Abstract
Purpose
The purpose of this research study was to gain a greater understanding of adolescent’s experiences living with diabetes, and to build a theoretical paradigm to inform interventional design.
Methods
Classical grounded theory was utilized; fifteen in-depth interviews of eleven subjects were conducted with Caucasian adolescents’ ages 11 to 15 with Type 1 diabetes. Interviews were recorded and transcribed verbatim. Data was analyzed using constant comparative analysis. Codes were linked to create the paradigm.
Results
A theoretical model was developed about the concept of “normalizing.” Normalizing is defined as the ability of the adolescents to integrate diabetes into the background of their daily life by creating routines to make diabetes ‘part of me.’ Codes identified in normalizing included: a) ‘recognizing life is changing’; b) ‘taking action to prevent a crisis’; c) ‘disclosing to engage support’; d) ‘taking on the burden of care’; e) ‘accepting the ‘new normal’; and f) ‘hoping for a normal future’.
Conclusions
Normal developmental tasks of adolescence were closely related and contribute to understanding why adolescents struggle with diabetes. These research findings place a different and positive perspective on diabetes management; the focus shifts to supporting wellness and maintaining a normal life rather than on illness. Findings are expected to be of value to health providers working with adolescents with Type 1 diabetes, parents, nursing researchers, and adolescents facing the challenge of diabetes management.
Introduction
Type 1 diabetes mellitus (T1DM) is the most common chronic illness in children.1 Approximately 1 in every 400–600 children (approx. 186,300) in the United States (US) under age 20 have T1DM.2 Complications from diabetes include nephropathy, neuropathy, retinopathy, cardiovascular disease, and amputations, and are the 7th leading cause of death in the US,2 however, maintaining glucose levels near normal decreases risk.3 Diabetes is a complex, multifaceted disease affecting the health and emotional well-being of adolescents trying to cope with multiple daily insulin administration, blood glucose monitoring (BGM), dietary and exercise changes.4 Many studies have examined issues in adolescent diabetes management,5–9 with limited progress helping adolescent’s effectively manage their diabetes.
A significant reduction in BGM occurs during late childhood with 39% testing 4 times daily, while during early adolescence only 10% are testing 4 times.5 Decreased BGM is associated with poor glucose control and higher hemoglobin A1C (A1C) levels.5, 10–11 Less than 1/3 of adolescents maintain target A1C levels for their age.12 Adolescents with poor glucose control have increased hospitalizations for life threatening diabetic ketoacidosis (DKA) than adolescents with good glucose control.10 Persistent high blood glucose (BG) with poor adherence to diet, exercise, BGM, and insulin administration lasts into adulthood13 for many with T1DM suggesting difficulty with diabetes self-management is long lasting. Only 1/3 of adults with T1DM are able to maintain A1C levels <7.5% with >12% having very poor control of their diabetes with A1C >10%.14
Poor adherence to dietary changes15 and a decrease in exercise necessary to maintain normal BG levels are common during adolescence.16 Psychological issues experienced by adolescents with diabetes include anxiety,17 depression,18 poor self-esteem,19 problems with coping,20 and struggles with peer and parental relationships.21 Anxiety, depression, and poor coping behaviors are more common in adolescents with diabetes than their peers.20 Adolescents also do poorly in school.22
Having diabetes is challenging during the already difficult adolescent years and adds additional burden.23 During this transition to adulthood, adolescents increase diabetes self-care while gaining independence from their parents.24 Problem solving skills,25 independence,26 and autonomy27 are important features of adolescent development posing challenges as they attempt to incorporate diabetes self-management.
With independence comes an increase in parent-child conflict that is detrimental to care,8 and is associated with a lower frequency of BGM and higher A1C levels.8 Parental and peer support28 are helpful in monitoring BG and maintaining lower A1C levels.5 While it is not clear if conflict is the cause of decreased parental monitoring during adolescence, parental involvement improves short term BG control and quality of life,5 yet is not viewed as helpful by many adolescents.29
A meta-analysis of 15 randomized controlled trials to improve adherence to the diabetes treatment regimen30 was done. A total of 997 participants were included with a mean effect size of 0.11 for pre to post treatment change comparing the intervention groups to controls. Interventions including psychosocial and behavioral strategies were most effective. Grey31 studied the effect of coping skills training with 77 adolescents and found decreases in A1C levels in both the intervention and control group. Damiao & Pinto32 conducted a grounded theory study in 7 adolescents addressing their experiences of living with T1DM and found 3 themes: a) what it was like to be diagnosed with diabetes, b) being transformed by diabetes, and c) having a prickly life. These studies explored adolescent diabetes management; however, no studies have shown long term improvement in A1C levels or self-management. Limited research has been completed from the adolescents’ perspective on improving self-management to control BG.
Developing an understanding from the adolescent’s perspective of how they manage diabetes and control their BG led to utilizing grounded theory as the methodology for this study. The process of theory development utilizing grounded theory is based on interviews with adolescent’s using gerund coding to seek the conditions when adolescent’s employ behaviors where they engage in self-management of their diabetes. Grounded theory as a qualitative method is unique in the rigorous data analysis grounded directly in the subjects’ words that includes conceptual definitions and an understanding of the relationships between and within categories. The theory developed with the grounded theory research process is then foundational work derived directly from adolescent experiences that enhances understanding of how adolescent’s manage their diabetes and promotes use of this theory as a guide for future research that will potentially lead to more successful interventions in this population.
