Abstract
Objectives
To determine whether ICU readmission is associated with higher severity of illness scores in adult patients.
Background
Readmissions to the intensive care unit (ICU) are associated with increased costs, morbidity, and mortality.
Methods
We performed searches of MEDLINE, EMBASE, and grey literature databases. We selected studies reporting data from adults who were hospitalized in an ICU, received severity of illness scores, and were discharged from the ICU. Characteristics of readmitted and non-readmitted patients were examined.
Results
We screened 4766 publications and included 31 studies in our analysis. In most studies, severity of illness scores were higher in patients readmitted to the ICU. Readmission was also associated with higher mortality and longer ICU and hospital stays. Excessive heterogeneity precluded the reporting of results in the form of a meta-analysis.
Conclusions
ICU readmission is associated with higher severity of illness scores during the same hospitalization in adult patients.
Keywords: Intensive care unit, Readmission, Severity of illness, Systematic review
Introduction
Readmission to the intensive care unit (ICU) is a frequent adverse outcome in the critically ill population. [1] Approximately 10% of patients discharged from the ICU require readmission during the same hospital stay. [2] Readmission exposes patients to increased risks, as transfers between healthcare professionals have been linked to an increased rate of adverse events, higher mortality, and longer hospital stays. [2–5] Furthermore, the financial impact of ICU care is considerable, as up to 30% of total hospital costs and 1% of the US gross national product are directly linked to ICU expenses. [6] The management of critically ill patients therefore pose significant challenges to healthcare systems seeking to improve quality and reduce unplanned healthcare utilization. [7, 8]
Given the sizeable proportion of health care resources dedicated to critical care, reductions in ICU readmission rates could be an indicator of improved hospital performance. [9, 10] An important first step in reducing the number of ICU readmissions is identifying patients who are most likely to be readmitted. Therefore, there is substantial interest in examining risk factors associated with ICU readmission.
A 2009 systematic review and meta-analysis suggested that the Acute Physiology and Chronic Health (APACHE) score and the Simplified Acute Physiology Score (SAPS) may be useful in predicting ICU readmission. Both of these severity of illness scoring systems are routinely used in ICUs to predict mortality risk. [14–16] Prediction models for ICU readmission that incorporate severity of illness scores have been proposed, but are not routinely used in clinical practice. [17–20] The prospect of predicting ICU readmission risk using only APACHE or SAPS scores is an attractive one, as implementation of these systems would not require additional ICU resources.
Since the publication of the prior review, the delivery of healthcare services in the US has been changing to adjust to Affordable Care Act (ACA) priorities. Adopted by the US Congress in 2010, the primary aim of the ACA is to increase affordability of health insurance to Americans. The ACA has also introduced programs through which payment for health care services are linked to quality of care. ACA programs provide incentives for hospitals to improve value by reducing complicated care transitions and unplanned healthcare utilization, including hospital and ICU readmissions. This has led to an increased number of studies focusing on quality of care and predictors of readmission. Furthermore, novel interventions, such as critical care transition programs, may lower discharge thresholds and modify readmission rates. [21] The objective of this systematic review is to evaluate whether readmission to the ICU during the same hospitalization remains associated with the most commonly used severity of illness scores (APACHE and SAPS) in adult patients.
Methods
Data Sources
Our analysis was performed in accordance with methodology described in the Cochrane Handbook for Systematic Reviews of Interventions. [22] We searched the MEDLINE and EMBASE databases for literature published from inception to February 3 2014. Our search strategy included a combination of controlled vocabulary (MeSH and Emtree) and free-text keywords. Searches were developed in consultation with information specialists from the Johns Hopkins Welch Medical Library. We selected search terms related to three concepts: intensive care; severity of illness; and ICU readmission. We did not restrict the searches with regards to language, study type, or publication year. The full search strategy is presented in Supplementary Data Table 1. We searched the reference lists from our included articles to identify any additional relevant citations and completed forward citation searching through Web of Science. Using an abbreviated search strategy, we identified potentially relevant unpublished studies from the following databases: the NIH clinical trials registry (www.clinicaltrials.gov), WHO International Clinical Trials Registry Platform, Cochrane Register of Controlled Trials (CENTRAL), OpenSIGLE (System for Information on Grey Literature in Europe) and the New York Academy of Medicine Grey Literature Report and Database. We also searched conference proceedings of the American Thoracic Society and the European Respiratory Society.
Study Selection
All titles and abstracts were randomly assigned to be independently screened by two of five investigators (EGW, AMP, DGL, EPB and AIA). Observational studies (prospective or retrospective cohort studies, and case-control studies) that collected severity of illness measures and ICU readmission data were included in our systematic review. Abstracts as well as full-length publications were included in order to minimize potential publication bias. Reviews, case reports, randomized-controlled trials (RCTs), editorials, and case series were excluded. Studies were subsequently excluded during the selection process if they: 1) did not study adult ICU patients (≥18 years of age, predefined as “adults” by the manuscript authors, or admitted to an adult ICU); 2) did not categorize patients based on readmission status; 3) did not report a severity of illness score (SAPS, APACHE); 4) were not in English, Spanish, or French (languages spoken by the investigators); or 5) were not observational studies. The full texts of all studies selected based on titles and abstracts were also reviewed by two independent investigators, and the same exclusion criteria were applied. Any disagreements regarding inclusion of a specific article were adjudicated by discussion among investigators.
