Abstract
Purpose: Obesity is one of the most serious health problems among American Indian/Alaska Native (AI/AN) children. We investigated Indian Health Service (IHS) primary care providers' implicit and explicit attitudes about weight and race and their association with treatment approaches to overweight in children.
Methods: We conducted an online survey of long-term primary care clinicians in two western regions of the IHS. We used the existing Weight Attitude Implicit Association Test (IAT) and developed a new Native American Attitude IAT to measure implicit attitudes. Explicit attitudes about weight and race were assessed through self-report. We assessed self-rated treatment approaches to childhood overweight. We used linear regression models to evaluate the association of attitudes about weight and race with treatment approaches.
Results: Our sample included 75 clinicians (56% response rate) who, on average, saw 74 patients per week. Fifty-five percent of clinicians reported that 30–60% of their child and adolescent patients were overweight or obese, and 25% of clinicians reported that 60–100% of their patients were overweight or obese. We found strong implicit bias favoring thin people (Cohen's d=1.44) and weak implicit bias favoring whites (Cohen's d=0.35). We found no association between implicit or explicit bias scores and self-reported treatment of childhood overweight. Continuing education on obesity was associated with self-rated success and competence in weight management.
Conclusions: Weight and race bias exists among long-term IHS clinicians, but may not influence treatment approaches for overweight AI/AN children. Further research should assess the effect of clinicians' attitudes on real-world weight management.
Introduction
Prevalence of obesity among all US children ages 2–19 years is estimated at 17%, with greater prevalence among minority children.1 Obesity is one of the most serious health problems among American Indian/Alaska Native (AI/AN) children, with 24% of all AI/AN children obese at age 5.2,3 A recent national study of AI/AN children in the US Mountain West and Southwest found that 48% of children were overweight or obese.4 In one rural school district, prevalence of obesity was 38% overall, with 51% of Hispanic children, 52% of African American children, and 54% of American Indian children classified as obese.5
Obesity is defined as a BMI in the 95th percentile or higher, and a child is considered overweight with a BMI in the 85th percentile or higher.6 Obese children and adolescents are more likely to be obese as adults.2,7 The long-term health implications of childhood obesity include type 2 diabetes, asthma, sleep apnea, musculoskeletal problems, and psychological distress.8–15 Physicians generally agree that treatment of childhood obesity is necessary, but many do not feel competent to do so.16 In one study, only 56% of primary care physicians (PCPs) felt qualified to treat obesity,17 whereas another study reported that 5–33% of physicians felt competent to treat obesity in children and adolescents.16 Moreover, physicians' lack of confidence in their ability to manage obesity and influence patients' weight loss is related to their negative attitudes about obesity.18 Studies of PCPs found that more than 50% viewed obese patients as awkward, unattractive, and noncompliant.18 The proportion of physicians that endorse the stereotype of obese people as lazy increased 145%, from 4% to 9.8% between 1998 and 2005, with younger physicians more likely to endorse this attitude.19
In addition to self-reported negative attitudes about obesity, a few studies show that providers hold strong implicit or unconscious antifat bias.20–22 In contrast to explicit attitudes, of which an individual is consciously aware, implicit attitudes are beliefs that are not readily apparent to the individual; in fact, a person can hold explicit and implicit attitudes that are in conflict with one another.23–27 Implicit bias can exist even among individuals who report egalitarian beliefs.24,28 In socially sensitive areas, implicit attitudes measured using the Implicit Association Test are more likely than explicit attitudes to be associated with behaviors related to prejudice and discrimination.29 One of the few published studies to investigate implicit weight bias among health professionals found that they implicitly associated “fat” with “bad,” “lazy,” “stupid,” and “worthless.”21
No research has examined implicit and explicit attitudes about weight and race among AI/AN people in general, or more specifically, among PCPs who treat AI/AN people in the Indian Health Service (IHS). Nor has any research evaluated whether such biases, if they exist, are associated with weight management approaches, such as counseling, routine monitoring of weight, and specialist referrals, or with the quality of care received by IHS patients. We therefore conducted a pilot study to measure providers' implicit and explicit attitudes about weight and race, as well as the association of these attitudes with providers' self-rated weight management of AI/AN children and adolescents. A secondary aim was to examine whether and how many hours of obesity and diversity education clinicians received. We also wanted to assess the association of obesity and diversity education with clinicians' attitudes, competence, and treatment approaches.
Methods
Population Studied
Demographic characteristics
Working with the chief medical officers in two regions of the IHS in the western United States, we studied all family physicians, pediatricians, internists, nurse practitioners, and physician assistants actively practicing in reservation-based and urban Indian health clinics. We excluded clinicians with a temporary IHS appointment. We invited all 134 eligible IHS PCPs, who see AI/AN patients almost exclusively and whose patients include children and adolescents to participate. We conducted an online survey of these providers from November 1, 2011, to April 3, 2012. We implemented the survey through Project Implicit®, using secure Web servers at Harvard University. We received approval to conduct the study from the National Indian Health Service Institutional Review Board, the University of Washington Institutional Review Board, the appropriate local Tribal review bodies, and regional leaders of the IHS.
