Abstract
A 50-year-old patient, a smoker, was admitted to the hospital, with a solitary scalp lump. Subcutaneous lumps of the scalp are common but usually benign; however, the painless lump in our patient turned out to be a malignant osteolytic lesion of the skull. Frontal bone was involved, and the disease had spread to the dura. Neuroimaging showed osteolytic lesions involving the axial skeleton, skull and several vertebrae. MRI showed the involvement of the second cervical vertebra, which prompted us to start treatment with dexamethasone. Since the spinal cord was not involved, Oncologists decided not to start radiotherapy treatment until we had reached the final diagnosis. A frontal bone biopsy confirmed the diagnosis of lung carcinoma. Chest X-ray did not identify the pulmonary nodule, but CT scan revealed a 1 cm peripheral, spiculated, pulmonary nodule within a pathological parenchyma (severe diffuse pulmonary emphysema).
Background
Primary lung cancers most commonly metastasise to the brain, bones, liver and adrenal glands. About 30% of lung cancers are squamous-cell carcinoma. They typically occur close to large airways, unlike the case reported here. Although lung cancer may not produce any noticeable symptoms in the early stages, in about 35–40%, the diagnosis may be made in an advanced stage of the disease. Even though the patient had been a smoker for over 30 years, he had no respiratory or systemic symptoms, such as coughing, wheezing, weight loss or fatigue. He only reported sporadic neck pain, but he thought it was muscle strain or tension. Bone pain or headache are frequent when metastasis spreads to the skull, the vertebrae or the brain. However, our patient only noticed a swelling lump on his head but did not ask for medical advice, because it was painless.
This report discusses a 53-year-old patient who presented with an advanced stage of lung cancer, except for the fact that he presented with a lump on the frontal bone of the skull, which turned out to be a metastasis.
Case presentation
A 53-year-old man was admitted to our hospital, presenting with an intermittent cervical ache. He said he had been taking high doses of painkillers. The lump had appeared several weeks before, but he was not concerned enough to ask for medical help.
He denied any further symptoms: he had no coughing, fever, weight loss or fatigue. Physical examination revealed a painless lump on his head (4 cm in diameter). It was firm, not movable, and smooth and hard in consistency. No skin changes were observed. The rest of the clinical examination was normal.
Investigations
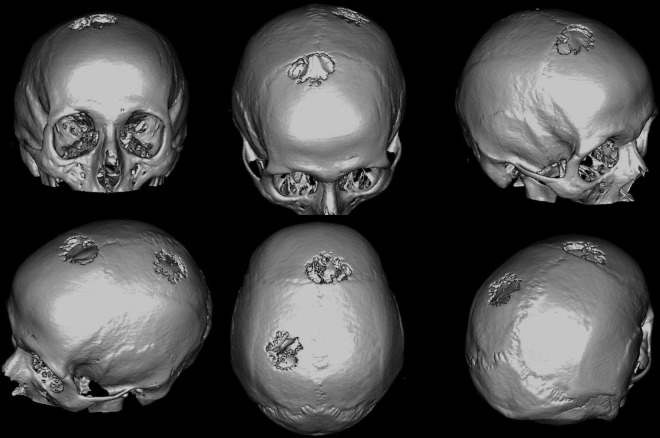
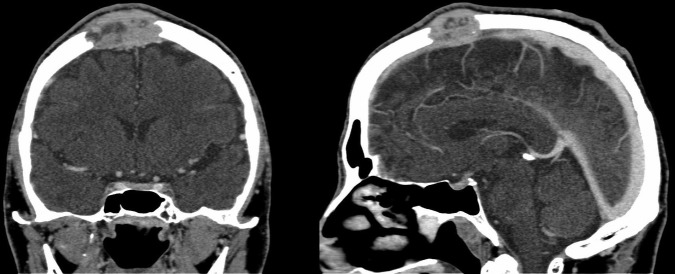
Routine blood test was normal, including measurement of serum calcium, liver enzymes and alkaline phosphatase. Chest X-ray was normal, as well. Since we did not suspect a tumour, neuroimaging was performed to assess the lump and the neck pain. CT scan of the head showed two osteolytic lesions, one on the frontal bone (3.6 cm) and the other on the left parietal bone (4.1 cm) (figure 1). There was extensive bony erosion with dural thickening. However, the brain was not involved (figure 2). MRI also showed a lytic lesion in the second cervical vertebra (axis), hypointense in T1 and T2. The odontoid process was not involved, and cord compression could be ruled out. According to MRI, these three lytic lesions showed features suggesting aggressiveness, and were therefore regarded as metastasis.
