Abstract
Chronic, unresolved stress is a major risk factor for the development of clinical depression. While many preclinical models of stress-induced depression have been reported, the unpredictable chronic mild stress (UCMS) protocol is an established translationally-relevant model for inducing behavioral symptoms commonly associated with clinical depression, such as anhedonia, altered grooming behavior, and learned helplessness in rodents. The UCMS protocol also induces physiological (e.g., hypercortisolemia, hypertension) and neurological (e.g., anhedonia, learned helplessness) changes that are clinically associated with depression. Importantly, UCMS-induced depressive symptoms can be ameliorated through chronic, but not acute, treatment with common SSRIs. As such, the UCMS protocol offers many advantages over acute stress protocols or protocols that utilize more extreme stressors. Our protocol involves randomized, daily exposures to 7 distinct stressors: damp bedding, removal of bedding, cage tilt, alteration of light/dark cycles, social stresses, shallow water bath, and predator sounds/smells. By subjecting rodents 3-4 hr daily to these mild stressors for 8 weeks, we demonstrate both significant behavioral changes and poor health outcomes to the cardiovascular system. This approach allows for in-depth interrogation of the neurological, behavioral, and physiological alterations associated with chronic stress-induced depression, as well as for testing of new potential therapeutic agents or intervention strategies.
Keywords: Behavior, Issue 106, Models of Clinical Depression, Models of Chronic Stress, cortisol, anhedonia, learned helplessness, behavioral impairments
Introduction
Depressive mental illness is a complex neurological disorder that is currently recognized as a leading cause of disability and disease burden worldwide. The NIMH reports that approximately 12% of Americans suffer from clinical depression, with twice as many women affected versus men1. In the US alone, depression accounts for billions of dollars direct healthcare costs and an estimated $193 billion more in indirect costs (lowered earnings and lost productivity)2. Symptoms of depression include anhedonia, changes in weight and sleep cycles, decreased physical activity and personal hygiene, feelings of hopelessness or guilt, and/or reoccurring thoughts of death or suicide. During the last decade, epidemiologic and clinical studies have indicated that depression is an independent risk factor for cardiovascular disease (CVD) morbidity and mortality3, and is predictive of more severe prognosis of cardiovascular pathologies, including atherosclerosis, hypertension, myocardial infarction, and coronary artery disease, regardless of prior history of overt CVD4. Despite the increasing prevalence and adverse public health impact of depression, the etiology and related pathophysiology of this disease is poorly understood and the heterogeneity of the disorder due to various factors (e.g., genetic, biological, and environmental components) has made clinical diagnosis difficult to define.
Evidence indicates that irresolvable psychological stress is a major contributing factor for developing depressive illnesses and may also be a potent pathogenic factor linking depression and CVD, in part due to disruption and dysregulation of the hypothalamic-pituitary-adrenal (HPA) axis5,6. Dysfunction of the HPA axis is a major mechanism that has been linked to the behavioral and physiological changes observed in depression and the development of several CVD risk factors, including dyslipidemia, obesity, and diabetes7. Multiple preclinical models of depression have been developed in attempt to replicate the mechanism of altered HPA axis activity characteristic of clinical depression; such models provide a validated means for investigating the behavioral, neurological, and physiological changes associated with chronic and acute stress in animals. The validity of an animal model of disease is based on the relevance of the etiology and progression of the model design and its ability to recapitulate anatomical, neurophysiological, and behavioral features observed in human disease. In addition, preclinical responses to treatments (such as SSRIs) should yield similar results to those observed in clinical settings.
