Abstract
Insurance coverage has increased among young adults due to the 2010 dependent coverage provision of the Affordable Care Act. However, little is known about the provision's effects on clinical outcomes and insurance coverage of patients with trauma – the most frequent cause of death and physical disability among young adults. Using the 2007-2012 National Trauma Databank, we conducted a difference-in-differences analysis of coverage rates among 19-25 year-old trauma patients, compared to 26-34 year-old controls, and examined trauma-relevant outcomes by patient, injury, and hospital characteristics. We found a 3.4 percentage point decrease in uninsured status among younger trauma patients following the policy change, concentrated among nonminority patients, those with less severe injuries, and those with lower trauma-related mortality risk. We did not detect significant changes in intensive care use or overall mortality. The heterogeneous coverage impact of this provision on high- versus low-risk trauma patients has implications for future efforts to expand coverage.
Background
Prior to the Affordable Care Act (ACA), approximately three in ten young adults in the United States lacked health insurance, the highest proportion of any age group.1 One of the earliest provisions of the ACA aimed to expand coverage to young adults by allowing them to stay on their parents' insurance plans until age 26, commonly referred to as the dependent coverage provision (DCP).2-5 Analyses of the provision's initial impact showed that as many as 3 million young adults gained insurance by 2012,4 accompanied by improvements in access to care.2,5,6 While, recent studies have also demonstrated increases in self-reported physical and mental health due to the policy,2,6,7 little is known about the impact of DCP on other health outcomes for young adults.
Traumatic injuries disproportionately account for the largest share of morbidity and mortality in young adults.8 For example, traumatic injuries — unintentional injury, suicide, and homicide — make up the top three causes of death among 15-34 year olds, together resulting in over 46,000 deaths annually (Appendix A1).8,9 By comparison, the next leading cause of death (cancer) is responsible for 5,000. While prior studies focused on the link between coverage for young adults and their access to primary care,2,5,6 emergency care,2,6,10 and mental health,2,7 this recent coverage expansion provides a unique opportunity to assess the impact of insurance access among young adults in the domain that contributes most to their risk of death and disability: trauma.
The Dependent Coverage Provision
The Dependent Coverage Provision (DCP) of the ACA took effect for plans renewing on or after September 23, 2010. Prior studies comparing 19-25 year olds to older adults not affected by this provision have found significant increases in private insurance coverage ranging from 3 to 10 percentage points.2-6,10-12 This increase in insurance has been uneven across groups, as the DCP led to greater insurance coverage increases among men5,13 and the unmarried.5 Detection of population level differences in coverage gains by racial or ethnic group, employment status, and educational status have, however, shown mixed results.5,6,13,14 Additional analyses focused on access to care have suggested that the policy has led to increased rates of primary care access,2-6,10-12 and fewer delays in seeking care due to cost concerns,5,6 with some suggestions that such gains have been greatest among the more highly educated.6,11
Despite the evidence on the effect of the DCP on insurance rates for young adults, little is known about the effects of the DCP on processes of care and health outcomes. Because young adults are relatively healthy, metrics that are typically studied for older adults - including primary care access, chronic disease management, and long-term survival – may provide minimal insight on the effectiveness of this particular insurance expansion. Here, we focus instead on acute traumatic injury as a highly prevalent, morbid, and costly clinical condition in this age group.
Although the DCP increased insurance coverage among young adults seeking emergency care,2,6,10 since the policy differentially favored young adults whose parents had private health insurance (who are likely to have higher incomes and educational backgrounds), it may have worsened existing disparities in coverage across socioeconomic racial/ethnic groups.6,7,13 A robust literature based on observational studies documents disparities in health outcomes after trauma between the insured and the uninsured.15-29 Compared to insured trauma patients, and after controlling for known risk factors at the patient, injury, and facility level, uninsured patients receive less care,16,17,30 are less likely to undergo a surgical procedure,17,30 have shorter length of hospital and intensive care unit (ICU) stay,26,27 have lower rates of discharge to a rehabilitation facility,18,22,24,27 and have higher in-hospital mortality.17,19-21,23,26-30 Though some have suggested that these disparities are driven by provider sensitivity to insurance status and subsequent treatment decisions,17,21,30 the findings to date are limited to suggestive associations since they were all derived from observational data. The 2012 DCP thus provides a unique opportunity to further understand the relationship between insurance coverage and trauma outcomes by exploiting a quasi-experimental research design.
In this study, we use the largest national database of trauma centers to explore three phenomena: the effect of the DCP on insurance coverage among young adult trauma patients, the differential coverage effect of this policy on subgroups of trauma patients, and the impact of DCP on trauma outcomes.
Study Data and Methods
Data
We used the 2007-2012 National Trauma Databank (NTDB) research data set. The NTDB was created by the American College of Surgeons and is the largest centralized source of trauma registry data in the nation, representing the vast majority of trauma centers in the United States.31,32 To date, the NTDB consists of data on over six million patient encounters from over 900 voluntarily enrolled trauma centers.
In this study, we included all encounters for patients aged 19-34 years old between 2007-2009 and 2011-2012. Our final sample included 841,600 patient encounters (Appendix A2).9 Consistent with prior studies, our treatment group was defined as patients aged 19-25 years old with our control group being those aged 26-34 years old. The two groups are similar in their medical conditions, job-market trends, baseline coverage trends, and clinical trauma-related characteristics (Exhibit 1).5,14,31,33
Exhibit 1. Patient and Injury Characteristics, 2007-2009.
