Abstract
Feeding difficulties and feeding disorders are a commonly occurring problem for young children, particularly children with developmental delays including autism. Behavior analytic interventions for the treatment of feeding difficulties oftentimes include escape extinction as a primary component of treatment. The use of escape extinction, while effective, may be problematic as it is also associated with the emergence of challenging behavior (e.g., extinction burst). Such challenging behavior may be an acceptable side effect in treatment cases where feeding problems are severe and chronic (e.g., failure to thrive). However, in more acute cases (e.g., selective eating), the negative side effect may be unwarranted and undesired. More recent research on the behavioral treatment of food selectivity has begun to evaluate treatments for feeding difficulties that do not include escape extinction (e.g., demand fading, behavioral momentum), with some success. However, research to date reveals individual differences in responsiveness to such treatments and no clear preferable treatment has emerged. This manuscript describes a multi-component treatment package that includes shaping, sequential presentation and simultaneous presentation, for the treatment of food selectivity in four young children with developmental delays. This treatment package extends the literature on the behavioral treatment for food selectivity and offers a multi-component treatment protocol that may be clinically applicable across a range of treatment scenarios and settings.
Keywords: Behavior, Issue 102, food selectivity, children, escape extinction, autism spectrum disorders, autism
Introduction
Food selectivity, defined as a reluctance to try new foods based on some dimension of the food (e.g., texture, color, or presentation) often characterizes the feeding behavior of young children with autism spectrum disorders (ASD) and other developmental delays2,4,7,10.
Although children who exhibit food selectivity often eat some foods, these foods are frequently limited in variety (e.g., snacks and carbohydrates) and may not provide adequate nutrition. Food selectivity may never lead to total food refusal requiring medical attention (e.g., a diagnosis of failure to thrive or the insertion of a gastric feeding tube) however, the limited food repertoires of children with food selectivity may lead to nutritional inadequacies.
An effective intervention to increase food acceptance in children with acute food selectivity is escape extinction, in the forms of non-removal of the spoon and/or physical guidance1,6,11.
Children who engage in severe maladaptive feeding behavior often engage in total food refusal that leads to limited weight gain and growth and may require the use of gastric-tube feedings. When a child’s feeding behavior is impacting their development, escape extinction may be essential to quickly increase food acceptance. For example, Cooper and colleagues5 found that escape extinction was a necessary component in the treatment packages of 3 of 4 participants who all exhibited poor growth and engaged in tantrum behavior (e.g., gagging, spitting and screaming) when food was presented.
Escape extinction has been repeatedly demonstrated as a valuable component in treatment packages for children with chronic feeding problems, however; these procedures may not be necessary for children who engage in less severe feeding behavior (i.e., food selectivity). Children who engage in severe feeding behavior may differ from children who engage in food selectivity, in that severe feeding behavior may involve total food refusal where as children with food selectivity may consume some foods, although limited in range and nutritional value.
Consistent consumption of even a limited number of foods may lead to children being responsive to reinforcement-based interventions that do not require the addition of escape extinction. For children with autism, positive reinforcement procedures are viewed as best practice9 and should be implemented in the treatment of food selectivity when the child’s behavior may not warrant the use of escape extinction. Recent research on the use of antecedent manipulations and positive reinforcement methodologies as possible alternatives to the use of escape extinction suggest that these methods may be effective for some children who exhibit food selectivity3,11,12.
Studies evaluating the use of antecedent manipulations to treat food selectivity have incorporated a variety of procedures including, high-p sequences6,11,12, and sequential and simultaneous food presentation1,8,13. Results of studies evaluating these procedures have shown that antecedent manipulations are effective in increasing food acceptance for children who engage in food selectivity12,14. For example, Penrod and colleagues12 effectively increased food consumption in two children diagnosed with ASD who engaged in active food refusal (e.g., spitting, gagging and vomiting), using a treatment package consisting of a high-p sequence and demand fading procedure.
