Abstract
Depressive symptoms may be the only expression of brain tumours. Thus, it is challenging to suspect a brain tumour when patients with depression have a normal neurological examination. We illustrate this by a case report regarding a meningiomatosis revealed by a treatment-resistant depressive syndrome that improved after surgery. This case highlights the importance of identifying signs of brain tumour in patients with depression. Although there is no consensus about whether brain imaging is indicated for depressive syndromes, it should be performed, particularly in late onset of depressive syndrome (after 50 years of age), treatment-resistant depression or in apathy with a reduced emotional response or without dysphoric manifestations.
Background
In addition to neurological symptoms, brain tumours may cause psychiatric syndromes, such as depression, mania, hallucinations, anxiety disorders or anorexia nervosa.1 Sometimes, no neurological signs of brain tumour are found and only psychiatric symptoms manifest.
The detection of brain tumours is essential, because they can lead to functional disaster, and may be life-threatening. Tumour removal can avoid these risks and reduce or alleviate associated psychiatric symptoms. However, brain imaging in psychiatric disorders, particularly in depression, is not systematically carried out and there is no consensus guideline concerning its performance.
Depression is a widespread pathology. In addition, some brain tumours can cause depressive symptoms. The present case report describes a patient in whom depression was the only sign of a brain tumour. The results led to some guidelines that indicate the need for brain imaging in patients who experience depression.
Case presentation
A 54-year-old woman visited the University Department of Psychiatry due to depression, which had continued for 6 months. The main symptoms were apathy, abulia, asthenia and sleep disorders (mainly sleep latency). She had been treated with fluoxetine and bromazepam, but she had stopped taking them after 5 months. She had no history of personal or familial mental illness. She had to cope with several stressful events. There were no suicidal thoughts and no sense of guilt. However, she admitted self-accusation, due to insufficient effectiveness in her job. She also reported irritability, sensitivity and difficulty in making decisions and initiating action. She had not lost weight, and she showed no abnormalities on basic laboratory examinations. A treatment of duloxetine was initiated and escalated up to 60 mg/day; after several weeks, this treatment was found inefficacious, and she was switched to venlafaxine up to 225 mg/day. No improvement was observed in the following weeks. She reported concentration and attention problems. She lost interest in her usual pastimes, but did not feel exceptionally sad. The major symptom was asthenia. She stopped participating in usual tasks and showed a trend towards clinophilia. Suicidal ideations appeared but she talked about them with a kind of detachment. Her husband was worried about her unusual behaviour and mentioned the emergence of memory disorders in his wife.
Investigations
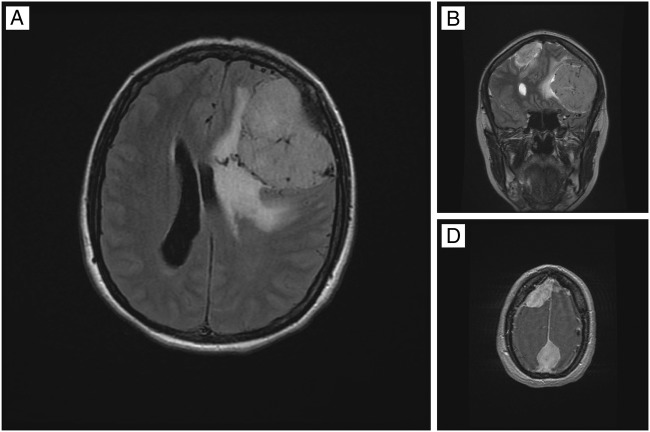
On testing, we found that the Mini-Mental State Examination score was 19/30. Neurological examination was normal, except for a mild frontal syndrome characterised by abulia. The neuropsychological assessment showed verbal and visual episodic memory disorders, language disorders, a dysexecutive syndrome, visuoconstructional deficits, dyspraxia and acalculia. Brain CT scan and MRI revealed meningiomatosis, with a giant meningioma in the left frontal lobe (figure 1).
Figure 1.
MRIs indicating multiple brain meningiomas. (A) Brain MRI, axial plane, T2 fluid-attenuated inversion recovery (FLAIR) sequence: giant meningioma on the left frontal lobe with cerebral oedema and mass effect. (B) Brain MRI, coronal plane, T2 FLAIR sequence: meningioma on the left frontal lobe and a smaller meningioma on the right frontal lobe. (C) Brain MRI, axial plane, T2 FLAIR sequence: meningioma on the right frontal lobe and another meningioma on the parasagittal parietal lobe.
Treatment
The patient underwent emergency surgery of the frontal lesion. A meningothelial meningioma (WHO grade I) was diagnosed.
Outcome and follow-up
One month after surgery, there were no depressive symptoms. The antidepressant treatment was stopped. There were no recurrences of depressive symptoms 24 months after surgery.
