Abstract
Storm-related carbon monoxide (CO) poisoning outbreaks occurred in Connecticut in 2011 and 2012, despite efforts to improve public messaging. We describe the cases and incidents and identify possible preventive interventions. We defined cases as blood carboxyhemoglobin ≥9.0% among persons exposed to alternative power or heat sources because of storm-related losses. We identified 133 cases, including 3 deaths, in 2011 and 30 in 2012, associated with 72 and 11 incidents, respectively. Racial/ethnic minorities were overrepresented (60% of 2011 patients; 48% in 2012), compared with Connecticut’s minority population (29%). Generator or charcoal misuse (83% in 2011; 100% in 2012) caused the majority of incidents. Few CO-source operators recalled media or product CO warnings. Incorrect generator and charcoal use, racial/ethnic disparities, and incomplete penetration of warning messages characterized both outbreaks. A multifaceted approach is needed to decrease postdisaster CO poisonings.
Keywords: carbon monoxide poisoning, disaster medicine, environmental exposure, communications media, hazardous substances
Annually in the United States, unintentional carbon monoxide (CO) poisoning is a substantial cause of acute toxic substance poisoning-related morbidity and mortality. An average of 15,000–20,000 hospital visits and 450 deaths yearly are attributable to unintentional, non–fire-related CO poisoning.1–3 The true exposure incidence is probably higher because signs and symptoms of CO poisoning can be nonspecific. According to national poison control center data, thousands of persons per year do not present for medical care after calling regarding possible CO exposures.4
On October 29, 2011, a severe storm left 6–18 inches of heavy wet snow throughout much of Connecticut, causing downed trees, power lines, and supply towers and leaving >860,000 customers without power—many for approximately 2 weeks.5 Early inquiries by the Connecticut Department of Public Health (CDPH) to the state poison control center and hospital emergency departments indicated an increase in CO poisoning cases substantially greater than baseline in what became one of the largest CO poisoning outbreaks recorded in the United States.6–8
Exactly 1 year later, on October 29, 2012, Hurricane Sandy brought high winds and coastal flooding to Connecticut, damaging power plants and downing trees and power lines, leaving >625,000 customers without power for a week.9 Three days before Hurricane Sandy was due to arrive in Connecticut, CDPH launched a multimedia campaign warning the public about CO poisoning; this campaign included enhanced outreach to racial/ethnic minorities and messaging to local public health personnel and first responders. Nevertheless, another CO poisoning outbreak occurred. We describe the extent of both outbreaks, patient and exposure incident characteristics, and implications for prevention strategies.
Methods
In Connecticut, blood carboxyhemoglobin (COHb) levels ≥9% are physician- and laboratory-reportable to the Department of Public Health as suspect cases of CO poisoning so that state health officials are alerted to unsafe practices of citizens or employers that might necessitate a public health intervention. Three days after the 2011 storm and 3 days before the 2012 storm, CDPH enhanced its passive reporting of CO poisoning by requesting that laboratories report cases daily. For both storms, we defined an outbreak case of CO poisoning as laboratory-measured COHb ≥9% in a person from an unintentional CO exposure related to the storm and power outage and not related to unintentional fire, during October 29–November 9, 2011, or October 29–November 5, 2012 (from date of storms to date power was restored for >99% of customers). We defined a CO exposure source as CO-producing equipment used to generate electricity or heat. A CO exposure incident was defined as the specific CO exposure circumstance involving 1 or more CO poisoning cases epidemiologically linked by location and time. An affected household refers both to the physical location of the CO-producing source equipment and to the persons exposed at that location. The CO exposure source operator was the person responsible for setting up or maintaining the CO-producing equipment or exposure source in an affected household.