Type 1 diabetes is prevalent, costly, influences quality of life, school, relationships and ultimately long term survival; is difficult to manage and difficulties persist into adulthood. Adolescents struggle to manage diabetes and maintain BG control as they become independent. There is a gap in understanding why adolescents with diabetes decrease BGM, giving insulin, and managing their diet and exercise. Understanding the experience of having T1DM from the perspective of the adolescent is needed to build a theoretical model and generate hypotheses to design future interventions. The purpose of this research was to gain a greater understanding of adolescent’s (ages 11–15 years) perspectives of their experiences living with diabetes; associated challenges and management issues.
Methods
Study design
Grounded theory,33 a qualitative method, was selected because it provides a greater understanding of conditions under which behaviors occur and supports the creation of a theoretical paradigm and related hypothesis.33–34 The focus of developing this theory using this methodology is to understand the social processes that occur that help to predict, explain and describe behaviors.33–34 A key feature of grounded theory is understanding the process, the structure and the interactions that occur in the social setting.33–34 Symbolic interactionism is the theoretical framework for grounded theory.35 Symbolic interaction is based on how the person is able to view themselves based on others in their world and the person’s perception on how they view their reality as they interact with others in their world.35
Study questions
The initial study questions included: 1) Let’s discuss your experiences of living with diabetes. 2) Let’s talk about taking care of or managing your diabetes. Can you tell me about that? Probes included: a) What is it like for you to take care of your diabetes? b) Tell me about taking your insulin and testing your BG. c) What do you do to keep your BG balanced? d) What, if any, challenges have you experienced. Subsequent interviews started with these questions and additional questions were added to saturate emerging codes and included: a) When you heard you had the diagnosis of diabetes, tell me about that time. b) Talk about transitioning to self-care, and c) Some people talk about coming to a place that says “I can take care of my diabetes,” tell me about that.
Study sample
The sample consisted of early adolescent’s ages 11 to 15. Inclusion criteria determined by parent report included participants who: 1) had T1DM using insulin; 2) diagnosed six months or more; 3) were able to read and speak English; and 4) identified as Caucasian. Exclusion criteria by parental report included: 1) no other diagnosed medical or psychological conditions except controlled hypothyroidism; 2) no clinic provider visit with this researcher during the past year; and 3) emotional or mental disabilities that would prevent them from providing an interview.
Recruitment and sampling
Recruitment was done using posters, handouts at clinic, and a mailed letter. Interested parents contacted the researcher to participate in the study. A verbal questionnaire with the parent determined eligibility. Participants received a $25 gift card.
Interviewing process
Three interviews were done with purposeful sampling choosing subjects who met study criteria and varied by sex and age, to provide the anchor interviews and identify initial codes. Additional interviews were conducted using theoretical sampling which sought subjects able to provide detailed information about the growing theory, add additional codes, and to eventually saturate the data. Interviews were digitally recorded and lasted approximately 60 minutes. Recordings were transcribed verbatim and reviewed for accuracy. Sampling, coding, and analysis were done simultaneously. Each interview was transcribed, coded and analyzed and integrated into the theory prior to the next interview being conducted. Data was hand analyzed creating code cards described below. After three to five interviews the framework of major codes and categories was identified. Additional interviews were completed totaling fifteen interviews to reach data saturation. Data saturation was reached when no new information was obtained, the categories were well defined and relationships between categories understood, and the social process was clearly understood.36–37 Formal interviews and one focus group were conducted.
Data analysis
The first step in grounded theory data analysis was to engage in “first line,” or “open ended” coding. Three initial interviews were coded using a gerund coding process (-ing words) looking for behaviors that were occurring. Code cards included: a) the gerund code; b) quotes with the code from the data; c) code definition; d) conditions when the code occurred or not; and e) hunches about relationships among codes. The second step was “second line”, or theoretical coding, where code groupings were clustered. Additional interviews used the full interview guide and the last four interviews used specific probes. Sampling continued until categories were saturated with a clear understanding of relationships between categories, and the social process was fully defined.36–37 In the third step “constant comparative analysis” or “axial coding” emerging codes and categories were compared to those already identified to understand category relationships, and identify the core phenomenon. In the fourth step codes were linked to create the paradigm. During the fifth step the theory was delimited setting aside codes not a major part of the story. The final paradigm fully describes the codes, their relationships, the moving processes, defines the major task of the participants, and hypotheses about conditions.
Assessing Rigor in Grounded Theory
In a qualitative study it is important to assess for rigor of the study, but it needs to be done in different ways than quantitative research assessing validity and reliability. This study followed criteria described by Chiovitti and Piran describing ways to address rigor through credibility, fittingness, and auditability.38 To address credibility the actual words of the participants were used to build the theory and a journal was kept that documented the thoughts of the researcher’s personal views, codes were discussed with some adolescents during interviews and in a focus group on how the findings reflected their experiences and for feedback on the paradigm. To address auditability the researcher kept a detailed journal and used memo writing describing how categories were developed and how participants were chosen with sufficient detail that would allow another researcher to replicate the research process.38–39 To address fittingness the researcher clearly described the sample and their characteristics, the level of theory, and linked existing research through a secondary literature review to categories of the theory.
Human subjects
IRB approval was also obtained from the study site and the University of Washington. Consents were signed by the parent. Assents were signed by the adolescent’s for study participation.
