Abstract
The presence of a curve of Spee (COS) of variable depth is common finding in the occlusal arrangement and is sixth key of occlusion The understanding of COS in the field of orthodontics is very important as orthodontists deal with it in virtually every patient they treat. An excessive COS is a common form of malocclusion that may be addressed in many ways, including posterior extrusion, anterior intrusion, and incisor proclination. The specific approach to leveling of COS should be selected based on each patient's needs. Soft tissue, crown–gingival relations, occlusal plane, and skeletofacial concerns are among the special considerations for treatment planning for leveling of COS.
Keywords: Curve of Spee, extrusion, intrusion, levelling
INTRODUCTION
The curve of Spee (COS) was first described by Spee in 1890, who used skulls with abraded teeth to define a line of occlusion. He defined the line of occlusion as the line on a cylinder tangent to the anterior border of the condyle, the occlusal surface of the second molar, and the incisal edges of the mandibular incisors.[1] Spee located the center of this cylinder in the midorbital plane, so that it had a radius of 6.5–7.0 cm.[1,2]
According to the glossary of prosthodontic terms, 1994 COS, was defined as the anatomical curve established by the occlusal alignment of the teeth, as projected onto the median plane, beginning with the cusp tip of the mandibular canine and following the buccal cusp tips of the premolar and molar teeth, continuing through the anterior border of the mandibular ramus and ending at the anterior aspect of the mandibular condyle. The curvature of the arc would relate, on average, to part of a circle with a 4-inch radius.
However, “clinical” of COS in orthodontics differ substantially from original COS as defined by Spee and the definition of COS given in prosthodontic literature. The presence of a COS of variable depth is common finding in the occlusal arrangement and is the sixth key of occlusion. Clinically in orthodontics today, the COS refers to the occlusal curvature of the mandibular dentition that runs tangent from the buccal cusp tips of the posterior molars to the incisal edges of the anterior incisors when viewed in the sagittal plane.[3]
DEVELOPMENT OF CURVE OF SPEE
Factors affecting the development of curve of Spee.
Dental factors
Overall, the development of the COS is likely due to a combination of factors including dental eruption timing, craniofacial variation, and neuromuscular factors.[3] Perhaps the mandibular molars and incisors are permitted to erupt beyond the original occlusal plane due to the fact that they erupt earlier than their maxillary antagonist and are, therefore, unopposed.[3]
Dentition stage
The occlusal plane is flat in the complete deciduous dentition. During the transition into mixed dentition, increases largely with the eruption of the central incisors and first permanent molars, and finally reaches a maximum with the eruption of the permanent second molars where it remains stable throughout adolescence and into adulthood.[3]
Malocclusion
Curve of Spee is the most severe in Class II division 2 subjects, followed by Class II division 1 subjects, then Class I subjects, with the least amount of depth is detected in Class III subject.[4]
Facial pattern
In humans, an increased COS is often seen in brachycephalic facial patterns and associated with short mandibular bodies.
WHY SHOULD WE FLATTEN THE OCCLUSAL CURVE
Proper biomechanical function
For proper biomechanical function during food processing by increasing the crush/shear ratio between the posterior teeth and the efficiency of occlusal forces during mastication.[5]
Muscular balance
Exaggerated COS may alter the muscle balance, ultimately leading to the improper functional occlusion.
Resist the forces of occlusion
In a mechanical sense, the presence of a COS may make it possible for a dentition to resist the forces of occlusion during mastication.
Key to normal occlusion
A deep COS may make it almost impossible to achieve a Class I canine relationship, it may also result in occlusal interferences that will manifest during mandibular function. According to Andrews the COS in subjects with good occlusion ranges from flat to mild, the best static intercuspation occurs when the occlusal plane is relatively flat.
Normal functional movement of the mandible
A deep COS results in more confined areas for the upper teeth. A flat COS is most receptive to normal occlusion and a reverse COS results in excessive room for the teeth.
MEASUREMENT OF CURVE OF SPEE
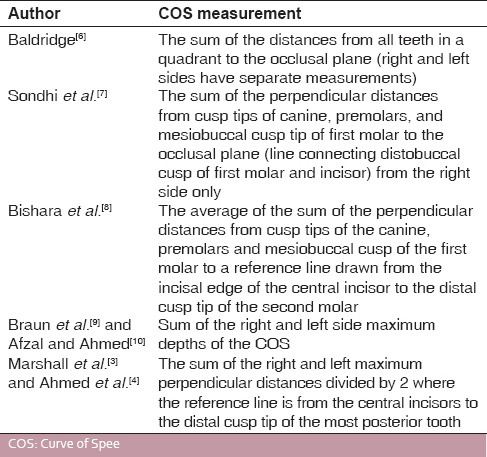
Different authors have advocated their own methods for the measurement of the curve of the Spee [Table 1].
