Abstract
Background: Studies suggest that outpatient palliative care can reduce hospitalization and increase hospice utilization for patients with cancer, however there are insufficient resources to provide palliative care to all patients from time of diagnosis. It is also unclear whether inpatient consultation alone provides similar benefits. A better understanding of the timing, setting, and impact of palliative care for patients with cancer is needed.
Objectives: The purpose of this study was to measure timing of referral to outpatient palliative care and impact on end-of-life (EOL) care.
Design: The Comprehensive Assessment with Rapid Evaluation and Treatment (CARE Track) program is a phased intervention integrating outpatient palliative care into cancer care. In Year 1 patients were referred at the discretion of their oncologist.
Setting: Academic medical center.
Measurements: We compared EOL hospitalization, hospice utilization, and costs of care for CARE Track patients compared to those never seen by palliative care or seen only in hospital.
Results: Patients were referred a median of 72.5 days prior to death. CARE Track patients had few hospitalizations at end of life, were less likely to die in hospital, had increased hospice utilization, and decreased costs of care; these results were significant even after controlling for differences between groups. Inpatient consultation alone did not impact these variables. However, only approximately half of patients with incurable cancers were referred to this program.
Conclusion: Referral outpatient palliative care within 3 months of death improved EOL care and reduced costs, benefits not seen with inpatient care only. However, many patients were never referred, and methods of systematically identifying appropriate patients are needed.
Introduction
Several recent studies suggest that integration of outpatient palliative care services into the care of patients with advanced cancer can improve care by decreasing troubling symptoms1–6 and reducing the rate of hospitalization, emergency department visits, and chemotherapy at the end of life.7–10 One of these studies, which compared patients with metastatic lung cancer seen concurrently by oncologists and palliative care clinicians from the time of diagnosis to those seen by oncology alone also found improvements in mortality, with concurrent care patients living almost 4 months longer than those without palliative care services.7 For these reasons, a recent position statement by the American Society of Clinical Oncology stated, “By potentially improving quality of life (QOL), cost of care, and even survival in patients with metastatic cancer, palliative care has increasing relevance for the care of patients with cancer.”11
Initiating outpatient palliative care at time of diagnosis for all patients with advanced cancer allows for uniform access to this service early enough to make a difference for these patients. Unfortunately, the standard of monthly visits from the time of diagnosis to death is a model that is not practical in most settings, simply because there are insufficient resources to meet this demand.12,13 In 2010, the American Academy of Hospice and Palliative Medicine Workforce Task Force estimated that there was a 6,000–18,000 person shortage for palliative care clinicians.14 Furthermore, most existing palliative care services are based in hospitals and do not see patients in the outpatient setting, while another segment of palliative care physicians only see patients in hospice settings.15 It is also unclear whether patients with metastatic cancers other than lung cancer require such care from initiation of treatment.7 Many patients, such as those with metastatic prostate, breast, thyroid, and carcinoid cancers, may be stable for a longer period of time before needing involvement of specialist level palliative care.
The purpose of this intervention was to determine whether alternative methods of referral to outpatient palliative care services could provide benefits to patients with cancer similar to that achieved with referral at diagnosis and allow for a more sustainable model of concurrent care. In addition, because most palliative care programs are hospital-based, we were interested in whether inpatient palliative care consultation only provided benefits comparable to palliative care clinics in terms of avoiding excessive and ineffective care at the end of life.
The Comprehensive Assessment with Rapid Evaluation and Treatment (CARE Track) program is a phased palliative care intervention based in an academic cancer center. The CARE Track program provides outpatient consultation including symptom management and end-of-life (EOL) care planning with multidisciplinary care coordination. It provides these during the course of ongoing standard oncology care and is performed in close collaboration with treating oncologists. This article reports on Year 1 of this intervention in which we compare EOL outcomes (including hospitalization at the end of life, hospice utilization, and costs of care) between patients referred to the CARE Track palliative care clinic at the discretion of the oncologist, without specific triggers for referral, to a group of patients with similar diagnoses followed at our cancer center but never seen in our CARE Track palliative care clinic. The group never seen in palliative care is divided into those who never saw palliative care in any setting and those who only saw palliative care in the hospital.