| Ages 19-25 | Ages 26-34 | |
|---|---|---|
| Total Encounters | 246,282 | 217,886 |
| Mean Age | 21.8 | 29.7 |
| Male (%) | 76% | 76% |
| White (%) | 55% | 55% |
| Insurance Type | ||
| Private | 31% | 32% |
| Public | 18% | 19% |
| Other | 15% | 14% |
| Uninsured | 35% | 35% |
| Intent | ||
| Unintentional | 74% | 72% |
| Self-Harm | 2% | 2% |
| Assault | 23% | 26% |
| Mechanism | ||
| Fall | 10% | 14% |
| Gun shot wound | 12% | 9% |
| Motor vehicle collision | 41% | 36% |
| Motorcycle | 6% | 7% |
| Other | 7% | 9% |
| Ped/Cycle | 5% | 5% |
| Stab | 9% | 9% |
| Struck | 10% | 10% |
| Critical Inury (ISS ≥ 25) | 35% | 32% |
| Traumatic Brain Injury | 19% | 18% |
| Severe Extremity Injury | 13% | 12% |
| Level 1 Trauma Center | 63% | 64% |
| Safety Net Hospital | 11% | 11% |
| Non-Profit Hospital | 94% | 94% |
| University Teaching Hospital | 56% | 56% |
SOURCE: National Trauma Data Bank, 2007-2009 (n = 464,168) NOTE: MVC, motor vehicle collision; ISS, Injury severity score
Given the objective of the policy to increase insurance coverage among young adults, one of our primary outcomes was insurance status in this population. We categorized insurance status as private (including Blue Cross/Blue Shield, Private/Commercial Insurance, and workers' compensation), public (including Medicare, Medicaid, and other government), other (including no fault automobile and other), and uninsured (coded as “self pay” in the NTDB). To address the category of “unknown” insurance status in the NTDB, our primary analysis used multiple imputation to predict insurance status based on patient, injury, and facility factors; these results did not differ from an alternative approach in which we simply excluded patients with unknown insurance status from our sample (Appendix A2).9
We also examined three clinical outcomes of interest: 1) in-hospital mortality (which excluded patients who had already died by the time they had arrived at the hospital, but included deaths occurring in the emergency department or during the hospital admission); 2) ICU length of stay (LOS); and 3) rate of discharge to post-acute care facility (including rehabilitation facility, skilled nursing facility, and intermediate care facility).
Our analyses adjusted for patient demographics, including age, gender, and race, and injury characteristics, including injury severity score (ISS, a measure of anatomic severity),34 revised trauma score (RTS, a measure of physiologic injury severity),35 blunt versus penetrating injury type, mechanism of injury, and the presence of a severe head injury or severe extremity injury. Finally, we adjusted for the following facility characteristics: status as a level-1 or non-level-1 trauma center, teaching status, non-profit status, and safety-net status (safety-net hospitals defined as the top decile of facilities ranked by proportion of patients with no insurance or Medicaid).15,36 Each of these covariates were selected for their established association with our outcomes of interest.32,37
Analysis
We used a difference-in-differences (DID) approach comparing changes in outcomes in the treatment group before and after the DCP to the changes in our control group. This approach removes bias from secular trends, based on the assumption that these trends would have been similar for the two age groups in the absence of the DCP. The approach also accounts for time-invariant differences between the treatment and control group by adjusting for baseline differences in outcomes. To evaluate the effect of the DCP on young adults, we defined the pre-policy period as 2007-2009 and the post-policy period as 2011-2012. We excluded year 2010 as a washout period, since the policy gradually took effect from September of 2010 through the following September (as all plans renewed), and the NTDB does not provide monthly or quarterly variables.
We performed three primary analyses. First we examined how the uninsured rate changed among 19-25 year old trauma patients before and after the DCP, as compared to 26-34 year olds. Second, we used a similar design to examine which subgroups of trauma patients in this age group experienced the largest changes in rates of uninsured after the DCP. Finally, we used this quasi-experimental framework to examine whether the provision had any measureable impact on clinical outcomes that may be plausibly associated with changes in insurance status among trauma patients.17,19-29,38 For all analyses, we adjusted for facility-level fixed effects and clustered standard errors at the facility level to allow for within-facility correlation. For the subgroup analysis regarding changes in uninsurance, we tested for between subgroup differences in the policy's impact by adding an interaction term between post-period, young adult, the patient subgroup feature of interest.
This study has undergone human subjects approval at the Harvard Medical School. All analyses were completed using Stata version 13.0 (StataCorp). A two-sided p value of 0.05 was used to establish statistical significance.
Limitations
To our knowledge, this is the first quasi-experimental study to examine the impact of the DCP on trauma patients. Still, there remain a number of limitations to the analysis. First, while the NTDB is the largest national trauma database, it is a convenience sample as opposed to being drawn from a nationally representative sample. It does contain, however, data from approximately 95% of all Level 1 trauma centers, as defined by the American College of Surgeons (ACS). Though it purposefully over-represents the most severely injured patients, the NTDB has been used throughout the clinical literature to understand the state of trauma care in the country especially pertaining to meaningful clinical endpoints such as in-hospital mortality, ICU days, and discharge to a post-acute care facility.31,32,37 This potential oversampling of more severely injured patients – if anything - should increase the likelihood of finding an effect of the DCP on our clinical outcomes of interest.
Second, the NTDB is a visit-level database; thus, it does not follow individual patients over time and is potentially subject to double counting. Also, because this study relies upon a visit-level analysis with a sample limited to those individuals with a trauma event, our estimates are not analogous to previous population-based estimates of coverage changes due to the DCP.
Thirdly, the NTDB does not contain data on other potential drivers of variation in the DCP's effects, namely patient demographics such as educational status, income, employment, marital status, and state of residence.
Finally, we rely on a difference-in-differences analysis to evaluate for changing trends in the composition of the trauma patient population over time in an attempt to reduce bias from secular trends, but it is possible that our results were impacted by time-varying confounding factors. One such possibility is that voluntary enrollment by facilities into the NTDB has increased substantially over the last 10 years, with each additional year including more trauma centers and thus more patient encounters. If the age mix of the newly added trauma centers differed significantly from those already in the sample it could bias our results. A sensitivity analysis using only facilities present from 2008-2010, however, showed no change in any of our key findings.
Study Results
Coverage Changes After the DCP
After the policy was implemented, 19-25 year old trauma patients experienced a 3.4 percentage point decrease, or a 9.5% relative drop, in the risk of being uninsured (p<0.001) as compared to the 26-34 year old control group (Exhibit 2). This significant decrease in uninsured status among trauma patients was coupled with significant decreases in public insurance (-2.2%, p<0.001) and significant increases in private insurance (+5.3%, p<0.001) (Exhibit 3).