Results
The study sample consisted of adolescents (three boys (27.3%) and eight girls (72.7%) ages 11 to 15 (mean = 13.9), who identified as Caucasian and had T1DM from western Washington state. Both parents and adolescents read and spoke English. Diabetes care had not been provided by the researcher during the past year. No adolescents were in special education at school or were diagnosed or under treatment for a mental health condition during the past year. Participants had an average parent reported A1C of 8.2% (range 7.2% – 9.2%, median 8.4).
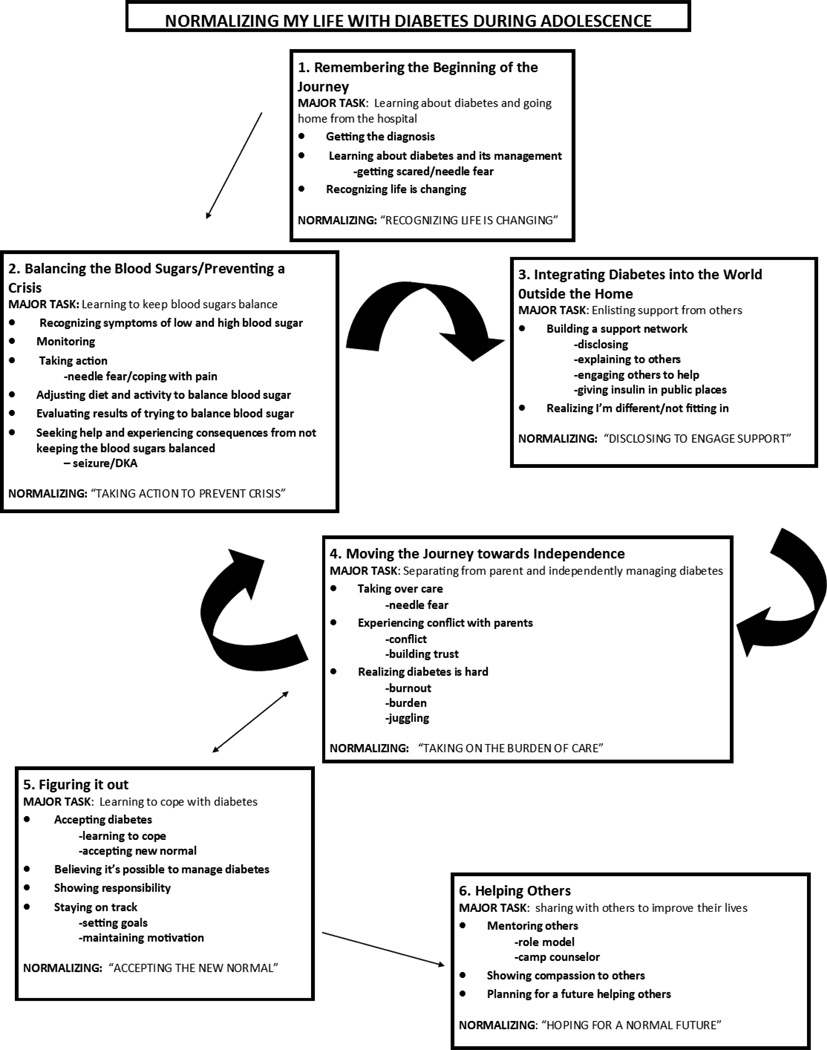
The substantive theory developed was about normalizing, the process of how adolescents with T1DM normalized their life while transitioning to independence. The theoretical findings are found in the model of ‘normalizing my life with diabetes during adolescence’ (see Figure 1). The six major axial codes (or phases) are the actions adolescents took to manage their diabetes. These phases are: remembering the journey, balancing blood sugar/preventing a crisis, integrating diabetes into the world outside the home, moving the journey towards independence, figuring it out and helping others.
Figure 1.
Normalizing my life with diabetes during adolescence. A summary of operational codes, and conceptual codes of the model.
Phase 1
Remembering the Beginning of the Journey was defined as the memories of the events that occurred when adolescents were first diagnosed with diabetes. Sub-codes include: 1) getting the diagnosis, 2) learning about diabetes and its management, and 3) recognizing my life is changing.
Getting the Diagnosis was defined as the point when adolescents recognized that something was wrong, sought medical care, and were first told about their condition.
Learning about Diabetes and its Management was defined as the process necessary to understand the medical condition of diabetes and how you need to manage it.
Recognizing My Life Is Changing was defined as realizing that diabetes is a life changing event that is permanent with no possibility of a cure.
“everyone just had to change their lives and adapt to it (diabetes) even though there is more drastic things out there- diseases that people had to adapt to but to me this is drastic because it is never going to go away I mean I am going to have it I mean they might find a cure after I die and I pray that they do but for my time being there probably won’t be anything found” Interview #7 p.7
The normalizing task during this phase was “recognizing my life is changing”.
Phase 2
Balancing Blood Sugars/Preventing a Crisis was defined as keeping the blood sugar in a target range that does not cause problems from either high or low blood sugars and prevents experiencing a crisis that could lead to hospitalization or a seizure. Sub-codes included: 1) recognizing symptoms of low and high blood sugar, 2) monitoring, 3) taking action, 4) adjusting diet and activity to balance blood sugars, 5) evaluating results from trying to balance blood sugars, and 6) seeking help and experiencing consequences from not keeping the blood sugars balanced.