Measures
Demographic, clinical, and practice characteristics
We collected clinicians' demographic and professional characteristics, such as age, sex, professional discipline, years in practice, and years in current position. We asked the following question to assess race/ethnicity: “Which of these categories best describes your racial or ethnic background? [Check all that apply] Black or African American, American Indian or Alaska Native, Asian or Native Hawaiian or Pacific Islander, White, Hispanic/ Latino, I don't name one racial background as more prominent than others, and Other.” We assessed self-rated clinical practice in weight management by asking participants whether they are competent in treating overweight, whether they discuss weight during well child visits, and their assessment of their own success in treating obesity.
Implicit Association Test
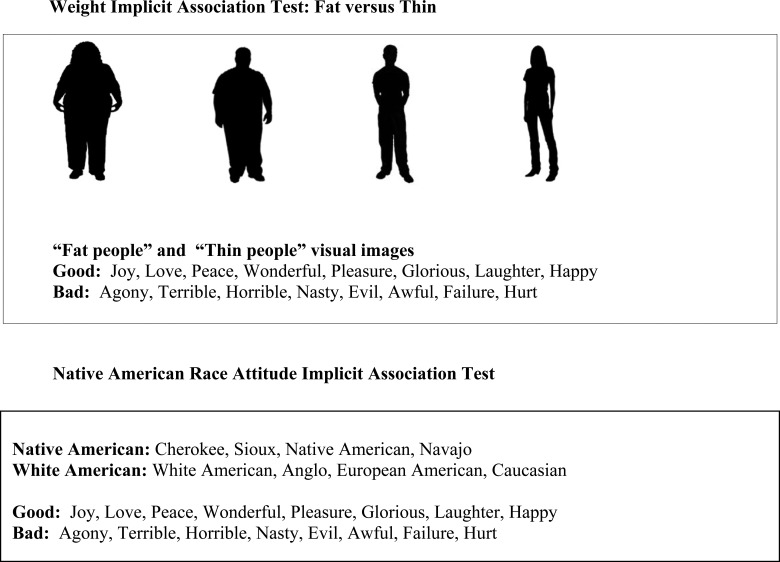
To assess clinicians' implicit attitudes about weight and race, we used one existing Implicit Association Test (IAT; Weight) and one new IAT (Native American) that we created for the present study.27 The IAT is a widely used tool to measure implicit social cognition. It measures the relative strength of the association between two pairs of concepts such as race (Native American vs. White American) and an evaluation (good vs. bad).27 In the IAT, test takers are asked to rapidly sort and pair images and words as they appear on a computer screen. The IAT is based on the theory that concepts that are strongly associated for the test taker will be paired more quickly than concepts with a less-robust association. The IAT achieves good reliability in comparison to other implicit measures.30–32 We used the existing Weight Attitude IAT with silhouette images of “fat people” and “thin people”33 (see Fig. 1). The standard Weight Attitude IAT is an indirect measure of implicit bias toward weight and uses the constructs of “fat people” versus “thin people” and the polarized attitudes of “good” and “bad” to detect implicit weight bias. The Weight IAT has been used with physicians in previous research.22 Using standard IAT design, which includes careful category label selection, and stimuli that clearly represent the category labels,31 we created a new Native American Attitude IAT, which we included in our assessments.
Figure 1.
Implicit Association Tests.
To ensure validity of the new IAT measure, we worked closely with faculty and staff at Project Implicit Inc. to develop the stimuli for the IAT target categories of Native American and White American. We beta tested many stimuli, both visual and text representations of potential stimuli, with Project Implicit staff, IAT researchers, and clinicians nationally. We did preliminary testing of the final version of the IAT with 6 individuals to determine whether the IAT was functioning properly. The Native American/White American IAT consisted of the following: words used to represent Native American: Cherokee, Sioux, Native American, Navajo; words used to represent White American: White American, Anglo, European American, Caucasian; words used to represent “good”: Joy, Love, Peace, Wonderful, Pleasure, Glorious, Laughter, Happy; and words used to represent “bad”: Agony, Terrible, Horrible, Nasty, Evil, Awful, Failure, Hurt.
Explicit questions corresponding to IAT
We asked providers to complete a series of statements (My feelings towards Native Americans are; My feelings towards White Americans are; My feelings towards fat people are; and My feelings towards thin people are) by using a scale ranging from 0 (extremely cold) to 10 (extremely warm), with 5=neither cold nor warm. We created difference scores for each explicit race and weight item by subtracting “feelings towards Native Americans/fat people” from “feelings towards White Americans/thin people.”
Clinicians' treatment approach to overweight
Our dependent variable was a self-rated treatment approach to overweight. To assess clinicians' weight management approaches, we created a 12-item scale, which we titled “Your Treatment Approaches to Overweight.” We chose the items for this measure because all of the items, except for one that asked about assessing quality of sleep, were used previously by Jelalian and colleagues to study attitudes and practices regarding pediatric obesity among family physicians and pediatricians in Southern New England, in the United States.34 We used a 5-point response ranging from 1=not at all likely to 5=extremely likely. The scale was comprised of the following 12 treatment options: counsel patient on how to lose weight; counsel family on how patient can lose weight; discuss health consequences of obesity; set follow-up visits to monitor progress; address weight issue at well visits for all patients; provide written health education materials; refer to a dietician; refer to a behavioral health specialist; prescribe medication; suggest exercise program; assess quality of sleep; and suggest a commercial weight loss program such as Weight Watchers®. Higher scores indicated higher likelihood of following a treatment approach.
