was essentially zero. Although a small and potentially meaningful increase in outpatient utilization was found, the effect was insignificant, and the substantial heterogeneity across publications suggests that this effect may not adequately represent the results of the literature. The statistically insignificant increase in outpatient care and the absence of an effect for inpatient care are not necessarily unexpected. SBI was developed for risky, nondependent drinkers who are less likely than dependent users to face major chronic health care events or treatment requiring inpatient stays as an effect of their alcohol use. A small increase in outpatient utilization could signify a targeted use of treatment and support services through primary care providers or outpatient counselors, a standard message of SBI.
Heterogeneity accounts for much of the variance for the outpatient and inpatient care analyses. High levels of heterogeneity are common in SBI meta-analyses.1,2,7,9,10 The limited number of publications prevented the use of conventional statistical tests (e.g., tests of publication bias) to examine heterogeneity further. The potential sources of heterogeneity can therefore only be discussed speculatively. Potential sources are differences in SBI setting and protocol, international regulatory differences across study settings, differences in the definition of type of care, and differences in data collection methods across publications.
The differing SBI protocols across setting and population are a potential source of heterogeneity. As noted in Ballesteros et al.,1 2 factors contributing to this variance are the authors' definition of risky drinking and the types of individuals included in the SBI protocol. The definition of risky drinking may or may not include heavy drinkers and may or may not have a stepped-intervention based on the level of drinking, where dosage increased with higher levels of drinking. Another distinction raised by Ballesteros et al. was whether the publications included treatment seekers and non-treatment seekers. Furthermore, there is an issue of whether the treatment effect is measured against a usual care, or control group, or against a simple advice group.10
The high number of international publications in our analysis may also contribute to the high level of heterogeneity across studies on outpatient care and inpatient care. For outpatient care, 5 publications were UK-based, 2 were Swiss-based, 1 was Australian-based, and 1 was US-based. For inpatient care, 3 publications were UK-based, 3 were US-based, 2 were Swiss-based, and 1 was Australian-based. In contrast, the ED care analysis included 4 US-based, 1 UK-based, and 1 Australian-based publication. The ED care analysis had the highest concentration of observations from 1 country and the lowest level of heterogeneity, whereas the inpatient care analysis had the least concentrated sample and highest level of heterogeneity; thus, the varying regulatory environments in the host countries may be a key source of heterogeneity across the inpatient and outpatient health care utilization results.
The definitions of the types of care (outpatient, inpatient, and ED) are another potential source of heterogeneity. There is not a standard definition across publications, so similar outcomes must be combined to find enough observable data points. For example, several publications27,28,38 include general practitioner consultations as outpatient care. Wutkze et al.34 include a more global “outpatient visits,” and Copeland et al.43 use “outpatient medical stops.” ED and inpatient care had more standardized definitions across publications, suggesting that the health care utilization definition was less of a contributor to heterogeneity for those outcomes.
In addition to varying definitions, publications used varying approaches to collecting health care utilization data. Some publications used health care claims data or medical records, whereas others used self-reported measures. In the current analyses, 2 of 9 outpatient care publications, 5 of 6 ED care publications, and 4 of 9 inpatient care publications used objective health care data. The low proportion of publications using objective health care data in the outpatient and inpatient utilization analyses may contribute to the heterogeneity in those analyses.
A key limitation of this meta-analysis is the limited sample size. Of the 29 separate publications found in the systematic review, 11 – or less than 50% – were included in the meta-analysis. Several prominent and rigorous trials18,36,39,42 were omitted from the meta-analysis; all except Bray et al.18 indicate significant decreases in utilization. Two were omitted because insufficient data were available36,42 and two were omitted because they utilized a cluster randomized design.18,39 Because there were not enough publications to conduct an Egger test, publication or dissemination bias was not examined.
An additional consideration is the exclusion of non-English publications. Given the high heterogeneity present in outpatient and inpatient care, including additional publications from multiple countries would further dampen any interpretation of the results. Inclusion of non-English publications for ED care could affect the results of this meta-analysis, but because the outcomes and quality of these publications cannot be readily assessed, it is difficult to surmise the magnitude and direction of those inclusion effects.
This systematic review and meta-analysis has 2 implications for the SBI field: (1) more evidence is needed on the effect of SBI on health care utilization, and (2) more evidence is needed on SBI conducted in non-primary care settings. The systematic review highlighted the lack of available data for SBI conducted in ED and non-ED hospital settings and the need for more complete and consistent reporting on health care utilization effects across all settings.
While the meta-analysis suggests that SBI may be associated with decreased health care utilization, the effect sizes are very small and insignificant. These results also support the conclusions of studies on the cost-effectiveness of SBI that most publications do not collect the necessary information for robust economic analyses, and there is not enough independent data in the field to robustly support policy. Nonetheless, results of this analysis suggest cautious optimism that SBI may reduce ED utilization. Because ED care is generally very expensive, SBI may indeed reduce overall health care costs as a result.