Only a few executive functional deficits remained.
Discussion
This case report described a case of a patient with a brain tumour revealed by depressive symptoms.
The location of the tumour pointed to an important role in the development of depression for patients with a brain tumour. Mainio et al2 reported that a tumour located in the frontal cerebral lobe was associated with more severe depressive symptoms than a tumour in the posterior region of the brain. In fact, disruption of the frontolimbic connections appeared to play a more important role than the frontal cortex lesions themselves, in the development of depressive mood states.3
In the present case, the patient was diagnosed with a meningioma, the most common primary benign brain tumour. This type of tumour is likely to be asymptomatic. In some instances, the only clinical expression of the tumour is the presence of psychiatric signs, with no abnormalities in the neurological assessment. A retrospective study by Gupta and Kumar4 showed that, among 72 cases of meningioma, 21% presented with psychiatric symptoms with no neurological signs. The majority of those cases (80%) presented depressive or anxiety symptoms.
In patients with depressive symptoms, a brain tumour cannot be excluded by a normal neurological examination, as suggested several times in the literature.5–8 Therefore, it is crucial to identify other signs that might indicate a brain tumour. A first depressive episode after the age of 50 years and a resistance to antidepressant treatment are the first clues.1 9 10 The presence of apathy must also be carefully identified, because it is not always linked to depression. Apathy was redefined by Levy and Dubois11 as a quantifiable reduction in voluntary, goal-directed behaviours. The mechanisms underlying apathy can be divided into three types of disruptions in processing, including ‘emotional-affective’, ‘cognitive’ and ‘auto-activation’. The emotional-affective type is related to the medial and orbital prefrontal cortex; the cognitive type is related to the lateral prefrontal cortex or the associative part of the basal ganglia; and the auto-activation type is related to the associative and limbic territories of the basal ganglia.
Apathy and depression share some signs in common. For example, loss of interest, which characterises the apathy syndrome, is one of two essential DSM-5 Diagnostic and Statistical Manual of Mental Disorders- fifth edition) criteria for major depressive disorder, namely, depressive feel or loss of interest. Other signs, such as psychomotor slowdown and asthenia, are present in both, apathy and depressive syndromes.
In contrast, Dujardin12 defined some specific depressive symptoms that do not pertain to apathy. These symptoms are dysphoria, as well as sadness, a sense of guilt, depreciation, pessimism and suicidal thoughts. Conversely, some symptoms are more specific to apathy, such as a lack of motivation, a lack of initiative, reduced emotional responses and indifference.
An apathy syndrome, related to depression, is characterised by disturbed emotional and affective processes. The syndrome is expressed by a strong emotional response to negative stimuli and few experiences of positive emotions (anhedonia).11 An apathy syndrome without depression is characterised by an absence of emotional responses for either positive or negative stimuli. Overall, these patients often exhibit indifferent behaviours that can be associated with anosodiaphoria or anosognosia.13
Detecting a brain tumour in patients with depression is a primary concern. Indeed, removing a brain tumour can mitigate brain damage, but may also decrease or alleviate depressive symptoms.1 Mainio et al2 found a significant reduction in depression in 77 patients within 3 months after the surgical removal of ‘primitive’ brain tumours. For patients with lesions in the frontal lobe, the depression decreased immediately after surgery.
Our results give rise to the question of whether or not depressive syndrome should indicate brain imaging. It seems unrealistic to prescribe brain imaging in every patient with a depressive syndrome. Indeed, depression is a frequent mental disorder, and brain tumours are remarkably rare in patients with depression. In fact, among 200 patients who died in a psychiatric unit, autopsies showed that only 3% had brain tumours.14
Currently, there is no consensus on indications for brain imaging in patients with depressive syndromes. We recommend brain imaging in cases with some abnormalities in a neurological examination, or in the absence of neurological signs, in the following cases: (1) late onset of depressive syndrome (after 50 years of age); (2) treatment-resistant depression; (3) apathy without dysphoric manifestations or with a reduced emotional response. In addition, Madhusoodanan et al15 suggested that neuroimaging must be considered when there is an index of suspicion, such as new-onset psychosis, new-onset mood/memory symptoms, occurrence of new or atypical psychiatric symptoms, new-onset personality changes and anorexia without body dysmorphic symptoms.
In conclusion, we recommend using brain imaging for tracking these clinical particularities in patients with depression. This approach can lead to an early diagnosis of brain tumours and, thus, improve the functional and vital prognosis of these patients.
Learning points.
Psychiatric symptoms such as depression, even without any neurological signs, may be the expression of a brain tumour.
Delay to perform brain imaging impacts on functional outcome and survival of patients with a brain tumour.