Data Extraction and Risk of Bias Assessment
Studies selected for analysis were randomly distributed across the five-investigator group. Data was independently extracted from each study by two investigators and subsequently verified between the dyad. Any discrepancies were resolved through discussion. Study design, participant, exposure, and outcome information was collected and entered into an electronic database. Risk of bias assessments were performed using the Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomized Studies in Meta-Analysis. [23] Two investigators independently assessed each study for the following characteristics that would increase the risk of bias: selection of study subjects; comparability of exposure groups; and measurement of the exposure or outcome. Potential reporting and publication biases were examined graphically with a funnel plot.
Data Synthesis and Analysis
Our primary measure of association was the standardized mean difference (SMD) in severity of illness scores between readmitted and non-readmitted patients. This measure was selected so that different severity of illness indices could be compared. If studies reported both APACHE and SAPS scores, we used the APACHE scores in our combined analysis because this measure was the most frequently reported. When both ICU admission and discharge scores were available, admission scores were used to maximize comparability with the other included studies. For studies reporting severity of illness scores as medians and interquartile ranges (IQR), a normal distribution was assumed: medians were substituted for the mean, and IQRs were converted to standard deviations as recommended by the Cochrane Handbook. [22] Secondary outcomes included ICU length of stay (LOS), hospital LOS, and in-hospital mortality.
We assessed the degree of clinical heterogeneity between studies by comparing multiple types of study characteristics: study participants; type of ICU; type of severity of illness score; and timing of severity of illness measurement. In addition, we evaluated methodological heterogeneity by comparing study designs and risk of bias assessments. Forest plots were generated using Stata 12/IC software (StataCorp LP, College Station, TX) to assess for heterogeneity between studies. Poor overlap of the confidence intervals of SMD’s would suggest significant heterogeneity. Quantitative assessment for heterogeneity was performed by calculating I2 statistics. We considered an I2 value above 50% as evidence of significant heterogeneity. We also calculated chi-squared statistics (Cochran’s Q test) to assess for heterogeneity, with a p-value <0.05 suggesting significant heterogeneity.
Subgroup analyses were performed for the following pre-specified groups: type of severity score used (APACHE vs. SAPS); version of score used (APACHE I-IV, SAPS I-III); time of severity score assessment (ICU admission vs. ICU discharge); type of ICU (medical vs. surgical vs. mixed); risk of bias (low, moderate, high); type of study design (case-control vs. cohort); and continent in which the study was performed. We conducted sensitivity analyses to determine the impact of excluding studies with higher risk of bias, or studies reported in the grey literature. We also performed a sensitivity analysis to determine the impact of excluding studies that reported medians and inter-quartile ranges instead of means and standard deviations. Medians and inter-quartile ranges may have been used to report data that does not fall under a normal distribution, and this could influence the results of our analysis.
Results
Study Selection
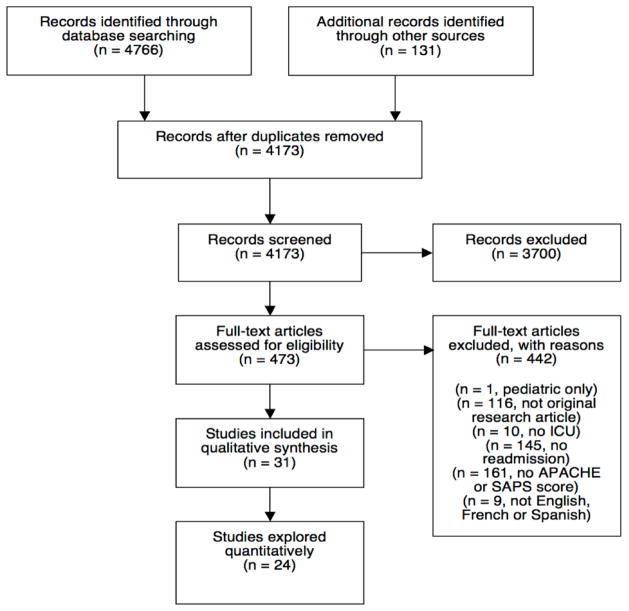
We identified 4766 citations using the search strategy described above (Figure 1). Screening of titles and abstracts yielded 473 articles for full-text review. Thirty-one publications on 30 unique study populations met the pre-defined eligibility criteria for inclusion in the final qualitative synthesis. Two publications that reported on the same study population were analyzed as one study. Ultimately, 24 studies presented enough information to calculate SMDs in severity of illness scores between readmitted and non-readmitted patients.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Flow Diagram
Characteristics of Included Studies
The 31 studies included in the qualitative review were highly variable in terms of their characteristics and outcome reporting (Tables 1–2). Most of the included studies were cohort studies (n=27), and 4 were case-control studies. There were 23 full-text articles and eight abstracts. Studies were conducted between 1987 and 2011 and included approximately 480,000 patients (one study did not report sample size at the patient level [24]). Of these, 32,537 were readmitted to the ICU. The most common severity of illness instrument used was APACHE II (11 studies). Nineteen studies reported ICU LOS, ten studies reported hospital LOS, and 19 studies reported inhospital mortality (Supplementary Data Table 2). Studies were published from five continents, including: North America (n= 11), South America (n=3), Europe (n=9), Asia (n=3), and Australia (n=3). Two studies were collaborations between European and North American countries. More studies were conducted in the United States (n=9) than in any other nation. The studies varied regarding the following characteristics: types of patients studied (subspecialty populations, such as tracheostomy patients, vs. general medical or surgical populations); type of ICU (medical vs. surgical vs. mixed); and hospital and ICU sizes.
Table 1.