Monitoring was done to validate symptoms, to keep bloods sugar balanced and avoid a crisis. Testing Blood Sugars is a sub-code and was associated with negative feelings such as fear, and it is also described as being annoying.
“It has been annoying, um, ‘cuz like anytime I have to eat I have to check my blood sugar and then do this whole process …and that is kind of a pain” Interview #1 p. 1
The normalizing task during this phase was “taking action to prevent crisis”.
Phase 3
Integrating Diabetes into the World Outside the Home was defined as those actions taken to address diabetes management outside the home such as managing the diet, giving insulin, and engaging in physical activity. Sub-codes included: a) building support and b) realizing I’m different.
Building Support was undertaken for the purpose of gaining greater independence from parents and integrating diabetes into normal activities outside the home
Realizing I’m Different was defined as feeling “different” or “not normal” or like you do not “fit in” or have friends.
“at the beginning it’s kind of like you know you are different you know, you are not going to be like everyone else so it’s not one of those things I didn’t really like about myself, it’s not like I’m not perfect I guess is how you want to put it and it was kind of hard to get used to” Interview #4 p.2
The normalizing task during this phase was “disclosing to engage support”.
Phase 4
Moving the Journey Towards Independence was defined as the ability of the adolescents to successfully transition to independence by taking on primary responsibility for their diabetes management tasks. Sub-codes include: 1) taking over care, 2) experiencing conflict with parents, and 3) realizing diabetes is hard.
Taking over care was defined as the adolescents wanting to independently manage their diabetes. One of the challenges in taking over care from the parent was the willingness of the parent to let go of the care and for the parent to not transition before the adolescent is ready.
Experiencing Conflict with parents was defined as the parent and adolescents not agreeing on diabetes management or arguing over care being done.
Realizing diabetes is hard was defined as struggling to manage diabetes independently all day every day, not having blood sugars respond as expected, and the emotional burden of having diabetes and just wanting to give up.
“Sometimes it is kind of hard, you just have those days where like it seems like everything is harder than it really is, when you are young and when you have those days, basically when you have diabetes it’s like you just want to give up” Interview #4 p. 13
The normalizing task during this phase was “taking on the burden of care”. Phases 2, 3, and 4 were cyclical, and adolescents reverted back and forth through them before finally reaching phase 5; but often transitioned back to phase 2 through 4 several times before moving forward permanently.
Phase 5
Figuring It Out was defined as the ability to come to the realization that you can manage your diabetes and maintain your glucose control, being able to accept diabetes and stay on track. The adolescents experienced a shift in their mental framework that helped them understand that diabetes is a part of who they are, accepting and realizing their life with diabetes is their ‘new normal’. Sub-codes included: 1) accepting diabetes, 2) believing it’s possible to manage diabetes, 3) showing responsibility, and 4) staying on track.
Accepting Diabetes was defined as developing an understanding that diabetes is part of you and that having diabetes is normal.
“It (diabetes) is there, it will never go, but it is just how much you let it get to you is just the key to it, it never goes away it is always a part of you, until you just accept it, it is always just there” Interview #6 p. 16–17
Believing it’s possible to manage diabetes was defined as the ability to have the confidence to know how to manage your diabetes, in your decision making skills, and in your desire to control your diabetes successfully.
Showing responsibility was defined as the mental ability to see the consequences of their actions and understand why being responsible is important.
“if you’re older you are more responsible, you are more mature you don’t have hormones messing with you … you don’t have as much rebellion” Interview #6 p. 1
Staying on track was defined as learning to manage diabetes in a physically and emotionally healthy way.
The normalizing task during this phase was “accepting the new normal”.
Phase 6
Helping Others was defined as providing information, assistance, and compassion to those around them to improve their future. Sub -codes included: 1) mentoring others, 2) showing compassion to others, and 3) planning for a future helping others.
“actually growing up with diabetes I have actually been able to help some people too” Interview #4 p. 1
Mentoring others was defined as giving back to others through education, motivation, and role modeling to help younger children with diabetes cope and adjust to their illness.
Showing Compassion for Others was defined as the ability to understand other’s feelings and make a connection with them.
Planning for a Future Helping Others was defined as seeking career goals in life allowing one to help others.
“I’ve always kind of had a goal of going into the medical field but now I think now one of my biggest goals is to just either be a researcher or be an endocrinologist because I see what she has done for me and how much she has helped me and I want to be able to do that for other people” Interview #10 p. 15
The normalizing task during this phase was “hoping for a normal future”.
Some of the conditions when the adolescent was or was not able to proceed through these phases included the adolescent’s emotional response to getting a diabetes diagnosis, experiencing needle fear, not wanting to care for self in front of others, not fitting in with peers, feeling self-conscious or embarrassed, conflict with parents, reactions from parents affect adjustment, and rebellion and laziness do not lead to success. Key hypothesis from this paradigm of normalizing include: a) the pain and annoyance of testing BG hinders adolescents from consistently performing this task, strategies for decreasing needle fear will be beneficial; b) remembering to test and log BG is challenging for adolescents so finding creative ways for success utilizing today’s technology will be useful; c) helping the adolescent and parent work through the transition process together will decrease conflict and improve care; d) reactions and interactions of friends, teachers, and others enhance feelings of embarrassment and how adolescents view themselves as normal; thus interventions with friends and teachers in understanding diabetes, will help support adolescents; e) utilizing insulin pump therapy decreases the need for extra injections for snacks and meals and enhances adolescents ability to feel normal, thus working with insurance companies in allowing use of technology is important.
