Abstract
We report three asteroid hyalosis cases in which internal higher-order aberrations (HOAs) were improved concomitant with improved visual symptoms after vitrectomy. Cases 1 and 2 reported severe floaters and glare disability, although their visual acuities were fairly good. Case 3 showed poor visual acuity since this patient also suffered from mild macular degeneration. For these three asteroid hyalosis cases, we were unsure if treatment with vitrectomy could improve visual symptoms. Therefore, we measured internal HOAs with an aberrometer, and found that the internal HOA values in these cases were high. We suspected that internal high HOAs values were associated with visual disturbance, and performed vitrectomy. After the vitrectomy, the internal HOA values in these three asteroid hyalosis cases markedly decreased, and visual symptoms improved. These observations suggested that measurement of internal HOAs may be useful to determine the indication for vitrectomy.
Background
Asteroid hyalosis is a specific degenerative vitreous disease; it is quite common and has an incidence of about 1% in people aged over 40 years.1–4 Although this disease is commonly known as having minimal subjective symptoms,5–7 some patients report floaters, glare and blurred vision even when visual acuity is good. Vitrectomy has been reported to be an effective treatment for the subjective symptoms of asteroid hyalosis.7–10 Since there are few objective examinations to assess the visual symptoms in patients with asteroid hyalosis, it is difficult to determine the indication for vitrectomy. Ocular higher-order aberrations (HOAs) have been reported to increase with various diseases and to be associated with visual functions.11–18 The current report suggested the clinical importance of measuring internal HOAs in patients with asteroid hyalosis.
Case presentation
Case 1
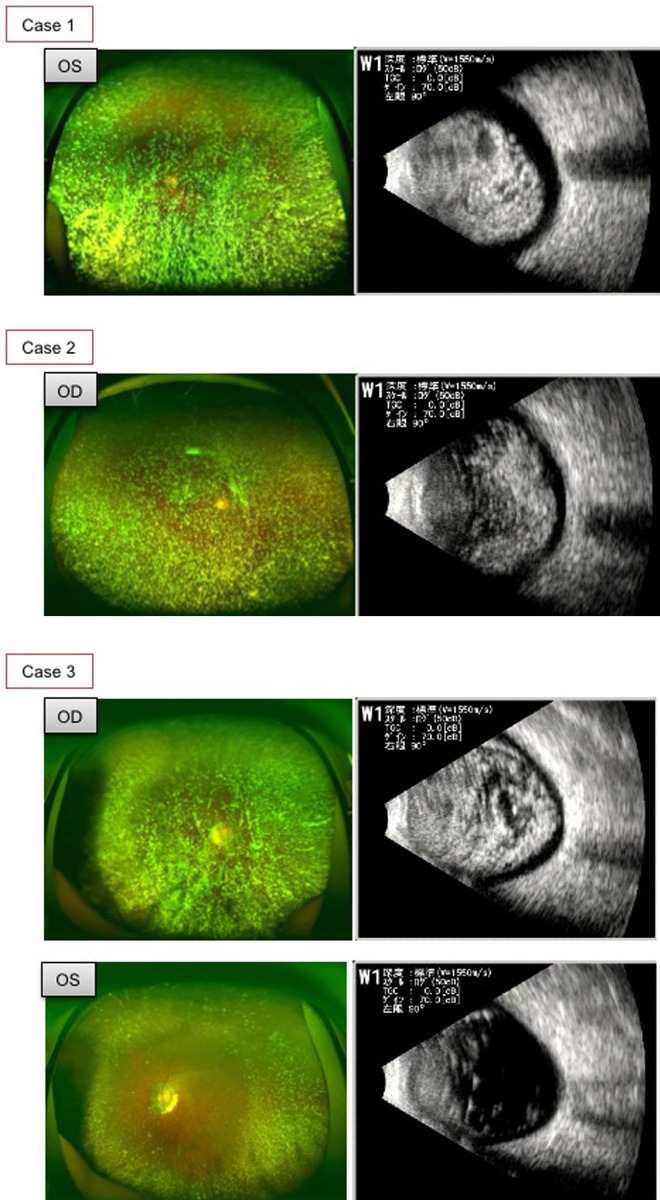
A 68-year-old man reported severe glare in his entire visual field and floaters in his left eye despite having good visual acuity. He was referred to our hospital by his primary care physician to determine the cause of his symptoms and whether he was a candidate for surgery. The patient had experienced floater symptoms during the previous 5 years that had gradually worsened, and he developed severe glare symptoms 2–3 weeks prior to being examined at our hospital. At his first visit, the best-corrected visual acuity (BCVA) was 20/16 in the left eye. The left eye showed a mild cataract with Emery-Little grade I. Since the vitreous in his left eye had dense opacity due to asteroid hyalosis, we could barely observe the fundus (figure 1, case 1). Optical coherence tomography (OCT) showed normal retinal architecture, while an ultrasound B scan showed a high acoustic echo in almost the entire vitreous cavity (figure 1, case 1).