Methods
CARE Track is a multiyear study with a phased palliative care intervention the goal of which was to improve the quality of life for patients with incurable malignancies at the University of Virginia Emily Couric Cancer Center while reducing costs and decreasing hospitalization at end of life. This article reports on the impact of Year 1 of this intervention on EOL care variables including hospitalization at end of life, deaths in hospital, use of hospice services, and cost of care. The Palliative Care Clinic at the University of Virginia was established in 2001, as part of an existing palliative care service, which includes inpatient consultation, a palliative care unit, and home hospice components. All of these settings are staffed by the same physicians and nurse practitioners ensuring continuity of care across settings. The clinic is housed in the Emily Couric Clinical Cancer Center, and prior to this study saw patients 3 days per week. Patients referred to this clinic are followed concurrently with medical oncology, radiation oncology, and surgical oncology for symptom management and EOL care planning. The palliative care clinic staff includes reginstered nurses, physicians, and nurse practitioners. Patients referred to this clinic are typically followed concurrently with their treating cancer physicians, and palliative care providers often serve as the hospice attending once a patient is referred to that service. Social worker and chaplaincy services are available at our cancer center but were not specifically assigned to palliative care.
In Year 1 of this project, no specific triggers for palliative care consultation were initiated; all patients were referred at the discretion of their oncologist. In this phase we reduced external barriers to concurrent care in two ways. We reduced wait times for palliative care clinics by additional staffing that increased the average number of half-day clinic sessions per week from 6 to 14. In addition, we established a weekly interdisciplinary meeting (Supportive Care Tumor Board)16 in order to improve care coordination for CARE Track patients. All disciplines working at the cancer center were invited to present patients with worsening symptoms, difficult social situations, and those facing transitions of care for discussion at this meeting.
Patients were entered into the CARE Track Year 1 program on referral to palliative care clinic if they met entry criteria (stage IV solid tumor or other advanced cancer identified as incurable by the referring oncologist or surgeon). A control group consisting of patients with similar diagnoses followed at the same academic cancer center but not seen in palliative care clinic was identified using the Clinical Data Repository (CDR), a data warehouse managed by the Clinical Informatics Division of the Department of Public Health Sciences that contains information about patients seen at the University of Virginia Health System. This comparison group was divided into two categories: those who died without any contact with palliative care, and those were never referred to the CARE Track outpatient palliative care clinic but were seen by the inpatient palliative care consultation service during a hospitalization. Almost all patients in this latter group were referred during their last hospitalizations prior to death.
Data regarding EOL resource utilization including hospitalization in the last month of life, chemotherapy in the last 2 weeks of life, referral rates to hospice, and hospice length of stay, was obtained from the electronic medical record (EMR), the CDR, and other sources for these three groups (concurrent palliative and oncology, no contact with palliative care, and palliative care only during last hospitalization). Costs of care were obtained from these resources as well and therefore reflect costs at University of Virginia.
This project was approved by the University of Virginia Institutional Review Board and supported by a 2012 Centers for Medicare & Medicaid Services Innovation Award.
Statistical methods
The χ2 test was used to assess the significance of differences in the proportion of categorical values of outcomes, demographics, and cancer diagnoses between patient groups. The significance of differences in mean values of continuous variables was assessed using the Wilcoxon rank sum test. Logistic regression analysis was used to assess the statistical significance of the difference in the odds of death in the hospital, the difference in the odds of hospitalization within 30 days of death, and the difference in the odds of receiving hospice care between patient groups. Odds ratios for each outcome were calculated without adjustment, with bivariable adjustment for each demographic and cancer diagnosis group, and with multivariable adjustment for all demographic and cancer diagnosis groups included simultaneously. Statistical significance was assessed for each odds ratio using the 95% confidence interval.