Exhibit 2. Proportion of Among Young Adult Trauma Patients Without Insurance, Ages 19–25 and 26–34, By Year, 2007–12.
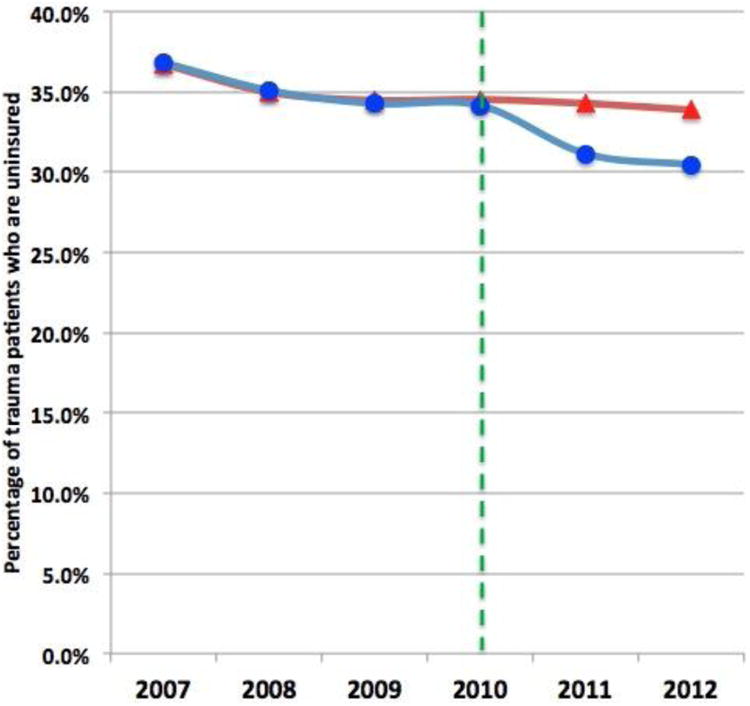
| 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | |
| Ages 19-25 | 36.9% | 35.1% | 34.3% | 34.2% | 31.2% | 30.5% |
| Ages 26-34 | 36.7% | 35.0% | 34.5% | 34.5% | 34.3% | 33.9% |
Exhibit 3. Changes in Insurance Status for Young Adult Trauma Patients Ages 19-25 vs 26-34, before and after the ACA-DCP.
| Ages 19-25 | Ages 26-34 | Difference in change between age groups1 | p value for between-group difference | |||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Before ACA-DCP | After ACA-DCP | Before ACA-DCP | After ACA-DCP | |||
| Insurance Status | ||||||
|
| ||||||
| Private | 31.3% | 34.7% | 32.4% | 30.3% | 5.3% | <0.001*** |
| Public | 18.2% | 18.7% | 18.4% | 21.1% | -2.2% | <0.001*** |
| Other | 15.2% | 15.8% | 14.0% | 14.5% | 0.2% | 0.18 |
| Uninsured | 35.3% | 30.8% | 35.3% | 34.1% | -3.4% | <0.001*** |
SOURCE: National Trauma Data Bank, 2007-2009 & 2011-2012 (n = 841,600). Data for patients with unknown insurance status were estimated using 20 rounds of multiple imputation (n=152,169). NOTE: ACA, Affordable Care Act; DCP, dependent coverage provision; CI, confidence interval; ICU, intensive care unit. 1. Adjusted for age, year, and facility effects;
p < 0.05,
p < 0.01,
p < 0.001
Subgroup Changes in Coverage After the DCP
Notably, the coverage expansion provided by the DCP was not evenly distributed across all uninsured populations. Young adults who experienced the greatest reductions in uninsurance were men, non-Hispanic Whites, those with less severe injuries, and those presenting to non-teaching hospitals (Exhibit 4). Those experiencing significantly smaller decreases in uninsured status were racial/ethnic minorities, assault victims, gunshot wound and motor vehicle collision victims, those with severe or critical injury severity, and those presenting to safety-net facilities.
Exhibit 4. Changes in Uninsured Status for Young Adult Trauma Patients Ages 19-25 and 26-34, By Subgroup of Patient and Injury Characteristics.
| Group1 | Adults ages 19-25 who are uninsured, before ACA (%) | Percentage-point change, before versus after ACA | Difference in change between age groups | p value for between-subgroupdifference2 | |
|---|---|---|---|---|---|
|
| |||||
| Ages 19-25 | Ages 26-34 | ||||
| Full Sample | 35.3% | -4.5% | -1.2% | -3.3% | <0.001*** |
|
| |||||
| age3 | |||||
|
| |||||
| Age 19-21 | 33.4% | -5.0% | (-1.2%) | -3.8% | Ref |
| Age 22-25 | 36.9% | -4.1% | (-1.2%) | -2.9% | 0.01* |
|
| |||||
| sex | |||||
|
| |||||
| Males | 37.7% | -4.4% | -0.8% | -4.4% | Ref |
| Females | 27.8% | -4.2% | -2.2% | -2.0% | 0.001** |
|
| |||||
| race | |||||
|
| |||||
| White | 29.9% | -5.3% | -0.5% | -4.8% | Ref |
| Nonwhite | 42.5% | -3.7% | -1.8% | -1.8% | <0.001*** |
|
| |||||
| intent | |||||
|
| |||||
| Unintentional | 30.8% | -4.5% | -0.9% | -3.5% | Ref |
| Self-Harm | 41.1% | -5.3% | -2.1% | -3.2% | 0.36 |
| Assault | 47.0% | -3.8% | -1.7% | -2.1% | 0.01* |
|
| |||||
| mechanism | |||||
|
| |||||
| Fall | 31.5% | -4.5% | -0.4% | -4.1% | Ref |
| Motorcycle | 27.6% | -2.9% | 0.9% | -3.8% | 0.97 |
| Other | 34.5% | -3.9% | -0.6% | -3.4% | 0.68 |
| Ped/Cycle | 32.4% | -5.3% | -2.2% | -3.1% | 0.41 |
| Stab | 47.1% | -4.0% | -1.0% | -3.0% | 0.26 |
| Struck | 39.5% | -4.3% | -1.4% | -2.9% | 0.30 |
| Motor vehicle collision | 30.3% | -4.9% | -2.1% | -2.8% | 0.06 |
| Gun shot wound | 48.9% | -4.0% | -1.8% | -2.1% | 0.04* |
|
| |||||
| injury severity | |||||
|
| |||||
| Minor (ISS 1-9) | 35.1% | -5.6% | -1.8% | -3.8% | Ref |
| Moderate (ISS 10-15) | 33.4% | -4.3% | -0.3% | -4.0% | 0.98 |
| Severe (ISS 16-24) | 31.7% | -3.8% | -1.0% | -2.8% | 0.10 |
| Critical (ISS >= 25) | 38.5% | -3.7% | -1.0% | -2.7% | 0.04* |
|
| |||||
| traumatic brain injury (TBI) | |||||
|
| |||||
| With TBI | 33.1% | -5.0% | -1.7% | -3.3% | Ref |
| No TBI | 35.9% | -4.5% | -1.1% | -3.4% | 1.00 |
|
| |||||
| severe extremity injury | |||||
|
| |||||
| Severe Extremity Injury | 31.1% | -4.7% | -2.4% | -2.3% | Ref |
| No Severe Extremity Injury | 36.0% | -4.5% | -1.1% | -3.4% | 0.13 |
|
| |||||
| trauma center level | |||||
|
| |||||
| Level 1 Trauma Center | 35.8% | -4.7% | -1.5% | -3.1% | Ref |