Descriptive characteristics of included studies
| First author | Study design | Location | Number of patients | ICU type | Year(s) | ICU beds | Hospital beds | Age Mean (S.D.) or median (interquartile range) | |
|---|---|---|---|---|---|---|---|---|---|
| Readmitted | Non-Readmitted | ||||||||
| Durbin et al.35 | case-control | US | 1803 | Mixed | 24 | 650 | 59.5 (15.2) | 59.1 (15.8) | |
| Chen et al.31 | prospective cohort | Canada | 236 | 1995–1996 | |||||
| Cooper et al.9 | prospective cohort | US | 121161 | Mixed | 1991–1995 | 65.4 (29.0) | 63.4 (18.1) | ||
| Bracco et al. 36 | prospective cohort | Germany & Canada | 44 | Mixed | 1995–1996 | 14 | 280 | ||
| Chung et al.32 | case-control | UK | 65 | SICU | 1998 | 17 | |||
| Metnitz et al.34 | prospective cohort | Austria | 15180 | Mixed | 1998–2000 | 64.8 (14.9) | 62.6 (17.0) | ||
| Alban et al.29,37 Nishi et al. |
retrospective cohort | US | 10840 | SICU | 1996–2001 | 20 | 850 | 60.6 (18.8) | 58.7 (30.3) |
| Gajic et al.19 | prospective cohort | US & Netherlands | 1131 | MICU | 2004–2005 | 64 (18) | 66 (18) | ||
| Conlon et al. 38 | prospective cohort | Ireland | 73 | Mixed | 2004 | 18 | 570 | 66.9 (14.8) | 61.7 (15.2) |
| Kaben et al. 39 | prospective cohort | Germany | 381 | SICU | 2004–2006 | 64 (14) | 62 (15) | ||
| Campbell et al.30 | retrospective cohort | Scotland | 385 | Mixed | 1995–2005 | 66 (54–73) | 60 (43–71) | ||
| Park et al.40 | retrospective cohort | UK | 873 | Mixed | 1995–2007 | 65.6 (9.7) | 64.2 (9.9) | ||
| Chan et al.41 | retrospective cohort | Taiwan | 110 | SICU | 2003–2003 | 64.10 (16.98) | 58.66 (17.42) | ||
| Gerber et al. 25 | retrospective cohort | US | 15 | Mixed | 2004–2006 | 24 | 500 | 59.4 (17.8) | 67.5 (15.0) |
| Butler et al. 42 | prospective cohort | US | 390 | 2002–2008 | |||||
| Ho et al. 33 | prospective cohort | Australia | 16926 | Mixed | 1987–2002 | 22 | 56.3 (17.0) | 53.8 (19.4) | |
| Arsenault et al.43 | case-control | Canada | Mixed | 10–15 | |||||
| Park et al.44 | prospective cohort | South Korea | 4257 | SICU | 2007–2010 | 32 | |||
| Lee et al.45 | case-control | Taiwan | 116 | Neurologic | 2003–2005 | 92 | 60.9 (19.4) | 50.6 (16.9) | |
| Silva et al.46 | prospective cohort | Brazil | 600 | Mixed | 2006–2007 | ||||
| Carrillo Alcaraz et al.47 | prospective cohort | Spain | 12934 | ||||||
| Roehrig et al.48 | prospective cohort | Brazil | 1277 | 2008–2009 | 72 (17) | 66 (17) | |||
| Khaja et al. 24 | prospective cohort | US | 3724 | MICU | 2008–2009 | ||||
| Nassar et al.49 | prospective cohort | Brazil | 3993 | 2010–2011 | 73 (56–82) | 63 (47–77) | |||
| Renton et al. 12 | retrospective cohort | Australia | 247103 | 2000–2007 | 62.5 (16.8) | 59.9 (18.3) | |||
| Timmers et al.50 | prospective cohort | Netherlands | 1682 | SICU | 1995–2000 | 32 | 673 | 65 (15) | 58 (18) |
| Ouanes et al. 20 | prospective cohort | France | 3462 | Mixed | 1998–2010 | 10–18 | 460–1500 | ||
| Willsie et al.51 | prospective cohort | US | 10324 | Mixed | 2003–2009 | 63 | 59 | ||
| Lissauer et al.52 | prospective cohort | US | 703 | SICU | 2011 | 19 | 570 | 59.8 (13.5) | 56.6 (15.1) |
| Yip et al. 53 | prospective cohort | Australia | 1599 | 2009–2010 | 23 | 800 | 53 (34–67) | 50 (32–65) | |
ICU=Intensive care unit; MICU=Medical ICU; SICU=Surgical ICU
Table 2.