After each storm, from November 15 to December 16, 2011 and from November 15 to 28, 2012, respectively, the CPDH environmental and infectious disease staff telephoned reported patients and asked them to participate in a standardized questionnaire, which was administered in either English or Spanish. The 2012 questionnaire differed slightly from the 2011 questionnaire: the question order was changed; answer options were clarified; and the country of birth was added. When multiple family members were involved, we attempted to obtain individual patient information on each case reported. However, if necessary, information from a family member or other household proxy was accepted. Additionally, interpreters were used when necessary for households where English was not the primary language spoken. Data collected included information regarding both cases and CO exposure incidents. Basic demographics, symptoms, smoking status, past medical history, and treatment history were collected for each patient. Information about CO exposure source equipment, including placement, reason for use, experience of source operator, training received, and safety practices and awareness of CO warning messages, was assessed. Incorrect generator placement was defined as placement inside living space, basement, or attached structure, including garage or enclosed porch, or outdoors but <20 feet from the house. Incorrect charcoal grill or kerosene/propane heater placement was defined as placement indoors. Household type and CO alarm use were assessed for each exposure incident. If a patient or proxy could not be reached, we attempted to review hospital records regarding the CO poisoning. Medical record reviews occurred on various dates from December 13, 2011, to January 6, 2012, following the 2011 storm and from November 28, 2011, to January 10, 2013, following the 2012 storm. We also queried the state medical examiner’s office regarding deaths attributable to CO exposure after both storms. For deceased persons, we attempted to interview the next of kin, or if unavailable, we reviewed death certificates. Patient-level data for 2011 and 2012 cases, respectively, was collected by patient interview (76 [57%] and 5 [17%]), proxy interview (34 [26%] and 10 [33%]), chart review (20 [15%] and 10 [33%]), or a combination of interview and chart review (3 [2%] and 5 [17%]). We developed a database by using the Connecticut Electronic Disease Surveillance Suite outbreak module and exported the data for analysis with SAS version 9.2 (SAS Institute, Cary, NC). These investigations underwent the Centers for Disease Control and Prevention (CDC) human subjects review and were determined to be public health practice, not research.
Results
Of 148 suspect cases reported to CDPH after the 2011 storm, 133 cases were determined to be storm-related CO poisonings, including 3 deaths. We excluded 15 suspect cases: 2 related to fire, 2 duplicate reports, 3 with COHb <9%, 2 involving smokers who had no identifiable CO source and who had laboratory studies performed for other purposes, and 6 for which we were unable to obtain information (including 2 CO poisoning–related deaths with unknown CO source). These 133 cases represented 72 separate CO exposure incidents (mean: 2 cases/incident). After Hurricane Sandy in 2012, CDPH received 43 suspect CO poisoning case reports, of which 30 were storm-related CO poisoning cases. We excluded 13 suspect cases: 8 with COHb <9%, 3 not related to power outages, 1 duplicate report, and 1 suicide attempt. These 30 cases represented 11 separate CO exposure incidents (mean: 3 cases/incident).
Patient demographic information for both outbreaks is displayed in Table 1. The majority of CO cases were among males (59% [78] in 2011; 60% [18] in 2012). Median patient age was 38 and 41 years, respectively. Of patients who provided race/ethnicity information, 60% (79 of 131) of cases in the 2011 storm and 48% (14 of 29) of cases in the 2012 storm occurred among racial/ethnic minorities; additionally, 13% of affected households (9 of 72) in 2011 and 44% (4 of 9) in 2012 were non–English-speaking, requiring an interpreter (information involving 2 households in 2012 was acquired by chart review without documentation of spoken language).
Table 1.