Several animal models of stress-induced depression are currently utilized in research, such as learned helplessness, early life stress, and social defeat stress. However, each of these models has inherent disadvantages that lessen their translational efficacy8. Within the last decades, the Unpredictable Chronic Mild Stress (UCMS) protocol has emerged as one of the most translationally-relevant models for studying the pathophysiology of depression in rodents9. This model is based on the fundamental concept that chronic exposure to stressors disrupts stress response systems and ultimately leads to the development of depressive disorders. During the UCMS protocol, animals are exposed to a randomized series of mild environmental and social stressors on a daily basis. A crucial factor that enhances the relevance of this model to human situations lies in the high degree of unpredictability and uncontrollability of the stressors, as well as the time at which they are introduced. Additionally, the UCMS protocol uses only mild stressors, instead of relying on early life or aggressive physical stimuli. Over a period of UCMS exposure, depressive behaviors develop and are comparable to clinical symptoms, including decreased responsiveness to rewards (anhedonia), changes in physical activity and investigative behavior (helplessness and despair), deterioration of the coat state and altered sexual activity10. Almost all demonstrable symptoms of depression have been reported using this model, and studies have demonstrated that these behaviors persist for several weeks following the cessation of stress. In addition, these UCMS-induced depressive behaviors can gradually be revered by chronic, but not acute, treatment with particular antidepressants, suggesting similar neurological effects of therapeutic improvement that closely mirrors the clinical action and variable efficacy of these agents in humans11,14-18 . Here, we report a detailed description of the UCMS protocol and describe typical behavioral and vascular outcomes in mice.
Protocol
All procedures described below have been reviewed and approved by the Institutional Animal Care and Use Committee at the West Virginia University Health Sciences Center.
1. Selection of Animal Model
NOTE: Most commonly used species in the UCMS model include Sprague Dawley, and Wistar rats and the BALB/cJ mouse; other murine models have shown limited efficacy (DBA/2, C57BL/6). However, careful consideration should be given to the particular mouse or rat strain of choice, as the genetic background and susceptibility to environmental stressors vary widely among species and have been shown to be critical factors affecting the outcomes of the study11,14,15,19.
Use animals of the appropriate age (e.g., if the desired endpoint is to be evaluated in a 17-week old rat, then the rats must start the UCMS protocol at ~9 weeks of age) as this protocol takes at least 7-9 weeks to fully induce depressive symptoms.
Single-house animals undergoing UCMS in IACUC-approved cages and facilities, with food and standard chow available ad libitum (unless otherwise required by specific protocol).
Take special care to ensure controls are housed in a quiet room with minimal activity to reduce effects of any possible unknown environmental stressors.
2. Unpredictable Chronic Mild Stress Protocol
NOTE: Animals undergoing UCMS are transported daily (>5 days per week) to a clean room used for UCMS manipulations. Animals are exposed to 1 or 2 of the stressors listed below each day. Stressors are performed on a randomized schedule, and each stress is administered for a minimum of 3-4 hr (see Table 1).
Dampen the bedding by pouring 10-20 oz. of clean water into each standard cage. Adjust the amount of water accordingly to the size of the cage in order to fully dampen the bedding but not to cause pooling of water. Reside the animals in damp cage for 3-4 hr.
Remove bedding from each cage for 3-4 hr, after which animals are transitioned into another stressor requiring an empty cage (shallow bath, cage tilt) or placed into a clean cage with fresh bedding.
Tilt cages to approximately 45° (without bedding) for 3-4 hr. Cages can be tilted with a sturdy object that will remain in place as the animal moves around in the cage.
Alter normal 12 hr/12 hr light/dark cycles into successions of 30 min periods lasting for 8 hr. After, return animals to the normal cycle.
Transfer each animal from its home cage to that of the cage of a neighboring animal that has been removed for 3 hr.
Remove all bedding from each cage and add water to a depth of ~0.25 inches for mice or ~0.5 inches for rats for approximately 4 hr. Use water that is warmer than RT (~30 °C) to minimize hypothermia potential. Briefly dry animals with a soft towel at the conclusion of the water exposure prior to placement into clean cages.
Expose animals to predator smells/sounds by adding randomly distributed sample tufts of fur or urine (10-20 ml) from a natural predator species into the cage for 3-4 hr. Alternatively, play growling or predatory noises from natural predator species in close proximity to cages for 3 hr.
At the end of each daily stress period, place all animals into clean cages and return them to the housing facility.
3. Animal Monitoring/Grooming Scores
- Inspect each animal daily for the development of wounds or sores that may require veterinary treatment. Animals that develop mild injuries may continue in the UCMS protocol on the consent of the veterinarian.