These six phases of normalizing provide an important level of understanding adolescents with Type 1 diabetes and challenges they face as they strive for independence with diabetes care. Supporting adolescents address these tasks to achieve normalcy in their life will assist with successful self-management. Adolescents often get mired in the emotions and complexity of diabetes management during phases 2 through 4 making it difficult to transition to phase 5. As they make diabetes part of them and ‘figure it out’ they learn to manage diabetes successfully.
Conclusions
The major task adolescents were addressing in this study was “normalizing”. Included with normalizing was integrating diabetes as ‘part of me’, while monitoring blood glucose, giving insulin, and monitoring diet and activity to feel diabetes is manageable and that they are in control. This also included an attitude of acceptance and the ability to cope, thus allowing them to independently manage their diabetes.
A major hypothesis was that helping adolescents normalize their lives while managing the tasks of diabetes during adolescence will lead to a decrease in A1C’s, in hospitalizations from DKA, and an increased ability to cope with diabetes. Based on the findings from this study it is important to note that: a) needle fear is a significant and ongoing major issue in allowing adolescents to normalize their experience and independently manage their care; b) the manner in which transition happens is a major part of how adolescents are able to normalize their life during puberty; c) conflict between the parent and adolescent is a significant deterrent and social support is a significant positive factor in the smooth transition to independent management; and d) the ability of the parent to ‘let go’ of monitoring the adolescent during puberty significantly influences the adolescent’s ability to normalize.
The conceptual codes for normalizing in adolescents with diabetes are closely related to normal adolescent developmental tasks26, 40: a) ‘recognizing life is changing’ fits with coping with loss; b) ‘taking action to prevent a crisis’ fits with being interested in present with little thought for the future and concrete thinking; c) ‘disclosing to engage support’ fits with struggling with body image, wanting privacy and wanting to be normal; d) ‘taking on the burden of care’ fits with wanting independence, having more conflict with parents and rule and limit testing; e) ‘accepting the ‘new normal’ fits with abstract thinking and the ability to set goals; and f) ‘hoping for a normal future’ fits with an increased sense of identity and concern for others. These adolescent developmental tasks help explain why adolescents struggle with diabetes. These tasks are critical in understanding the adolescent’s actions during adolescence and their ability to manage BG appropriately while they try to ‘be normal’ and ‘fit in’ with their friends.
Normalizing has been described in the literature in a variety of settings often as a term, not related to a process. Strauss41 described preventing a crisis, maintain a regimen, feelings of isolation, illness as a burden and attempts to normalize their life that are similar to several normalizing tasks adolescents experience. Parents normalize chronic illness by acknowledging the change in their lifestyle,42 focusing on day to day tasks,43 and living a difficult life.44 This research provides an understanding of the concept of normalizing for adolescents with T1DM not previously described in the literature. These important findings will lead to the development of interventions to support adolescents in normalizing their life with diabetes.
This paradigm on normalizing for the adolescent with diabetes is a novel contribution that increases understanding about their experiences during transition to self-care. Linking the phases of normalizing with developmental tasks allows researchers a different perspective on adolescent transition to create new interventions utilizing this model. Previous intervention work has not focused on the transition process, helping the parents in this process, the developmental aspects of the adolescent, or from a framework that understands that the adolescent is trying to ‘be normal’ and ‘fit in’. Designing interventions at multiple levels are more likely to achieve success in normalizing and achieving good glucose control with positive outcomes.
Future Directions
The following are recommendations for future research: Adolescent: a) The design of interventions to decrease needle fear, and to enhance the ability of adolescents to safely achieve independence; and b) the exploration of phone apps to help adolescents remember and log their blood sugars in a device they are already carrying. Parent: The design of interventions on transition of care to enhance supportive parental behaviors. Peers: The design of interventions in the school and community enhancing supportive attitudes among students, families, and friends. System Changes: Engaging policy makers, funding agencies and health insurance companies to increase adolescents’ use of today’s new technologies to manage their diabetes.
This study has provided a framework for normalizing in adolescents with T1DM and chronic illness management. Multiple hypotheses were created providing opportunities for further research in assisting adolescents with diabetes self-management emphasizing wellness and normal growth and development. Focusing research on novel ways to help adolescents normalize their life may assist in achieving success in adolescent diabetes management.
Recommendations
Interventions by the diabetes educator or providers need to be directed toward meeting the adolescent and parental needs, as well as school system educators, psychologists, counselors, and administration. Interventions need to include both individual and group education, as well as advocacy efforts to influence change in systems and structures. The following are recommendations for working with A. Adolescents: 1) Assessing and addressing emotional state through program development or referral to facilitate ‘accepting the new normal’. 2) Developing teaching methods that facilitate coping with loss and ‘recognizing life is changing’. 3) Assessing and addressing needle fear with a coherent plan. 4) Developing a plan for sick day that encourages seeking assistance to ‘take action to prevent a crisis’. B. Parents: 1) Assessing parental emotional responses to diagnosis and interactions, referring for counseling, or developing individual plans or educational program to help them understand how their responses affect their child. 2) Developing programs assisting parents in providing emotional support to decrease ‘taking on the burden of care’. 3) Developing programs to assist parents in healthy transition of care with decreased nagging. C. School/Community: 1) Develop outreach programs or information to increase knowledge, supportive behaviors, and allowing for ‘disclosing to engage support’. D. System/Policy Change: 1) Advocating for funding and approval of technologies and therapies that enhance the ability to ‘hope for a normal future’.