Figure 1.
Three-dimensional CT reconstruction depicting two osteolytic lesions: frontal bone and parietal bone.
Figure 2.
Osteolytic skull metastasis with dural involvement.
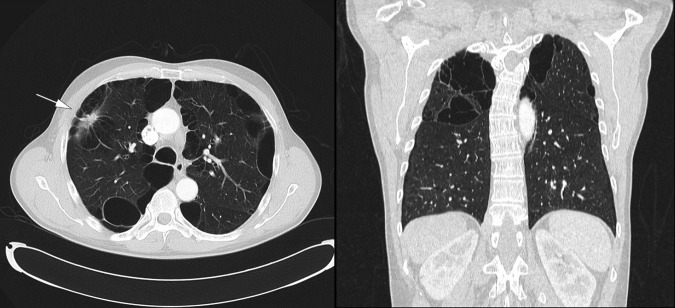
A CT scan of the whole body showed severe diffuse pulmonary emphysema, with massive apical bullae and several smaller bullae seen throughout the right and left lungs. There was a solitary lesion (2 cm in diameter) with spiculated borders and contrast enhancement in the right upper lobe of the lung (figure 3). Besides, several vertebrae were affected (D4, D6, D12 and L2) with lytic lesions suggesting metastasis.
Figure 3.
Spiculated, solitary pulmonary nodule in the right upper lobe. The surrounding parenchyma was pathological: severe diffuse pulmonary emphysema, showing massive apical bullae and several smaller bullae throughout both lungs.
Differential diagnosis
Although tumours of the skull are uncommon (1–4% of all bone tumours), up to 80% can be malignant.1 They present as an enlarging soft or hard mass over the skull, and the differential diagnosis is broad, as it includes benign and malignant lesions: inclusion cyst, fibrous dysplasia, haemangioma, osteomyelitis, plasmacytoma and granuloma. Metastatic lesions include breast, lung, kidney and prostate. Radiological features of the lytic lesions and the finding of a suspicious pulmonary nodule led us to believe the most likely diagnosis was lung cancer.
None of the imaging findings could be considered diagnostic, therefore a biopsy was required to confirm the diagnosis and to rule out other conditions.
CT-guided core needle biopsy of the frontal bone was performed and showed squamous cell carcinoma. Immunohistochemistry staining was negative for thyroid transcription factor-1 and positive for p63, which confirmed the diagnosis.
Treatment, outcome and follow-up
The patient underwent combination chemotherapy treatment with carboplatin-vinorelbine. To assess radiotherapeutic treatment for bone metastases, the patient was referred to radiotherapy Oncologists, where he was given radiotherapeutic treatment. His condition improved as a result of this treatment. However, 3 weeks after the first cycle of chemotherapy, the patient got worse, he was presenting with dyspnoea, persistent vomiting and neck pain. Chest X-ray revealed a large lung tumour mass and a massive pleural effusion. The patient was given palliative treatment and died on day 8 after admission.
Discussion
Bone metastases are frequent during the natural history of some malignant diseases.2 Moreover, lung cancer is the most frequently diagnosed cancer worldwide, and the first cause of cancer deaths.3 Most cases are diagnosed in an advanced stage of the disease (over two-thirds of the patients). Therefore, skeletal metastatic disease is present in up to 36% of patients. The spinal cord is often involved when bone metastases are present, which highlights the advanced stage and implies a high mortality.4 Vertebrae, pelvis, ribs and skull are the most common locations for bone metastasis.5 It is not frequent to find acrometastasis, such as in the hands or feet.6 However, isolated skull metastasis are rarely found in patients with cancer, and they are not often the presenting signs of an unknown primary. However, some examples of temporal7 8 or calvarial9–11 metastases are found in the medical literature, or even metastases to the femora12 or the phalanges,6 13 14 as the inaugural presentation of a lung cancer.
Bone metastases are usually lytic, but symptomatic, with a significant decrease in quality of life.2
When managing bone metastases, the main focus is on reducing the pain, to improve functionality and to avoid complications. Frequent complications are pathological fractures and compression of the spinal cord.15 Management of these metastases can often be complex and demands a multidisciplinary approach: analgaesic, surgical and radiotherapy treatment.11 In many patients, current treatment is palliative and not curative. Some of the indications for radiotherapy are the presence of pain, instability or neurological symptoms due to the compression of the spinal cord. Our patient was given an orthopaedic cervical collar and encouraged to take bisphosphonates. He was referred to a Radiation Oncologist. Notwithstanding, the patient ended up with a bad outcome.