Figure 1.
Preoperative fundus photographs obtained by Optos200 Tx (Optos left images) and ultrasound B scan images (right images) in three cases. Owing to the dense opacity of the vitreous associated with the asteroid hyalosis, details of the fundus were unclear in the left eye in case 1, the right eye in case 2 and the right eye in case 3. Ultrasound B scan showed high acoustic echo in almost the entire vitreous cavity in these three eyes. In the left eye of case 3, which had mild opacity of the vitreous due to asteroid hyalosis, the ultrasound B scan showed a mild acoustic echo in the vitreous.
Case 2
A 69-year-old man reported glare and severe floaters in his right eye despite good visual acuity. He was referred to our hospital by his primary care physician to examine the cause of his symptoms and to determine whether he was a candidate for surgery. He had developed floater symptoms 5 years previously, and they had gradually worsened over the past 2–3 years. The glare symptoms emerged recently prior to his first visit to our hospital. At his first examination, his BCVA was 20/16 in the right eye. The right eye showed a mild cataract with Emery-Little grade II, and the vitreous exhibited dense opacity due to asteroid hyalosis (figure 1, case 2). Although we could not clearly observe the fundus, OCT confirmed that there was normal architecture of the retina. An ultrasound B scan revealed that there was a high acoustic echo in almost the entire vitreous cavity, and a posterior vitreous detachment was observed (figure 1, case 2).
Case 3
A 71-year-old man reported glare and severe floaters. He described his vision as if a spider web was stretched in his right eye. He was referred to our hospital by his primary care physician to determine if he was a candidate for surgery. The floater symptoms had started 2 years previously, with a gradual worsening over the past year. When he visited our outpatient clinic, his BCVA was 20/33 in the right eye and 20/25 in the left eye. The intraocular lenses were properly implanted bilaterally. Both eyes in this patient had vitreous opacity due to asteroid hyalosis (figure 1, case 3). Severe vitreous opacity made it barely possible to observe the fundus of the right eye. Although his left eye had mild opacity, we were able to observe the fundus. OCT revealed a mild degree of macular degeneration in both fundi. The ultrasound B scan showed a high acoustic echo in almost the entire vitreous cavity in the right eye, while there was a mild acoustic echo of the vitreous in the left eye. The scan revealed a posterior vitreous detachment in his right eye (figure 1, case 3).
Investigations
Ocular aberrations are generally divided into corneal and internal aberrations, and advancements in the ocular aberrometer have enabled these two components to be calculated separately. Ocular HOAs, especially internal spherical aberration, increase with ageing. Previous reports showed that ageing changes of ocular HOAs were due to the changes of crystalline lens with ageing.19 20 Also, corneal ocular HOAs have been reported to increase in eye diseases such as dry eye and keratoconus.11–15 On the other hand, internal HOAs have been reported to increase in eyes with a cataract.16–18 These previous reports showed that ocular HOAs were associated with decreased visual functions.
Patients 1 and 2 reported severe floaters and glare disability, although their visual acuity was fairly good. On the other hand, patient three had decreased visual acuity since this patient also had mild macular degeneration. For these three asteroid hyalosis cases, we were unsure if treatment with vitrectomy could improve visual symptoms. Therefore, we measured internal HOAs with an aberrometer (OPD-Scan III, Nidek Co, Aichi, Japan) before and after surgical treatment. HOAs were measured with a 4 mm diameter pupil that was dilated using 0.5% tropicamide/0.5% phenylephrine mixed eye drops (Mydrin-P).