Summary of exposure by primary outcome
| First author | N | # Readmitted | #Non-readmitted | Cutoff for readmission | Severity scale | Severity of illness score timinga | Score Mean (S.D.) or median (interquartile range) [absolute range] | |
|---|---|---|---|---|---|---|---|---|
| Readmitted | Non-Readmitted | |||||||
| Durbin et al.35 | 1803 | 83 | 82 | same hospitalization | APACHE II | discharge | 10.6 (5.5) | 8.8 (5.2) |
| Chen et al.31 | 2250 | 140 | 2110 | same hospitalization | APACHE II | admission | 21.4 (8.1)b | 19.8 (8.1)b |
| 2878 | 95 | 2782 | admission | 16.8 (6.8)c | 13.3 (7.2)c | |||
| Cooper et al.9 | 121161 | 6371 | 97613 | same hospitalization | APACHE III | admission | 54.3 (24.3) | 43.7 (22.3) |
| Bracco et al.36 | 1024 | 44 | SAPS II | admission | 22d | 16d | ||
| Chung et al.32 | 65 | 65 | same hospitalization | APACHE III | admission | 63.3e | 57.4e | |
| Metnitz et al34 | 15180 | 780 | 14400 | same hospitalization | SAPS II | 28 (21–38) | 25 (18–35) | |
| Alban et al.29, Nishi et al.37 | 10840 | 296 | 10544 | same hospitalization | APACHE II | admission | 18.4 (8.9) | 15.3 (8.5) |
| discharge | 15.7 (6.7) | 13.8 (7.1) | ||||||
| SAPS | admission | 13.7 (5.8) | 11.5 (5.5) | |||||
| discharge | 12.2 (4.8) | 10.7 (4.9) | ||||||
| Gajic et al.19 | 1131 | 100 | 1026 | <7 days after ICU discharge | APACHE III | admission | 58.1 (22.9) | 69.6 (26.8) |
| discharge | 49.4 (18.2) | 56.8 (18.8) | ||||||
| Conlon et al.38 | 1061 | 73 | 988 | same hospitalization | APACHE II | admission | 14.4 (5.1) | 10.2 (6.6) |
| Kaben et al.39 | 2852 | 381 | 2471 | same hospitalization | SAPS II | 37.1 (16.4) | 32.9 (16.3) | |
| Campbell et al.30 | 4376 | 385 | 3981 | same hospitalization | APACHE II | admission | 20 (16–24) | 17 (13–22) |
| SAPS II | admission | 37 (28–48) | 33 (23–43) | |||||
| Park et al.40 | 7227 | 873 | 6354 | same hospitalization | APACHE II | admission | 14.3 (4.5) | 13.8 (4.9) |
| SAPS II | admission | 25.8 (10.1) | 25.0 (10.6) | |||||
| Chan et al.41 | 945 | 110 | 835 | same hospitalization | APACHE II | 12.80 (6.69) | 11.36 (7.31) | |
| Gerber et al.25 | 42 | 15 | 27 | same hospitalization | APACHE II | 18.7 (7.0) | 21.4 (6.8) | |
| Butler et al.42 | 6511 | 390 | 6121 | same hospitalization | APACHE II | admission | 16 (12–20) | 14 (10–19) |
| SAPS II | admission | 31 (23–42) | 29 (20–39) | |||||
| Ho et al.33 | 16926 | 654 | 16272 | same hospitalization | APACHE II | 14 (13)f | 14.1(13)f | |
| Arsenault et al.43 | 85g | ≤ 72 hours after ICU discharge | APACHE II | admission | ||||
| SAPS | discharge | |||||||
| Park et al. 44 | 4257 | 271 | 3986 | same hospitalization | APACHE II | admission and discharge | ||
| Lee et al. 45 | 116 | 58 | 58 | same hospitalization | APACHE II | admission | 15 (6.8) | 10.1 (5.9) |
| discharge | 12.1 (5.4) | 7.3 (4.8) | ||||||
| Silva et al.46 | 600 | 44 | 556 | same hospitalization | SAPS II | admission | ||
| discharge | ||||||||
| Carrillo Alcaraz et al.47 | 12934 | 730 | 12204 | same hospitalization | SAPS II | 40 (18) | 30 (15) | |
| Roehrig et al. 48 | 1277 | 126 | 1151 | same hospitalization | APACHE II | 18 (9) | 13 (7) | |
| Khaja et al.24 | 3724h | 163 | 3495 | same hospitalization | APACHE IV | 67.5 (30.7) | 88.5 (31.2) | |
| Nassar et al.49 | 3993 | 283 | 3354 | same hospitalization | APACHE II | admission | 37 [23–51] | 26 [18–36] |
| Renton et al.12 | 247103 | 13598 | 223505 | same hospitalization | APACHE III | 56 (42–73) | 47 (34–64) | |
| SAPS II | 31 (23–41) | 26 (19–36) | ||||||
| Timmers et al.50 | 1682 | 141 | 1541 | <30 days after ICU discharge | APACHE II | admission | 12 (6) | 11 (6) |
| SAPS III | admission | 46 (12) | 42 (13) | |||||
| Ouanes et al.20 | 3462 | 74 | 3360 | <7days after ICU discharge | SAPS II | admission | 40 (19) | 33 (20) |
| Willsie et al.51 | 10324 | 1197 | 9127 | <48 hrs, 48 hrs-30 days, >30 days after ICU discharge | APACHE II | admission | 7.4 | 6.0 |
| Lissauer et al.52 | 703 | 77 | 610 | same hospitalization | APACHE III | admission | 69.5 (54.9) | 54.9 (23.5) |
| Yip et al.53 | 1599 | 106 | 1340 | same hospitalization | APACHE II | discharge | 20 (16–24) | 19 (14–24) |
Admission = index admission unless otherwise specified;
Academic hospital;
Community hospital;
p=0.001;
p=0.05;
Reported as median and SD;
Total N – number in each group not reported;
Unit of analysis is number of readmissions
Methodological Quality of Included Studies
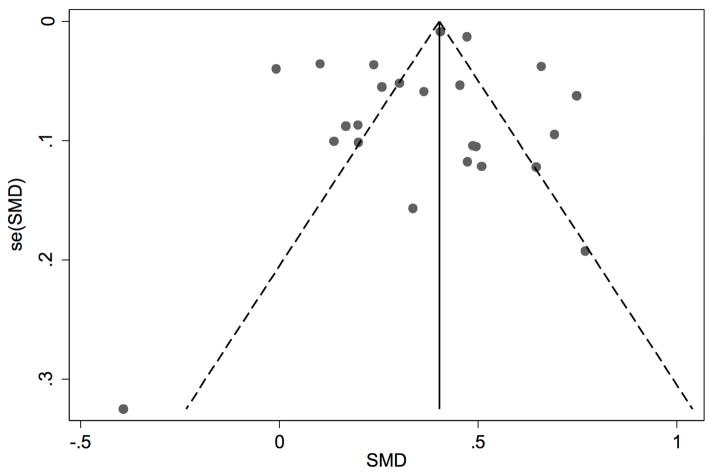
We classified 22 studies as having low risk of bias, 4 as having moderate risk of bias, and 4 as having high risk of bias. We assigned high risk of bias for the following reasons: no description of how severity of illness was ascertained and verified; no statement of how cohorts were followed up; and concerns about comparability of cases and controls in case-control studies. The funnel plot showed high variability in the SMD, even in studies with low standard error (Figure 2). There was one clear outlier on the funnel plot, [25] but otherwise, we did not observe significant asymmetry that would raise concerns for publication bias.