Acknowledgments
This work was supported through the Warren G. Magnuson, the Hester McLaws, the Gladys N. Stevenson, the Joyce Carr, and the Hahn Scholarships and from NNCRR Grant TL1 RR 025016. Blinded interview data and journals are available from lead author upon request.
Contributor Information
Elizabeth Babler, Email: babler@uwm.edu, University of Wisconsin – Milwaukee, College of Nursing, Cunningham Hall, Office 475, P.O. Box 413, Milwaukee, WI, USA 53201-0413, Phone: 1-360-620-2268, Fax: 1- 414-229-6474.
C. June Strickland, University of Washington School of Nursing, Psychosocial & Community Health, Box 357263, Seattle, WA, USA 98195-7263, Phone: 425-747-7268, Fax: 206-685-9551.
References
- 1.CDC. Center for Disease Control. [accessed 2010]; http://wwwcdcgov/diabetes/statistics/hosp/kidtable2htm.
- 2.ADA. American Diabetes Association. [Accessed 2010]; http://wwwdiabetesorg/diabetes-basics/type-1/. [Google Scholar]
- 3.DCCT. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. The Diabetes Control and Complications Trial Research Group. N Engl J Med. 1993;329(14):977–986. doi: 10.1056/NEJM199309303291401. Epub 1993/09/30. PubMed PMID: 8366922. [DOI] [PubMed] [Google Scholar]
- 4.Silverstein J, Klingensmith G, Copeland K, et al. Care of children and adolescents with type 1 diabetes: a statement of the American Diabetes Association. Diabetes Care. 2005;28(1):186–212. doi: 10.2337/diacare.28.1.186. Epub 2004/12/24. doi: 28/1/186 [pii]. PubMed PMID: 15616254. [DOI] [PubMed] [Google Scholar]
- 5.Anderson B, Ho J, Brackett J, Finkelstein D, Laffel L. Parental involvement in diabetes management tasks: relationships to blood glucose monitoring adherence and metabolic control in young adolescents with insulin-dependent diabetes mellitus. J Pediatr. 1997;130(2):257–265. doi: 10.1016/s0022-3476(97)70352-4. Epub 1997/02/01. doi: S0022-3476(97)70352-4 [pii]. PubMed PMID: 9042129. [DOI] [PubMed] [Google Scholar]
- 6.Evans JM, Newton RW, Ruta DA, MacDonald TM, Stevenson RJ, Morris AD. Frequency of blood glucose monitoring in relation to glycaemic control: observational study with diabetes database. BMJ. 1999;319(7202):83–86. doi: 10.1136/bmj.319.7202.83. PubMed PMID: 10398627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Levine BS, Anderson BJ, Butler DA, Antisdel JE, Brackett J, Laffel LM. Predictors of glycemic control and short-term adverse outcomes in youth with type 1 diabetes. J Pediatr. 2001;139(2):197–203. doi: 10.1067/mpd.2001.116283. Epub 2001/08/07. doi: S0022-3476(01)75473-X [pii] 10.1067/mpd.2001.116283 [doi]. PubMed PMID: 11487743. [DOI] [PubMed] [Google Scholar]
- 8.Anderson BJ, Vangsness L, Connell A, Butler D, Goebel-Fabbri A, Laffel LM. Family conflict, adherence, and glycaemic control in youth with short duration Type 1 diabetes. Diabet Med. 2002;19(8):635–642. doi: 10.1046/j.1464-5491.2002.00752.x. Epub 2002/07/31. doi: 752 [pii]. PubMed PMID: 12147143. [DOI] [PubMed] [Google Scholar]
- 9.Kyngas H, Barlow J. Diabetes: an adolescent's perspective. J Adv Nurs. 1995;22(5):941–947. doi: 10.1111/j.1365-2648.1995.tb02646.x. Epub 1995/11/01. PubMed PMID: 8568069. [DOI] [PubMed] [Google Scholar]
- 10.Ziegler R, Heidtmann B, Hilgard D, Hofer S, Rosenbauer J, Holl R. Frequency of SMBG correlates with A1C and acute complications in children and adolescents with type 1 diabetes. Pediatr Diabetes. 2010 doi: 10.1111/j.1399-5448.2010.00650.x. Epub 2010/03/27. doi: PDI650 [pii] 10.1111/j.1399-5448.2010.00650.x [doi]. PubMed PMID: 20337978. [DOI] [PubMed] [Google Scholar]
- 11.Ingerski LM, Anderson BJ, Dolan LM, Hood KK. Blood glucose monitoring and glycemic control in adolescence: contribution of diabetes-specific responsibility and family conflict. J Adolesc Health. 2010;47(2):191–197. doi: 10.1016/j.jadohealth.2010.01.012. Epub 2010/07/20. doi: S1054-139X(10)00035-2 [pii] 0.1016/j.jadohealth.2010.01.012 [doi]. PubMed PMID: 20638012; PubMed Central PMCID: PMC2907244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hoey H. Psychosocial factors are associated with metabolic control in adolescents: research from the Hvidoere Study Group on Childhood Diabetes. Pediatr Diabetes. 2009;10(Suppl 13):9–14. doi: 10.1111/j.1399-5448.2009.00609.x. Epub 2009/11/26. doi: PDI609 [pii] 10.1111/j.1399-5448.2009.00609.x [doi]. PubMed PMID: 19930221. [DOI] [PubMed] [Google Scholar]