Basic Case Demographics, Storm-Related Carbon Monoxide Poisoning Outbreaks, Connecticut, 2011 and 2012
| Characteristic | 2011 (n = 133) | 2012 (n = 30) | State population (US Census Bureau, 2013) |
|---|---|---|---|
| Male | 59% | 60% | 49% |
| Age (years) | |||
| Median | 38 | 41 | 40 |
| Range | 1–86 | 8–93 | |
| 0–17 | 17% | 27% | 23% |
| 18–44 | 45% | 30% | 36% |
| 45–64 | 20% | 33% | 28% |
| ≥65 | 17% | 10% | 13% |
| Race/ethnicity | |||
| Non-Hispanic white | 35% | 53% | 71% |
| Non-Hispanic black | 15% | 0% | 11% |
| Asian/Pacific Islander | 17% | 3% | 4% |
| Hispanic | 28% | 37% | 12% |
| Other or Multirace/ethnicity | 5% | 7% | 2% |
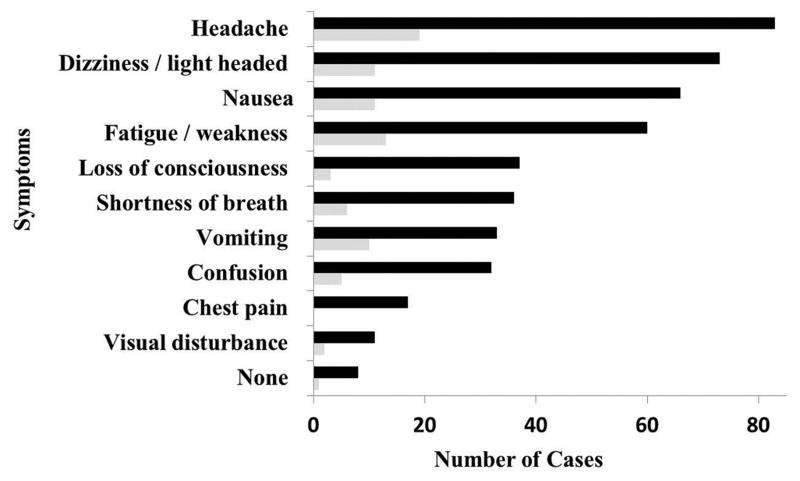
The majority of patients from both storms (94% [125 of 133] in 2011; 97% [29 of 30] in 2012) experienced ≥1 symptom consistent with CO poisoning, usually headache, dizziness, nausea, or fatigue (Figure 1). Among asymptomatic patients, 7 patients from the 2011 storm and 1 from the 2012 storm were identified as having CO poisoning when tested for COHb after other household members were identified as having CO poisoning. Further information regarding the remaining asymptomatic patient from 2011 was unavailable. Clinically significant comorbidities were present in 20% of cases (26 of 133) in the 2011 storm and 10% of cases (3 of 10) in the 2012 storm, with respiratory and heart disease being the most common. The majority of patients in both outbreaks, 78% (93 of 120) and 93% (25 of 27), respectively, reported having never smoked. Of those receiving medical attention, the highest level of care received varied, depending on severity of poisoning and other comorbidities. Normobaric oxygen therapy in the emergency department was used to treat the majority of CO poisonings during both storms, 65% (85 of 130) and 77% (23 of 30), respectively. Hospitalization was required for 15% (20 of 130) and 13% (4 of 30) of patients, respectively, and hyperbaric oxygen therapy for 15% (20 of 130) and 20% (6 of 30), respectively. The remaining 4% (5 of 130) in 2011 either did not require supplemental oxygen or only needed oxygen in transport and did not report needing further treatment in the emergency department. The 3 deaths included in our study from 2011 died without receiving medical care..
Fig. 1.
Symptoms among patients, storm-related carbon monoxide poisoning outbreaks, Connecticut, 2011 (n = 133) and 2012 (n = 30).
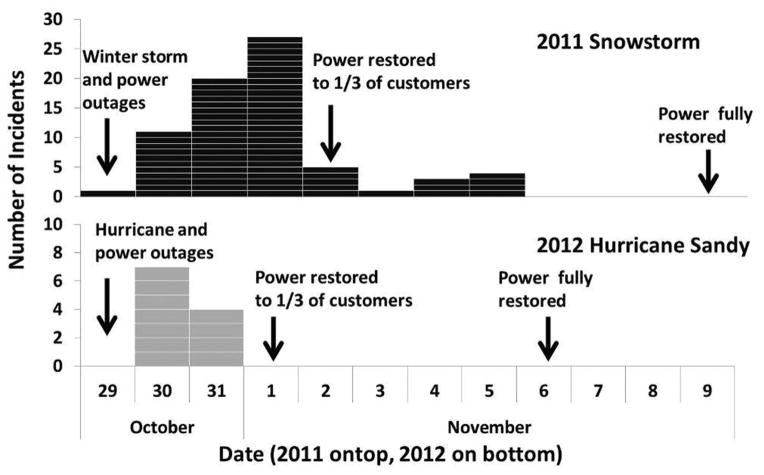
The 72 CO exposure incidents related to the 2011 snowstorm occurred during October 29–November 5, 2011 (Figure 2), with the majority of incidents (82%) occurring within the first 3 days after the storm. The 11 CO exposure incidents associated with the 2012 hurricane all occurred on October 30 or 31, 2012, the first 2 days after the storm. Locations of CO exposure incidents corresponded to areas of greatest snow accumulation and power outages in 2011 and greatest power outages from winds and flooding in 2012. The majority of incidents occurred in urban areas (88% in 2011; 91% in 2012) and in single-family homes (62% in 2011; 56% in 2012), corresponding to the distribution of Connecticut residents, with approximately 88% of the state living in urban areas and 59% living in 1-unit detached homes.