- Two investigators trained in evaluating coat grooming inspect each animal and assign a weekly coat score on a scale of 0-1. This score is determined by assigning individual scores (0- clean, 1-dirty) to each of 8 body regions- head, neck, dorsal coat, ventral coat, tail, forelimbs, hind limbs, and genital region. The same investigators are to perform this task throughout the UCMS protocol to maintain consistency in assigning coat scores.
- Any animal that experiences a sharp reduction in body weight (i.e., >15%) should be reported to the veterinary staff and must be removed from the protocol.
4. Behavioral Testing and Outcome Measurements
NOTE: Several methods of assessment can be used to quantify behavioral changes from the UCMS protocol in rodents.
- Cumulative Coat Grooming Score.
- As described above, a weekly coat grooming score is assigned for each animal.
- Sucrose Splash Test:
- Place the animal in a clean cage lined with an cotton pad or towel to prevent bedding from adhering to its coat. Spray a 10% sucrose solution onto the head and dorsal coat of each animal and record total grooming behavior for 5 min.
- Grooming activity (defined as cleaning of the fur by licking or scratching) is measured by latency (idle time between the first spray and initiation of grooming) and frequency (number of times grooming a particular body part).
- Sucrose Preference Test:
- Habituate animals to drink 1% sucrose solution (w/v) 72 hr before the test and then provide exposure to two bottles (1% sucrose solution versus tap water in different bottles). After habituation, provide animals with ad libitum access to sucrose solution and tap water for 3 hr. After 3 hr record the consumption volumes of sucrose solution and tap water and calculate sucrose preference as: [(sucrose consumption)/(water consumption + sucrose consumption)]×100.
- Tail Suspension Test (Mice Only):
- Suspend mice by the tail from a stable rod (20 cm from the floor) using adhesive tape (2 cm from tip of tail). Record immobility time over 5 min. Mice are considered immobile only when they hang passively and completely motionless.
- The Forced Swim Test:
- Place animals in a container (~15-20 cm diameter for mice; ~55-60 cm diameter for rats) filled with water at a temperature of 26 ± 0.5 °C. Record the latency to the first bout of mobility and the time spent immobile during the 5-min testing period. At the end of a test, place the wet animal in a holding cage on a heating pad (30–35 °C) with normal bedding covered by an absorbent paper towel until dry.
- Elevated Plus Maze:
- Allow each animal to explore the maze freely for 5 min. Record total entries into each arm, and total time spent in each arm, according to a priori criteria20.
- Locomotor Activity:
- Record activity levels, defined as overall movement, fine movements, rearing movements, and inactivity, for both acute (30 min) and/or chronic (12 hr) time periods. Do this using the home cage or a novel environment, depending on the individual environment (although consistency should be maintained) in real time by an observer or post-hoc by replaying and analyzing camera footage.
5. Expansion/Variation of UCMS Protocol
Administer appropriate therapeutic agents or challenges to study their ability to either blunt the development of UCMS-induced outcomes (if initiated early) or to reverse severity of established UCMS-induced outcomes (if initiated late). This is dependent on the individual laboratory or protocol11.
6. Final Outcome Assessments
Following the conclusion of UCMS protocols and behavioral testing, utilize animals in subsequent experiments in a manner that addresses the specific hypotheses, aims or goals of the individual laboratory. NOTE: As examples, this can include cardiovascular, inflammatory or endocrine responses to chronic stress. Alternatively, therapeutic interventions can be introduced at this point to evaluate their effectiveness and mechanistic underpinnings.
Representative Results
An example of the schedule for one week following the UCMS procedure is shown in Table 1. Each week, stressors were randomized to prevent acclamation and to ensure unpredictability of the stress challenge each day.