Figure 2.
Funnel plot of included studies with standardized mean differences (SMD) and associated standard error (se(SMD))
The studies that were included in our systematic review had significant variation in the reporting of their methods of ascertainment. While most investigators identified readmission through hospital databases, many did not report methods of assessing severity scores. Some investigators provided differing case and control definitions. Not all studies included the secondary outcomes we included in our data extraction protocol. For instance, only 5 studies reported the time to readmission.
There were also several methodological factors contributing to the heterogeneity among studies. While all studies defined ICU readmission as a readmission occurring during the same hospitalization, several used time-based cut points (e.g., 48 hours) after ICU discharge to classify early vs. late readmissions. Other studies limited the time they followed patients during their hospitalization.
Outcomes
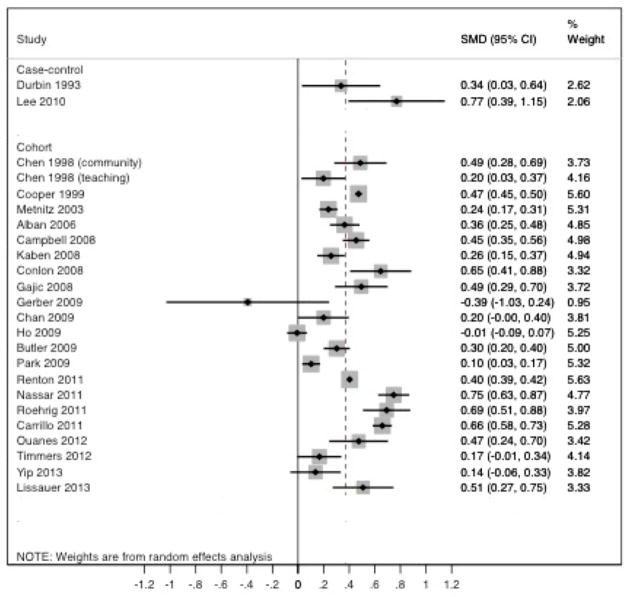
The overall readmission rate was 5.7% (27,517/482,338) in the cohort studies. There was substantial statistical heterogeneity across studies, with SMDs ranging from −0.39 (95%CI −1.03–0.24; Gerber 2009) to 0.77 (0.39–1.15; Lee 2010). The I2 statistic was 94.1% (p<0.001) for cohort studies (Q statistic 356.40), and 67.2% (p<0.001) for case-control studies (Q statistic 3.05). The excessive heterogeneity precluded reporting of summary estimates in the form of a meta-analysis.
A majority of studies found that readmission was associated with higher APACHE and SAPS scores, with all but five studies demonstrating a statistically significant association between readmission and increased severity of illness (Figure 3). The remaining studies [25, 33, 41, 50, 53] had 95% CIs that overlapped the null value, suggesting that there was no statistically significant difference in severity of illness scores between readmitted and non-readmitted patients. Sensitivity analyses revealed similar results.
Figure 3.
Forest plot depicting standardized mean differences (SMD) and 95% confidence intervals (95% CI) of severity of illness scores between re-admitted and non re-admitted patients
Subgroup analyses (stratifying by type and version of severity score, time of score assessment, type of ICU, risk of bias, study design, and continent of origin) did not rectify the significant heterogeneity and also precluded summary estimates. None of these analyses significantly modified the association between ICU readmission and severity scores.
Overall, mortality was greater in patients who were readmitted to the ICU vs. those who were not readmitted (Supplementary Data Table 2). Hospital mortality in non-readmitted patients varied widely (from 1% to 18%). Hospital mortality in the readmitted patients ranged from 10% to >50%, with the surgical ICUs showing overall lower mortality. ICU LOS was longer in the readmitted vs. non-readmitted patients. Most studies did not specify whether the LOS for readmitted patients included both the index and second admission, or whether the data referred only to the index admission. Hospital LOS was consistently longer in the readmitted vs. non-readmitted patients. In studies that reported hospital LOS, the readmitted patients spent approximately twice as much time in the hospital as the non-readmitted patients.
Discussion
The results of this systematic review found that ICU readmission is associated with higher severity of illness scores in patients discharged alive from the ICU. This association does not appear to be modified by type of severity score, timing of measurement, or type of ICU. Patients readmitted to the ICU were older, had longer hospital and ICU stays, and had higher mortality than non-readmitted patients.
Our findings were consistent with those of Frost et al., who reviewed studies published up until 2008. [14] Our review differed from that of Frost et al. in that we included searches of the grey literature, and we did not include a search of the CINAHL database. Our search strategy identified all of the articles that were used for the Frost systematic review, as well as 14 additional studies published after 2008. Given the interval of time that had passed since our original search, an updated literature search was performed in August 2015. This new search identified three additional publications that would likely have been included in the original systematic review. [26–28] Two of these studies found significantly higher APACHE II scores in readmitted ICU patients, while the third found a non-statistically significant increase in SAPS III scores among readmitted patients. Because these studies were not prospectively screened and analyzed, these findings have not been merged with those of the systematic review. However, we believe the inclusion of these studies would not alter our conclusions.