Results
A total of 207 patients with advanced cancer were referred to palliative care in the first year of this intervention (CARE Track Y1 concurrent care cohort); of these, 178 had died at the time of analysis. Mean time between referral and death was 72.5 days. The control group included 198 deceased patients with similar diagnoses but not referred to CARE Track outpatient palliative care clinic were identified; 126 of these did not see palliative in any setting and 72 were in the inpatient palliative consultation only group.
Demographic data
Demographic characteristics of CARE Track and control patients are summarized in Table 1. Compared to controls, patients in the concurrent care groups were more likely to be female and younger, more likely to have Medicaid, or lack insurance all together. Most common malignancies are noted, and because patients may have had more than one primary malignancy these numbers add up to more than 100%. CARE Track concurrent care patients were more likely to have gynecologic malignancies, breast cancer, and head and neck cancer than controls.
Table 1.
Demographics
| CARE Track patients: 178 | Control patients: 198 | |
|---|---|---|
| Age (years, median)a | 59 | 66 |
| Gender (% female)b | 60.7% | 40.9% |
| Ethnicity(%): white | 76.4% | 80.8% |
| African American | 18.5% | 15.5% |
| Hispanic | 3.4% | 2.0% |
| Other | 4.5% | 4.0% |
| Payer (%):Medicarec | 41.6% | 55.6% |
| Medicaid | 21.4% | 6.6% |
| Self/uninsured | 6.2% | 3.5% |
| Private/commercial | 25.3% | 27.8% |
| Most common diagnosesd | Lung: 28.0% | 35.9% |
| Gyn: 24.2% | 3.0%d | |
| Head and neck: 18.5% | 7.1%d | |
| Colo-rectal: 18.0% | 13.6% | |
| Breast: 12.4% | 3.0%d |
p < 0.0001.
p = 0.0001.
p < 0.001.
p < 0.005.
Hospitalization at end of life
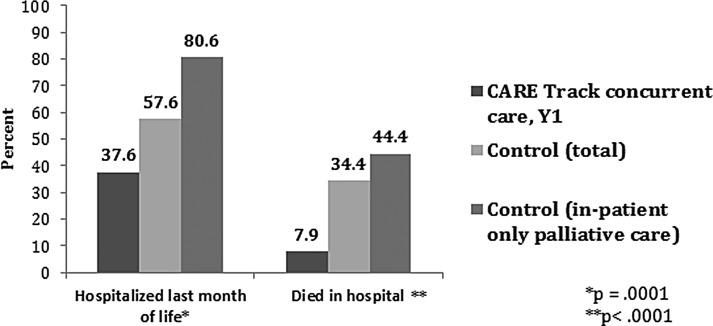
Figure 1 illustrates the comparison between CARE Track intervention patients and the total control group, as well as that portion of controls who were referred to inpatient palliative care only.
FIG. 1.
Hospitalization at end-of-life. Percent of CARE Track patients who were hospitalized in the last month of life and percent who died in the hospital were compared to UVA controls and subset of controls seen by palliative care only on the inpatient service. CARE Track patients were significantly less likely to be admitted to the hospital in the last month and significantly less likely to die in the hospital than either control group. CARE Track, Comprehensive Assessment with Rapid Evaluation and Treatment; UVA, University of Virginia.