Statistical Analysis
We report descriptive statistics using mean and range for continuous variables and percentages for categorical variables. Survey responders and nonresponders were compared using t- and chi-square tests. The IAT effect, known as the IAT D score, was calculated according to the standard IAT scoring algorithm.35 We used one-sample t-tests to determine whether mean implicit and explicit bias scores were significantly different from zero. We also computed standardized effect size (Cohen's d)36 for implicit and explicit attitudes about race and weight. Exploratory factor analysis with varimax rotation was used to determine factor loadings for clinicians' treatment approach to overweight. After the factor analysis, we created two scales for treatment approach by totaling the relevant items for each resulting factor. Higher scores for Factor I (treatment behaviors) represent better quality of clinical treatment approach. Higher scores for Factor II (referral/prescribing patterns) indicate a higher likelihood of referring patients for weight management care. Cronbach's alpha was used to assess construct reliability for each factor.
We used linear regression models to evaluate how attitudes about race and weight were associated with treatment approach to overweight. First, we fit a series of unadjusted models where treatment approach was the outcome and attitude or clinician characteristic was the independent variable. After fitting the unadjusted models, we fit an adjusted model that simultaneously included implicit and explicit attitudes along with clinician characteristics. We report regression (beta) coefficients and 95% confidence intervals (CIs) for all models. The regression coefficients are interpreted as the difference in treatment approach score for a 1-unit change in the independent variable. Attitudes toward race and weight were considered in separate models, except when their product term was included in a model to assess the interaction between race and weight attitudes. All analyses were performed by using Stata software (12.1 for Windows; StataCorp LP, College Station, TX).
Results
Of the 134 primary care clinicians approached, 75 enrolled in the study, for a response rate of 56%. Clinicians who did and did not enroll were similar with respect to IHS area, sex, and professional discipline (p value range=0.10–0.31). For analyses of the association between IATs and clinicians' treatment approaches, we used a complete case approach for each IAT. Fifty-six respondents (42%) were available for the Weight Attitude IAT, 57 (43%) were available for the Native American Attitude IAT, and 54 (40%) responded to both IATs. Clinicians who were and were not included in IAT analyses were similar with respect to IHS area, age, sex, race, and professional title (p value range=0.52–0.89).
Characteristics
Table 1 presents the descriptive characteristics of study participants. Mean age was 48 years; slightly more than half (55%) were female; and 69% reported their race as white. Sixty-seven percent were physicians, with a majority in family medicine; 29% were nurse practitioners; and 4% were physician assistants. Clinicians reported a mean of 14 years in practice and 7 years in their current IHS position. On average, they saw 74 patients per week, with a range of 20–150 patients, and 25% reported that 60–100% of their child and adolescent patients are overweight or obese. Within the past 12 months, 61% reported receiving continuing education on diversity, and 43% reported continuing education on child and adolescent obesity.
Table 1.
Participant Characteristics (N=75)
| Characteristic | |
|---|---|
| Personal characteristics | |
| Age, mean years (range) | 48 (30, 70) |
| Female, % | 55 |
| Race/ethnicity, % | |
| White | 69 |
| American Indian or Alaska Native | 16 |
| Hispanic/Latino | 8 |
| Other | 7 |
| Professional characteristics | |
| Type of provider (N=75), % | |
| Physician | 67 |
| Nurse practitioner | 29 |
| Physician assistant | 4 |
| Years in clinical practice, mean years (range) | 14 (<1, 40) |
| Years in current position, mean years (range) | 7 (<1, 28) |
| Clinical characteristics | |
| Patients seen per week, mean number (range) | 74 (20, 150) |
| Continuing education with content on working with ethnically diverse populations in past 12 months, % | 61 |
| Continuing education with content on child and adolescent obesity in past 12 months, % | 43 |
| Child and adolescent patients, % | |
| Less than 20 | 38 |
| 20–40 | 35 |
| 40–50 | 10 |
| >50 | 17 |
| Child/adolescent patients overweight or obese, % | |
| 0–29 | 20 |
| 30–59 | 55 |
| 60–100 | 25 |
| Self-rated clinical practice behavior | |
| Often or very often give patients a choice in decision when there is a variety of treatment options, % | 88 |
| Often or very often make an effort to give patients control over their treatment, % | 91 |
| Often or very often ask patients to take responsibility for their treatment,a % | 91 |
| Agree that I am able to communicate effectively with my patients, % | 93 |
| Agree that it is easy for me to gain patients' trust, % | 92 |
| Agree that I am able to establish patients as partners in their treatment | 93 |
| Self-rated clinical practice in weight management | |
| Answered moderately, quite, or extremely competent in treating overweight children 2–12 years old, % | 53 |
| Answered moderately, quite, or extremely competent in treating overweight adolescents 12–18 years old, % | 68 |
| Answered sometimes, frequently, or all the time discuss weight with child/adolescent patients and parents during well visit,b % | 89 |
| Answered sometimes, frequently, or all the time have success in treating pediatric patients for obesity,a % | 31 |
n=1 missing value.
n=2 missing values.