Unlike the previous systematic review, we decided that the significant heterogeneity among the selected studies precluded a meta-analysis, which would inappropriately combine widely disparate findings into a single summary measure. This heterogeneity persisted despite controlling for multiple characteristics (type of severity score, timing of measurement, type of ICU, risk of bias, study design, and continent of origin) through subgroup analyses. This finding suggests that the association between ICU readmission and severity of illness scores varies substantially across settings, and this variability is not explained by factors evaluated in our subgroup analyses. This heterogeneity may be related to unreported patient or hospital factors, such as source of admission, time of discharge, ICU staffing, and safety culture.
Numerous patient-level and hospital-level factors influence ICU readmission, and multiple complex prediction models for ICU readmission have been proposed. [5, 29–34] A 2013 systematic review of risk stratification tools identified eight models developed to predict ICU readmission and/or in-hospital mortality. [17] Although these prediction tools show promise, their complexity and lack of validation may limit their use. The widespread use and familiarity of APACHE and SAPS scores make them more likely to be clinically accepted and implemented. Although our analysis was not intended to assess the predictive value of severity of illness scores, it does provide evidence that severity of illness scores may have wider clinical use and could be considered for inclusion in future ICU readmission prediction models.
This systematic review has some notable limitations. Although our initial goal was to study severity of illness scores as the exposure of interest, the ways in which data were reported in the published studies made this analysis impossible. Instead, we used readmission as the exposure of interest, and this should be taken into account when extrapolating findings. Second, we limited our studies to those containing the two most commonly used severity of illness scores, APACHE and SAPS. Findings might differ if other severity of illness scores were included. Third, our selection criteria led to the exclusion of a few large cohort studies specifically evaluating severity of illness and ICU readmission; these studies did not permit a direct comparison of APACHE or SAPS scores between readmitted and non-readmitted patients. [4, 11] Fourth, a number of included studies were conference abstracts (8 of 31 studies), and these studies included limited information on their methods. Finally, there was limited information on hospital-level factors (such as characteristics of individual ICUs) that could be important sources of confounding and heterogeneity among studies.
Despite these limitations, the findings of our review contribute to current efforts to identify high-risk patients and to design interventions to reduced unplanned healthcare utilization. The study of ICU readmissions has important implications across the healthcare system. At the patient and caregiver level, unplanned ICU readmissions may become a publicly reported outcome used for benchmarking hospital performance, which could subsequently influence patients’ choice of hospitals. At the health system level, identifying excessive numbers of unplanned readmissions may lead to the development of new service systems and interventions to improve quality of care and reduce readmissions. Ultimately, at the payer and policymaker level, payment strategies may be developed to incentivize readmission prevention and reduce health care costs.
Conclusions
Based on our systematic review of data from over 480,000 ICU patients and more than 32,000 readmissions, we conclude that ICU readmission is associated with increased severity of illness scores. The APACHE and SAPS severity of illness measures are routinely measured in clinical practice, are easily retrievable from health system databases, and can be used as part of a larger effort to understand ICU readmissions. Because a broad range of factors contribute to readmission risk, future studies examining ICU readmission should include ICU and health-system characteristics in addition to patient-level variables. These studies would provide useful information for health systems aiming to reduce the risk of ICU readmission—an important goal for patients, caregivers, providers, health systems, payers, and policymakers.
Supplementary Material
Acknowledgments
This research was primarily conducted while Drs. Arbaje, Parker and Leung were Johns Hopkins Clinical Research Scholars, supported by grant # KL2TR001077. Dr. Arbaje received funding from the National Patient Safety Foundation and the Johns Hopkins University School of Nursing Center for Innovative Care in Aging. She currently receives funding from the Agency for Healthcare Research and Quality (grant # 1K08HS022916). Dr. Brigham is currently supported through the National Heart Lung and Blood Institute, grant # 1F32HL120396.
Footnotes
Conflicts of interest: None
The funders had no role in any of the following activities: design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Garland A, Olafson K, Ramsey CD, et al. Epidemiology of critically ill patients in intensive care units: a population-based observational study. Crit Care. 2013;17:R212. doi: 10.1186/cc13026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rosenberg AL, Watts C. Patients readmitted to ICUs: A systematic review of risk factors and outcomes. Chest. 2000;118:492–502. doi: 10.1378/chest.118.2.492. [DOI] [PubMed] [Google Scholar]