Patients seen in the palliative care clinic were less likely to be admitted to the hospital in the last month of life. In the intervention group, 37.6% were hospitalized in the last month of life compared to 57.6% % of all controls, and 80.6% of patients who received palliative care in the hospital only were hospitalized in the last month of life. Patients in the intervention group had significantly lower odds of hospitalization within 30 days of death (odds ratio [OR] = 0.29, 95% confidence interval [CI] 0.16–0.52), compared to patients in the control group, after adjusting for differences in patient demographics and malignancy characteristics. Patients in the intervention group were also much less likely to die in the hospital. Only 7.8% of CARE Track concurrent care patients died in the hospital compared to 34.3% of all controls, and 44.4% among those controls seen by inpatient palliative care only in the hospital. The odds of death in the hospital were significantly lower in the intervention group (OR = 0.16, 95% CI 0.07–0.37) compared to the control group, adjusted for differences in patient demographics and malignancy characteristics.
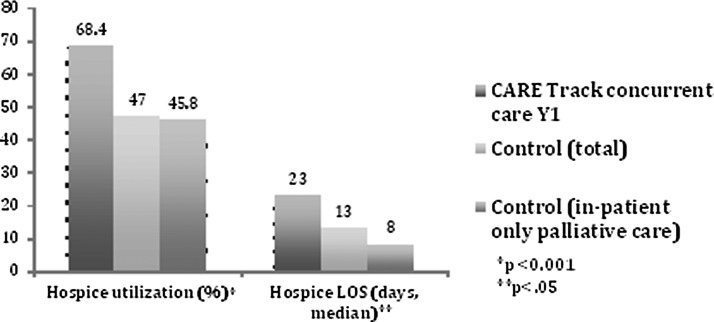
Hospice care
CARE Track patients (cared for by oncology and palliative care concurrently) had higher rate of hospice referral than those who were never seen in palliative care clinic. As shown in Figure 2, 68.4% of concurrent care patients received hospice services at the time of death (median length of stay, 23 days; mean, 37.7 days) compared to 47.0% of all controls, and 45.8% of those controls who were seen by inpatient palliative care only (p < 0.001). Hospice length of stay was also longer for intervention patients with an average LOS of 23 day (median) for intervention 13 days for all controls, and 8 days for controls who were seen by inpatient palliative care (p < 0.05).
FIG. 2.
Hospice utilization and length of stay. Percent of CARE Track patients who were referred to hospice prior to death, and median hospice length of stay (days) were compared to UVA controls and subset of controls seen by palliative care only on the inpatient service. CARE Track patients were significantly more likely to be referred to hospice and had a longer length of stay on hospice care than either control group. CARE Track, Comprehensive Assessment with Rapid Evaluation and Treatment; UVA, University of Virginia.
Results from the multivariable logistic regression analysis demonstrate that patients in the intervention group had more than three times the odds of receiving hospice care (OR = 3.11, 95% CI 1.71–5.66), compared to patients in the control group, after adjusting for differences in patient demographics and malignancy characteristics.
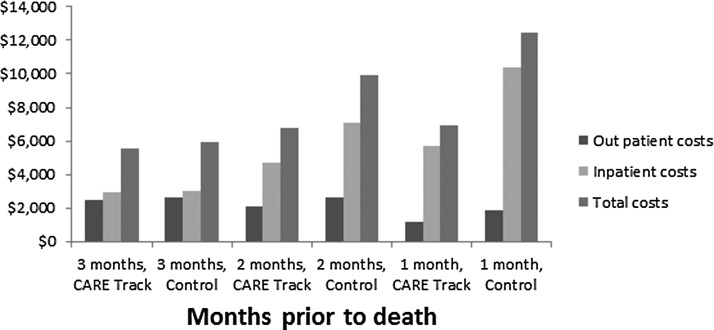
Cost of care
Figure 3 shows costs of care for patients in the CARE Track and control group in the last 3 months of life as well. Costs of care were less for CARE Track patients during the last 3 months of life, with decreased spending on inpatient care making up the bulk of this difference. The differences in mean costs at 3, 2, and 1 month prior to death between patients in the intervention and control groups was assessed using the general linear model and the type III F test. Differences between our groups were significant at the p < 0.05 threshold level.
FIG. 3.