The way in which preferred and non-preferred foods are presented (e.g., sequential versus simultaneous presentation) may also contribute to the effectiveness of treatment packages for children who engage in food selectivity. Both sequential (i.e., presenting the non-preferred food followed by the preferred food) and simultaneous (i.e., combining a non-preferred and preferred food together) presentation methods have demonstrated some success in increasing food acceptance13,14. For example, Piazza et al.13, found that the simultaneous presentation procedure, without escape extinction was effective in increasing food acceptance in 3 of 4 participants and that sequential presentation was ineffective for 2 participants. In contrast, Pizzo and colleagues14 successfully used a treatment package consisting of sequential presentation and appetite manipulation to increase food acceptance in a 16-year-old boy with ASD. While the degree to which these presentation procedures are successful without the addition of escape extinction is unclear; some studies suggest that these procedures may be an effective antecedent manipulation for some children. More research is required to determine the utility of both sequential and simultaneous procedures in treatment packages that do not include an escape extinction component.
In designing treatment packages for children who engage in food selectivity, it is important to consider the differences between children who eat a limited number of foods and those who engage in total food refusal as this may impact responsiveness to intervention. For children who engage in food selectivity, parents and clinicians may be less willing to implement intrusive escape extinction procedures since they may not view the child’s behavior as severe enough to warrant these interventions. Tarbox, Schiff and Najdowski15 suggest that anecdotal reports indicate that escape extinction procedures may be difficult for parents to accept. The authors propose that it may be useful to evaluate the effectiveness of other behavioral treatment procedures that may be less intrusive for cases where escape extinction may be not accepted by the parents.
Results from the studies reviewed provide evidence that antecedent manipulations are an important and powerful component to treatment packages for food selectivity. Antecedent manipulations may take many forms (e.g., high-p sequences and sequential and simultaneous food presentation) and it is important that research focuses on which components may be combined in treatment packages to effectively increase food acceptance without the addition of escape extinction; as these interventions may provide less intrusive alternatives when escape extinction procedures are not necessary. This manuscript describes a treatment package that combines shaping, sequential and simultaneous presentation procedures. These procedures have been effective in increasing food acceptance when combined with other antecedent manipulations but have not previously been combined in a treatment package. The current protocol extends the literature on sequential and simultaneous presentation procedures by including them in a treatment package with a shaping procedure that may serve as a first line of treatment that could be implemented by parents, teachers, and clinicians with limited training before seeking more intensive treatment.
Protocol
This protocol follows Florida International University’s guidelines for research with human subjects and consent is always obtained from parents/caregivers before any treatment is started. In addition, obtain clearance from a physician before the start of treatment.
NOTE: Although specific age ranges and individual variables have not been empirically validated, this protocol has been used clinically for children ages 2-7 with autism and developmental delays. Participants should be referred for behavioral intervention by their caregiver and a medical professional. Clear participants of any medical or physical underlying issues related to feeding as part of the screening for eligibility for behavioral intervention protocols to address food selectivity.
1. Session Structure and Clinical Environment
Conduct treatment sessions in an outpatient treatment setting, between two and four times per week, for approximately 1 hr per session. Conduct sessions in treatment rooms equipped with a table, chairs, and items that are used during mealtimes (i.e., plates, napkins and utensils). Additionally, bring toys and other tangible items into the room to serve as reinforcers throughout out the intervention procedure.
2. Pre-treatment Assessments
Preference Assessment.
Conduct a brief, informal preference assessment at the start of each session, to determine tangible items that may function as reinforcers for compliance during that session. Present an array of toys on the table and the give the child the opportunity to choose the toys he/she wants to work for that day.
- Food Assessment
- Ask parents or caregivers to indicate foods that the child is likely to eat 100% of the time when they are offered, 80% of the time, 60% of the time, and so on down to those foods the child would not accept (0%) in twenty percent increments.
- Begin the intervention with those foods the child is likely to eat (100% of the time when offered) and proceeded to more difficult foods that the child has never tried. NOTE: The purpose of including a preferred (100%) food in the first intervention condition is to initially foster compliance with the demand fading steps.