These three patients also completed a vision-related questionnaire before and after vitrectomy to assess possible changes in subjective visual symptoms. They rated the difficulty of seeing far objects with full refractive error correction on a scale of 0 (completely invisible) to 10 (clearly visible), and they also rated the severity of floaters as 0 (none), 1 (mild), 2 (moderate), 3 (severe) or 4 (very severe).
Differential diagnosis
Differential diagnoses of vitreous opacities include ocular diseases such as a Weiss ring, intraocular inflammation, intraocular infection, clumps of pigment, blood, amyloidosis, lymphoma, melanoma and asteroid hyalosis.
A Weiss ring is a commonly seen vitreous opacity noted in front of the optic nerve. This opacity is the hallmark of a posterior vitreous detachment.21 Vitritis, or white cells in the vitreous, signals inflammation and possibly infection. Chronic inflammation leads to larger clusters of cells. Clusters of small, white preretinal nodules can be seen in the inferior vitreous cavity in sarcoidosis. A similar type of vitreous opacity is common in pars planitis, in which preretinal ‘snowballs’ form in front of the peripheral retina or pars plana. Early bacterial endophthalmitis is characterised by fine cells in the vitreous. Clumps of pigment in the vitreous provide a clinical suspicion of a retinal tear or detachment. Red blood cells in the vitreous may be due to a retinal tear, trauma, preretinal neovascularisation or subretinal blood that has diffused into the vitreous cavity. Old blood appears white and may be confused with an inflammatory or neoplastic process. In amyloidosis, white amyloid material forms cobweb-like opacities in the vitreous and may, if dense, obscure vision. White tumour cells in the vitreous (identified by vitreous biopsy) may be a presenting sign of ocular-central nervous system lymphoma, and brown tumour cells can be seen in cases of metastatic cutaneous melanoma.22
On the other hand, asteroid hyalosis is a common, benign, degenerative condition in which many characteristic minute yellow-white spheres of calcium soaps are seen in the centre of the vitreous.3 In the three cases that we examined, the vitreous opacities were characteristic of asteroid hyalosis (figure 1, cases 1–3), and there were no clinical findings to suggest other causes of the vitreous opacities.
Treatment
All patients gave written informed consent before vitrectomy after receiving sufficient explanation of the effects and side effects of the vitrectomy. The effects included the improvement of visual symptoms, and the side effects included retinal tears, retinal detachment and endophthalmitis. A pars plana vitrectomy with three ports by 23-gauge or 25-gauge using a Constellation Vision System (Alcon, Inc, NYSE) was performed for all cases. A core vitrectomy was performed with the aid of triamcinolone acetonide (MaQaid; Wakamoto, Tokyo, Japan). There were no intraoperative or postoperative complications in all three cases. The success of the treatment was assessed with internal HOA values and vision-related questionnaire scores. The detailed processes of treatment and assessment are described as follows:
Case 1
The internal HOA value in the patient's left eye was 1.699 µm, which was much higher than that caused by ageing in the normal population, as previously reported.19 20 We suspected that the high internal HOA value and his visual disturbance were due to asteroid hyalosis and performed a 23-gauge vitrectomy.
Case 2
The internal HOA value in the patient's right eye was 1.896 µm, which was high. First, we performed the phacoemulsification and intraocular lens implantation. Three days after cataract surgery, BCVA in the right eye was 20/20, and the internal HOA value decreased to 1.310 µm. Even after cataract surgery, the internal HOA value was still high, and the patient continued to experience glare disability, and no difference was seen in vision as compared to before cataract surgery. We suspected that the visual disturbance in the right eye was due to asteroid hyalosis and performed a 23-gauge vitrectomy.
Case 3
The internal HOA value in the patient's right eye was 0.819 µm, which was much higher than that in the normal population and that in his left eye (0.076 µm). This patient's high internal HOA value and visual disturbance were only the right eye, so we suspected that they were due to asteroid hyalosis and performed a 25-gauge vitrectomy.
Outcome and follow-up
Case 1
Three months after the vitrectomy, BCVA in the patient's left eye was 20/16. Although the BCVA did not change after the vitrectomy, the patient reported the disappearance of glare and floaters. In addition, the internal HOA value in his left eye markedly decreased from 1.699 to 0.125 µm, which was within the normal range. On the other hand, the corneal HOA value did not change very much from 0.107 to 0.129 µm. The vision-related questionnaire score indicated a slight improvement from 6 to 7 points, while the score for the severity of floaters improved from 3 points to 1 point (table 1, case 1).