Costs of care. Costs of care for CARE Track patients compared to control patients were calculated for the last 3 months of life. Costs here represent UVA charges only on the inpatient and outpatient sides. Overall costs of care, and costs for each month prior to death were less for CARE Track patients than for controls, with the most significant differences noted for inpatient charges in the last months of life. CARE Track, Comprehensive Assessment with Rapid Evaluation and Treatment; UVA, University of Virginia.
Relation between hospice care and hospitalization
Differences in hospice utilization between groups accounted for some of the observed differences in hospitalization at the end of life, however, the differences in hospitalization outcomes between groups were still significant after accounting for concurrent differences in hospice utilization. The odds of hospitalization within 30 days of death were still significantly lower for patients in the CARE Track program compared to the control patients (OR = 0.51, 95% CI 0.33–0.78), after adjustments for differences in hospice utilization. The odds of death in the hospital were also still significantly lower for patients in the CARE Track program compared to control patients (OR = 0.20, 95% CI 0.10–0.39).
Timing of referral
For the 178 patients enrolled in CARE Track Year 1, the median time between palliative care referral and death was 72.5 days, with a mean 126.5 days. Earlier referral was not correlated with increased use of hospice care; in fact those patients enrolled in hospice were referred to the CARE Track program on average 110.6 days prior to death compared to those who were never referred to hospice care (referred on average 161.1 days prior to death). This difference was statistically significant (p = 0.0280).
Discussion
Cancer is one of the most common causes of death in this country. Patients with incurable malignancies have an illness trajectory consisting of a variable period of stability followed by a 3–6 month period of declining functional status and increasing symptom burden prior to death.17–21 During the last 6 months of life, these patients will have an increasing number of hospital admissions, and most of these patients spend the end of life in and out of the hospital and often the intensive care setting, with decreasing marginal medical benefit and worsening quality of life as their cancer progresses.22 While hospice referrals for this patient population are increasing, the average length of stay on hospice is short23 and aggressive care near the end of life remains common and may be increasing.24–27 Improving the quality of care of these patients while decreasing the costs due to unnecessary and burdensome medical interventions is an important priority for Medicare and other payers. Early integration of palliative care services into the care of those with advanced malignancies is increasingly viewed as an important tool in achieving this goal.28
Multiple studies have demonstrated benefits of a concurrent care model. One of the earliest and best known of these studies, by Temel et al.,7 compared patients with metastatic lung cancer referred at time of diagnosis to palliative care clinic with those with standard oncologic care. Patients in the concurrent care group had fewer hospital admissions and less chemotherapy at the end of life, had a better quality of life, were referred to hospice earlier and more often, and lived almost 4 months longer than control patients. Since that seminal article, other studies have demonstrated similar results in terms of quality of life and health care utilization.6 Most of these interventions initiated palliative care at the time of diagnosis. Automatic referral at time of diagnosis has the benefit of ensuring that all patients have access to palliative care services, however, it is unlikely to be practical given the nationwide shortage of palliative care specialists. Some patients may have a long, stable course prior to needing specialty palliative care services. One of the largest studies of early palliative care showed significant improvement in many symptoms for referred patients, but only at 4 months after referral.4 Others may never require specialty level palliative care because their needs for symptom management and EOL care planning are easily handled by the oncology team.12 Identifying which patients with advanced cancer need palliative care specialists in a timely fashion therefore is crucial to the development of sustainable programs and improved patient care.29,30
Our data add to prior research regarding the benefit of concurrent outpatient palliative care. Patients enrolled in Year 1 of the CARE Track intervention who were referred to outpatient palliative care services at the discretion of their oncologists had benefits similar to those in the study by Temel et al.7 in terms decreased hospitalization at the end of life, and increased hospice utilization and length of stay, despite being referred an average of 3–4 months prior to death. On the other hand, many patients were never referred to palliative care or referred to our inpatient service only at the very end of life; only approximately half of the patients with advanced cancer seen at our cancer center who died during the time frame of this intervention were ever referred to the CARE Track palliative care program at all.