3. Sessions and Procedures
During baseline present a bite of each of the target foods that have not yet been exposed to the intervention on a white plate in front of the child and say, “Eat this.” Do not provide any consequences contingent on any response emitted during baseline.
If the child eats the food, then allow them time to consume it and then present the next bite. If the child does not eat the food after 10 sec the trials ends and then present the next food. NOTE: Present each food should 5 times during baseline in an alternating order. Conduct at least 2 baseline sessions prior to beginning intervention for any target food. Continue to probe the remaining foods in baseline at least one time per week.
Confirm parent report of the child’s food preferences by placing one food from each category (i.e., 100%, 80%, etc.) on a white plate in front of the child and say, “Eat this.” Present each of the foods five times in an alternating order. If the child eats the food, move on to the next trial. If the child does not eat the food after 10 sec, remove it from the plate and present the next food item. If the child throws the food or says they do not want it move on to the next food item without addressing the problem behavior. NOTE: Only use those foods that are consistent with parent report for intervention. If there are foods that do not match the parent report, for example the parent reports that the child eats an item 20% of the time and they eat it 100% of the time during this phase, do not include this food as a target for intervention.
Intervention Sessions.
Conduct all treatment sessions as trials (rather than time based) and a session includes five trials. A trial begins when the target food is placed on the placemat and the instruction is delivered. A trial ends contingent on compliance or after 10s of noncompliance. Vary the number of sessions completed during each 1 hr visit depending on child variables and characteristics, including compliance with instructions. NOTE: The mastery criterion for each step in the intervention is 80% or higher of compliance across two consecutive sessions. Compliance is defined as completing the presented task within 10 sec from the time the instruction is delivered.
4. Treatment Package
NOTE: The treatment package consists of shaping and sequential and simultaneous presentation procedures.
- Shaping
- Implement a shaping procedure for each target food, where successive approximations to eating are reinforced. The shaping procedure is composed of seven steps; a) put the food in therapist’s hand, b) touch the food to the child’s cheek, c) touch food to nose; d) touch food to lips; e) touch food to tongue; f) bite down on food; g) eat food (i.e., mouth clean [swallowing the food so that none of it remains in the child’s mouth]). NOTE: During each step the child has to complete the target behavior independently (e.g., the child has to put the food in the therapist’s hand).
- Sequential Presentation
- Use a placemat containing two different colored circles to serve as a visual representation of the sequential presentation procedure. Always place target foods on the left and less preferred foods on the right side of the placemat. NOTE: This presentation is designed to foster predictability in the procedure and to acquire stimulus control for compliance with foods presented on the left side.
- Additionally, place preferred tangible items on the right side of the placemat. Use the prompt, “First [shaping step] then [name of preferred food and tangible]” to introduce the instruction for the sequential presentation procedure. For example, “first touch the pea to your nose and then you can have your cookie and crayons.”
- Simultaneous Presentation
- Present both the preferred and non-preferred foods together during the simultaneous procedure. Specifically, place the non-preferred food on top of the preferred food (e.g., a grain of rice is placed on top of a chip) and place this combination on the left side of the placemat.
- Place preferred tangible and edible items on the right side of the placemat, as is done in the sequential procedure. Slowly increase the amount of non-preferred food placed on top of the preferred food until equal amounts of non-preferred and preferred foods are presented.
- Present all foods in bite size pieces. Use pieces that are small enough that the child can consume it with one bite, but large enough so that the child will need to chew it several times before swallowing. Present foods with or without a utensil depending on individual needs. Require that participants feed themselves during all sessions.
5. Intervention
- Training Phase (Preferred Food) NOTE: Use the most preferred food (i.e., the food identified as most likely to be eaten 100% of the time in the food assessment) during the training phase, aimed at facilitating familiarity with and compliance with the steps in the shaping sequence.
- Begin the training phase with the initial step of placing the food in the examiner’s hand and continue until the child reaches the mastery criterion (i.e., at least 80% compliance across two consecutive sessions) for the final step (i.e., eating).
- Shaping and Sequential Presentation
- Use the next food identified in the food assessment (child is likely to eat 80% of the time when offered) for this phase of the intervention. During each session, the participant and therapist sit side by side at the table.