Fig. 2.
Epidemic curve of carbon monoxide poisoning incidents, storm-related carbon monoxide poisoning outbreaks, Connecticut, 2011 (n = 72) and 2012 (n = 11).
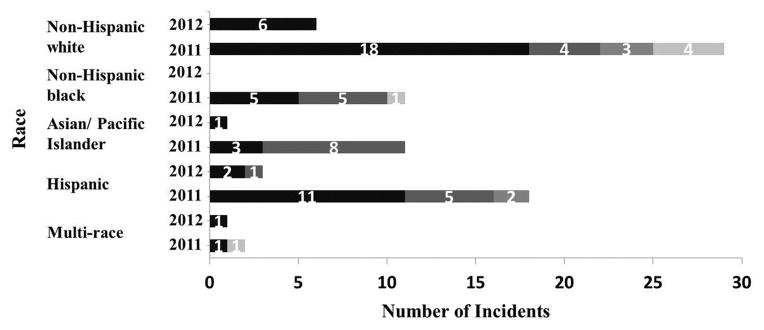
The most common CO sources in both storms were generators (53% [38 of 72] in 2011; 91% [10 of 11] in 2012) and charcoal (31% [22 of 72] and 9% [1 of 11], respectively). In 2011, propane and kerosene heaters, gas furnaces, fireplace use, gas hot water heaters, and gas stoves/ovens were responsible for the remaining incidents. In 2011, CO source type use varied by household primary racial/ethnic group: generators, charcoal, and propane/kerosene heaters were the most common illness-causing CO source among non-Hispanic whites (86% of incidents [25 of 29]); charcoal among Asians (73% [8 of 11]); generators and charcoal among non-Hispanic blacks (91% [10 of 11]); and generators and charcoal among Hispanics (89% [16 of 18]) (Figure 3).
Fig. 3.
Incident carbon monoxide source equipment used by primary race/ethnicity of household, storm-related carbon monoxide poisoning outbreaks, Connecticut, 2011 (n* = 70) and 2012 (n = 11).
Among the generator-associated incidents, 47% of generator operators (16 of 34) in 2011 and 33% (2 of 6) in 2012 bought or borrowed the generator during or immediately after the storm. In both outbreaks, approximately half of persons operating a generator were doing so for the first time. Receiving instruction on safe operation of the generator from a salesperson, family member, or the owner’s manual was reported by 32% of operators (10 of 31) in 2011 and none in 2012. Few operators (22% [7 of 32] in 2011; 17% [1 of 6] in 2012) reported seeing a warning about CO on the generator itself, and none reported receiving a verbal warning about the risk for CO poisoning from generators when purchasing or borrowing the generator. Among charcoal- and kerosene/propane heater-associated incidents in 2011, a total of 8% of responding charcoal grill operators (1 of 12) and 20% of propane heater operators (1 of 5) reported seeing CO warning labels on the charcoal bag or grill or on the heater, respectively. The 1 grill operator in 2012 did not see a warning label on the charcoal bag or on the grill. Incorrect placement accounted for 89% (34 of 38) and 100% (10 of 10) of generator-associated CO poisoning incidents in 2011 and 2012, respectively, and 100% of charcoal- or kerosene/propane heater-associated incidents in both 2011 (27) and 2012 (1). All 3 CO poisoning deaths in 2011 were associated with incorrect generator placement.
Of 54 source equipment operators in 2011, 43% recalled seeing or hearing warnings in the media about the danger of CO poisoning either within the previous year or immediately before or during the storm. After accounting for those who had heard messages during both periods, 62% of non-Hispanic white source equipment operators (13 of 21), compared with 30% of other racial/ethnic groups combined (9 of 30), reported any exposure to messages within the previous year, including immediately before or during the storm. In 2012, only 1 source equipment operator reported hearing warnings about CO poisoning within the previous year, and none had heard messaging immediately before or during the storm.