Acknowledgments
This study was supported by NIAAA grant no. R01 AA013925.
References
- 1.Ballesteros J, Duffy JC, Querejeta I, Arińo J, González-Pinto A. Efficacy of brief interventions for hazardous drinkers in primary care: systematic review and meta-analyses. Alcohol Clin Exp Res. 2004;28(4):608–618. doi: 10.1097/01.alc.0000122106.84718.67. [DOI] [PubMed] [Google Scholar]
- 2.Bertholet N, Daeppen J, Wietlisbach V, Fleming MF, Burnand B. Reduction of alcohol consumption by brief alcohol intervention in primary care: systematic review and meta-analysis. Arch Intern Med. 2005;165:986–995. doi: 10.1001/archinte.165.9.986. [DOI] [PubMed] [Google Scholar]
- 3.Bien TH, Miller WR, Tonigan JS. Brief interventions for alcohol problems: a review. Addiction. 1993;88:315–336. doi: 10.1111/j.1360-0443.1993.tb00820.x. [DOI] [PubMed] [Google Scholar]
- 4.D'Onofrio G, Degutis LC. Preventive care in the emergency department: screening and brief intervention for alcohol problems in the emergency department: a systematic review. Acad Emerg Med. 2002;9(6):627–638. doi: 10.1111/j.1553-2712.2002.tb02304.x. [DOI] [PubMed] [Google Scholar]
- 5.Emmen MJ, Schippers GM, Bleijenberg G, Wollersheim H. Effectiveness of opportunitistic brief interventions for problem drinking in a general hospital setting: systematic review. BMJ. 2004;328(318):1–5. doi: 10.1136/bmj.37956.562130.EE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kahan M, Wilson L, Becker L. Effectiveness of physician-based interventions with problem drinkers: a review. Can Med Assoc J. 1995;152(6):851–859. [PMC free article] [PubMed] [Google Scholar]
- 7.Kaner EF, Dickinson HO, Beyer FR, et al. Effectiveness of brief alcohol interventions in primary care populations (review) Cochrane Database Syst Rev. 2007;18(2):CD004148. doi: 10.1002/14651858.CD004148.pub3. [DOI] [PubMed] [Google Scholar]
- 8.Moyer A, Finney JW, Swearingen CE, Vergun P. Brief interventions for alcohol problems: a meta-analytic review of controlled investigations in treatment-seeking and non-treatment-seeking populations. Addiction. 2002;97:279–292. doi: 10.1046/j.1360-0443.2002.00018.x. [DOI] [PubMed] [Google Scholar]
- 9.Poikolainen K. Effectiveness of brief intervention to reduce alcohol intake in primary health care populations: a meta-analysis. Prev Med. 1999;28:503–509. doi: 10.1006/pmed.1999.0467. [DOI] [PubMed] [Google Scholar]
- 10.Vasilaki EI, Hosier SG, Cox WM. The efficacy of motivational interviewing as a brief intervention for excessive drinking: a meta-analytic review. Alcohol Alcohol. 2006;41(3):328–335. doi: 10.1093/alcalc/agl016. [DOI] [PubMed] [Google Scholar]
- 11.Whitlock EP, Polen MR, Green CA, Orleans T, Klein J. Behavioral counseling interventions in primary care to reduce risky/harmful alcohol use by adults: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2004;140(7):557–568. doi: 10.7326/0003-4819-140-7-200404060-00017. [DOI] [PubMed] [Google Scholar]
- 12.Wilk AI, Jensen NM, Havinghurst TC. Meta-analysis of randomized control trials addressing brief interventions in heavy alcohol drinkers. J Gen Intern Med. 1997;12:274–283. doi: 10.1046/j.1525-1497.1997.012005274.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Solberg LI, Maciosek MV, Edwards NM. Primary care intervention to reduce alcohol misuse: ranking its health impact and cost effectiveness. Am J Prev Med. 2008;34(2):143–152. doi: 10.1016/j.amepre.2007.09.035. [DOI] [PubMed] [Google Scholar]
- 14.Mortimer F, Segal L. Economic evaluation of interventions for problem drinking and alcohol dependence: cost per QALY estimates. Alcohol Alcohol. 2005;40(6):549–555. doi: 10.1093/alcalc/agh192. [DOI] [PubMed] [Google Scholar]
- 15.Kraemer KL. The cost-effectiveness and cost-benefit of screening and brief intervention for unhealthy alcohol use in medical settings. Substance Abuse. 2007;28(3):67–77. doi: 10.1300/J465v28n03_07. [DOI] [PubMed] [Google Scholar]
- 16.Latimer N, Guillaume L, Goyder E, Chilcott J, Payne N. Prevention and Early Identification of Alcohol Use Disorders in Adults and Young People: Screening and Brief Interventions: Cost Effectiveness Review. Sheffield: ScHARR Public Health Collaborating Centre; 2009. [Google Scholar]
- 17.Substance Abuse and Mental Health Services Administration. [Accessed March 14, 2010];Screening, brief intervention and referral to treatment. Available at: http://sbirt.samhsa.gov.