- 13.Moreland EC, Volkening LK, Lawlor MT, Chalmers KA, Anderson BJ, Laffel LM. Use of a blood glucose monitoring manual to enhance monitoring adherence in adults with diabetes: a randomized controlled trial. Arch Intern Med. 2006;166(6):689–695. doi: 10.1001/archinte.166.6.689. Epub 2006/03/29. doi: 166/6/689 [pii] 10.1001/archinte.166.6.689 [doi]. PubMed PMID: 16567610. [DOI] [PubMed] [Google Scholar]
- 14.Toljamo M, Hentinen M. Adherence to self-care and glycaemic control among people with insulin-dependent diabetes mellitus. J Adv Nurs. 2001;34(6):780–786. doi: 10.1046/j.1365-2648.2001.01808.x. Epub 2001/06/26. doi: jan1808 [pii]. PubMed PMID: 11422548. [DOI] [PubMed] [Google Scholar]
- 15.Mayer-Davis EJ, Nichols M, Liese AD, et al. Dietary intake among youth with diabetes: the SEARCH for Diabetes in Youth Study. J Am Diet Assoc. 2006;106(5):689–697. doi: 10.1016/j.jada.2006.02.002. Epub 2006/05/02. doi: S0002-8223(06)00139-8 [pii] 10.1016/j.jada.2006.02.002 [doi]. PubMed PMID: 16647326. [DOI] [PubMed] [Google Scholar]
- 16.Schweiger B, Klingensmith G, Snell-Bergeon JK. Physical activity in adolescent females with type 1 diabetes. ACTA Paediatrica. 2010;2010:328318. doi: 10.1155/2010/328318. Epub 2010/07/24. doi: 10.1155/2010/328318 [doi]. PubMed PMID: 20652080; PubMed Central PMCID: PMC2905719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kovacs M, Goldston D, Obrosky DS, Bonar LK. Psychiatric disorders in youths with IDDM: rates and risk factors. Diabetes Care. 1997;20(1):36–44. doi: 10.2337/diacare.20.1.36. Epub 1997/01/01. PubMed PMID: 9028691. [DOI] [PubMed] [Google Scholar]
- 18.Grey M, Whittemore R, Tamborlane W. Depression in type 1 diabetes in children: natural history and correlates. J Psychosom Res. 2002;53(4):907–911. doi: 10.1016/s0022-3999(02)00312-4. Epub 2002/10/16. doi: S0022399902003124 [pii]. PubMed PMID: 12377302. [DOI] [PubMed] [Google Scholar]
- 19.Helgeson VS, Snyder PR, Escobar O, Siminerio L, Becker D. Comparison of Adolescents with and without Diabetes on Indices of Psychosocial Functioning for Three Years. J Pediatr Psychol. 2007;32(7):794–806. doi: 10.1093/jpepsy/jsm020. [DOI] [PubMed] [Google Scholar]
- 20.Grey M, Cameron ME, Thurber FW. Coping and adaptation in children with diabetes. Nurs Res. 1991;40(3):144–149. Epub 1991/05/01. PubMed PMID: 2030992. [PubMed] [Google Scholar]
- 21.Davidson M, Penney ED, Muller B, Grey M. Stressors and self-care challenges faced by adolescents living with type 1 diabetes. Appl Nurs Res. 2004;17(2):72–80. doi: 10.1016/j.apnr.2004.02.006. Epub 2004/05/22. doi: S0897189704000266 [pii]. PubMed PMID: 15154119. [DOI] [PubMed] [Google Scholar]
- 22.Northam EA, Lin A, Finch S, Werther GA, Cameron FJ. Psychosocial well-being and functional outcomes in youth with type 1 diabetes 12 years after disease onset. Diabetes Care. 2010;33(7):1430–1437. doi: 10.2337/dc09-2232. Epub 2010/04/02. doi: dc09-2232 [pii] 10.2337/dc09-2232 [doi]. PubMed PMID: 20357379; PubMed Central PMCID: PMC2890334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hood KK, Huestis S, Maher A, Butler D, Volkening L, Laffel LM. Depressive symptoms in children and adolescents with type 1 diabetes: association with diabetes-specific characteristics. Diabetes Care. 2006;29(6):1389–1391. doi: 10.2337/dc06-0087. Epub 2006/05/30. doi: 29/6/1389 [pii] 10.2337/dc06-0087 [doi]. PubMed PMID: 16732028. [DOI] [PubMed] [Google Scholar]
- 24.Cunningham NR, Vesco AT, Dolan LM, Hood KK. From Caregiver Psychological Distress to Adolescent Glycemic Control: The Mediating Role of Perceived Burden around Diabetes Management. J Pediatr Psychol. 2010 doi: 10.1093/jpepsy/jsq071. Epub 2010/08/26. doi: jsq071 [pii] 10.1093/jpepsy/jsq071 [doi]. PubMed PMID: 20736389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McCaul KD, Glascow RD, Schafer LC. Diabetes Regimen Behaviors. Predicting Adherence. Med Care. 1987;25(9):868–881. [PubMed] [Google Scholar]
- 26.Neinstein LS. Adolescent health care : a practical guide. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins; 2008. [Google Scholar]