Measures of Depressive like Behaviors
Following 8 weeks of UCMS, there were significant alterations to both behavioral and physiological outcomes in chronically stressed rodents relative to their non-stressed control strains. Development of depressive like symptoms following UCMS was assessment via coat score, sucrose splash test, and tail suspension (mice only; references12,13). A progressive decline in coat grooming scores was observed in all UCMS animals (Figure 1, Panel A), and this marked degradation in the physical state of the coat suggests decreased grooming activity. This behavior may parallel the lack of motivation to or loss of interest in performing everyday tasks, such as the maintenance of minimal personal care.
UCMS animals also demonstrated an increased latency to groom and reduced total grooming time in the sucrose splash test (Figure 1, Panels B and C). Increased time to initiate grooming behavior along with decreased time spent grooming is associated with reduced motivation and a decline in self stimulatory behavior, or reduced sensitivity to pleasure. This is representative of the core symptom of depression, anhedonia. In addition, there was a significant increase in the immobility time during the tail suspension test in mice. As stated previously, this behavior is a measure of behavioral despair with greater immobility representing a more severe depressive like symptom.
Measures of Physiological Changes
MAP can be significantly elevated as a result of the UCMS protocol, but this is not consistently observed (Table 1). A significant reduction in the dilator response to methacholine was observed in the aortic rings of UCMS BALB/cJ mice compared to controls (Figure 2). This increased shift towards blunted dilator responses is observed in clinical cases of increased risk for development of cardiovascular disease.
UCMS mice manifested increased plasma levels of cortisol, a marker of chronic physiological stress, and nitrotyrosine, a marker of chronic oxidative stress (Table 2).
Additionally, UCMS mice showed significantly elevated levels of the pro-inflammatory markers TNF-α and MCP-1. Together, these results suggest that stressed animals develop a pathophysiological disease profile following 8 weeks of UCMS (Table 2).
Divergence with Sex
Recent evidence has suggested that there is a substantial quantitative divergence in the responses to UCMS between male and female mice (13). Specifically, data suggest that female mice, exposed to the identical UCMS protocol as age-matched males, develop more severe behavioral responses to the protocol than do males (Table 3 and Figure 3), with elevated levels of cortisol, nitrotyrosine and markers of inflammation.
However, despite this divergence between sexes following the UCMS protocol, the vasculopathy that develops as a result appears to be blunted in the female sex as compared to the males, strongly suggesting a superior maintenance of endothelial function, despite the compromised environment (Figure 4).
For Figures 1 and 3, results were obtained using the techniques described above, with the application of ANOVA and t-tests as appropriate. For Figures 2 and 4, results were obtained using concentration-response relationships in ex vivo aortic ring preparations. Curves were fit with a three parameter logistic equation, with ANOVA and t-tests as appropriate for the lower bounds of the curves. Please see references12,13 for details.
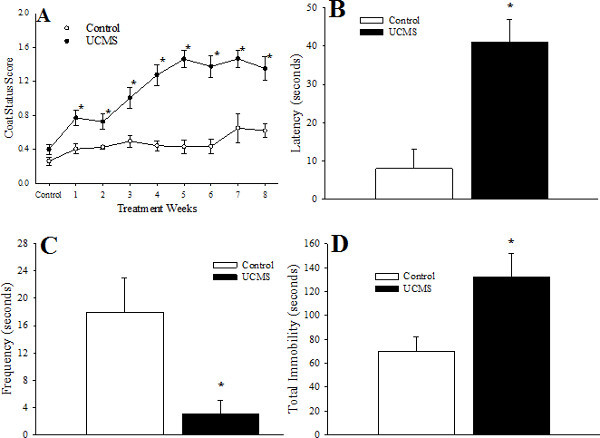 Figure 1. Depressive Symptoms Following Eight Weeks of UCMS in Mice. Data are presented for coat status (Panel A), the latency (Panel B) and frequency (Panel C) of facial grooming following a 10% sucrose solution spray, and the total period of immobility during the tail suspension test (Panel D) for control and UCMS mice. * p <0.05 versus control.Please see reference12 for details. Please click here to view a larger version of this figure.