Implicit and Explicit Attitudes About Weight and Race
Table 2 shows the mean and effect size for implicit and explicit attitudes for the standard Weight Attitude IAT and our new Native American Attitude IAT. Reliability analysis of the new Native American IAT using split-half analysis demonstrated internal consistency (Chronbach's alpha of 0.70). We found strong implicit pro-thin bias (mean [M]=0.71; Cohen's d=1.44). Scores for weight attitudes ranged from −0.87 to+1.50, with 91% showing some degree of pro-thin bias (e.g., percentage of IAT scores, ≥0.15). We found, on average, weak implicit prowhite bias (M=0.19; Cohen's d=0.35). Scores for race bias ranged from −1.92 to +1.16, with 56% showing some degree of pro-white bias (e.g., percentage of IAT scores, ≥0.15). Self-reported or explicit attitudes about weight showed a weak explicit pro-thin bias (M=0.08; Cohen's d=0.28), and self-reported attitudes about race showed a moderate explicit bias in favor of Native Americans (M=−0.19; Cohen's d=−0.57).
Table 2.
Implicit and Explicit Attitudes: Weight and Native American Implicit Association Tests
| Weight | Native American | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Attitude | N | Mean | (Range) | Effect sizea | P Value | N | Mean | (Range) | Effect sizea | P Value |
| Implicit | 56 | 0.71 | (−0.87, 1.50) | 1.44 | <0.01 | 58 | 0.19 | (−1.93, 1.16) | 0.35 | 0.01 |
| Explicit | 63 | 0.08 | (−0.80, 1.00) | 0.28 | 0.03 | 62 | −0.19 | (−1.00, 0.00) | −0.57 | <0.01 |
Implicit and explicit measures range from –2 to 2, with zero indicating no bias. A positive mean indicates preference for White Americans/“thin” people; a negative mean indicates preference for Native Americans/“fat” people.
Effect size: Cohen's d is a standardized effect size, interpreted as follows: d of 0.2=small effect; d of 0.5=medium effect; and d of 0.80=large effect.
We found no significant association between the Weight Attitude and Native American Attitude IATs (r=0.17; p=0.23), Weight Attitude IAT and explicit weight measures (r=−0.08; p=0.55), or Native American Attitude IAT and explicit race measures (r=−0.01; p=0.92).
Clinician's Treatment Approach to Overweight
Table 3 shows the result of factor analysis for treatment approaches to overweight. We created two scales for clinicians' treatment approaches to overweight. Our two-factor analysis explained a total of 63% of the variance. Factor I, which included five items and explained 43% of the scale variance, represents clinicians' self-reported treatment behaviors for childhood overweight; the Cronbach's alpha coefficient for this factor was 0.85. Factor II, which included three items and explained 20% of the scale variance, represents referral and prescribing patterns; the Cronbach's alpha coefficient for this factor was 0.65. Four items did not load on either factor or form a separate factor and were thus excluded from further analyses
Table 3.
Factor Analysis of Treatment Approaches to Childhood Overweight
| Factor loading | |||
|---|---|---|---|
| Item | I (Treatment) | II (Referral/prescribing) | Item mean |
| Counsel patient on how to lose weight | 0.87 | 3.85 | |
| Counsel family on how patient can lose weight | 0.85 | 3.78 | |
| Discuss health consequences of obesity | 0.79 | 4.08 | |
| Set follow-up visits to monitor progress | 0.74 | 3.41 | |
| Address weight issue at well visits for all patients | 0.62 | 3.62 | |
| Refer to a behavioral health specialist | 0.85 | 2.47 | |
| Refer to a dietician | 0.77 | 3.68 | |
| Prescribe medication | 0.63 | 1.34 | |
| Percent variance explained | 42.82 | 20.48 | |
Factor loadings>0.50 are shown. Item score: 1=“Not at all likely”; 5=“Extremely likely”.
Association of Attitudes About Weight and Race With Treatment Approaches
Table 4 shows the association of attitudes about weight and race with treatment approaches to childhood overweight. The adjusted model showed no relation between implicit weight attitude and treatment behaviors (p=0.88) or referral behaviors (p=0.43). Similarly, we found no significant association between explicit weight attitude and treatment behaviors (p=0.31) or referral behaviors (p=0.42). Table 5 shows the association of attitudes about weight and race with treatment approaches to childhood overweight. The adjusted model showed no relation between implicit race attitude and treatment behaviors for weight management (p=0.21) or referral patterns (p=0.89). Similarly, we found no significant association between explicit race attitude and treatment behaviors (p=0.20) or referral patterns (p=0.20). We found no significant interaction between implicit weight and race attitude for either treatment behaviors (p=0.68) or referral patterns (p=0.54).
Table 4.