Brain imaging should be performed if the patient presents a late onset of depressive syndrome (after 50 years of age), a treatment-resistant depression or an apathy with a blunted emotional response or without dysphoric manifestations.
Acknowledgments
The authors acknowledge Eric MacKenzie for checking the English translation of this article.
Footnotes
Contributors: S Dollfus followed the patient, wrote the case report and supervised the manuscript. Sophie Dautricourt analysed the literature and wrote the manuscript. Vincent Marzloff supervised Sophie Dautricourt.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Bunevicius A, Deltuva VP, Deltuviene D et al. Brain lesions manifesting as psychiatric disorders: eight cases. CNS Spectr 2008;13:950–8. [DOI] [PubMed] [Google Scholar]
- 2.Mainio A, Hakko H, Niemelä A et al. Depression and functional outcome in patients with brain tumors: a population-based 1-year follow-up study. J Neurosurg 2005;103:841–7. 10.3171/jns.2005.103.5.0841 [DOI] [PubMed] [Google Scholar]
- 3.Weitzner MA. Psychosocial and neuropsychiatric aspects of patients with primary brain tumors. Cancer Invest 1999;17:285–91. 10.3109/07357909909040599 [DOI] [PubMed] [Google Scholar]
- 4.Gupta RK, Kumar R. Benign brain tumours and psychiatric morbidity: a 5-years retrospective data analysis. Aust N Z J Psychiatry 2004;38:316–19. 10.1080/j.1440-1614.2004.01357.x [DOI] [PubMed] [Google Scholar]
- 5.Pranckeviciene A, Bunevicius A. Depression screening in patients with brain tumors: a review. CNS Oncol 2015;4:71–8. 10.2217/cns.14.60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Litofsky NS, Resnick AG. The relationships between depression and brain tumors. J Neurooncol 2009;94:153–61. 10.1007/s11060-009-9825-4 [DOI] [PubMed] [Google Scholar]
- 7.Wen PY, Schiff D, Kesari S et al. Medical management of patients with brain tumors. J Neurooncol 2006;80:313–32. 10.1007/s11060-006-9193-2 [DOI] [PubMed] [Google Scholar]
- 8.Madhusoodanan S, Danan D, Brenner R et al. Brain tumor and psychiatric manifestations: a case report and brief review. Ann Clin Psychiatry 2004;16:111–13. 10.1080/10401230490453770 [DOI] [PubMed] [Google Scholar]
- 9.Wellisch DK, Kaleita TA, Freeman D et al. Predicting major depression in brain tumor patients. Psychooncology 2002;11:230–8. 10.1002/pon.562 [DOI] [PubMed] [Google Scholar]
- 10.Uribe VM. Psychiatric symptoms and brain tumor. Am Fam Physician 1986;34:95–8. [PubMed] [Google Scholar]
- 9.Cheema FA, Badr A, Iqbal J. Glioblastoma multiforme presenting as treatment-resistant depression. J Neuropsychiatry Clin Neurosci 2010;22:123.e26 10.1176/jnp.2010.22.1.123.e26 [DOI] [PubMed] [Google Scholar]
- 10.Mumoli N, Pulerà F, Vitale J et al. Frontal lobe syndrome caused by a giant meningioma presenting as depression and bipolar disorder. Singapore Med J 2013;54:e158–9. 10.11622/smedj.2013160 [DOI] [PubMed] [Google Scholar]
- 11.Levy R, Dubois B. Apathy and the functional anatomy of the prefrontal cortex–basal ganglia circuits. Cereb Cortex 2006;16:916–28. 10.1093/cercor/bhj043 [DOI] [PubMed] [Google Scholar]
- 12.Dujardin K. Apathie et pathologies neuro-dégénératives : physiopathologie, évaluation diagnostique et traitement. Rev Neurol (Paris) 2007;163:513–21. 10.1016/S0035-3787(07)90458-0 [DOI] [PubMed] [Google Scholar]
- 13.Cretin B, Echaniz-Laguna A, Meyer C et al. Apathie ou dépression ? Une question de nez ? Illustration par quatre cas de tumeurs frontales paramédianes. Rev Neurol (Paris) 2010;166:704–10. 10.1016/j.neurol.2010.03.014 [DOI] [PubMed] [Google Scholar]
- 14.Cole G. Intracranial space-occupying masses in mental hospital patients: necropsy study. J Neurol Neurosurg Psychiatry 1978;41:730 10.1136/jnnp.41.8.730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Madhusoodanan S, Danan D, Moise D. Psychiatric manifestations of brain tumors: diagnostic implications. Expert Rev Neurother 2007;7:343–9. 10.1586/14737175.7.4.343 [DOI] [PubMed] [Google Scholar]