Figure 1. Depressive Symptoms Following Eight Weeks of UCMS in Mice. Data are presented for coat status (Panel A), the latency (Panel B) and frequency (Panel C) of facial grooming following a 10% sucrose solution spray, and the total period of immobility during the tail suspension test (Panel D) for control and UCMS mice. * p <0.05 versus control.Please see reference12 for details. Please click here to view a larger version of this figure.
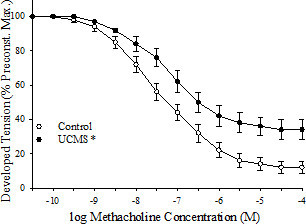 Figure 2. Vasodilator Responses to Methacholine from Mice Following Eight Weeks of UCMS. Data are presented for mice under control conditions (control lower bound = 10.3 ± 2.4%) and following eight weeks of the imposed UCMS protocol (UCMS lower bound = 33.6 ± 4.4%). * p <0.05 versus responses in untreated vascular rings from control mice. Re-printed from reference12 with permission. Please click here to view a larger version of this figure.
Figure 2. Vasodilator Responses to Methacholine from Mice Following Eight Weeks of UCMS. Data are presented for mice under control conditions (control lower bound = 10.3 ± 2.4%) and following eight weeks of the imposed UCMS protocol (UCMS lower bound = 33.6 ± 4.4%). * p <0.05 versus responses in untreated vascular rings from control mice. Re-printed from reference12 with permission. Please click here to view a larger version of this figure.
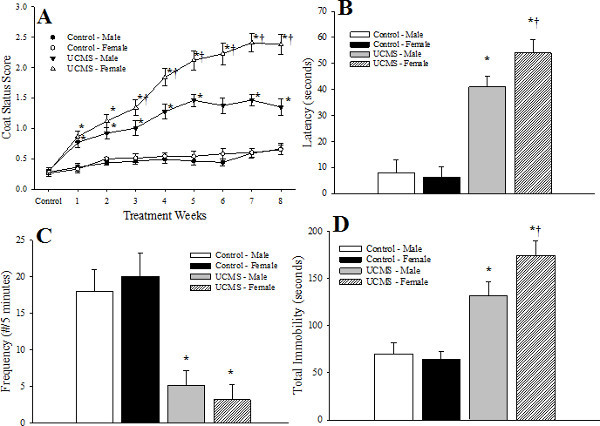 Figure 3. Differences in Depressive Symptoms Following Eight Weeks of UCMS in Male and Female Mice. Data are presented for coat status (A), the latency (B) and frequency (C) of facial grooming following a 10% sucrose solution spray, and the total period of immobility during the tail suspension test (D) for control and UCMS mice. * p <0.05 versus Control in the sex; † p <0.05 versus UCMS-Male. Re-printed from reference13 with permission. Please click here to view a larger version of this figure.
Figure 3. Differences in Depressive Symptoms Following Eight Weeks of UCMS in Male and Female Mice. Data are presented for coat status (A), the latency (B) and frequency (C) of facial grooming following a 10% sucrose solution spray, and the total period of immobility during the tail suspension test (D) for control and UCMS mice. * p <0.05 versus Control in the sex; † p <0.05 versus UCMS-Male. Re-printed from reference13 with permission. Please click here to view a larger version of this figure.
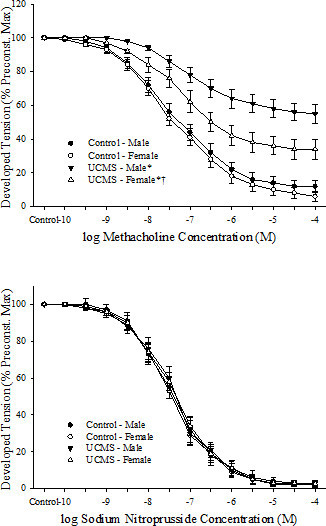 Figure 4. Differences inVasodilator Responses from Male and Female Mice Following Eight Weeks of UCMS. Dilator responses of aortic rings to increasing concentrations of methacholine (upper panel) and sodium nitroprusside (lower panel) from mice under control conditions and after eight weeks of UCMS. * p <0.05 versus Control in the sex; † p <0.05 versus UCMS-Male. Re-printed from reference13 with permission. Please click here to view a larger version of this figure.