Association between Attitudes About Weight and Self-Rated Treatment Approach to Childhood Overweight
| Treatment behaviors | Referral/prescribing patterns | |||||||
|---|---|---|---|---|---|---|---|---|
| Unadjusted | Full model | Unadjusted | Full model | |||||
| Independent variable | β | (95% CI) | β | (95% CI) | β | (95% CI) | β | (95% CI) |
| Implicit weight attitude | −0.25 | (−2.54, 2.04) | 0.19 | (−2.30, 2.68) | 0.56 | (−0.70, 1.81) | 0.55 | (−0.83, 1.93) |
| Explicit weight attitude | −2.07 | (−6.20, 2.06) | −2.24 | (−6.64, 2.16) | −1.14 | (−3.43, 1.14) | −0.98 | (−3.42, 1.46) |
| Age | −0.01 | (−0.12, 0.10) | −0.02 | (−0.15, 0.10) | 0.00 | (−0.06, 0.06) | 0.00 | (−0.07, 0.07) |
| Female | 0.24 | (−2.01, 2.49) | −0.02 | (−2.49, 2.44) | 0.53 | (−0.71, 1.77) | 0.31 | (−1.06, 1.68) |
| White | −0.61 | (−3.01, 1.80) | −0.57 | (−3.06, 1.92) | −0.82 | (−2.13, 0.49) | −0.75 | (−2.13, 0.63) |
| Obesity education | 1.91 | (−0.31, 4.14) | 2.04 | (−0.39, 4.48) | 0.24 | (−1.02, 1.50) | 0.40 | (−0.95, 1.75) |
| >70 patients/week | −0.53 | (−2.77, 1.71) | −0.17 | (−2.57, 2.23) | −0.50 | (−1.73, 0.74) | −0.20 | (−1.53, 1.13) |
Full model includes all variables simultaneously; β reflects the difference in treatment approach score for a 1-unit change in the independent variable.
CI, confidence interval.
Table 5.
Association between Attitudes About Native Americans and Self-Rated Treatment Approach to Childhood Overweight
| Treatment behaviors | Referral/prescribing patterns | |||||||
|---|---|---|---|---|---|---|---|---|
| Unadjusted | Full model | Unadjusted | Full model | |||||
| Independent variable | β | (95% CI) | β | (95% CI) | β | (95% CI) | β | (95% CI) |
| Implicit race attitude | −1.22 | (−3.18, 0.73) | −1.55 | (−4.02, 0.91) | −0.17 | (−1.24, 0.89) | 0.09 | (−1.22, 1.41) |
| Explicit race attitude | −2.48 | (−5.85, 0.88) | −2.45 | (−6.24, 1.33) | 0.90 | (−0.94, 2.73) | 1.30 | (−0.72, 3.33) |
| Age | −0.03 | (−0.14, 0.08) | 0.01 | (−0.11, 0.13) | 0.01 | (−0.05, 0.07) | 0.02 | (−0.05, 0.08) |
| Female | 0.55 | (−1.63, 2.73) | 0.06 | (−2.65, 2.76) | 0.36 | (−0.81, 1.54) | 0.03 | (−1.42, 1.48) |
| White | −0.90 | (−3.31, 1.52) | 0.44 | (−2.59, 3.47) | −0.61 | (−1.91, 0.69) | −0.35 | (−1.98, 1.27) |
| Diversity education | 1.07 | (−1.17, 3.31) | 0.56 | (−2.34, 3.46) | 0.96 | (−0.23, 2.16) | 1.14 | (−0.41, 2.70) |
| >70 patients/week | −0.78 | (−2.95, 1.40) | −0.76 | (−3.04, 1.51) | −0.23 | (−1.41, 0.94) | −0.29 | (−1.51, 0.93) |
Full model includes all variables simultaneously; β reflects the difference in treatment approach score for a 1-unit change in the independent variable.
CI, confidence interval.
Obesity and Diversity Education
Table 6 shows the association between continuing education and clinicians' competence, attitudes, and treatment approaches. Attending continuing education on child obesity was significantly related to greater self-rated success in treating child obesity (r=0.24; p=0.04), greater self-rated competence in treatment of overweight children 2–12 years old (r=0.31; p=0.01), and greater self-rated competence in treatment of overweight children 12–18 years old (r=0.30; p=0.01). We found no significant association between continuing education on child obesity and clinicians' implicit attitudes, explicit attitudes, or treatment approaches. We found a significant positive association between attending continuing education on diversity and referral patterns in treatment approach, specifically, a positive association with referral to behavioral specialist, referral to a dietitian, and prescribing medication (r=0.22; p=0.05).
Table 6.