Table 1.
Methods of measurement of COS
HOW MUCH SPACE DOES A CURVE OF SPEE REQUIRE TO BE FLATTENED?
A curved arch has a greater circumference than a flat arch. A popular theory is that 1 mm of arch circumference is needed to level each millimeter of the COS.[11] Baldridge[6] and Garcia[12] found the ratio to be more accurately expressed by the formulas Y = 0.488 X −0.51 and Y = 0.657 X +1.34, respectively, where Y is the arch length differential in millimeters and X is the sum of right and left side maximum depths of the COS in millimeters. In a mathematical model, Germane et al.[13] determined the relationship to be nonlinear, and the arch circumference differential less than a one-to-one ratio for curves of Spee having a depth of 9 mm or less. According to Woods,[14] the amount needed is variable depending on the type of mechanics used. Later on, the COS and/or leveling of this has related to incisor over-bite[9,15,16] and lower arch circumference.[9]
More recently, Ahmed et al.[4] and Afzal and Ahmed[10] used a Boley gauge to measure arch length before and after orthodontic treatment where a reverse curve archwire was used to level the COS. Their results showed that the leveling of each millimeter of the COS increases mandibular arch length by 0.8 mm.
METHODS OF LEVELING
Over the years, different orthodontic techniques have been used to assist in leveling the COS.
Correction of exaggerated COS can be achieved by the following tooth movements:
Extrusion of molars
Intrusion of incisors
Combination of both movements
Proclination.
Extrusion of molars
Can be achieved by the following methods:
Reverse COS and/or maxillary exaggerated COS wires
Step bends
Anterior bite plate
Altering bracket placement heights.
One millimeter of upper or lower molar extrusion effectively reduces the incisor overlap by 1.5–2.5 mm.
Indications
Patients with short lower facial height
Excessive COS
Moderate-to-minimal incisor display.
Disadvantages
Intrusion of incisors
Intrusion of upper and/or lower incisors is a desirable method to level COS in many adolescent and adult patients.[22,23,24]
The four common methods:
All four designs apply tipback bends at the molars to provide an intrusive force at the incisors. Utility arches are arch wires that are bent is such a way that they bypass the buccal segment and are engaged on the incisors. These arches can be used to perform a number of tooth movements including intrusion of incisors, protraction or even retraction of incisors. They are activated by giving a V bend in the buccal segment of the wire so as to produce an intrusive force on the anteriors.
Recommended forces for intrusion of lower incisors are in the range of 12.5 g/tooth and for maxillary incisors about 15–20 g/tooth. The reactionary extrusive force on molars is prevented by natural interdigitating occlusion or in extreme cases by giving a posterior bite plane of minimum thickness.
Indications
Patients with a large vertical dimension
Excessive incision-stomion distance
Large interlabial gap.
Disadvantage
External apical root resorption.[4,28,29,30,31,32,33,34,35,36,37,38]
STABILITY AND RELAPSE
The stability of deep overbite correction may be dependent on the specific nature of its correction (intrusion, extrusion, or flaring). Various other factors, such as growth and neuromuscular adaptation, may also play a role in relapse.
Simons and Joondeph, in a 10-year postretention study of deep overbite correction, reported that proclination of lower incisors and a clockwise rotation of the occlusal plane during treatment were significant relapse factors.[38]
The stability of posterior extrusion is controversial, with conflicting reports of favorable long-term results versus high relapse potential.[39] Variables such as the amount of growth and the patient's age during treatment, muscle strength, adaptation, and the original malocclusion have all beenpostulated as factors contributing to the long-term stability of COS correction.
Burzin and Nanda specifically investigated the stability of incisor intrusion.[40] In this study, the average treatment time was 2.3 years and the average posttreatment observation period was 2 years. Overbite showed a mean reduction of 3.5 mm during treatment and a mean posttreatment relapse of 0.8 mm. The maxillary incisors were intruded an average of 2.3 mm and an insignificant relapse was noted (0.15 mm). This study showed that intrusion of maxillary incisors appears to be a stable procedure.