- 3.Li P, Stelfox HT, Ghali WA. A prospective observational study of physician handoff for intensive-care-unit-to-ward patient transfers. Am J Med. 2011;124:860–867. doi: 10.1016/j.amjmed.2011.04.027. [DOI] [PubMed] [Google Scholar]
- 4.Kramer AA, Higgins TL, Zimmerman JE. The association between ICU readmission rate and patient outcomes. Crit Care Med. 2013;41:24–33. doi: 10.1097/CCM.0b013e3182657b8a. [DOI] [PubMed] [Google Scholar]
- 5.Rosenberg AL, Hofer TP, Hayward RA, et al. Who bounces back? Physiologic and other predictors of intensive care unit readmission. Crit Care Med. 2001;29:511–518. doi: 10.1097/00003246-200103000-00008. [DOI] [PubMed] [Google Scholar]
- 6.Oye RK, Bellamy PE. Patterns of resource consumption in medical intensive care. Chest. 1991;99:685–689. doi: 10.1378/chest.99.3.685. [DOI] [PubMed] [Google Scholar]
- 7.Milbrandt EB, Kersten A, Rahim MT, et al. Growth of intensive care unit resource use and its estimated cost in Medicare. Crit Care Med. 2008;36:2504–2510. doi: 10.1097/CCM.0b013e318183ef84. [DOI] [PubMed] [Google Scholar]
- 8.Cooper LM, Linde-Zwirble WT. Medicare intensive care unit use: analysis of incidence, cost, and payment. Crit Care Med. 2004;32:2247–2253. doi: 10.1097/01.ccm.0000146301.47334.bd. [DOI] [PubMed] [Google Scholar]
- 9.Cooper GS, Sirio CA, Rotondi AJ, et al. Are readmissions to the intensive care unit a useful measure of hospital performance? Med Care. 1999;37:399–408. doi: 10.1097/00005650-199904000-00009. [DOI] [PubMed] [Google Scholar]
- 10.Baker DR, Pronovost PJ, Morlock LL, et al. Patient flow variability and unplanned readmissions to an intensive care unit. Crit Care Med. 2009;37:2882–2887. doi: 10.1097/ccm.0b013e3181b01caf. [DOI] [PubMed] [Google Scholar]
- 11.Brown SES, Ratcliffe SJ, Kahn JM, et al. The epidemiology of intensive care unit readmissions in the United States. Am J Respir Crit Care Med. 2012;185:955–964. doi: 10.1164/rccm.201109-1720OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Renton J, Pilcher DV, Santamaria JD, et al. Factors associated with increased risk of readmission to intensive care in Australia. Intensive Care Med. 2011;37:1800–1808. doi: 10.1007/s00134-011-2318-x. [DOI] [PubMed] [Google Scholar]
- 13.Elliott M, Worrall-Carter L, Page K. Intensive care readmission: A contemporary review of the literature. Intensive Crit Care Nurs. 2013 doi: 10.1016/j.iccn.2013.10.005. [DOI] [PubMed]
- 14.Frost SA, Alexandrou E, Bogdanovski T, et al. Severity of illness and risk of readmission to intensive care: a meta-analysis. Resuscitation. 2009;80:505–510. doi: 10.1016/j.resuscitation.2009.02.015. [DOI] [PubMed] [Google Scholar]
- 15.Knaus WA, Draper EA, Wagner DP, et al. APACHE II: A severity of disease classification system. Critical Care Medicine. 1985;13:818–829. [PubMed] [Google Scholar]
- 16.Le Gall JR, Lemeshow S, Saulnier F. A new simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. Journal of the American Medical Association. 1993;270:2957–2963. doi: 10.1001/jama.270.24.2957. [DOI] [PubMed] [Google Scholar]
- 17.Hosein FS, Bobrovitz N, Berthelot S, et al. A systematic review of tools for predicting severe adverse events following patient discharge from intensive care units. Crit Care. 2013;17:R102. doi: 10.1186/cc12747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Frost SA, Tam V, Alexandrou E, et al. Readmission to intensive care: development of a nomogram for individualising risk. Crit Care Resusc. 2010;12:83–89. [PubMed] [Google Scholar]
- 19.Gajic O, Malinchoc M, Comfere TB, et al. The stability and workload index for transfer score predicts unplanned intensive care unit patient readmission: Initial development and validation. Crit Care Med. 2008;36:676–682. doi: 10.1097/CCM.0B013E318164E3B0. [DOI] [PubMed] [Google Scholar]
- 20.Ouanes I, Schwebel C, Francais A, et al. A model to predict short-term death or readmission after intensive care unit discharge. J Crit Care. 2012;27:422.e1–422.e9. doi: 10.1016/j.jcrc.2011.08.003. [DOI] [PubMed] [Google Scholar]
- 21.Niven DJ, Bastos JF, Stelfox HT. Critical care transition programs and the risk of readmission or death after discharge from an ICU: a systematic review and meta-analysis. Crit Care Med. 2014;42:179–187. doi: 10.1097/CCM.0b013e3182a272c0. [DOI] [PubMed] [Google Scholar]
- 22.Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions. The Cochrane Collaboration; 2011. Version 5.1.0 updated March 2011. Available from www.cochrane-handbook.org. [Google Scholar]
- 23.Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses [Google Scholar]
- 24.Khaja M, Diaz-Fuentes G, Sahasranaman V, et al. Readmissions to medical intensive care units in an inner city hospital-does readmission diagnosis matter? Chest. 2011:140. [Google Scholar]
- 25.Gerber DR, Chaaya A, Schorr CA, et al. Can outcomes of intensive care unit patients undergoing tracheostomy be predicted? Respir Care. 2009;54:1653–1657. [PubMed] [Google Scholar]
- 26.Elshafey M, Hewidy A. Predictors of pulmonary critical care recidivism. Egypt J Chest Dis Tuberc. 2014;63:947–954. [Google Scholar]
- 27.Lee H, Lim CW, Hong HP, et al. Efficacy of the APACHE II score at ICU discharge in predicting post-ICU mortality and ICU readmission in critically ill surgical patients. Anaesth Intensive Care. 2015;43(2):175–86. doi: 10.1177/0310057X1504300206. [DOI] [PubMed] [Google Scholar]