Influence of Continuing Education on Clinicians' Competence, Attitudes, and Self-Rated Treatment Approaches
| Variable | Diversity education r (p value) | Obesity education r (p value) |
|---|---|---|
| Successful treating pediatric patients for obesity | 0.06 (0.60) | 0.24 (0.04) |
| N=74 | N=74 | |
| Competent treating overweight children ages 2–12 years | 0.08 (0.51) | 0.31 (0.01) |
| N=75 | N=75 | |
| Competent treating overweight adolescents ages 12–18 years | 0.08 (0.50) | 0.30 (0.01) |
| N=75 | N=75 | |
| Implicit weight attitude | 0.04 (0.76) | −0.20 (0.14) |
| N=56 | N=56 | |
| Implicit race attitude | −0.14 (0.28) | −0.23 (0.08) |
| N=58 | N=58 | |
| Explicit race attitude | −0.14 (0.27) | 0.02 (0.89) |
| N=63 | N=63 | |
| Explicit weight attitude | −0.24 (0.06) | −0.01 (0.91) |
| N=62 | N=62 | |
| Treatment behaviors (Factor 1) | 0.17 (0.14) | 0.21 (0.08) |
| N=73 | N=73 | |
| Referral/prescribing behaviors (Factor 2) | 0.22 (0.05) | −0.01 (0.94) |
| N=74 | N=74 |
A positive correlation means that continuing education in the past 12 months is associated with a higher value for “variable”;
r=Pearson's correlation coefficient. Statistically significant results are indicated in bold.
Discussion
Our study makes several unique contributions to understanding provider attitudes about weight, race, and the healthcare of AI/AN children. First, this is the first study ever to measure implicit attitudes about weight and race among long-term primary care clinicians in the IHS. Second, we created a new Native American Attitude IAT using standard IAT method design, which has the potential to benefit future research. Our study expands existing knowledge by examining approaches to pediatric overweight among providers in the IHS. In addition, we assessed the association between self-rated treatment approaches and implicit and explicit attitudes about weight and race. Finally, we explored the association of continuing education with IHS clinicians' self-ratings of competence and treatment behaviors.
We hypothesized that clinicians would hold implicit biases, and that these biases would be related to weight management approaches. Although implicit weight bias was strong among clinicians in the IHS, similar to medical doctors (MDs) in other settings, and the general population,22,37 contrary to our expectation, we found only weak implicit pro-white bias in this group of long-term IHS clinicians. In addition, the strength of implicit weight and race bias was not related either to providers' self-reported treatment approaches or to any provider or practice characteristics. Strength of explicit attitudes was also unrelated to self-rated treatment approaches. One other study that examined implicit attitudes toward African Americans versus White Americans among pediatricians found weak implicit pro-white bias, similar to our study.38 Other studies have shown that strong implicit pro-white versus African American bias exists among MDs,39 and that such bias affects medical care.40,41
We speculate that clinicians whose patient population includes children may be less inclined to develop strongly negative implicit attitudes about race. This may be the result of specific family-centered training or other unknown factors in clinical care of children. Long-term providers in our study saw only AI/AN patients, which may have a positive effect on their implicit attitudes toward race. Clinicians in our study were long-term providers in their current position, on average, for 7 years. These clinicians have chosen to practice in the IHS, often in remote and rural areas, and are members of the communities they serve, all of which may contribute to lack of racial bias. Future research should identify characteristics that create weak implicit bias in a group of providers such as the clinicians in our study. Understanding why and under what circumstances providers hold weak or no implicit biases could contribute to development of evidence-based interventions to reduce implicit bias among clinicians.
Research has shown that implicit bias affects quality of medical care.40–42 Cooper and colleagues found that stronger implicit race bias was associated with less patient centeredness in clinicians' communication with African American patients, compared to white patients.41 Sabin and colleagues found that as pediatricians' implicit race bias increased, prescribing pain medication for a hypothetical African American adolescent patient decreased, but not for a white patient, even among a generally low-biased group of physicians.40 However, for three other pediatric conditions, there was no association between implicit bias and treatment recommendations.40 In the present study, we found strong weight bias, but this bias did not affect self-reported treatment. Future research needs to determine under what circumstances implicit attitudes affect real-world medical care.
Our study has certain limitations. First, ours was a convenience sample of very busy clinicians who practice in remote and rural areas, and selection bias may have influenced our results. For example, the busiest clinicians may not have had time to complete our survey. A related issue is that IHS clinicians care for a patient panel that was virtually 100% AI/AN; such practice characteristics have unknown influences on our findings, Second, we used a Web-based approach to data collection, which may have presented a barrier for some clinicians in extreme remote areas. In recent years, Web-based surveys of physicians have had a lower response rate than paper-and-pencil surveys.43 Our survey included implicit measures that are entirely computer based, so no paper option was available. Another limitation is that clinicians' self-reports of clinical care may not be an accurate reflection of actual real-world care and responses may be biased. However, we purposefully chose measures that have been used by others to approximate clinical care. Most of the self-reported items were previously used in a study by Jelalian and colleagues.34 Future research should examine the association of implicit and explicit bias among providers who treat AI/AN children with actual clinical care delivered to this population. Another limitation of this study is that the content of the continuing education is unknown. Further research should assess the content of diversity and obesity continuing education, so that evidence-based educational programs can be designed.
In this pilot study, our sample size was small, so our results may not be generalizable to all IHS providers, especially given that we included only permanent long-term IHS providers. Further, our results should be considered hypothesis generating owing to the large number of statistical tests performed in our small sample. Future research may be advised to use a system-wide approach that includes all IHS PCPs, identify strategies to improve response rates, and conduct similar studies in settings with AI/AN, White, and patients of other races and ethnicities.