Learning points.
Lung cancer may be very advanced with minimal symptoms when a definitive diagnosis is performed. Isolated skull metastases are a rare condition in these patients and they are an uncommon initial presentation.
The axial skeleton is often involved at diagnosis, in the form of painful bone metastasis.
Pain is frequent when bone metastases are present, and can impair the mobility and hence the patient’s quality of life. Bone fractures and compression of the spinal cord must lead to the initiation of treatment to improve the patient’s quality of life.
Bisphosphonates, calcitonin or radiotherapy, can be useful for the palliation of these lesions. Palliative radiotherapy is one of the most important management tools in these patients.
Acknowledgments
The authors would like to thank Sabrina and Ronan Mulhern for their great contribution in fixing the spelling and grammar issues, and also for their support on the completion of this manuscript.
Footnotes
Twitter: Follow Rafael García Carretero at @rafa_linux
Contributors: RGC drafted the manuscript. JS-R amended some issues. M-JB-A and M-PL-M made useful suggestions for the final paper.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Coleman RE. Clinical features of metastatic bone disease and risk of skeletal morbidity. Clin Cancer Res 2006;12:6243s–9s. 10.1158/1078-0432.CCR-06-0931 [DOI] [PubMed] [Google Scholar]
- 2.Mundy GR. Metastasis to bone: causes, consequences and therapeutic opportunities. Nat Rev Cancer 2002;2:584–93. 10.1038/nrc867 [DOI] [PubMed] [Google Scholar]
- 3.Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin 2013;63:11–30. 10.3322/caac.21166 [DOI] [PubMed] [Google Scholar]
- 4.Tsuya A, Kurata T, Tamura K et al. Skeletal metastases in non-small cell lung cancer: a retrospective study. Lung Cancer 2007;57:229–32. 10.1016/j.lungcan.2007.03.013 [DOI] [PubMed] [Google Scholar]
- 5.Mitsuya K, Nakasu Y, Horiguchi S et al. Metastatic skull tumors: MRI features and a new conventional classification. J Neurooncol 2011;104:239–45. 10.1007/s11060-010-0465-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lamarca A, Hindi N, Belda-Iniesta C et al. Foot pain: uncommon presentation of lung cancer. BMJ Case Rep 2012;2012:bcr1220115360.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cheng C-J, Yao N-S. Isolated temporal bone metastasis in a patient with non-small cell lung cancer. Eur J Radiol Extra 2005;55:75–7. 10.1016/j.ejrex.2005.07.008 [DOI] [Google Scholar]
- 8.Bakhos D, Chenebaux M, Lescanne E et al. Two cases of temporal bone metastases as presenting sign of lung cancer. Eur Ann Otorhinolaryngol Head Neck Dis 2012;129:54–7. 10.1016/j.anorl.2011.07.001 [DOI] [PubMed] [Google Scholar]
- 9.Isaka T, Maruno M, Suzuki T et al. Skull metastases from atypical pulmonary carcinoid tumor in a 19-year-old man. Neurol Med Chir (Tokyo) 2006;46:609–13. 10.2176/nmc.46.609 [DOI] [PubMed] [Google Scholar]
- 10.Jindal T, Sinha RK, Mukherjee S et al. Calvarial and cutaneous metastasis as the primary presentation of a renal cell carcinoma. BMJ Case Rep 2014;2014:bcr2013202830 10.1136/bcr-2013-202830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kotecha R, Angelov L, Barnett GH et al. Calvarial and skull base metastases: expanding the clinical utility of Gamma Knife surgery. J Neurosurg 2014;121:91–101. 10.3171/2014.7.GKS141272 [DOI] [PubMed] [Google Scholar]
- 12.Imanishi J, Yazawa Y, Meguro S et al. A bone metastasis of non-small cell lung carcinoma with prominent clear cell features. BMJ Case Rep 2014;2014:bcr2013203357 10.1136/bcr-2013-203357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Huang FX, Zhang N, Liu L et al. Metastasis of lung adenocarcinoma to the fifth distal phalange of right hand. BMJ Case Rep 2011;2011:bcr0520114276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Myrehaug S, Bezjak A. Rapidly progressive bone destruction of the finger as first presentation of systemic metastases from lung cancer. BMJ Case Rep 2010;2010:bcr05.2009.1912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yu HH, Tsai Y-Y, Hoffe SE. Overview of diagnosis and management of metastatic disease to bone. Cancer Control 2012;19:84–91. [DOI] [PubMed] [Google Scholar]