RETENTION
Corrected COS in either Class I or Class II malocclusions usually require retention in a vertical plane (moderate retention). If anterior teeth were depressed to achieve overbite correction, a bite plate on a maxillary retainer is desirable. It is worn continuously for perhaps the first 4–6 months. Often the incisal edges of the anterior teeth are unworn and require spot grinding and adjusting in some class II division I cases. If cases of skeletal deep bite correction is achieved as a result of bite opening. In these cases the mandible is forced away from the maxilla and the vertical dimensions should be held until growth (i.e., mandibular ramal height) can catch up. The changes of the mandibular plane angle suggest proper retention.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Spee FG. The gliding path of the mandible along the skull. J Am Dent Assoc. 1980;100:670–5. [PubMed] [Google Scholar]
- 2.Hitchcock HP. The curve of Spee in Stone Age man. Am J Orthod. 1983;84:248–53. doi: 10.1016/0002-9416(83)90132-x. [DOI] [PubMed] [Google Scholar]
- 3.Marshall SD, Caspersen M, Hardinger RR, Franciscus RG, Aquilino SA, Southard TE. Development of the curve of Spee. Am J Orthod Dentofacial Orthop. 2008;134:344–52. doi: 10.1016/j.ajodo.2006.10.037. [DOI] [PubMed] [Google Scholar]
- 4.Ahmed I, Nazir R, Gul-e-Erum, Ahsan T. Influence of malocclusion on the depth of curve of Spee. J Pak Med Assoc. 2011;61:1056–9. [PubMed] [Google Scholar]
- 5.Osborn JW. Relationship between the mandibular condyle and the occlusal plane during hominid evolution: Some of its effects on jaw mechanics. Am J Phys Anthropol. 1987;73:193–207. doi: 10.1002/ajpa.1330730206. [DOI] [PubMed] [Google Scholar]
- 6.Baldridge DW. Leveling the curve of Spee: its effect on mandibular arch length. JPO J Pract Orthod. 1969;3:26–41. [PubMed] [Google Scholar]
- 7.Sondhi A, Cleall JF, BeGole EA. Dimensional changes in the dental arches of orthodontically treated cases. Am J Orthod. 1980;77:60–74. doi: 10.1016/0002-9416(80)90224-9. [DOI] [PubMed] [Google Scholar]
- 8.Bishara SE, Jakobsen JR, Treder JE, Stasi MJ. Changes in the maxillary and mandibular tooth size-arch length relationship from early adolescence to early adulthood. A longitudinal study. Am J Orthod Dentofacial Orthop. 1989;95:46–59. doi: 10.1016/0889-5406(89)90135-2. [DOI] [PubMed] [Google Scholar]
- 9.Braun S, Hnat WP, Johnson BE. The curve of Spee revisited. Am J Orthod Dentofacial Orthop. 1996;110:206–10. doi: 10.1016/s0889-5406(96)70110-5. [DOI] [PubMed] [Google Scholar]
- 10.Afzal A, Ahmed I. Leveling curve of Spee and its effect on mandibular arch length. J Coll Physicians Surg Pak. 2006;16:709–11. [PubMed] [Google Scholar]
- 11.Proffit WR, Epker BN. Treatment planning for dentofacial deformities. In: Bell WH, Proffit WR, White RP, editors. Surgical Correction of Dentofacial Deformities. Philadelphia: WB Saunders; 1980. p. 167. [Google Scholar]
- 12.Garcia R. Leveling the curve of Spee: A new prediction formula. J Tweed Found. 1985;13:65–72. [PubMed] [Google Scholar]
- 13.Germane N, Staggers JA, Rubenstein L, Revere JT. Arch length considerations due to the curve of Spee: A mathematical model. Am J Orthod Dentofacial Orthop. 1992;102:251–5. doi: 10.1016/S0889-5406(05)81060-1. [DOI] [PubMed] [Google Scholar]
- 14.Woods M. A reassessment of space requirements for lower arch leveling. J Clin Orthod. 1986;20:770–8. [PubMed] [Google Scholar]
- 15.Orthlieb JD. The curve of Spee: Understanding the sagittal organization of mandibular teeth. Cranio. 1997;15:333–40. doi: 10.1080/08869634.1997.11746028. [DOI] [PubMed] [Google Scholar]
- 16.De Praeter J, Dermaut L, Martens G, Kuijpers-Jagtman AM. Long-term stability of the leveling of the curve of Spee. Am J Orthod Dentofacial Orthop. 2002;121:266–72. doi: 10.1067/mod.2002.121009. [DOI] [PubMed] [Google Scholar]
- 17.Dake ML, Sinclair PM. A comparison of the Ricketts and Tweed-type arch leveling techniques. Am J Orthod Dentofacial Orthop. 1989;95:72–8. doi: 10.1016/0889-5406(89)90138-8. [DOI] [PubMed] [Google Scholar]
- 18.Weiland FJ, Bantleon HP, Droschl H. Evaluation of continuous arch and segmented arch leveling techniques in adult patients – A clinical study. Am J Orthod Dentofacial Orthop. 1996;110:647–52. doi: 10.1016/s0889-5406(96)80042-4. [DOI] [PubMed] [Google Scholar]