Table 1.
Changes of visual acuity, internal higher-order aberrations (HOAs) and questionnaire scores before and after vitrectomy
| Time point at examination | BCVA | Internal HOAs (μm) | Questionnaire score |
|
|---|---|---|---|---|
| General vision (pts) | Severity of floaters (pts) | |||
| Case 1 | ||||
| Before vitrectomy | 20/16 | 1.699 | 6 | 3 |
| After virectomy | 20/16 | 0.125 | 7 | 1 |
| Case 2 | ||||
| Before vitrectomy | 20/20 | 1.310 | 5 | 4 |
| After virectomy | 20/13 | 0.238 | 8 | 1 |
| Case 3 | ||||
| Before vitrectomy | 20/33 | 0.819 | 3 | 4 |
| After virectomy | 20/33 | 0.188 | 6 | 0 |
Although best-corrected visual acuity (BCVA) did not change after vitrectomy in cases 1 and 3, an improvement in the internal HOAs concomitant with an improvement in questionnaire scores was observed. In case 2, we observed an improvement in the BCVA and questionnaire scores concomitant with decreased internal HOAs after the vitrectomy.
BCVA; best corrected visual acuity. HOA; higher-order aberration.
Case 2
At 1 month after the vitrectomy, BCVA in the patient's right eye was 20/13, and the internal HOA value in his right eye markedly decreased from 1.310 to 0.238 µm, which was within the normal range. On the other hand, the corneal HOA value did not change very much from 0.320 to 0.318 µm. The patient reported that both the glare and floaters disappeared, with his vision-related questionnaire score improving from 5 to 8 points, while the score for the severity of floaters improved from 4 points to 1 point (table 1, case 2).
Case 3
At 1 month after the vitrectomy, BCVA in the patient's right eye was 20/33. Although his BCVA did not improve after the vitrectomy, he no longer experienced floaters in this eye. The internal HOA value in his right eye markedly decreased from 0.819 to 0.188 µm, which was within the normal range. On the other hand, the corneal HOA value did not change very much from 0.129 to 0.139 µm. His vision-related questionnaire score improved from 3 to 6 points, while the score for the severity of floaters markedly improved from 4 to 0 points (table 1, case 3).
Discussion
Parnes et al9 performed vitrectomies in 10 eyes of 10 patients with asteroid hyalosis. All patients had floaters and decreased visual acuity, and nine eyes showed improved visual acuity after surgery. Feist et al10 performed vitrectomies in seven eyes of six patients with asteroid hyalosis. All patients experienced glare and decreased visual acuity. Visual acuity improved in three eyes after surgery.
As in previous reports,9 10 it is not difficult to determine the indication for vitrectomy in patients with decreased visual acuity due to severe asteroid hyalosis. On the other hand, in cases with fairly good visual acuity, it is challenging to determine the indication for vitrectomy. Additionally, it can be even more difficult when patients have asteroid hyalosis concomitant with other ocular diseases such as age-related macular degeneration, epiretinal membrane and retinitis pigmentosa. The measurements of internal HOAs are relatively easy to perform, and these measurements appeared to be useful in determining the indication for vitrectomy, especially when patients exhibit good visual acuity (as seen in cases 1 and 2) or when they have other diseases of the fundus (as seen in case 3).
In the current report, the internal HOA values in all three cases before vitrectomy were much higher than those caused by ageing in the normal population, as previously reported.19 20 We suspected that high internal HOA values and visual disturbances were due to asteroid hyalosis, and performed the vitrectomy. After the vitrectomy, the internal HOA values in these three cases markedly decreased and visual symptoms improved.
The advancement of minimally invasive vitrectomy using 23-gauge or 25-gauge systems has contributed to a reduction in postoperative intraocular inflammation, ocular discomfort and time to recovery of visual functions.23 24 While the indication for vitrectomy has yet to be established for asteroid hyalosis, current trends for minimally invasive vitrectomy suggest that there will be an expansion of the indication for use in these cases in the near future. Although there were no intraoperative or postoperative complications observed in any of the current cases, longer follow-ups should be performed so that the risks and benefits of vitrectomy in asteroid hyalosis cases can be definitively evaluated.