CO alarms were present in 35% of incident households (21 of 60) in the 2011 storm for which CO alarm information was available. Of the 21 households with a CO alarm, 13 reportedly had CO alarm(s) powered by batteries alone or with battery backup, and in 6 households, the alarm reportedly had sounded. Of the 13 households with a CO alarm that used batteries, 7 reportedly had had the battery changed within the previous 6 months. During the 2012 storm, 1 household had a CO alarm among the 8 exposure incidents with CO alarm information available. This alarm was powered by battery, and the alarm had sounded.
Comment
CO poisoning outbreaks associated with severe weather events have been well documented during the past 2 decades.4,6–8,10–18 Different types of disasters tend to be associated with certain CO exposure sources: gasoline-powered generators, charcoal, and propane/kerosene heat sources after winter and ice storms,6–8,10–12 gasoline-powered generators after hurricanes,13–16 and pressure washers or other gasoline-powered equipment used in cleanup activities after floods.17 Connecticut’s storm-related CO poisoning outbreaks in October 2011 and October 2012 fit this pattern in that the majority of incidents in the snowstorm-associated outbreak in 2011 were caused by generators, charcoal, or propane/kerosene heaters and the majority of the incidents in the hurricane-associated outbreak in 2012 were caused by generators. Connecticut’s 2 outbreaks were also similar to those reported in the scientific literature regarding timing of incidents, unsafe generator or charcoal use, lack of CO alarms, incomplete penetration of warning messaging and labeling, and disproportionate impact on racial/ethnic minorities.
In storm-related CO outbreaks, the majority of cases occur within 3–5 days after the storm, and both the 2011 and 2012 Connecticut outbreaks fit this pattern. An explanation often given is that the number of persons exposed to CO sources for heat or electricity production decreases sharply as power is restored. However, this seems an unlikely explanation for the 2011 outbreak because power was restored to only 1/3 of ~860,000 affected customers by day 5, temperatures remained near or below freezing for another week, and power was not fully restored until day 12. Similarly, during the 2012 outbreak, 1/3 of ~625,000 affected customers remained without power 4 days after the storm, yet all storm-related CO poisonings had occurred within 2 days after the storm.6,9 One possible alternative explanation for the timing of CO poisoning incidents simply might be that unsafe use of CO-producing equipment results in poisoning within the first few days, depending on extent of use.
Although we did not formally assess risk factors for CO poisoning, our findings support existing evidence that unsafe use of generators and charcoal is a major risk factor. CDC recommendations state that generators should be placed outside, >20 feet from one’s home, doors, and windows19 and that charcoal or gas grills should never be used indoors.20 In our outbreaks, 70 of 71 incidents related to generator or grill use were characterized by incorrect placement. Reasons for incorrect placement of generators included weather conditions, concern regarding theft, and extension cord length. For charcoal users, the main reason reported for incorrect placement was the weather (i.e., use of charcoal indoors to heat home or cook indoors because of severe weather outdoors). Although not asked systematically, charcoal users also incorrectly believed that bringing the charcoal grill inside after the charcoal stopped smoking was safe.
A limited number of responders reported having CO alarms in the home, and even fewer had battery-backup alarms in which the batteries had been changed during the previous 6 months, thus compounding the problems of incorrect generator or grill placement. In 7 poisoning incidents, the CO alarm reportedly had sounded. Although not systematically asked, patients reported that they thought the alarm was malfunctioning or that they did not hear the alarm over the noise of the generator. In certain incidents for which the CO alarm reportedly had not sounded, the alarms were located in the basement, away from the CO-producing equipment.
Racial/ethnic disparities have been well documented in postdisaster CO poisoning outbreaks.6–8,10,13,16,18 Such disparities were observed during both the 2011 and 2012 Connecticut outbreaks in which the majority of cases and affected households involved persons of racial/ethnic minorities in 2011 and Hispanics in 2012, compared with the state population.21 Prior studies also have reported that recent immigrants and non–English-speaking persons are at high risk for CO poisoning after disasters.6,10,18 Although we did not collect the data systematically, we determined that in the 2001 outbreak, 13% of cases (representing 13% of CO exposure incidents) required translators to administer the questionnaire and that others spoke English only as a second language. Primary languages other than English included Spanish, Armenian, Vietnamese, Chinese, Greek, and Portuguese.