Improving quality of care often involves continuing education for clinicians on a specific topic. Training in diversity was positively associated with referral of AI/AN children to behavior specialists, a dietitian, and prescribing medication, all of which are effective tools in weight management. Similar to Jelalian and colleagues,34 we found that physicians who reported receipt of training in treating child obesity rated themselves as more successful and competent in this clinical area. Similarly, Davis and colleagues44 found that training in obesity increased community pediatricians' confidence in treating obesity and was associated with greater frequency of weight counseling.
Conclusions
In conclusion, strong weight and weak race biases exist among long-term IHS clinicians, but may not influence treatment approaches for overweight AI/AN children. Further research should assess the effect of implicit bias among all IHS clinicians and other clinicians who treat AI/AN children and adolescents on real-world weight management. We also conclude that the positive impact of training in obesity on clinician's self-reported competence and success in treating overweight American Indian children and adolescents is one important factor for healthcare systems to use to help reverse the obesity epidemic.
Acknowledgment
Financial support: Grant P60 MD000507 (PI, Manson) from the National Institute of Minority Health and Health Disparities.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Ogden CL, Carroll MD, Kit BK, et al. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 2014;311:806–814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zephier E, Himes JH, Story M, et al. Increasing prevalence of overweight and obesity in Northern Plains American Indian children. Arch Pediatr Adolesc Med 2006;160:34–39 [DOI] [PubMed] [Google Scholar]
- 3.Schell LM, Gallo MV. Overweight and obesity among North American Indian infants, children, and youth. Am J Hum Biol 2012;24:302–313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ness M, Barradas DT, Irving J, et al. Correlates of overweight and obesity among American Indian/Alaska Native and Non-Hispanic White children and adolescents: National Survey of Children's Health, 2007. Matern Child Health J 2012;16(Suppl 2):268–277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eichner JE, Moore WE, Perveen G, et al. Overweight and obesity in an ethnically diverse rural school district: The Healthy Kids Project. Obesity (Silver Spring) 2008;16:501–504 [DOI] [PubMed] [Google Scholar]
- 6.CDC. Data and statistics childhood obesity. CDC: Washington, DC, 2013. [Google Scholar]
- 7.Gahagan S, Silverstein J; American Academy of Pediatrics Committee on Native American Child Health; American Academy of Pediatrics Section on Endocrinology. prevention and treatment of type 2 diabetes mellitus in children, with special emphasis on American Indian and Alaska Native children. Pediatrics 2003;112:e328–e347 [DOI] [PubMed] [Google Scholar]
- 8.Bethell C, Simpson L, Stumbo S, et al. National, state and local disparities in childhood obesity. Health Aff (Millwood) 2010;29:347–356 [DOI] [PubMed] [Google Scholar]
- 9.Liu L, Lawrence JM, Davis C, et al. Prevalence of overweight among US diabetic youth. Pediatr Diabetes 2010;11:4–11 [DOI] [PubMed] [Google Scholar]
- 10.Story M, et al. Obesity in American-Indian children: Prevalence, consequences, and prevention. Prev Med 2003;37:S3–S12 [DOI] [PubMed] [Google Scholar]
- 11.Dietz WH, Robinson TN. Overweight in children and adolescents. N Engl J Med 2005;352:2100–2109 [DOI] [PubMed] [Google Scholar]
- 12.Barlow SE; Expert Committee. Expert committee recommendations regarding prevention, assessment and treatment of child and adolescent overweight and obesity: Summary report. Pediatrics 2009;120:S169–S192 [DOI] [PubMed] [Google Scholar]
- 13.Gohdes DG, Oser CS, Harwell TS, et al. Diabetes in Montana's Indians: The epidemiology of diabetes in the Indians of the Northern Plains and Canada. Curr Diab Rep 2004;4:224–229 [DOI] [PubMed] [Google Scholar]
- 14.Liu LL, Hironaka K, Pihoker C. Type 2 diabetes in youth. Curr Probl Pediatr Adolesc Health Care 2004;34:254–272 [DOI] [PubMed] [Google Scholar]
- 15.Moore KR, Harwell TS, McDowall JM, et al. Three-year prevalence and incidence of diabetes among American Indian youth in Montana and Wyoming. J Pediatr 2003;143:368–371 [DOI] [PubMed] [Google Scholar]
- 16.van Gerwen M, Franc C, Rosman S, et al. Primary care physicians' knowledge, attitudes, beliefs and practices regarding childhood obesity: A systematic review. Obes Rev 2009;10:227–236 [DOI] [PubMed] [Google Scholar]
- 17.Jay M, Kalet A, Ark T, et al. Physicians' attitudes about obesity and their associations with competency and specialty: A cross-sectional study. BMC Health Serv Res 2009;106:1–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Foster GB, Wadden TA, Makris AP, et al. Primary care physicians' attitudes about obesity and its treatment. Obes Res 2003;11:1168–1177 [DOI] [PubMed] [Google Scholar]