- 19.Burstone CJ, Van Steenbergen E, Hanley KJ. Modern Edgewise Mechanics and the Segmented Arch Technique. Farmington, CT: Department of Orthodontics, University of Connecticut, School of Dental Medicine; 1995. [Google Scholar]
- 20.Nanda R. The differential diagnosis and treatment of excessive overbite. Dent Clin North Am. 1981;25:69–84. [PubMed] [Google Scholar]
- 21.Burstone CJ. Deep overbite correction by intrusion. Am J Orthod Dentofacial Orthop. 1977;72:1–22. doi: 10.1016/0002-9416(77)90121-x. [DOI] [PubMed] [Google Scholar]
- 22.Nanda R, Marzban R, Kuhlberg A. The Connecticut intrusion arch. J Clin Orthod. 1998;32:708–15. [PubMed] [Google Scholar]
- 23.Melsen B, Agerbaek N, Eriksen J, Terp S. New attachment through periodontal treatment and orthodontic intrusion. Am J Orthod Dentofacial Orthop. 1988;94:104–16. doi: 10.1016/0889-5406(88)90358-7. [DOI] [PubMed] [Google Scholar]
- 24.Melsen B. Tissue reaction following application of extrusive and intrusive forces to teeth in adult monkeys. Am J Orthod. 1986;89:469–75. doi: 10.1016/0002-9416(86)90002-3. [DOI] [PubMed] [Google Scholar]
- 25.Begg PR, Kesling PC. The differential force method of orthodontic treatment. Am J Orthod. 1977;71:1–39. doi: 10.1016/0002-9416(77)90175-0. [DOI] [PubMed] [Google Scholar]
- 26.Ricketts RM. Bioprogressive therapy as an answer to orthodontic needs. Part I. Am J Orthod. 1976;70:241–68. doi: 10.1016/0002-9416(76)90332-8. [DOI] [PubMed] [Google Scholar]
- 27.Greig DG. Bioprogressive therapy: Overbite reduction with the lower utility arch. Br J Orthod. 1983;10:214–6. doi: 10.1179/bjo.10.4.214. [DOI] [PubMed] [Google Scholar]
- 28.DeShields RW. A study of root resorption in treated Class II, Division I malocclusions. Angle Orthod. 1969;39:231–45. doi: 10.1043/0003-3219(1969)039<0231:ASORRI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 29.Harris E. Root resorption during orthodontic therapy. Semin Orthod. 2000;6:183–94. [Google Scholar]
- 30.Linge BO, Linge L. Apical root resorption in upper anterior teeth. Eur J Orthod. 1983;5:173–83. doi: 10.1093/ejo/5.3.173. [DOI] [PubMed] [Google Scholar]
- 31.Harry MR, Sims MR. Root resorption in bicuspid intrusion. A scanning electron microscope study. Angle Orthod. 1982;52:235–58. doi: 10.1043/0003-3219(1982)052<0235:RRIBI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 32.Ketcham A. A progress report of an investigation of apical root resorption of vital permanent teeth. Int J Orthod Oral Surg Radiogr. 1929;25:310–28. [Google Scholar]
- 33.Baumrind S, Korn EL, Boyd RL. Apical root resorption in orthodontically treated adults. Am J Orthod Dentofacial Orthop. 1996;110:311–20. doi: 10.1016/s0889-5406(96)80016-3. [DOI] [PubMed] [Google Scholar]
- 34.Kaley J, Phillips C. Factors related to root resorption in edgewise practice. Angle Orthod. 1991;61:125–32. doi: 10.1043/0003-3219(1991)061<0125:FRTRRI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 35.Goerigk B, Diedrich P, Wehrbein H. Intrusion of the anterior teeth with the segmented-arch technic of Burstone – A clinical study. Fortschr Kieferorthop. 1992;53:16–25. doi: 10.1007/BF02165141. [DOI] [PubMed] [Google Scholar]
- 36.Dermaut LR, De Munck A. Apical root resorption of upper incisors caused by intrusive tooth movement: A radiographic study. Am J Orthod Dentofacial Orthop. 1986;90:321–6. doi: 10.1016/0889-5406(86)90088-0. [DOI] [PubMed] [Google Scholar]
- 37.Costopoulos G, Nanda R. An evaluation of root resorption incident to orthodontic intrusion. Am J Orthod Dentofacial Orthop. 1996;109:543–8. doi: 10.1016/s0889-5406(96)70140-3. [DOI] [PubMed] [Google Scholar]
- 38.Simons ME, Joondeph DR. Change in overbite: A ten-year postretention study. Am J Orthod. 1973;64:349–67. doi: 10.1016/0002-9416(73)90243-1. [DOI] [PubMed] [Google Scholar]
- 39.Berg R. Stability of deep overbite correction. Eur J Orthod. 1983;5:75–83. doi: 10.1093/ejo/5.1.75. [DOI] [PubMed] [Google Scholar]
- 40.Burzin J, Nanda R. The stability of deep overbite correction. In: Nanda R, editor. Retention and Stability. Philadelphia: WB Saunders; 1993. [Google Scholar]