- Place the placemat in front of the child and all food and tangible items are placed on the table next to the therapist.
- Begin each trial by placing the target food on the left side of the placemat and the potential reinforcers on the right side. The therapist then provides the first-then prompt.
- Contingent on compliance, allow the child to have access to the reinforcers (consumption of preferred food and access to tangible item for approximately 30 sec). Contingent on noncompliance (not completing the target behavior within 10 sec or throwing the target food), represent the first-then prompt.
- Begin this phase with step 1 of the shaping procedure (put the food in therapist’s hand) and tell the participant “first put ___in my hand and then you can have (reinforcer).” Continue until the mastery criteriais met (80% or higher compliance across two consecutive sessions).
- Move to step 2 of the shaping procedure (touch the food to the child’s cheek) when mastery criteria are met. Continue sessions in this manner until the last step of eating the food is mastered. Introduce the next food identified at this point starting with step 1 of the shaping procedure and repeating the shaping steps as described.
- Shaping, Sequential, and Simultaneous Presentation NOTE: Introduce a simultaneous presentation phase in instances when shaping and sequential presentation are not effective in increasing compliance for the last step in the shaping sequence (i.e., mouth clean).
- Begin this phase by first combining the two foods so that the non-preferred food is not visible to the child. For example, place the non-preferred food inside of the preferred and placed on the placemat so that the child cannot see the non-preferred food.
- Systematically increase the size of the non-preferred food and decrease the preferred food until the non-preferred food is presented alone. The ratio of the two foods (i.e., preferred and non-preferred) is systematically changed when compliance reaches 80% or better across two consecutive sessions. Continue to use the placemat and first-then prompt in this phase.
6. Data
Record yes or no data on compliance for each trial. A trial begins when the if-then prompt is delivered and compliance is defined as initiating the behavior within 10 sec from the time the prompt is presented.
Make separate graphs for each target food with the independent variable being the session (i.e., 5 trials) and the dependent variable the percent compliance for the session. Enter the percent compliance in spreadsheet in order to create a graphical display of the session data in a spreadsheet. Enter the data into columns.
Then select the data, click Insert then Chart. When the chart choices are presented select the marked line chart choice. Draw vertical lines between the phases of the procedure. Insert a text box with the label “baseline” above the data for the baseline sessions.
Insert a text box with a number corresponding to the step of the procedure at the top of the figure for each step of the procedure. Place a label at the top of the chart denoting which food is being displayed (e.g., “100% food”, “80% food). Copy and paste the first chart at the top of a blank page and copy and paste the subsequent charts below in order.
Representative Results
The procedure of shaping and sequential presentation described can result in initial compliance with behaviors related to eating (e.g., touching the food) that can be strengthened through the use of reinforcement and shaping. By reinforcing successive approximations (shaping steps) behavior can be shaped slowly until reaching the target behavior of eating. The results depicted in Figure 1 show that the technique of shaping is capable of increasing compliance with food acceptance and the steps in the protocol that can ultimately lead to eating. The results also show that the simultaneous presentation procedure can be effective at increasing compliance when the shaping technique is not effective. These results show that when used together, the shaping and simultaneous presentation procedures are effective at increasing compliance with eating.