Most palliative care services are hospital-based, and studies have noted a positive impact on resource utilization and quality of life for patients seen by these consultative teams.31,32 This study suggests that inpatient consultation only does not provide the same level of benefits as a combination of outpatient and inpatient palliative care. Those patients only seen by our inpatient team were usually consulted for EOL planning and almost all of these either died during that hospitalization (often after withdrawal of life support) or were sent home with hospice care for the last few days of life. While improved quality of EOL care and decreased hospital costs are an important contribution of palliative care programs, avoiding terminal hospitalization is arguably more important for those with incurable malignancies, and meeting this goal may require relationship building and coordination of care that can only occur when concurrent outpatient care is available in addition to inpatient palliative services.33
Much of the differences between the control and CARE Track care patients in terms of hospitalizations were due to earlier and more frequent referral to hospice services by those in the CARE Track group. At the very end of life, virtually all patients with cancer will be increasingly bedbound, have worsening symptoms, and increasing care requirements. Patients and family members who are unprepared for this part of the natural history of this disease will seek urgent care for these problems wherever it is available. If hospice services are not in place, this usually means bringing the patient to the hospital. Anticipating and identifying this part of the illness trajectory and educating the patient and family about this topic is an important part of the function of the early referral to palliative care clinic. This type of education allows for earlier hospice referral, but also resulted in fewer hospitalizations at end of life in the CARE Track group even for those without hospice care.
Interestingly, it was observed that patients with a short time between CARE Track referral and death had higher rates of hospice referral than those patients with longer length of stay on the CARE Track program. One possible interpretation of this data is that a common reason for referral to palliative care was anticipation of the need for hospice care. Because our program had strong connections to local hospices and a willingness to provide ongoing oversight of symptom management for patients enrolled in hospice, part of its function was to serve as prehospice program for patients identified by their oncologists as likely to need those services in the near future. Concurrent care with oncology and palliative care in the CARE Track program for these patients resulted in significantly earlier referral to hospice care than those referred to hospice by oncologists alone.
There are several important limitations to these data. This study was done at a single medical center, which serves a mainly white, rural population. This was not a randomized intervention and there were significant differences between the control and intervention patients in terms of age, gender, payer source, and type of malignancy. On the other hand, even when these variables were controlled for, differences between groups remained highly significant. Furthermore, the patients referred to our program were younger and were more likely to have Medicaid or no insurance, characteristics that have been shown to be correlated with decreased use of hospice services and/or increased likelihood of in-hospital death in prior studies.34–37
It is also possible that physicians who referred patients to the CARE Track program had a practice pattern of less aggressive care and early hospice referral as well. However, controlling for tumor type did not alter the differences between groups, and in this academic setting controlling for tumor type essentially controlled for provider as well.
Our data suggest areas for further study. As noted above, only approximately half of patients with incurable cancer seen at our institution were referred to the CARE Track program. This suggests that discretionary referral alone, while more sustainable than seeing every patient from time of diagnosis, may be insufficient to identify all of those who might benefit from palliative care services, and that there is a need for more research into how best to identify high-risk patients. The next phases of the CARE Track intervention utilize patient-reported outcome data based on NIH PROMIS items collected during clinic visits and integrated into the EMR (Epic Systems Corporation), as a tool to better identify those who may need palliative care services.