- 19.Warner CH, Warner CM, Morganstein J, et al. Military family physician attitudes toward treating obesity. Mil Med 2008;173:978–984 [DOI] [PubMed] [Google Scholar]
- 20.Teachman BA, Brownell KD. Implicit anti-fat bias among health professionals: Is anyone immune? Int J Obes Relat Metab Disord 2001;25:1525–1531 [DOI] [PubMed] [Google Scholar]
- 21.Schwartz MB, Chambliss HO, Brownell KD, et al. Weight bias among health professionals specializing in obesity. Obes Res 2003;11:1033–1039 [DOI] [PubMed] [Google Scholar]
- 22.Sabin JA, Marini M, Nosek BA. Implicit and explicit anti-fat bias among a large sample of medical doctors by BMI, race/ethnicity and gender. PLoS One 2012;7:e48448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Greenwald A.G. and Banaji M.R., Implicit social cognition: Attitudes, self-esteem, and stereotypes. Psychol Rev 1995. 102(1): p. 4–27 [DOI] [PubMed] [Google Scholar]
- 24.Dovidio JF, Kawakami K, Gaertner SL. Implicit and explicit prejudice and interracial interaction. J Pers Soc Psychol 2002;82:62–68 [DOI] [PubMed] [Google Scholar]
- 25.Devine PG, Monteith MJ. Automaticity and control in stereotyping. In: Chaiken S, Trope Y. (eds), Dual Process Theories in Social Psychology. Guilford: New York, 1999, pps. 339–360. [Google Scholar]
- 26.Hofmann W, Gawronski B, Gschwendner T, et al. A meta-analysis on the correlation between the Implicit Association Test and explicit self-report measures. Pers Soc Psychol Bull 2005;31:1369–1385 [DOI] [PubMed] [Google Scholar]
- 27.Greenwald AG, McGhee DE, Schwartz JL. Measuring individual differences in implicit cognition: The Implicit Association Test. J Pers Soc Psychol 1998;74:1464–1480 [DOI] [PubMed] [Google Scholar]
- 28.Dovidio J, Gaertner SL. Aversive racism and selection decisions: 1989 and 1999. Psychol Sci 2000;11:315–319 [DOI] [PubMed] [Google Scholar]
- 29.Greenwald AG, Poehlman TA, Uhlmann EL, et al. Understanding and using the Implicit Association Test: III. Meta-analysis of predictive validity. J Pers Soc Psychol 2009;97:17–41 [DOI] [PubMed] [Google Scholar]
- 30.Cunningham WA, Preacher KJ, Banaji MH. Implicit attitude measures: Consistency, stability, and convergent validity. Psychol Sci 2001;12:163–170 [DOI] [PubMed] [Google Scholar]
- 31.Nosek BA, Greenwald AG, Banaji MR. The Implicit Association Test at age 7: A methodological and conceptual review. In: Bargh JA. (ed), Automatic Processes in Social Thinking and Behavior. Psychology Press: New York, 2007, pps. 265–292. [Google Scholar]
- 32.Kim DY. Voluntary controllability of the Implicit Association Test (IAT). Soc Psychol Quart 2003;66:83–96 [Google Scholar]
- 33.Project Implicit. Stimuli images for weight IAT. 2011. Available at http://implicit.harvard.edu Last accessed June10, 2014
- 34.Jelalian E, Boergers J, Alday CS, et al. Survey of physician attitudes and practices related to pediatric obesity. Clin Pediatr (Phila) 2003;42:235–245 [DOI] [PubMed] [Google Scholar]
- 35.Greenwald AG, Nosek BA, Banaji MR. Understanding and using the Implicit Association Test I: An improved scoring algorithm. J Pers Soc Psychol 2003;85:197–216 [DOI] [PubMed] [Google Scholar]
- 36.Cohen J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed. Erlbaum: Hillsdale, NJ, 1988. [Google Scholar]
- 37.Nosek BA, Smyth FL, Hansen JJ, et al. Pervasiveness and variability of implicit attitudes and stereotypes. Eur Rev Soc Psychol 2007;18:36–88 [Google Scholar]
- 38.Sabin JA, Rivara FP, Greenwald AG. Physician implicit attitudes and stereotypes about race and quality of medical care. Med Care 2008;46:678–685 [DOI] [PubMed] [Google Scholar]
- 39.Sabin JA, Nosek BA, Greenwald A, et al. Physicians' implicit and explicit attitudes about race by MD race, ethnicity and gender. J Health Care Poor Underserved 2009;20:896–913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sabin JA, Greenwald AG. The influence of implicit bias on treatment recommendations for 4 common pediatric conditions: Pain, urinary tract infection, attention deficit hyperactivity disorder, and asthma. Am J Public Health 2012;102:988–995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cooper LA, Roter DL, Carson KA, et al. The associations of clinicians' implicit attitudes about race with medical visit communication and patient ratings of interpersonal care. Am J Public Health 2012;102:979–987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Green AR, Carney DR, Pallin DJ, et al. Implicit bias among physicians and its prediction of thrombolysis decisions for black and white patients. J Gen Intern Med 2007;22:1231–1238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shih TH, Fan X. Comparing response rates from Web and mail surveys: A meta-analysis. Field Methods 2008;20:249–271 [Google Scholar]
- 44.Davis MM, Gance-Cleveland B, Hassink S, et al. Recommendations for prevention of childhood obesity. Pediatrics 2007;120(Suppl 4):S229–S253 [DOI] [PubMed] [Google Scholar]