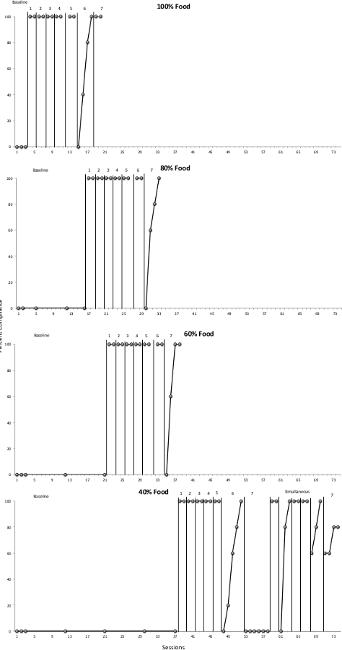 Figure 1. Compliance across baseline and shaping phases. The top panel shows compliance with food identified as likely to be eaten 100% of the time (training phase), the second panel shows compliance with food identified as likely to be eaten 80% of the time, the third panel shows compliance with food identified as likely to be eaten 60% of the time, and the third panel shows compliance with food identified as likely to be eaten 40% of the time. These data show the effects of the shaping procedure at increasing compliance across successive approximations to the target behavior of eating the food. These results can be seen for the first 3 foods (i.e., 100% food, 80% food and then 60% food). The fourth panel of Figure 1 (40% food) shows the results for a situation in which the shaping and sequential presentation procedure did not result in increases in compliance with the last step (i.e., eat). In these situations it is appropriate to use the shaping, sequential and simultaneous presentation procedure. The fourth panel shows compliance in the last step of the procedure (step 7: eat) after introducing the simultaneous presentation procedure. Please click here to view a larger version of this figure.
Figure 1. Compliance across baseline and shaping phases. The top panel shows compliance with food identified as likely to be eaten 100% of the time (training phase), the second panel shows compliance with food identified as likely to be eaten 80% of the time, the third panel shows compliance with food identified as likely to be eaten 60% of the time, and the third panel shows compliance with food identified as likely to be eaten 40% of the time. These data show the effects of the shaping procedure at increasing compliance across successive approximations to the target behavior of eating the food. These results can be seen for the first 3 foods (i.e., 100% food, 80% food and then 60% food). The fourth panel of Figure 1 (40% food) shows the results for a situation in which the shaping and sequential presentation procedure did not result in increases in compliance with the last step (i.e., eat). In these situations it is appropriate to use the shaping, sequential and simultaneous presentation procedure. The fourth panel shows compliance in the last step of the procedure (step 7: eat) after introducing the simultaneous presentation procedure. Please click here to view a larger version of this figure.
Discussion
This paper presents a treatment package composed of antecedent manipulations that have demonstrated success in increasing food acceptance for children who exhibit food selectivity. Notably, this paper presents a set of procedures that may be effective without the use of escape extinction. These methods are consistent with previous literature (Penrod et al., 2012) that suggests that a shaping procedure can be used to increase food acceptance with children who engage in active food refusal (e.g., throwing food and gagging) without having to implement escape extinction procedures.
A critical component of the protocol is the shaping procedure. Shaping allows clinicians to reinforce behaviors that are easier for the individual to comply with, and then reinforce successive approximations to the target behavior of eating. Another critical component of the protocol is simultaneous presentation. Simultaneous presentation allows clinicians to overcome compliance issues that were not successfully addressed with the shaping procedure. Simultaneous presentation provides an alternative tool to improve compliance without the use of the escape extinction procedure.
This paper extends the literature on the treatment of food selectivity by presenting a treatment package that incorporated the use of sequential and simultaneous presentation procedures along with a reinforcement procedure. This treatment package may provide an alternative intervention when escape extinction is not warranted. Although, social validity was not directly assessed anecdotally parents reported that they liked the procedure and were happy with the results.
It should be noted that although the sequential presentation procedure may be effective in increasing food acceptance for some foods, it may not be effective for all participants or for all foods. One possible limitation of the procedure is that shaping and sequential presentation of the target food may not be effective for all cases. In cases where shaping and sequential presentation are not effective, a simultaneous presentation phase can be used as a modification to the shaping procedure. The shaping procedure is designed to introduce the non-preferred food gradually however; some foods may require an even slower and more progressive introduction to the non-preferred food. Specifically, the simultaneous presentation procedure may allow the child to become habituated to the taste and texture of the non-preferred food more slowly and increase food acceptance by gradually exposing the child to greater amounts of the non-preferred food.
Although this may be a limitation of the shaping procedure, the treatment package described addresses this limitation and presents a treatment package that may have real practical and clinical significance in the treatment of feeding issues related to food selectivity. Future studies should further evaluate this procedure for other populations of children and adults with similar issues as well as evaluate additional procedures that may improve the efficiency and effectiveness of the current protocol.