| Level 2 or greater | 34.5% | -4.2% | -0.7% | -3.5% | 0.59 |
|
| |||||
| hospital profit status | |||||
|
| |||||
| Non-profit Hospital | 35.2% | -4.8% | -1.6% | -3.2% | Ref |
| For-profit Hospital | 37.9% | -2.6% | 1.2% | -3.7% | 0.34 |
|
| |||||
| hospital safety net status | |||||
|
| |||||
| Safety Net Hospital | 54.6% | -3.7% | -1.9% | -1.8% | Ref |
| Non-Safety Net Hospital | 33.0% | -4.8% | -1.3% | -3.5% | 0.04* |
|
| |||||
| hospital teaching status | |||||
| University | 36.7% | -4.8% | -2.0% | -2.8% | Ref |
| Community Affiliated | 32.4% | -4.0% | -0.4% | -3.6% | 0.38 |
| Non-teaching | 37.5% | -4.7% | -0.2% | -4.5% | 0.06 |
SOURCE: National Trauma Data Bank, 2007-2009 & 2011-2012 (n = 841,600). Data for patients with unknown insurance status were estimated using 20 rounds of multiple imputation (n=152,169). NOTE: ACA, Affordable Care Act; DCP, dependent coverage provision; ISS, injury severity score; TBI, traumatic brain injury. 1. p-values for difference in change after the policy for 19-25 year olds, as compared to 26-34 year olds, are all p < 0.05; 2. adjusted for age, year, gender, and facility; 3. Each age subgroup was compared against the entire control group to determine adjusted changes in insurance status;
p < 0.05,
p < 0.01,
p < 0.001
Changes in Clinical Outcomes After the DCP
In Exhibit 5, we summarize the changes in in-hospital mortality, length of ICU stay, and rates of discharge to post-acute care facility for 19-25 years olds after the policy, relative to controls. The technical appendix provides a detailed explanation of all models.9 Overall, there were no significant differences in in-hospital mortality, length of ICU stay, or rate of discharge to post-acute care facility after the DCP took effect.
Exhibit 5. Changes in Clinical Outcomes for Young Adult Trauma Patients Ages 19-25 vs 26-34, before and after the ACA-DCP.
| Ages 19-25 | Ages 26-34 | Unadjusted difference in change between age groups | Risk adjusted difference in change between age groups (95% CI)1 | p value for between-group difference | |||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| Before ACA-DCP | After ACA-DCP | Before ACA-DCP | After ACA-DCP | ||||
| Clinical outcomes among young adult trauma patients | |||||||
|
| |||||||
| Mortality (per 100K)2 | 2876 | 2626 | 2660 | 2426 | -15 | 44 (-94, 183) | 0.53 |
| ICU stay (days)3 | 5.11 | 5.01 | 5.34 | 5.24 | -0.01 | 0.01 (-0.15, 0.12) | 0.85 |
| Discharge to rehabilitation facility (%)4 | 10.1% | 10.3% | 10.6% | 10.8% | 0.0% | 0.0% (-0.3, 0.3) | 0.89 |
SOURCE: National Trauma Data Bank, 2007-2009 & 2011-2012. NOTE: ACA, Affordable Care Act; DCP, dependent coverage provision; CI, confidence interval; ICU, intensive care unit. 1. Risk adjusted models for clinical outcomes adjusted for age, year, facility, gender, race, injury severity, injury mechanism, traumatic brain injury, level-1 trauma center status, teaching status, for-profit status, and safety-net hospital status; 2. n= Entire sample, excluding dead on arrival: 832,876; 3. n= Patients with any ICU stay: 204,981; 4. n= Patients surviving to discharge: 618,063.
p < 0.05,
p < 0.01,
p < 0.001
Sensitivity Analyses
Sensitivity analyses that included only patients with known insurance status and thus no imputed data showed similar results for insurance coverage changes (Appendix A3).9 In order to focus on the patients at highest risk for clinical outcomes of interest, we performed sensitivity analyses including only patients with moderate, severe, or critical injuries (ISS >8). This also did not meaningfully alter our results. A third set of sensitivity analyses comparing patients 23-25 years of age to patients 27-29 years of age found similar results for both changes in insurance category and clinical outcomes (Appendix A4).9
Discussion
Our results suggest that the ACA's DCP led to a decrease in the uninsured rate among young adults experiencing trauma, the greatest cause of death and physical disability for this population. These data also highlight the heterogeneous effect of the DCP across populations. We found that coverage gains were smallest among minorities, patients of safety-net hospitals, gunshot or motor vehicle crash victims, and those with high-severity injuries, whereas gains were greatest among white males with less severe injuries.