- 18.Bray JW, Zarkin GA, Davis KL, Mitra D, Higgins-Biddle JC, Babor TF. The effect of screening and brief intervention for risky drinking on health care utilization in managed care organizations. Med Care. 2007;45:177–182. doi: 10.1097/01.mlr.0000252542.16255.fc. [DOI] [PubMed] [Google Scholar]
- 19.Fleming MF, Barry KL, Manwell LB, Johnson K, London R. Brief physician advice for problem alcohol drinkers. JAMA. 1997;277:1039–1045. [PubMed] [Google Scholar]
- 20.Fleming MF, Mundt MP, French MT, Manwell LB, Stauffacher EA, Barry KL. Benefit-cost analysis of brief physician advice with problem drinkers in primary care settings. Med Care. 2000;38(1):7–18. doi: 10.1097/00005650-200001000-00003. [DOI] [PubMed] [Google Scholar]
- 21.Fleming MF, Mundt MP, French MT, Manwell LB, Stauffacher EA, Barry KL. Brief physician advice for problem drinkers: long-term efficacy and benefit-cost analysis. Alcohol Clin Exp Res. 2002;26(1):36–43. [PubMed] [Google Scholar]
- 22.Manwell LB, Fleming MF, Mundt MP, Stauffacher EA, Barry KW. Treatment of problem alcohol use in women of childbearing age: results of a brief intervention trial. Alcohol Clin Exp Res. 2000;24(10):1517–1524. [PubMed] [Google Scholar]
- 23.Grossberg PM, Brown DD, Fleming MF. Brief physician advice for high-risk drinking among young adults. Ann Fam Med. 2004;2:474–480. doi: 10.1370/afm.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mundt MP. Analyzing the cost and benefits of brief intervention. Alcohol Research & Health. 2006;29(1):34–36. [PMC free article] [PubMed] [Google Scholar]
- 25.Fleming MF, Manwell LB, Barry KL, Adams W, Stauffacher EA. Brief physician advice for alcohol problems in older adults: a randomized community-based trial. J Fam Pract. 1999;48(5):378–384. [PubMed] [Google Scholar]
- 26.Mundt MP, French MT, Roebuck MC, Manwell LB, Barry KL. Brief physician advice for problem drinking among older adults: an economic analysis of costs and benefits. J Stud Alcohol. 2005;66:389–394. doi: 10.15288/jsa.2005.66.389. [DOI] [PubMed] [Google Scholar]
- 27.Scott E, Anderson P. Randomized controlled trial of general practitioner intervention in women with excessive alcohol consumption. Drug Alcohol Rev. 1990;10:313–321. doi: 10.1080/09595239100185371. [DOI] [PubMed] [Google Scholar]
- 28.Anderson P, Scott E. The effect of general practicioner's advice to heavy drinking men. Br J Addict. 1992;87:891–900. doi: 10.1111/j.1360-0443.1992.tb01984.x. [DOI] [PubMed] [Google Scholar]
- 29.Crawford MJ, Patton R, Touquet R, et al. Screening and referral for brief intervention of alcohol-misusing patients in an emergency department: a pragmatic randomised controlled trial. The Lancet. 2004;364(9442):1334–1339. doi: 10.1016/S0140-6736(04)17190-0. [DOI] [PubMed] [Google Scholar]
- 30.Barrett B, Byford S, Crawford MJ, et al. Cost-effectiveness of screening and referral to an alcohol health worker in alcohol misusing patients attending an accident and emergency department: a decision-making approach. Drug Alcohol Depend. 2006;81:47–54. doi: 10.1016/j.drugalcdep.2005.05.015. [DOI] [PubMed] [Google Scholar]
- 31.Miller WR, Brown JM, Simpson TL. What works? A methodological analysis of the alcohol treatment outcome literature. In: Hester RK, Miller WR, editors. Handbook of Alcohol Treatment Approaches, Effective Alternatives. 2nd. Boston: Allyn and Bacon; 1991. [Google Scholar]
- 32.Miller WR, Willbourne PL. Mesa Grande: a methodological analysis of clinical trials of treatments for alcohol use disorders. Addiction. 2002;97:265–277. doi: 10.1046/j.1360-0443.2002.00019.x. [DOI] [PubMed] [Google Scholar]
- 33.Lipsey MW, Wilson DB. Practical Meta-analysis. Thousand Oaks: Sage Publications; 2001. [Google Scholar]