Warning messages and labels are an important component of preventing postdisaster CO poisonings. Delayed media warnings, not targeting non–English-speaking persons, non-pictorial labels in English only, and not placing warning labels prominently all contribute to postdisaster CO poisonings.11,15 During the 2011 outbreak, television warning messages were not broadcast until days after the snowstorm, but similar television and newspaper warning messages had been distributed 2 months earlier during Tropical Storm Irene. Use of social media, including Twitter and Facebook, to warn citizens of the dangers of CO poisoning began shortly after the storm, after power outages became evident. However, effectiveness of the media campaign for the 2011 storm is called into question because 35% of CO-source operators in the 2011 outbreak had heard or seen warning messages immediately before or during the storm, yet still operated the equipment incorrectly. With regard to product warning labels, the US Consumer Product Safety Commission (CPSC) has required pictorial warning labels on all generators since May 2007 and all charcoal bags since November 1997. However, according to the 1996 CPSC voting document for revision of charcoal bag warning labels, the approved pictogram warning obtained a 74% correct response rate by focus groups, falling short of the recommended 85% used in the American National Standards Institute (ANSI) Z535 testing methods.22 Our study suggests that the effectiveness of warning labels was questionable, with only 19% of generator operators and 4% of charcoal operators in the affected households recalling having seen pictorial warning labels for the 2 outbreaks combined.
On the basis of the case demographics in the 2011 outbreak, CDPH’s Environment and Occupational Health section developed improved educational materials for future use. Posters and Internet fact sheets were created in 10 different languages, and door hangers were made with Spanish on 1 side and English on the other. Posters and door hangers were distributed to town governments for distribution to residents when severe weather events or other disasters threatened community power supplies. Additionally, CDPH’s Office of Communications prepared messaging to be released in anticipation of future storms. During October 26–November 7, 2012, before and during Hurricane Sandy and its aftermath, the Office of Communications issued health alerts to local health departments, multiple press releases, and >100 tweets and Facebook postings; CDPH’s Internet site for Hurricane Sandy,23 which included CO poisoning information, received >7,000 views. In addition, CDPH targeted Spanish-language newspapers and television stations to alert the public to the dangers of CO poisoning before the 2012 hurricane.
Our investigation had certain limitations. Direct comparison with other outbreaks is difficult because different case definitions have been used, depending on the state reporting the outbreak, year of the event, whether smoking history was obtained, and the specific data set used for analysis. Connecticut’s use of a reported laboratory-measured COHb level of ≥9% was established in 1997 on the basis of National Health and Nutrition Examination Survey II data, demonstrating that COHb levels of 3%–8% potentially indicated smoking history rather than CO poisoning and thus only levels ≥9% should be investigated.24,25 Compared with other studies, Connecticut’s case definition is more restrictive, and we might have underestimated the number of cases by not accounting for smoking status.6,11 Additionally, we might have underestimated cases because we excluded symptomatic persons who had CO-oximetry only or who had known exposure to a CO source but no COHb measurement. Laboratories might have failed to report cases during the storm because of staffing shortages or miscommunication regarding enhanced surveillance requirements. Additional CO poisoning cases might have been missed because of delays in testing, resulting in COHb measurements <9%. Recall failure and proxy interviews might have limited our ability to assess behaviors of CO source equipment operators, including exposure to CO warning messaging with >30% source operators not responding to these questions.