Our results are broadly consistent with previous analyses of the DCP that have used population survey data.2,3,5-7,12–14,33 However, this study provides new evidence regarding the heterogeneous impact of the ACA's DCP across subpopulations in trauma as well as its potential impact on racial and ethnic disparities. Young adults presenting to the emergency departments of safety-net hospitals with the most severe injuries, especially after a gunshot wound or a motor vehicle crash, were significantly less likely to receive coverage through the DCP than other young adults. Furthermore, non-white trauma patients experienced significantly lower reductions in uninsured status than did non-Hispanic whites. This suggests that the effect of the DCP on the young adult trauma patients differs from its effects among the general population of young adults. Previous studies examining the effect of the DCP on the general population of young adults have shown no significant differences in the relative degree of coverage expansion between races.5,6,13,14 However, our findings among trauma patients add to the sub-analysis finding by Shane et al. that, among those patients below 133% of the federal poverty line, non-Hispanic whites were more likely to receive coverage than Hispanics.14
That those trauma patients least likely to gain coverage were the most severely injured, minorities, and those already relying on safety-net systems suggests that these high-risk populations may remain relatively outside of the reach of this new policy. This may be due in part to lower rates of parental employment and/or private insurance coverage, which are prerequisites for the DCP to have an impact, or to other factors related to less social support for this group of uninsured young adults. While this policy was not intended to be the only solution to lowering uninsurance among young adults, these data shed new light on the differential effects it has had consistent with longstanding socioeconomic disparities. This is particularly salient in light of the racial demographics of states that have elected not to expand Medicaid through the ACA.39,40 Minority uninsured young adults may be among the most vulnerable in society given that two key provisions of the ACA's DCP and Medicaid expansion may have limited impact on improving their access to insurance.
The quasi-experimental framework of our analysis adds insight to previous observational studies that have found an association between uninsurance and poor outcomes following trauma. We found no statistically significant changes in clinical outcomes linked to this policy among young adults. In the context of the literature highlighting an association between uninsured status and trauma outcomes,17,21,30 we had expected to find improvements in clinical outcomes associated with the coverage expansion. Moreover, a 2012 study showing that Medicaid expansion has lead to a reduction in all-cause mortality further supported this expectation, even though trauma was not the primary driver to the mortality rates in the study population.41 Nevertheless, our findings offer a contrasting view.
There are, however, many possible explanations for the lack of improvement in trauma-relevant clinical outcomes among young adults following the DCP. Most importantly, our findings must be interpreted in light of the 95% confidence interval around our difference-in-differences mortality estimate (Exhibit 5), which rules out a reduction in mortality of greater than -94 deaths per 100,000, from a baseline of 2,876 per 100,000 (a 3.3% relative reduction in mortality). Given that the coverage change in our sample was only 3.4 percentage points, our findings cannot rule out substantial individual-level mortality changes that would still be consistent with prior research.17,21
Another possibility is that prior observational studies showing a link between worse trauma outcomes and uninsured status are confounded by unmeasured covariates, rather than demonstrating a causal relationship. This is the first study to use a quasi-experimental approach to investigate this well-established association drawn from multiple prior observational studies. We do not find evidence to support a causal interpretation of this pattern. Possible unmeasured drivers include patient comorbidities, socioeconomic status, variability in pre-hospital care, and a segregated trauma system whereby predominately minority-serving hospitals have worse outcomes after trauma.21,38
Moreover, our findings raise the possibility that the magnitude of the health gains in the general population associated with insurance coverage41,42,43 may not extend to the care of traumatic injuries. This may be driven in part by policies such as the Emergency Medical Treatment and Labor Act (EMTALA) as well as the immediate nature of trauma care in which a significant proportion of life-saving treatment is provided before a patient's insurance status is known.
Another possible explanation for the lack of clinical findings is that those who gain coverage from the DCP were less severely injured patients who were not as likely to experience any of our clinical outcomes of interest. As such, the magnitude of improved outcomes may have been too small for our study to detect. However, this idea further emphasizes the fact that the uninsured trauma patients who were already at the highest risk of poor clinical outcomes were the least likely to benefit from coverage expansion.
The changing clinical makeup of the remaining uninsured pool of young adult trauma patients also has significant implications for economic projections in medical centers about the cost of caring for the uninsured. The DCP did in fact lead to significant decreases in the rate of uninsured trauma patients and the total number of non-paying trauma patients has decreased significantly. However, the cost per hospitalization of an uninsured young adult trauma patient is likely to be greater after the DCP due the increased injury severity — emphasizing the fact that a given percentage point reduction in uninsured patients does not equate to an identical percentage point reduction in uncompensated care.
Conclusion
The 2010 DCP of the ACA led to a significant 3.4 percentage point decrease in the rate of uninsured trauma patients aged 19-25. However, our results show an uneven effect of this coverage expansion among the observed sample of trauma patients, with smaller coverage gains among minorities, patients in safety net hospitals, and those with more severe injuries. Furthermore, we found no significant change in clinical trauma outcomes as a result of this coverage expansion. Understanding the drivers and consequences of heterogeneous impacts of coverage expansion will help inform future polices that aim to reduce the number of uninsured Americans.
Supplementary Material
Acknowledgments
The authors acknowledge John Orav and Jennifer Polinski for their assistance in early analyses of these data. John Scott is funded by the Henry Ellis Warren Fellowship and the Center for Surgery and Public Health at Brigham and Women's Hospital. Kirstin Scott is funded by the Agency for Healthcare Research and Quality (AHRQ; Grant No. T32HS000055) and the National Science Foundation Graduate Research Fellowship (Grant No. NSF 13-584) Aaron Schwartz was supported by the National Institute on Aging of the National Institutes of Health (Grant No. F30 AG044106). Zirui Song was supported by the National Institute on Aging (Grant No. NIA F30 AG039175–2). Thomas Tsai was supported by the National Cancer Institute's Program in Cancer Outcomes Research Training (Grant No. R25CA92203). Tsai serves as an adviser and Benjamin Sommers serves part time as an adviser in the Office of the Assistant Secretary for Planning and Evaluation at the Department of Health and Human Services (HHS). The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of AHRQ or HHS.