- 34.Wutzke SE, Congrave KM, Saunders JB, Hall WD. The long-term effectiveness of brief interventions for unsafe alcohol consumption: a 10-year follow-up. Addiction. 2002;97:665–675. doi: 10.1046/j.1360-0443.2002.00080.x. [DOI] [PubMed] [Google Scholar]
- 35.Israel Y, Hollander O, Sanchez-Craig M, et al. Screening for problem drinking and counseling by the primary care physician-nurse team. Alcohol Clin Exp Res. 1996;20(8):1443–1450. doi: 10.1111/j.1530-0277.1996.tb01147.x. [DOI] [PubMed] [Google Scholar]
- 36.Kristenson H, Oehlin H, Hulten-Nosslin MB, Trell E, Hood B. Identification and intervention of heavy drinking in middle-aged men: results and follow-up of 24-60 months of long-term study with randomized controls. Alcohol Clin Exp Res. 1983;7(2):203–209. doi: 10.1111/j.1530-0277.1983.tb05441.x. [DOI] [PubMed] [Google Scholar]
- 37.Tomson Y, Romelsjo A, Aberg H. Excessive drinking-brief intervention by a primary care nurse. Scand J Prim Health Care. 1998;16:188–192. doi: 10.1080/028134398750003160. [DOI] [PubMed] [Google Scholar]
- 38.Heather N, Campion PD, Neville RG, MacCabe D. Evaluation of a controlled drinking minimal intervention for problem drinkers in general practice (the DRAMS scheme) J R Coll Gen Pract. 1987;37:358–363. [PMC free article] [PubMed] [Google Scholar]
- 39.Lock CA, Kaner E, Heather N, et al. Effectiveness of nurse-led brief alcohol intervention: a cluster randomized controlled trial. J Adv Nurs. 2006;54(4):426–439. doi: 10.1111/j.1365-2648.2006.03836.x. [DOI] [PubMed] [Google Scholar]
- 40.Fleming MF, Brown R, Brown D. The efficacy of a brief alcohol intervention combined with %CDT feedback in patient being treated for type 2 diabetes and/or hypertension. J Stud Alcohol. 2004;65:631–637. doi: 10.15288/jsa.2004.65.631. [DOI] [PubMed] [Google Scholar]
- 41.Senft RA, Polen MR. Brief intervention in a primary care setting for hazardous drinkers. Am J Prev Med. 1997;13(6):464–470. [PubMed] [Google Scholar]
- 42.Freeborn DK, Polen MR, Hollis JF, Senft RA. Screening and brief intervention for hazardous drinking in an HMO: effects on medical care utilization. J Behav Health Serv Res. 2000;27:446–453. doi: 10.1007/BF02287826. [DOI] [PubMed] [Google Scholar]
- 43.Copeland LA, Blow FC, Barry KL. Health care utilization by older alcohol-using veterans: effects of a brief intervention to reduce at-risk drinking. Health Educ Behav. 2003;30(3):305–321. doi: 10.1177/1090198103030003006. [DOI] [PubMed] [Google Scholar]
- 44.Daeppen J, Gaume J, Bady P, et al. Brief alcohol intervention and alcohol assessment do not influence alcohol use in injured patients treated in the emergency department: a randomized controlled clinical trial. Addiction. 2007;102(8):1224–1233. doi: 10.1111/j.1360-0443.2007.01869.x. [DOI] [PubMed] [Google Scholar]
- 45.Gentilello LM, Rivara FP, Donovan D, et al. Alcohol interventions in a trauma center as a means of reducing the risk of injury recurrence. Ann Surg. 1999;230(4):473–483. doi: 10.1097/00000658-199910000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shourie S, Conigrave KM, Proude EM, Ward JE, Wutzke SE, Haber PS. The effectiveness of a tailored intervention for excessive alcohol consumption prior to elective surgery. Alcohol Alcohol. 2006;41(6):643–649. doi: 10.1093/alcalc/agl059. [DOI] [PubMed] [Google Scholar]
- 47.Watson HE. A study of minimal interventions for problem drinkers in acute care settings. Int J Nurs Stud. 1999;36:425–434. doi: 10.1016/s0020-7489(99)00028-0. [DOI] [PubMed] [Google Scholar]
- 48.Saitz R, Palfai TP, Cheng DM, et al. Brief intervention for medical inpatients with unhealthy alcohol use: a randomized, controlled trial. Ann Intern Med. 2007;146:167–176. doi: 10.7326/0003-4819-146-3-200702060-00005. [DOI] [PubMed] [Google Scholar]
- 49.Storer RM. A simple cost-benefit analysis of brief interventions on substance abuse at Naval Medical Center Portsmouth. Mil Med. 2003;168(9):765–768. [PubMed] [Google Scholar]