Taken together, Connecticut’s 2 outbreaks underscore the multifactorial nature of postdisaster CO poisonings and the need for a multifaceted approach to preventing them. Engineering controls and local requirements for using CO alarms can help counteract less-than-ideal placement of CO-producing alternative power or heat sources. Engineering controls for generators and other gasoline-powered equipment would decrease the CO output of the device. As in automobiles, catalytic converters and fuel-injection systems, if placed on generators, can decrease CO output by >93%.26 However, incorrect placement inside the living space will still lead to eventual accumulation of CO and result in poisoning. Laws that require CO alarms in homes have been reported to decrease severe poisoning and illness in communities affected by disasters.10 Legislation that includes recommendations to have battery-backup CO alarms located near all bedrooms should help reduce the number of CO poisonings. Consideration should also be given to co-locating or packaging CO alarms with CO-producing equipment in stores and rental facilities to encourage use and increase awareness. Both the 1996 CPSC report and our investigation reveal that more work is needed to make warnings understandable and effective for all populations. Continued, periodic reevaluation of product warning labels by CPSC can assist in ensuring they are understandable by persons of different races/ethnicities and that they surpass the ANSI Z535–recommended 85% correct response rate. Optimizing the size and placement of warning labels can improve consumer recognition and reduce risky product use. Assessment and improvement of storm-related media campaigns, with special attention to reaching persons of racial/ethnic minority groups, can increase their effectiveness.
Conclusions and Recommendations
In 2011, after an early snowstorm and massive power outages, Connecticut experienced one of the largest recorded postdisaster CO poisoning outbreaks in the United States; a similar, although smaller, outbreak occurred in 2012 after Hurricane Sandy. In both outbreaks, persons other than non-Hispanic whites were disproportionally affected; generators and charcoal were the primary CO sources identified; unsafe use of CO-producing equipment and lack of functional household CO alarms were common; and effectiveness of mass media warnings and product warning labels was questionable. A multifaceted approach is needed to decrease postdisaster CO poisonings.
Acknowledgments
The authors thank Joan Simpson, Jessica Brockmeyer, Jamie Krasnitski, Paul Gacek, David Kallander, Terry Rabatsky-Ehr, Carmen Marquez, Diana Lejardi, Mira Lami, Celeste Jorge, Fuyen Yip, Jacquelyn Clower, W. Randolph Daley, Andy Smith, and Daniel Chertow for their efforts and support of these investigations.
References
- 1.Centers for Disease Control and Prevention. Unintentional non-fire-related carbon monoxide exposures—United States, 2001–2003. MMWR Morb Mortal Wkly Rep. 2005;54:36–39. [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Carbon monoxide–related deaths—United States, 1999–2004. MMWR Morb Mortal Wkly Rep. 2007;56:1309–1312. [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Nonfatal, unintentional, non–fire-related carbon monoxide exposures—United States, 2004–2006. MMWR Morb Mortal Wkly Rep. 2008;57:896–899. [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Carbon monoxide exposures—United States, 2000–2009. MMWR Morb Mortal Wkly Rep. 2011;60:1014–1017. [PubMed] [Google Scholar]
- 5.Connecticut October 2011 Snowstorm Power Restoration Report. [Accessed January 30, 2014];Prepared by: Witt Associates. 2011 Dec 1; Available at: http://nuwnotes1.nu.com/apps/financial/nuinvest.nsf/0/5091F-0B5C3FFDAB58525795A00585F4F/$FILE/Witt%20report%20-on%20CL%26P%20power%20restoration.pdf.
- 6.Gulati RK, Kwan-Gett T, Hampson NB, et al. Carbon monoxide epidemic among immigrant populations: King County, Washington, 2006. Am J Public Health. 2009;99:1687–1692. doi: 10.2105/AJPH.2008.143222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hampson NB, Stock AL. Storm-related carbon monoxide poisoning: lessons learned from recent epidemics. Undersea Hyperb Med. 2006;33:257–263. [PubMed] [Google Scholar]
- 8.Lutterloh EC, Iqbal S, Clower JH, et al. Carbon monoxide poisoning after an ice storm in Kentucky, 2009. Public Health Rep. 2011;126(Suppl 1):108–115. doi: 10.1177/00333549111260S114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.US Department of Energy, Office of Electricity Delivery & Energy Reliability. [Accessed January 30, 2014];Hurricane Sandy “Situation Report # 5—1500 hours 10/30/12”. Available at: http://www.oe.netl.doe.gov/namedevent.aspx?ID=67.