Appendix A1: Leading Causes of Death for Young Adults, 2010
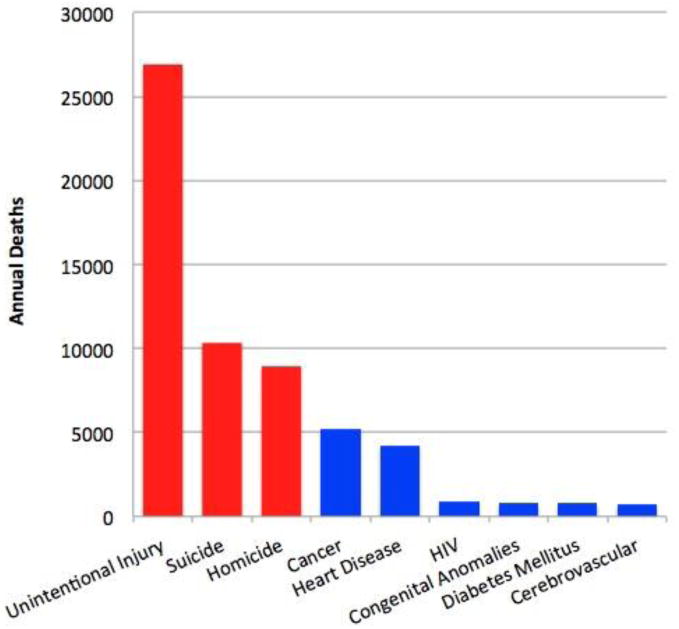
SOURCE: National Vital Statistics System, National Center for Health Statistics, Centers for Disease Control and Prevention, 2010. NOTE: Young Adults ages 15-34; Trauma-related causes are in red, nontrauma-related in blue; HIV, Human immunodeficiency virus
| Unintentional Injury | 26914 |
| Suicide | 10335 |
| Homicide | 8936 |
| Cancer | 5223 |
| Heart Disease | 4250 |
| HIV | 903 |
| Congenital Anomalies | 809 |
| Diabetes Mellitus | 771 |
| Cerebrovascular | 707 |
Appendix A3: Changes in Insurance Status for Young Adult Trauma Patients Ages 19-25 vs 26-34, before and after the ACA-DCP. Sensitivity Analysis in which unknown insurance status excluded from analysis
| Ages 19-25 | Ages 26-34 | Difference in change between age groups1 | p value for between-group difference | |||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Before ACA-DCP | After ACA-DCP | Before ACA-DCP | After ACA-DCP | |||
| Insurance Status2 | ||||||
|
| ||||||
| Private | 31.1% | 35.0% | 32.5% | 30.2% | 6.2% | <0.001*** |
| Public | 17.9% | 18.6% | 18.2% | 21.3% | -2.5% | <0.001*** |
| Other | 15.3% | 16.0% | 13.7% | 14.5% | -0.1% | 0.918 |
| Uninsured | 35.7% | 30.5% | 35.6% | 34.1% | -3.7% | <0.001*** |
SOURCE: National Trauma Data Bank, 2007-09 & 2011-12. NOTE: ACA, Affordable Care Act; DCP, dependent coverage provision; CI, confidence interval; ICU, intensive care unit. 1. Adjusted for age, year, and facility effects; 2. All patients with known insurance status (n= 709,206);
p < 0.05,
p < 0.01,
p < 0.001
Appendix A4: Changes in Insurance Status and Clinical Outcomes for Young Adult Trauma Patients Ages 23-25 vs 27-29, before and after the ACA-DCP
| Ages 19-25 | Ages 26-34 | Difference in change between age groups1 |
Risk
adjusted difference in change between age groups (95% CI)2 |
p value
for between- group difference |
|||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| Before ACA-DCP |
After ACA-DCP |
Before ACA-DCP |
After ACA-DCP |
||||
| Insurance Status3 | |||||||
|
| |||||||
| Private | 29.7% | 32.9% | 31.3% | 29.2% | 5.0% | n/a | <0.001*** |
| Public | 17.5% | 18.6% | 18.2% | 21.0% | -1.8% | n/a | <0.001*** |
| Other | 14.8% | 15.5% | 14.0% | 14.9% | 0.0% | n/a | 0.86 |
| Uninsured | 37.9% | 33.0% | 36.5% | 34.8% | -3.3% | n/a | <0.001*** |
|
| |||||||
| Clinical outcomes among entire population3 | |||||||
|
| |||||||
| Mortality (per 100K) | 2880 | 2538 | 2715 | 2386 | -14 | -38 (-238, 162) | 0.71 |
| ICU stay (days) | 5.26 | 5.04 | 5.27 | 5.12 | -0.06 | -0.04 (-0.27, 0.18) | 0.69 |
| Discharge to rehabilitation facility (%) | 10.12% | 10.16% | 10.23% | 10.26% | 0.0% | 0.0% (-0.5, 0.5) | 0.90 |
SOURCE: National Trauma Data Bank, 2007-2009 & 2011-2012. NOTE: ACA, Affordable Care Act; DCP, dependent coverage provision; CI, confidence interval; ICU, intensive care unit. 1. Risk adjusted models for clinical outcomes adjusted for age, year, facility, gender, race, injury severity, injury mechanism, traumatic brain injury, level-1 trauma center status, teaching status, for-profit status, and safety-net hospital status; 3. n= Patients age 23-25 and 27-29 with known insurance status: 326,033
p < 0.05,
p < 0.01,
p < 0.001
Contributor Information
John W. Scott, Email: jwscott@partners.org, both at Brigham and Women's Hospital, in Boston, Massachusetts.
Benjamin D. Sommers, At the Harvard School of Public Health and an assistant professor of medicine at Brigham and Women's Hospital, both in Boston.
Thomas C. Tsai, the Department of Health Policy and Management, Harvard School of Public Health.
Kirstin W. Scott, the Interfaculty Initiative in Health Policy, Harvard University, in Cambridge, Massachusetts.
Aaron L. Schwartz, the Department of Health Care Policy, Harvard University.
Zirui Song, At the Massachusetts General Hospital and a clinical fellow at Harvard Medical School, both in Boston.