Figure 4. Differences inVasodilator Responses from Male and Female Mice Following Eight Weeks of UCMS. Dilator responses of aortic rings to increasing concentrations of methacholine (upper panel) and sodium nitroprusside (lower panel) from mice under control conditions and after eight weeks of UCMS. * p <0.05 versus Control in the sex; † p <0.05 versus UCMS-Male. Re-printed from reference13 with permission. Please click here to view a larger version of this figure.
| Sunday | Monday | Tuesday | Wednesday | Thursday | Friday | Saturday | |
| Stressor 1 | Alter Light/Dark | Social Stress | No bedding | Damp Bedding | Alter light/dark | Predator sounds | Social Stress |
| Stressor 2 | Alter Light/Dark | Cage Tilt | Shallow Bath | Cage Tilt | Social Stress | Shallow Bath |
Table 1. Two sample weeks for imposition of unpredictable chronic mild stress (UCMS) protocol.
| Control | UCMS | |
| Mass (g) | 31 ± 2 | 29 ± 4 |
| MAP (mmHg) | 84 ± 5 | 93 ± 4 |
| Insulinplasma (ng/ml) | 1.3 ± 0.2 | 3.9 ± 0.6* |
| Glucoseblood (mg/dl) | 102 ± 8 | 104 ± 7 |
| Cholesterolplasma (mg/dl) | 75 ± 8 | 81 ± 8 |
| Triglyceridesplasma (mg/dl) | 102 ± 8 | 128 ± 10* |
| Nitrotyrosineplasma (ng/ml) | 17 ± 2 | 27 ± 4* |
Table 2.Baseline characteristics between mouse groups under control conditions and following 8 weeks of UCMS. All mice are aged 17-18 weeks. * p <0.05 versus control. Modified from reference12.
| Males | Females | UCMS-Males | UCMS-Females | |
| Mass (g) | 29 ± 2 | 28 ± 3 | 30 ± 3 | 29 ± 4 |
| MAP (mmHg) | 87 ± 4 | 91 ± 4 | 94 ± 5 | 90 ± 5 |
| Insulinplasma (ng/ml) | 1.1 ± 0.3 | 1.2 ± 0.4 | 4.1 ± 0.7* | 4.5 ± 0.5* |
| Glucoseblood (mg/dl) | 82 ± 7 | 80 ± 8 | 94 ± 8 | 101 ± 10 |
| Cholesterolplasma (mg/dl) | 71 ± 7 | 68 ± 8 | 78 ± 6 | 77 ± 10 |
| Triglyceridesplasma (mg/dl) | 94 ± 6 | 101 ± 8 | 109 ± 8 | 116 ± 12 |
| Nitrotyrosineplasma (ng/ml) | 12 ± 3 | 11 ± 4 | 29 ± 5* | 36 ± 6* |
| Cortisolplasma (pg/ml) | 12 ± 3 | 14 ± 4 | 29 ± 5* | 44 ± 4* |
| TNF-aplasma (pg/ml) | 2.3 ± 0.3 | 2.0 ± 0.2 | 4.1 ± 0.4* | 6.4 ± 0.4*† |
| MCP-1plasma (pg/ml) | 2.8 ± 0.3 | 3.3 ± 0.5 | 10.2 ± 1.0* | 14.8 ± 1.3*† |
Table 3.Baseline characteristics between male and female mouse groups under control conditions and following 8 weeks of UCMS. All mice are aged 17-18 weeks. * p <0.05 versus control. Modified from reference13.
Discussion
Extensive clinical and epidemiological evidence has indicated that chronic stress is one of the most potent precipitating factors for depression. Repeated exposure to stressors may potentiate individual vulnerability to depression and other neuropsychiatric disorders as a consequence of the psychological and physical demands within the body that accumulate over time. The use of validated preclinical animal models offers a valuable translational tool for studying depression and comorbid diseases. Firstly, an ideal animal model offers an opportunity to understand molecular, genetic and epigenetic factors that may lead to depression. By using such models, the underlying mechanisms and the causal relationship between genetic or environmental alterations and depression can be investigated, potentially allowing a more thorough insight into the pathophysiology of depression. Secondly, validated, improved models of depression are an indispensable tool for identifying and evaluating novel therapeutics and treatments, an essential first step towards developing improved diagnostic and treatment options.