On the other hand, recent reports by Manuel J et al showed that a Neodymium Yttrium Aluminium Garnet laser was effective for the treatment of vitreous opacities caused by asteroid hyalosis.25 This technique can be used as a possible treatment modality for vitreous opacity caused by asteroid hyalosis.
There were several limitations associated with our current report. Since we only evaluated a small number of patients, a larger number of cases that include control subjects are needed to conclusively prove that measurements of internal HOAs can be used to determine the indication for vitrectomy in patients with asteroid hyalosis. Furthermore, we only evaluated the total internal HOAs in our current study. Generally, HOAs consist of several components, such as spherical and coma aberrations. Thus, investigations that clarify which components of the internal HOAs affect visual problems or visual functions in patients with asteroid hyalosis are also needed.
Although the three cases described in the current report showed an improvement in the HOA values, we could not confirm the improvement in visual acuity. Since HOAs generally affect visual functions, including visual acuity or contrast sensitivity, further studies using contrast sensitivity should be performed to reveal the change in visual function after vitrectomy in eyes with asteroid hyalosis.
In conclusion, we measured internal HOAs in three patients with severe visual disturbances due to asteroid hyalosis. All cases exhibited very high total internal HOA values as compared with the average values for normal populations. In all three cases, there was a decrease in the total internal HOAs and an improvement in the visual symptoms after vitrectomy. Measurement of the internal HOAs is a promising parameter for determining the indication for vitrectomy in cases with asteroid hyalosis.
Learning points.
Patients with asteroid hyalosis sometimes experience visual disturbances such as glare and blurred vision, although the visual acuity is fairly good.
Since it is challenging to evaluate the visual symptoms and determine the indication for vitrectomy in patients with asteroid hyalosis, an alternative examination to assess the visual symptoms is needed.
The vision-related questionnaire was useful to quantify the visual disturbances before and after vitrectomy in cases with asteroid hyalosis.
Measurement of the internal higher-order aberrations is an important parameter for determining the indication for vitrectomy in patients with asteroid hyalosis.
Footnotes
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Kim JH, Roh MI, Byeon SH et al. . Prevalence of and risk factors for asteroid hyalosis in Seoul, Korea. Retina 2008;28:1515–21. 10.1097/IAE.0b013e318185ea3c [DOI] [PubMed] [Google Scholar]
- 2.Moss SE, Klein R, Klein BE. Asteroid hyalosis in a population: the Beaver Dam eye study. Am J Ophthalmol 2001;132:70–5. 10.1016/S0002-9394(01)00936-9 [DOI] [PubMed] [Google Scholar]
- 3.Bergren RL, Brown GC, Duker JS. Prevalence and association of asteroid hyalosis with systemic diseases. Am J Ophthalmol 1991;111:289–93. 10.1016/S0002-9394(14)72311-6 [DOI] [PubMed] [Google Scholar]
- 4.Mitchell P, Wang MY, Wang JJ. Asteroid hyalosis in an older population: the Blue Mountains Eye Study. Ophthalmic Epidemiol 2003;10:331–5. 10.1076/opep.10.5.331.17324 [DOI] [PubMed] [Google Scholar]
- 5.Noda S, Hayasaka S, Setogawa T. Patients with asteroid hyalosis and visible floaters. Jpn J Ophthalmol 1993;37:452–5. [PubMed] [Google Scholar]
- 6.Potter JW, Jones WL, Crutchfield M. Vision symptoms with asteroid bodies in the vitreous. J Am Optom Assoc 1984;55:419–22. [PubMed] [Google Scholar]
- 7.Renaldo DP. Pars plana vitrectomy for asteroid hyalosis. Retina 1981;1:252–4. 10.1097/00006982-198101030-00023 [DOI] [PubMed] [Google Scholar]