Endnotes
- 1.DeNavas-Walt C, Proctor BD, Smith JC. US Census Bureau. Washington, DC: US Government Printing Office; 2010. Income, Poverty, and Health Insurance Coverage in the United States: 2009; pp. 1–79. [Google Scholar]
- 2.Antwi YA, Moriya AS, Simon K. Access to Health Insurance and the Use of Inpatient Medical Care: Evidence from the Affordable Care Act Young Adult Mandate; Indiana University Working Paper; December, 2013; [DOI] [PubMed] [Google Scholar]
- 3.Cantor JC, Monheit AC, delia D, Lloyd K. Early impact of the Affordable Care Act on health insurance coverage of young adults. Health Serv Res. 2012;47:1773–1790. doi: 10.1111/j.1475-6773.2012.01458.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sommers BD. Number of young adults gaining insurance due to the Affordable Care Act now tops 3 million. Department of Health and Human Services ASPE Issue Brief. 2012 Jun; [Google Scholar]
- 5.Sommers BD, Buchmueller T, Decker SL, Carey C, Kronick R. The Affordable Care Act Has Led To Significant Gains In Health Insurance And Access To Care For Young Adults. Health Aff (Millwood) 2013;32:165–174. doi: 10.1377/hlthaff.2012.0552. [DOI] [PubMed] [Google Scholar]
- 6.Barbaresco S, Courtemanche C, Qi Y. Impacts of the Affordable Care Act Dependent Coverage Provision on Health-Related Outcomes of Young Adults; National Bureau of Economic Research Working Paper; May, 2014; [DOI] [PubMed] [Google Scholar]
- 7.Chua KP, Sommers BD. Changes in Health and Medical Spending Among Young Adults Under Health Reform. JAMA. 2014;311:2437–2439. doi: 10.1001/jama.2014.2202. [DOI] [PubMed] [Google Scholar]
- 8.National Vital Statistics System, National Center for Health Statistics, CDC. [internet] Ten Leading Causes of Death by Age Group United States -2010. cited 2014 July 28 Available from: http://www.cdc.gov/injury/wisqars/pdf/10lcid_all_deaths_by_age_group_2010-a.Pdf.
- 9.To access the Appendix, click on the Appendix link in the box to the right of the article online.
- 10.Mulcahy A, Harris K, Finegold K, Kellermann A, Edelman L, Sommers BD. Insurance coverage of emergency care for young adults under health reform. N Engl J Med. 2013;368:2105–2112. doi: 10.1056/NEJMsa1212779. [DOI] [PubMed] [Google Scholar]
- 11.Antwi YA, Moriya A, Simon K. Effects of Federal Policy to Insure Young Adults: Evidence From the 2010 Affordable Care Act Dependent Coverage Mandate. National Bureau of Economic Research Working Paper; June, 2012. [Google Scholar]
- 12.Sommers BD, Kronick R. The Affordable Care Act and insurance coverage for young adults. JAMA. 2012;307:913–914. doi: 10.1001/jama.307.9.913. [DOI] [PubMed] [Google Scholar]
- 13.O'Hara B, Brault MW. The Disparate Impact of the ACA-Dependent Expansion across Population Subgroups. Health Serv Res. 2013;48:1581–1592. doi: 10.1111/1475-6773.12067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shane DM, Ayyagari P. Will health care reform reduce disparities in insurance coverage?: evidence from the dependent coverage mandate. Medical Care. 2014;52:528–534. doi: 10.1097/MLR.0000000000000134. [DOI] [PubMed] [Google Scholar]
- 15.Bell TM, Zarzaur BL. Insurance status is a predictor of failure to rescue in trauma patients at both safety net and non-safety net hospitals. J Trauma. 2013;75:728–733. doi: 10.1097/TA.0b013e3182a53aaa. [DOI] [PubMed] [Google Scholar]
- 16.Bolorunduro OB, Haider AH, Oyetunji TA, Khoury A, Cubangbang M, Haut ER, Greene WR, Chang DC, Cornwell EE, Siram SM. Disparities in trauma care: are fewer diagnostic tests conducted for uninsured patients with pelvic fracture? Am J Surg. 2013;205:365–370. doi: 10.1016/j.amjsurg.2012.10.026. [DOI] [PubMed] [Google Scholar]
- 17.Doyle J, Joseph J. Health Insurance, Treatment and Outcomes: Using Auto Accidents as Health Shocks. Review of Economics and Statistics. 2005;87:256–270. [Google Scholar]
- 18.Englum BR, Villegas C, Bolorunduro O, Haut ER, Cornwell EE, Efron DT, Haider AH. Racial, Ethnic, and Insurance Status Disparities in Use of Posthospitalization Care after Trauma. J Am Col Surg. 2011;213:699–708. doi: 10.1016/j.jamcollsurg.2011.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Greene WR, Oyetunji TA, Bowers U, Haider AH, Mellman TA, Cornwell EE, Siram SM, Chang DC. Insurance status is a potent predictor of outcomes in both blunt and penetrating trauma. Am J Surg. 2010;199:554–557. doi: 10.1016/j.amjsurg.2009.11.005. [DOI] [PubMed] [Google Scholar]
- 20.Haider AH, Chang DC, Efron DT, Haut ER, Crandall M, Cornwell EE. Race and Insurance Status as Risk Factors for Trauma Mortality. Arch Surg. 2008;143:945–949. doi: 10.1001/archsurg.143.10.945. [DOI] [PubMed] [Google Scholar]
- 21.Haider AH, Weygandt PL, Bentley JM, Moon MF, Rehman KA, Zarzaur BL, Crandall ML, Cornwell EE, Cooper LA. Disparities in trauma care and outcomes in the United States. J Trauma. 2013;74:1195–1205. doi: 10.1097/TA.0b013e31828c331d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nirula R, Nirula G, Gentilello LM. Inequity of rehabilitation services after traumatic injury. J Trauma. 2009;66:255–259. doi: 10.1097/TA.0b013e31815ede46. [DOI] [PubMed] [Google Scholar]
- 23.Rosen H, Saleh F, Lipsitz S, Rogers SO, Gawande AA. Downwardly mobile: the accidental cost of being uninsured. Arch Surg. 2009;144:1006–1011. doi: 10.1001/archsurg.2009.195. [DOI] [PubMed] [Google Scholar]