For many years, the UCMS model has been validated for use in psychological and behavioral studies as a translationally relevant rodent model for chronic stress, human depression and depressive symptoms, as it does an excellent job at reproducing clinical symptoms of human depression, including anhedonia and learned helplessness21. In addition, the temporal development of the depressive symptoms is also relevant for human disease conditions, as animals experiencing UCMS develop depressive symptoms over time in response to stress, which is considered to be more translationally relevant. The representative results reported here showcase the ability of this model to generate a symptomatic profile of depression, including both behavioral and physiological changes, in both a rat and mouse model. In addition, the severity of behavioral and physiological outcomes shows sex-specific differences that could potentially be used to study the pathological effects of stress on men and women21.
It should be pointed out that the outcome of stress exposure is influenced by several variables under experimental conditions, including the nature of the stress (physical/systemic vs. cognitive/psychological), the severity of the stress, and exposure parameters. Different techniques can be used to measure depression-like behaviors and physiological outcomes and vary results among investigators21. For example, evaluation of the end points of behavioral tests may be variable depending on the use of recording methods as well as inconsistent methodology and bias amongst individual investigators. The particular strain/species used is also critical, as they have been shown to possess differences in susceptibility to UCMS. Further, other issues, such as the degree of control an animal has over stress exposure and the predictability of the stressor have been demonstrated to be important to the outcomes of the UCMS model, as greater unpredictability can reduce the probability of adaptive processes occurring upon repeated stress exposure and promote the appearance of stress effects on physiological and behavioral functions21.
Disclosures
The authors have nothing to disclose.
Acknowledgments
This study was supported by the American Heart Association (IRG 14330015, PRE 16850005, PRE 20380386, EIA 0740129N), and the National Institutes of Health (RR 2865AR; P20 RR 016477).
References
- NIMH Statistical Pages (Depression; Prevalence) 2014. [cited 2014 Dec 26]. Available from: http://www.nimh.nih.gov/health/statistics/prevalence/major-depression-among-adults.shtml.
- NIMH Statistical Pages (Depression; Costs) 2014. [cited 2014 Dec 26]. Available from: http://www.nimh.nih.gov/health/statistics/cost/index.shtml.
- Lett HS, et al. Depression as a risk factor for coronary artery disease: evidence, mechanisms, and treatment. Psychosom Med. 2004;66(3):305–315. doi: 10.1097/01.psy.0000126207.43307.c0. [DOI] [PubMed] [Google Scholar]
- Plante GE. Depression and cardiovascular disease: a reciprocal relationship. Metabolism. 2005;54:45–48. doi: 10.1016/j.metabol.2005.01.013. [DOI] [PubMed] [Google Scholar]
- Pizzi C, Manzoli L, Mancini S, Bedetti G, Fontana F, Costa GM. Autonomic nervous system, inflammation and preclinical carotid atherosclerosis in depressed subjects with coronary risk factors. Atherosclerosis. 2010;212(1):292–298. doi: 10.1016/j.atherosclerosis.2010.04.038. [DOI] [PubMed] [Google Scholar]
- Barden N. Implication of the hypothalamic-pituitary-adrenal axis in the physiopathology of depression. J Psychiatry Neurosci. 2004;29(3):185–193. [PMC free article] [PubMed] [Google Scholar]