- 27.Wysocki T, Taylor A, Hough BS, Linscheid TR, Yeates KO, Naglieri JA. Deviation from the developmentally approprate self-care autonomy. Association with diabetes outcomes. Diabetes Care. 1996;19:119–125. doi: 10.2337/diacare.19.2.119. [DOI] [PubMed] [Google Scholar]
- 28.Kyngas H, Rissanen M. Support as a crucial predictor of good compliance of adolescents with a chronic disease. J Clin Nurs. 2001;10(6):767–774. doi: 10.1046/j.1365-2702.2001.00538.x. Epub 2002/02/02. PubMed PMID: 11822848. [DOI] [PubMed] [Google Scholar]
- 29.Hanna KM, Juarez B, Lenss SS, Guthrie D. Parent-adolescent communication and support for diabetes management as reported by adolescents with type 1 diabetes. Issues Compr Pediatr Nurs. 2003;26(3):145–158. doi: 10.1080/01460860390223871. Epub 2003/08/26. doi: 10.1080/01460860390223871 [doi]AFA8ATM3YB222XB0 [pii]. PubMed PMID: 12936698. [DOI] [PubMed] [Google Scholar]
- 30.Hood KK, Rohan JM, Peterson CM, Drotar D. Interventions with adherence-promoting components in pediatric type 1 diabetes: meta-analysis of their impact on glycemic control. Diabetes Care. 2010;33(7):1658–1664. doi: 10.2337/dc09-2268. Epub 2010/07/01. doi: dc09-2268 [pii] 10.2337/dc09-2268 [doi]. PubMed PMID: 20587726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Grey M, Boland EA, Davidson M, Li J, Tamborlane WV. Coping skills training for youth with diabetes mellitus has long-lasting effects on metabolic control and quality of life. J Pediatr. 2000;137(1):107–113. doi: 10.1067/mpd.2000.106568. Epub 2000/07/13. doi: S0022-3476(00)61563-9 [pii] 10.1067/mpd.2000.106568 [doi]. PubMed PMID: 10891831. [DOI] [PubMed] [Google Scholar]
- 32.Damiao EB, Pinto CM. "Being transformed by illness": adolescents' diabetes experience. Rev Lat Am Enfermagem. 2007;15(4):568–574. doi: 10.1590/s0104-11692007000400008. Epub 2007/10/10. doi: S0104-11692007000400008 [pii]. PubMed PMID: 17923972. [DOI] [PubMed] [Google Scholar]
- 33.Glaser BG, Strauss AL. The discovery of grounded theory; strategies for qualitative research. Chicago: Aldine Pub. Co.; 1967. [Google Scholar]
- 34.Bowers BJ. Grounded Theory. In: Sarter B, editor. Paths to knowledge: innovative research methods for nursing. New York, NY: National League for Nursing; 1988. pp. 33–59. [Google Scholar]
- 35.Blumer H. Symbolic interactionism; perspective and method. Englewood Cliffs, N.J.: Prentice-Hall; 1969. [Google Scholar]
- 36.Glaser BG. Theoretical sensitivity : advances in the methodology of grounded theory. Mill Valley, Calif.: Sociology Press; 1978. [Google Scholar]
- 37.McCann TV, Clark E. Grounded theory in nursing research: Part 1--Methodology. Nurse Res. 2003;11(2):7–18. doi: 10.7748/nr2004.01.11.2.7.c5918. Epub 2004/01/08. PubMed PMID: 14708425. [DOI] [PubMed] [Google Scholar]
- 38.Chiovitti RF, Piran N. Rigour and grounded theory research. J Adv Nurs. 2003;44(4):427–435. doi: 10.1046/j.0309-2402.2003.02822.x. Epub 2003/12/04. doi: 2822 [pii]. PubMed PMID: 14651715. [DOI] [PubMed] [Google Scholar]
- 39.Lincoln YS, Guba EG. Naturalistic inquiry. Beverly Hills, Calif.: Sage Publications; 1985. [Google Scholar]
- 40.Early Head Start National Research Center (EHSNR) Stages of Adolescent development 2013. [accessed Feb 23, 2013]; Available from: http://www.ehsnrc.org/Publications/English%20Tip%20Sheets/TIP%20SHEET%2034_addendum.pdf. [Google Scholar]
- 41.Strauss AL. Chronic illness and the quality of life. 2nd ed. St. Louis: Mosby; 1984. [Google Scholar]
- 42.Deatrick JA, Knafl KA, Murphy-Moore C. Clarifying the concept of normalization. Image: J Nurs Sch. 1999;31(3):209–214. doi: 10.1111/j.1547-5069.1999.tb00482.x. PubMed PMID: 1999080370. Language: English. Entry Date: 19991201. Revision Date: 20041029. Publication Type: journal article. [DOI] [PubMed] [Google Scholar]
- 43.Peck B, Lillibridge J. Normalization behaviours of rural fathers living with chronically-ill children: An Australian experience. J Child Health Care. 2005;9(1):31–45. doi: 10.1177/1367493505049645. [DOI] [PubMed] [Google Scholar]
- 44.Knafl KA, Darney BG, Gallo AM, Angst DB. Parental perceptions of the outcome and meaning of normalization. Res Nurs Health. 2010;33(2):87–98. doi: 10.1002/nur.20367. [DOI] [PMC free article] [PubMed] [Google Scholar]