- 8.Miller H, Miller B, Rabinowitz H et al. . Asteroid bodies—an ultrastructural study. Invest Ophthalmol Vis Sci 1983;24:133–6. [PubMed] [Google Scholar]
- 9.Parnes RE, Zakov ZN, Novak MA et al. . Vitrectomy in patients with decreased visual acuity secondary to asteroid hyalosis. Am J Ophthalmol 1998;125:703–4. 10.1016/S0002-9394(98)00031-2 [DOI] [PubMed] [Google Scholar]
- 10.Feist RM, Morris RE, Witherspoon CD et al. . Vitrectomy in asteroid hyalosis. Retina 1990;10:173–7. 10.1097/00006982-199001030-00003 [DOI] [PubMed] [Google Scholar]
- 11.Montes-Mico R, Caliz A, Alio JL. Wavefront analysis of higher order aberrations in dry eye patients. J Refract Surg 2004;20:243–7. [DOI] [PubMed] [Google Scholar]
- 12.Saad A, Gatinel D. Evaluation of total and corneal wavefront high order aberrations for the detection of forme fruste keratoconus. Invest Ophthalmol Vis Sci 2012;53:2978–92. 10.1167/iovs.11-8803 [DOI] [PubMed] [Google Scholar]
- 13.Bühren J, Kook D, Yoon G et al. . Detection of subclinical keratoconus by using corneal anterior and posterior surface aberrations and thickness spatial profiles. Invest Ophthalmol Vis Sci 2010;51:3424–32. 10.1167/iovs.09-4960 [DOI] [PubMed] [Google Scholar]
- 14.Bühren J, Kühne C, Kohnen T. Defining subclinical keratoconus using corneal first-surface higher-order aberrations. Am J Ophthalmol 2007;143:381–9. 10.1016/j.ajo.2006.11.062 [DOI] [PubMed] [Google Scholar]
- 15.Jafri B, Li X, Yang H et al. . Higher order wavefront aberrations and topography in early and suspected keratoconus. J Refract Surg 2007;23:774–81. [DOI] [PubMed] [Google Scholar]
- 16.Lee J, Kim MJ, Tchah H. Higher-order aberrations induced by nuclear cataract. J Cataract Refract Surg 2008;34:2104–9. 10.1016/j.jcrs.2008.08.029 [DOI] [PubMed] [Google Scholar]
- 17.Rocha KM, Nosé W, Bottós K et al. . Higher-order aberrations of age-related cataract. J Cataract Refract Surg 2007;33:1442–6. 10.1016/j.jcrs.2007.03.059 [DOI] [PubMed] [Google Scholar]
- 18.Kuroda T, Fujikado T, Maeda N et al. . Wavefront analysis of higher-order aberrations in patients with cataract. J Cataract Refract Surg 2002;28: 438–44. 10.1016/S0886-3350(01)01176-2 [DOI] [PubMed] [Google Scholar]
- 19.Amano S, Amano Y, Yamagami S et al. . Age-related changes in corneal and ocular higher-order wavefront aberrations. Am J Ophthalmol 2004;137:988–92. 10.1016/j.ajo.2004.01.005 [DOI] [PubMed] [Google Scholar]
- 20.Lyall DA, Srinivasan S, Gray LS. Changes in ocular monochromatic higher-order aberrations in the aging eye. Optom Vis Sci 2013;90:996–1003. 10.1097/OPX.0b013e31829cac79 [DOI] [PubMed] [Google Scholar]
- 21.Akiba J, Ishiko S, Yoshida A. Variations of Weiss's ring. Retina 2001;21: 243–6. 10.1097/00006982-200106000-00008 [DOI] [PubMed] [Google Scholar]
- 22.Gill MK, Jampol LM. Variations in the presentation of primary intraocular lymphoma: case reports and a review. Surv Ophthalmol 2001;45:463–71. 10.1016/S0039-6257(01)00217-X [DOI] [PubMed] [Google Scholar]
- 23.Hikichi T, Matsumoto N, Ohtsuka H et al. . Comparison of one-year outcomes between 23- and 20-gauge vitrectomy for preretinal membrane. Am J Ophthalmol 2009;147:639–43.e1. 10.1016/j.ajo.2008.10.009 [DOI] [PubMed] [Google Scholar]
- 24.Rizzo S, Genovesi-Ebert F, Murri S et al. . 25-gauge, sutureless vitrectomy and standard 20-gauge pars plana vitrectomy in idiopathic epiretinal membrane surgery: a comparative pilot study. Graefes Arch Clin Exp Ophthalmol 2006;244:472–9. 10.1007/s00417-005-0173-6 [DOI] [PubMed] [Google Scholar]
- 25.John M, Ipe A, Jacob I. Manuel's asteroid disruption technique. Indian J Ophthalmol 2015;63:524–7. 10.4103/0301-4738.99867 [DOI] [PMC free article] [PubMed] [Google Scholar]