- Bowman RE, Beck KD, Luine VN. Chronic stress effects on memory: sex differences in performance and monoaminergic activity. Horm Behav. 2003;43:48–59. doi: 10.1016/s0018-506x(02)00022-3. [DOI] [PubMed] [Google Scholar]
- Baune BT, et al. The relationship between subtypes of depression and cardiovascular disease: a systematic review of biological models. Transl Psychiatry. 2012;2:e92. doi: 10.1038/tp.2012.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Leary OF, Cryan JF. Towards translational rodent models of depression. Cell Tissue Res. 2013;354(1):141–153. doi: 10.1007/s00441-013-1587-9. [DOI] [PubMed] [Google Scholar]
- Mineur YS, Belzung C, Crusio WE. Effects of unpredictable chronic mild stress on anxiety and depression-like behavior in mice. Behav Brain Res. 2006;175(1):43–50. doi: 10.1016/j.bbr.2006.07.029. [DOI] [PubMed] [Google Scholar]
- Yalcin I, Belzung I, Surget A. Mouse strain differences in the unpredictable chronic mild stress: a four-antidepressant survey. Behav Brain Res. 2008;193(1):140–143. doi: 10.1016/j.bbr.2008.04.021. [DOI] [PubMed] [Google Scholar]
- d'Audiffret AC, Frisbee SJ, Stapleton PA, Goodwill AG, Isingrini E, Frisbee JC. Depressive behavior and vascular dysfunction: a link between clinical depression and vascular disease. J Appl Physiol. 2010;108(5):1041–1051. doi: 10.1152/japplphysiol.01440.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanley SC, Brooks SD, Butcher JT, d'Audiffret AC, Frisbee SJ, Frisbee JC. Protective effect of sex on chronic stress- and depressive behavior-induced vascular dysfunction in BALB/cJ mice. J Appl Physiol. 2014;117(9):959–970. doi: 10.1152/japplphysiol.00537.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ibarguen-Vargas Y, Surget A, Touma C, Palme R, Belzung C. Multifaceted strain-specific effects in a mouse model of depression and of antidepressant reversal. Psychoneuroendocrinology. 2008;33(10):1357–1368. doi: 10.1016/j.psyneuen.2008.07.010. [DOI] [PubMed] [Google Scholar]
- Dalla C, Pitychoutis PM, Kokras N, Papadopoulou-Daifoti Z. Sex differences in animal models of depression and antidepressant response. Basic Clin Pharmacol Toxicol. 2010;106(3):226–233. doi: 10.1111/j.1742-7843.2009.00516.x. [DOI] [PubMed] [Google Scholar]
- Mutlu O, Gumuslu E, Ulak G, Celikyurt IK, Kokturk S, Kır HM, Akar F, Erden F. Effects of fluoxetine, tianeptine and olanzapine on unpredictable chronic mild stress-induced depression-like behavior in mice. Life Sci. 2012;91(25-26):1252–1262. doi: 10.1016/j.lfs.2012.09.023. [DOI] [PubMed] [Google Scholar]
- Gumuslu E, Mutlu O, Sunnetci D, Ulak G, Celikyurt IK, Cine N, Akar F. The effects of tianeptine, olanzapine and fluoxetine on the cognitive behaviors of unpredictable chronic mild stress-exposed mice. Drug Res (Stuttg) 2013;63(10):532–539. doi: 10.1055/s-0033-1347237. [DOI] [PubMed] [Google Scholar]
- Isingrini E, Belzung C, Freslon JL, Machet MC, Camus V. Fluoxetine effect on aortic nitric oxide-dependent vasorelaxation in the unpredictable chronic mild stress model of depression in mice. Psychosom Med. 2012;74(1):63–72. doi: 10.1097/PSY.0b013e31823a43e0. [DOI] [PubMed] [Google Scholar]
- Ripoll N, David DJ, Dailly E, Hascoët M, Bourin M. Antidepressant-like effects in various mice strains in the tail suspension test. Behav Brain Res. 2003;143:193–200. doi: 10.1016/s0166-4328(03)00034-2. [DOI] [PubMed] [Google Scholar]
- Komada M, Takao K, Miyakawa T. Elevated plus maze for mice. J Vis Exp. 2008. p. 1088. [DOI] [PMC free article] [PubMed]
- Golbidi S, Frisbee JC, Laher I. Chronic stress impacts the cardiovascular system: animal models and clinical outcomes. Am. J. Physiol. Heart Circ. Physiol. 2015. [DOI] [PubMed]