- 24.Sacks GDG, Hill CC, Rogers SOS. Insurance status and hospital discharge disposition after trauma: inequities in access to postacute care. J Trauma. 2011;71:1011–1015. doi: 10.1097/TA.0b013e3182092c27. [DOI] [PubMed] [Google Scholar]
- 25.Salim A, Ottochian M, DuBose J, Inaba K, Teixeira P, Chan LS, Margulies DR. Does insurance status matter at a public, level I trauma center? J Trauma. 2010;68:211–216. doi: 10.1097/TA.0b013e3181a0e659. [DOI] [PubMed] [Google Scholar]
- 26.Schoenfeld AJ, Belmont PJ, See AA, Bader JO, Bono CM. Patient demographics, insurance status, race, and ethnicity as predictors of morbidity and mortality after spine trauma: a study using the National Trauma Data Bank. Spine J. 2013;13:1766–1773. doi: 10.1016/j.spinee.2013.03.024. [DOI] [PubMed] [Google Scholar]
- 27.Taghavi S, Jayarajan SN, Duran JM, Gaughan JP, Pathak A, Santora TA, Willis AI, Goldberg AJ. Does payer status matter in predicting penetrating trauma outcomes? Surgery. 2012;152:227–231. doi: 10.1016/j.surg.2012.05.039. [DOI] [PubMed] [Google Scholar]
- 28.Tepas I, Joseph J, Pracht EE, Orban BL, Flint LM. Insurance Status, Not Race, Is a Determinant of Outcomes from Vehicular Injury. J Am Col Surg. 2011;212:722–727. doi: 10.1016/j.jamcollsurg.2010.12.016. [DOI] [PubMed] [Google Scholar]
- 29.Weygandt PL, Losonczy LI, Schneider EB, Kisat MT, Licatino LK, Cornwell EE, Haut ER, Efron DT, Haider AH. Disparities in mortality after blunt injury: Does insurance type matter? J Surg Research. 2012;177:288–294. doi: 10.1016/j.jss.2012.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Haas JS, Goldman L. Acutely injured patients with trauma in Massachusetts: differences in care and mortality, by insurance status. Am J Public Health. 1994;84(10):1605–8. doi: 10.2105/ajph.84.10.1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.National Trauma Databank, American College of Suregons. [internet] National Trauma Databank Annual Report. 2012 cited 2014 July 28 Available from: http://www.facs.org/trauma/ntdb/pdf/ntdb-annual-report-2012.pdf.
- 32.Haider AH, Saleem T, Leow JJ, Villegas CV, Kisat M, Schneider EB, Haut ER, Stevens KA, Cornwell EE, MacKenzie EJ, Efron DT. Influence of the National Trauma Data Bank on the study of trauma outcomes: is it time to set research best practices to further enhance its impact? J Am Col Surg. 2012;214:756–768. doi: 10.1016/j.jamcollsurg.2011.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kirzinger WK, Cohen RA, Gindi RM. Trends in insurance coverage and source of private coverage among young adults aged 19-25: United States, 2008-2012. NCHS Data Brief. 2013;137:1–8. [PubMed] [Google Scholar]
- 34.Baker SP, O'Neill B. The Injury Severity Score: An Update. J Trauma. 1976;16:882. doi: 10.1097/00005373-197611000-00006. [DOI] [PubMed] [Google Scholar]
- 35.Champion HR, Sacco WJ, Copes WS, Gann DS, Gennarelli TA, Flanagan ME. A Revision of the Trauma Score. J Trauma. 1989;29:623. doi: 10.1097/00005373-198905000-00017. [DOI] [PubMed] [Google Scholar]
- 36.Vettukattil AS, Haider AH, Haut ER, et al. Do Trauma Safety-Net Hospitals Deliver Truly Safe Trauma Care? A Multilevel Analysis of the National Trauma Data Bank. J Trauma. 2011;70:978–984. doi: 10.1097/TA.0b013e31820b5d0c. [DOI] [PubMed] [Google Scholar]
- 37.Haider AH, Hashmi ZG, Gupta S, Zafar SN, David J, Efron DT, Stevens KA, Zafar H, Schneider EB, Voiglio E, Coimbra R, Haut ER. Benchmarking of Trauma Care Worldwide: The Potential Value of an International Trauma Data Bank (ITDB) World J Surg. 2014;38:1882–91. doi: 10.1007/s00268-014-2629-5. [DOI] [PubMed] [Google Scholar]
- 38.Haider AH, Ong'uti S, Efron DT, Oyetunji TA, Crandall ML, Scott VK, Haut ER, Schneider EB, Powe NR, Cooper LA, Cornwell EE. Association between hospitals caring for a disproportionately high percentage of minority trauma patients and increased mortality: a nationwide analysis of 434 hospitals. Arch Surg. 2012;147:63–70. doi: 10.1001/archsurg.2011.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.The Henry J. Kaiser Family Foundation [internet] Status of State Action on the Medicaid Expansion Decision. 2014 cited 2014 July 28 Available from: http://kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act/
- 40.Clemans-Cope L, Kenney GM, Buettgens M, Carroll C, Blavin F. The Affordable Care Act's coverage expansions will reduce differences in uninsurance rates by race and ethnicity. Health Aff (Millwood) 312012:920–930. doi: 10.1377/hlthaff.2011.1086. [DOI] [PubMed] [Google Scholar]
- 41.Sommers BD, Baicker K, Epstein AM. Mortality and Access to Care among Adults after State Medicaid Expansions. N Engl J Med. 2012;367(11):1025–34. doi: 10.1056/NEJMsa1202099. [DOI] [PubMed] [Google Scholar]
- 42.Baicker K, Taubman SL, Allen HL, Bernstein M, Gruber JH, Newhouse JP, Schneider EC, Wright BJ, Zaslavsky AM, Finkelstein AN. The Oregon Experiment — Effects of Medicaid on Clinical Outcomes. N Engl J Med. 2013;368:1713–1722. doi: 10.1056/NEJMsa1212321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sommers BD, Long SK, Baicker K. Changes in Mortality After Massachusetts Health Care Reform. Ann Intern Med. 2014;160:585–593. doi: 10.7326/M13-2275. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