- 10.Centers for Disease Control and Prevention. Use of carbon monoxide alarms to prevent poisonings during a power outage—North Carolina, December 2002. MMWR Morb Mortal Wkly Rep. 2004;53:189–192. [PubMed] [Google Scholar]
- 11.Daley WR, Smith A, Paz-Argandona E, Malilay J, McGeehin M. An outbreak of carbon monoxide poisoning after a major ice storm in Maine. J Emerg Med. 2000;18:87–93. doi: 10.1016/s0736-4679(99)00184-5. [DOI] [PubMed] [Google Scholar]
- 12.Houck PM, Hampson NB. Epidemic carbon monoxide poisoning following a winter storm. J Emerg Med. 1997;15:469–473. doi: 10.1016/s0736-4679(97)00079-6. [DOI] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention. Carbon monoxide poisoning from hurricane-associated use of portable generators—Florida, 2004. MMWR Morb Mortal Wkly Rep. 2005;54:697–700. [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention. Carbon monoxide poisoning after Hurricane Katrina—Alabama, Louisiana, and Mississippi, August–September 2005. MMWR Morb Mortal Wkly Rep. 2005;54:996–998. [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention. Carbon monoxide exposures after hurricane Ike—Texas, September 2008. MMWR Morb Mortal Wkly Rep. 2009;58:845–849. [PubMed] [Google Scholar]
- 16.Van Sickle D, Chertow DS, Schulte JM, et al. Carbon monoxide poisoning in Florida during the 2004 hurricane season. Am J Prev Med. 2007;32:340–346. doi: 10.1016/j.amepre.2006.12.013. [DOI] [PubMed] [Google Scholar]
- 17.Daley WR, Shireley L, Gilmore R. A flood-related outbreak of carbon monoxide poisoning—Grand Forks, North Dakota. J Emerg Med. 2001;21:249–253. doi: 10.1016/s0736-4679(01)00380-8. [DOI] [PubMed] [Google Scholar]
- 18.Iqbal S, Clower JH, Hernandez SA, Damon SA, Yip FY. A review of disaster-related carbon monoxide poisoning: surveillance, epidemiology, and opportunities for prevention. Am J Public Health. 2012;102:1957–1963. doi: 10.2105/AJPH.2012.300674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention (CDC) Carbon monoxide poisoning fact sheets. Atlanta, GA: US Department of Health and Human Services, CDC; 2012. [Accessed November 20, 2013]. Available at: http://www.cdc.gov/co/factsheets.htm. [Google Scholar]
- 20.Centers for Disease Control and Prevention (CDC) Carbon monoxide poisoning frequently asked questions. Atlanta, GA: US Department of Health and Human Services, CDC; 2012. [Accessed November 20, 2013]. Available at: http://www.cdc.gov/co/faqs.htm. [Google Scholar]
- 21.US Census Bureau. State and county quickfacts. Washington, DC: US Department of Commerce; 2013. [Accessed November 20, 2013]. Available at: http://quickfacts.census.gov/qfd/states/09000.html. [Google Scholar]
- 22.Consumer Product Safety Commission (CSPC) CPSC votes to revise the carbon monoxide warning label on charcoal packaging. Bethesda, MD: CSPC; 1996. [Accessed November 20, 2013]. Available at: http://www.cpsc.gov/CPS-CPUB/PREREL/PRHTML96/96106.html. [Google Scholar]
- 23.Connecticut Department of Public Health (CDPH) [Accessed November 20, 2013];Hurricane Sandy: important health information. Available at: http://www.ct.gov/dph/cwp/view.asp?a=3115&q=513014. Published 2012.
- 24.Connecticut Department of Public Health (CDPH) [Accessed Published 1998];Reportable diseases and laboratory findings. 2013 Nov 20; Available at: http://www.ct.gov/dph/lib/dph/infectiousdiseases/ctepinews/vol18no1.pdf.
- 25.Radford EP, Drizd TA. Blood carbon monoxide levels in persons 3–74 years of age: United States, 1976–80. Adv Data. 1982;(76):1–24. [PubMed] [Google Scholar]
- 26.Emmerich SJ, Persily AK, Liangzhu W. Modeling and Measuring the Effects of Portable Gasoline Powered Generator Exhaust on Indoor Carbon Monoxide Level. Washington, DC: National Institute of Standards and Technology; 2013. NIST Publication No. TN-1781. [Google Scholar]