- 28.Kareliusson F, De Geer L, Tibblin AO. Risk prediction of ICU readmission in a mixed surgical and medical population. J Intensive Care. 2015;3(1):30. doi: 10.1186/s40560-015-0096-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Alban RF, Nisim AA, Ho J, et al. Readmission to surgical intensive care increases severity-adjusted patient mortality. Journal of Trauma - Injury, Infection and Critical Care. 2006;60:1027–1031. doi: 10.1097/01.ta.0000218217.42861.b7. [DOI] [PubMed] [Google Scholar]
- 30.Campbell AJ, Cook JA, Adey G, et al. Predicting death and readmission after intensive care discharge. Br J Anaesth. 2008;100:656–662. doi: 10.1093/bja/aen069. [DOI] [PubMed] [Google Scholar]
- 31.Chen LM, Martin CM, Keenan SP, et al. Patients readmitted to the intensive care unit during the same hospitalization: Clinical features and outcomes. Crit Care Med. 1998;26:1834–1841. doi: 10.1097/00003246-199811000-00025. [DOI] [PubMed] [Google Scholar]
- 32.Chung DA, Sharples LD, Nashef SAM. A case-control analysis of readmissions to the cardiac surgical intensive care unit. European Journal of Cardio-thoracic Surgery. 2002;22:282–286. doi: 10.1016/s1010-7940(02)00303-2. [DOI] [PubMed] [Google Scholar]
- 33.Ho KM, Dobb GJ, Lee KY, et al. The effect of comorbidities on risk of intensive care readmission during the same hospitalization: A linked data cohort study. J Crit Care. 2009;24:101–107. doi: 10.1016/j.jcrc.2007.11.015. [DOI] [PubMed] [Google Scholar]
- 34.Metnitz PGH, Fieux F, Jordan B, et al. Critically ill patients readmitted to intensive care units - Lessons to learn? Intensive Care Med. 2003;29:241–248. doi: 10.1007/s00134-002-1584-z. [DOI] [PubMed] [Google Scholar]
- 35.Durbin CG, Jr, Kopel RF. A case-control study of patients readmitted to the intensive care unit. Crit Care Med. 1993;21:1547–1553. doi: 10.1097/00003246-199310000-00025. [DOI] [PubMed] [Google Scholar]
- 36.Bracco D, Favre JB, Bissonnette B, et al. Human errors in a multidisciplinary intensive care unit: a 1-year prospective study. Intensive Care Med. 2001;27:137–145. doi: 10.1007/s001340000751. [DOI] [PubMed] [Google Scholar]
- 37.Nishi GK, Suh RH, Wilson MT, et al. Analysis of causes and prevention of early readmission to surgical intensive care. Am Surg. 2003;69:913–917. [PubMed] [Google Scholar]
- 38.Conlon N, O’Brien B, Herbison GP, et al. Long-term functional outcome and performance status after intensive care unit re-admission: A prospective survey. Br J Anaesth. 2008;100:219–223. doi: 10.1093/bja/aem372. [DOI] [PubMed] [Google Scholar]
- 39.Kaben A, Correa F, Reinhart K, et al. Readmission to a surgical intensive care unit: incidence, outcome and risk factors. Crit Care. 2008;12:R123. doi: 10.1186/cc7023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Park DP, Welch CA, Harrison DA, et al. Outcomes following oesophagectomy in patients with oesophageal cancer: a secondary analysis of the ICNARC Case Mix Programme Database. Crit Care. 2009;13(Suppl 2):S1. doi: 10.1186/cc7868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chan KS, Tan CK, Fang CS, et al. Readmission to the intensive care unit: an indicator that reflects the potential risks of morbidity and mortality of surgical patients in the intensive care unit. Surg Today. 2009;39:295–299. doi: 10.1007/s00595-008-3876-6. [DOI] [PubMed] [Google Scholar]
- 42.Butler I, Rachoin J, Schorr C, et al. Characteristics of patients readmitted to the ICU. Crit Care Med. 2009;37:A309. [Google Scholar]
- 43.Arsenault KA, Hamielec CM. Prediction of readmission: ICU risk and prognostic models. Am J Respir Crit Care Med. 2010:181. [Google Scholar]
- 44.Park H-P, Lee H-N, Lee J-H, et al. The discharge revised acute physiology and chronic health evaluation score as a predictor of readmission after discharge from surgical intensive care unit. Crit Care Med. 2010;38:A145. [Google Scholar]
- 45.Lee HF, Lin SC, Lu CL, et al. Revised Acute Physiology and Chronic Health Evaluation score as a predictor of neurosurgery intensive care unit readmission: a case-controlled study. J Crit Care. 2010;25:294–299. doi: 10.1016/j.jcrc.2009.12.007. [DOI] [PubMed] [Google Scholar]
- 46.da Silva MCM, de Sousa RMC, Padilha KG. Factors associated with death and readmission into the Intensive Care Unit. Rev Lat Am Enferm. 2011;19:911–919. doi: 10.1590/s0104-11692011000400009. [DOI] [PubMed] [Google Scholar]
- 47.Carrillo Alcaraz A, Gonzalez Diaz G, Lopez Martinez A, et al. Analysis of readmitted patients after intensive care discharge. Intensive Care Med. 2011;37:S217. [Google Scholar]
- 48.Roehrig C, Antonio AC, Castro P, et al. Swift score predict icu-readmission in South America? Intensive Care Med. 2011;37:S216. [Google Scholar]
- 49.Nassar AP, Salles LD, Brauer L. Patients readmitted to intensive care: Who they are and what happens to them? Crit Care. 2011;15:28. [Google Scholar]
- 50.Timmers T. Patients’ predictions of intensive care unit readmission in surgical ICU. Crit Care Med. 2010;38:A184. [Google Scholar]
- 51.Willsie P, Hunter K, Schorr C, et al. Identifying risk factors for ICU readmission. Crit Care Med. 2012;40:162. [Google Scholar]
- 52.Lissauer ME, Diaz JJ, Narayan M, et al. Surgical Intensive care unit admission variables predict subsequent readmission. Am Surg. 2013;79:583–588. [PubMed] [Google Scholar]
- 53.Yip CB, Ho KM. Eosinopenia as a predictor of unexpected re-admission and mortality after intensive care unit discharge. Anaesth Intensive Care. 2013;41:231–241. doi: 10.1177/0310057X1304100130. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.