Acknowledgments
The project described in this paper is supported by grant number 1C1CMS331031-01-00 from the U.S. Department of Health and Human Services, Centers for Medicare & Medicaid Services. The content of this publication is solely the responsibility of the authors and does not necessarily represent the official views of the U.S. Department of Health and Human Services or any of its agencies. The research presented was conducted by the awardee. Findings may or may not be consistent with or confirmed by the independent evaluation contractor.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Yennurajalingam S, Atkinson B, Masterson J, et al. : The impact of an outpatient palliative care consultation on symptom burden in advanced prostate cancer patients. J Palliat Med 2012;15:20–24 [DOI] [PubMed] [Google Scholar]
- 2.Follwell M, Burman D, Le LW, et al. : Phase II study of an outpatient palliative care intervention in patients with metastatic cancer. J Clin Oncol 2009;27:206–213 [DOI] [PubMed] [Google Scholar]
- 3.Muir JC, Daly F, Davis MS, et al. : Integrating palliative care into the outpatient, private practice oncology setting. J Pain Symptom Manage 2010;40:126–135 [DOI] [PubMed] [Google Scholar]
- 4.Zimmermanm C, Swami N, Krzyanowsla M, et al. : Early palliative care for patients with advanced cancer: A cluster-randomized controlled trials. Lancet 2014;383:1721–1730 [DOI] [PubMed] [Google Scholar]
- 5.Bakitas M, Lyons KD, Hegel MT, et al. : Effects of a palliative care intervention on clinical outcomes in patients with advanced cancer: The Project ENABLE II randomized clinical trial. JAMA 2009;302:733–742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bauman JR, Temel JS. The integration of early palliative care with oncology care: The time has come for a new tradition. J Natl Compr Canc Netw 2014;12:1763–1771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Temel JS, Greer JA, Muzikansky A, et al. : Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med 2010;363:733–742 [DOI] [PubMed] [Google Scholar]
- 8.Hui D, Kim SH, Roquemore J, et al. : Impact of timing and setting of palliative care referral on quality of end-of-life care in cancer patients. Cancer 2014;120:1743–1749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brumley R, Enguidanos S, Jamison P, et al. : Increased satisfaction with care and lower costs: Results of a randomized trial of in-home palliative care. J Am Geriatr Soc 2007;55:993–1000 [DOI] [PubMed] [Google Scholar]
- 10.Greer JA, Pirl WF, Jackson VA, et al. : Effect of early palliative care on chemotherapy use and end-of-life care in patients with metastatic non-small-cell lung cancer. J Clin Oncol 2010;30:394–400 [DOI] [PubMed] [Google Scholar]
- 11.American Society of Clinical Oncology: The integration of palliative care into standard oncology care. J Clin Oncol 2012;30:880–888 [DOI] [PubMed] [Google Scholar]
- 12.Block S, Billings A: A need for scalable outpatient palliative care interventions Lancet 2014;383:1699–1700 [DOI] [PubMed] [Google Scholar]
- 13.Quill TE, Abernathy AP: Generalist plus specialist palliative care—Creating a more sustainable model. N Engl J Med 2013;368:1173–1176 [DOI] [PubMed] [Google Scholar]
- 14.Lupu D; American Academy of Hospice and Palliative Care Workforce Task Force: Estimate of current hospice and palliative medicine physician workforce shortage. J Pain Symtom Manage 2010;40:899–911 [DOI] [PubMed] [Google Scholar]
- 15.Sprouse T: I wish that things were different … redux. J Support Oncol 2011;9:103–104 [DOI] [PubMed] [Google Scholar]
- 16.Blackhall LJ, Duska L, Goldstein D, et al. : Implementation and impact for the care of patients with advanced cancer [abstract]. J Pain Symptom Manage 2015;49:346 [Google Scholar]
- 17.Cheung WY, Le LW, Zimmerman C: Symptom clusters in patients with advanced cancers. Support Care Cancer 2009;17:1223–1230 [DOI] [PubMed] [Google Scholar]