Disclosures
The authors declare that they have no competing financial interests.
Acknowledgments
The authors wish to acknowledge the support of Florida International University and the Center for Children and Families.
References
- Ahearn WH, Kerwin ME, Eicher PS, Shantz J, Swearingin W. An alternating treatments comparison of two intensive interventions for food refusal. Journal of Applied Behavior Analysis. 1996;29(3):321–332. doi: 10.1901/jaba.1996.29-321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandini LG, Anderson SE, Curtin C, Cermak S, Evans EW, Scampini R, Must A. Food selectivity in children with autism spectrum disorders and typically developing children. The Journal of Pediatrics. 2010;157(2):259–265. doi: 10.1016/j.jpeds.2010.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bachmeyer MH. Treatment of selective and inadequate food intake in children: A review and practical guide. Behavior Analysis in Practice. 2009;2(1):43–50. doi: 10.1007/BF03391736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cermak SA, Curtin C, Bandini LG. Food selectivity and sensory sensitivity in children with autism spectrum disorders. Journal of the American Dietetic Association. 2010;110(2):238–246. doi: 10.1016/j.jada.2009.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper LJ, Wacker DP, Brown K, McComas JJ, Peck SM, Drew J, Asmus J, Kayser K. Use of concurrent operants paradigm to evaluate positive reinforcers during treatment of food refusal. Behavior Modification. 1999;23(1):3–40. doi: 10.1177/0145445599231001. [DOI] [PubMed] [Google Scholar]
- Dawson JE, Piazza CC, Sevin BM, Gulotta CS, Lerman D, Kelley ML. Use of the high-probability instructional sequence and escape extinction in a child with food refusal. Journal of Applied Behavior Analysis. 2003;36(1):105–108. doi: 10.1901/jaba.2003.36-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dovey TM, Staples PA, Gibson EL, Halford JCG. Food neophobia and 'picky/fussy eating in children: A review. Appetite. 2008;50:181–193. doi: 10.1016/j.appet.2007.09.009. [DOI] [PubMed] [Google Scholar]
- Kern L, Marder TJ. A comparison of simultaneous and delayed reinforcement as treatments for food selectivity. Journal of Applied Behavior Analysis. 1996;29(2):243–246. doi: 10.1901/jaba.1996.29-243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ledford JR, Gast DL. Feeding problems in children with autism spectrum disorders: A review. Focus on Autism and Other Developmental Disabilities. 2006;21(3):153–166. [Google Scholar]
- Munk DD, Repp AC. Behavioral assessment of feeding problems of individuals with severe disabilities. Journal of Applied Behavior Analysis. 1994;27(2):241–250. doi: 10.1901/jaba.1994.27-241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel MR, Piazza CC, Martinez CJ, Volkert VM, Santana CM. An evaluation of two differential reinforcement procedures with escape extinction to treat food refusal. Journal of Applied Behavior Analysis. 2002;35(4):363–374. doi: 10.1901/jaba.2002.35-363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penrod B, Gardella L, Fernand J. An evaluation of a progressive high-probability instructional sequence combined with low probability demand fading in the treatment of food selectivity. Journal of Applied Behavior Analysis. 2012;45(3):527–537. doi: 10.1901/jaba.2012.45-527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piazza CC, Patel MR, Santana CM, Goh H, Delia MD, Lancaster BM. An evaluation of simultaneous and sequential presentation of preferred and non-preferred food to treat food selectivity. Journal of Applied Behavior Analysis. 2002;35(3):259–270. doi: 10.1901/jaba.2002.35-259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pizzo B, Coyle M, Seiverling L, Williams K. Plate a-plate b: Use of sequential presentation in the treatment of food selectivity. Behavioral Interventions. 2012;27:175–184. [Google Scholar]
- Tarbox J, Schiff A, Najdowski AC. Parent-Implemented procedural modification of escape extinction in the treatment of food selectivity in a young child with autism. Education and Treatment of Children. 2010;33(2):223–234. [Google Scholar]