- 18.Gilbertson-White S, Aoouizerat BE, Jahan T, Miaskowski C: A review of the literature on multiple symptoms, their predictors and associated outcomes in patients with advanced cancer. Palliat Support Care 2011;9:81–102 [DOI] [PubMed] [Google Scholar]
- 19.Smith TJ, Hillner BE: Bending the cost curve in cancer care. N Engl J Med 2011;364:2060–2065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Teno JM, Weitzen S, Fennell ML, Mor V: Dying trajectory in the last year of life: Does cancer trajectory fit other diseases? J Palliat Med 2001;4:457–464 [DOI] [PubMed] [Google Scholar]
- 21.Bukki J, Scherbel J, Steil S, et al. : Palliative care needs, symptoms, and treatment intensity along the disease trajectory in medical oncology outpatients: A retrospective chart review. Support Care Cancer 2013;21:1743–1750 [DOI] [PubMed] [Google Scholar]
- 22.Chastek B, Harley C, Kallich J, et al. : Health care costs for patients with cancer at the end of life. J Oncol Pract 2012;8:75s–80s [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Morden NE, Chang CH, Jacobson JO, et al. : End of life care for Medicare beneficiaries with cancer is highly intensive overall and varies widely. Health Aff (Millwood) 2012;31:786–796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Temel JS, McCannon J, Greer JA, et al. : Aggressiveness of care in a prospective cohort of patients with advanced NSCLC. Cancer 2008;113:826–833 [DOI] [PubMed] [Google Scholar]
- 25.Behl D, Jatoi A: What do oncologists say about chemotherapy at the very end of life? Results from a semiqualitative survey. J Palliat Med 2010;13:831–835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ahmad S, O'Mahony MS: Where older people die: A retrospective population-based study. Q J Med 2005;98:865–870 [DOI] [PubMed] [Google Scholar]
- 27.Earle CC, Neville BA, Landrum MB, et al. : Trends in the aggressiveness of cancer care near the end of life. J Clin Oncol 2004;22:315–321 [DOI] [PubMed] [Google Scholar]
- 28.Rocque GB, Cleary JF: Palliative care reduces morbidity and mortality in cancer. Nat Rev Clin Oncol 2013;10:80–89 [DOI] [PubMed] [Google Scholar]
- 29.Hamann HA, Lee JW, Schiller JH, et al. : Clinician perceptions of care difficulty, quality of life, and symptom reports for lung cancer patients:an analysis from the Symptom Outcomes and Practice patterns (SOAPP) study. J Thorac Oncol 2013;8:1474–1483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Morita T, Fujimoto K, Namba M, et al. : Palliative care needs of cancer outpatients receiving chemotherapy: An audit of a clinical screening project. Support Care Cancer 2008;16:101–107 [DOI] [PubMed] [Google Scholar]
- 31.Penrod JD, Deb P, Luhrs C, et al. : Cost and utilization outcomes of patients receiving hospital-based palliative care consultation. J Palliat Med 2006;9:855–860 [DOI] [PubMed] [Google Scholar]
- 32.Smith TJ, Coyne P, Cassel B, et al. : A high-volume specialist palliative care unit and team may reduce in-hospital end-of-life care costs. J Palliat Med 2003;6:699–705 [DOI] [PubMed] [Google Scholar]
- 33.Yoong J, Park ER, Greer JA, et al. : Early palliative care in advanced lung cancer: A qualitative study. JAMA Intern Med 2013;173:283–290 [DOI] [PubMed] [Google Scholar]
- 34.Mack JW, Chen K, Boscoe FP, et al. : Underuse of hospice care by Medicaid-insured patients with stage IV lung cancer in New York and California. J Clin Oncol 2013;31:2569–2579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Keim-Malpass K, Erickson J, Malpass HC: End-of-life care characteristics for young adults with cancer who die in the hospital. J Palliat Med 2014;17:1359–1364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Barclay JS, Kuchibhatla M, Tulsky JA, Johnson KS: Association of hospice patients' income and care level with place of death. JAMA Intern Med 2013;173:450–456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Levinsky NG: Influence of age on Medicare expenditures and medical care in the last year of life. JAMA 2001;286:1349–1355 [DOI] [PubMed] [Google Scholar]