Abstract
Introduction
Benign neoplasms and hyperplastic tumorous lesions are common oral pathologies. These lesions require to be surgically removed by conventional surgery, laser, or electrosurgery. Surgical treatment aims at complete removal of pathological lesions and ensuring proper healing of the tissues to minimize the risk of lesion recurrence.
Aim
To present possible applications of Er:YAG and CO2 lasers in removal of benign neoplasms and tumorous lesions developing on oral mucosa as well as to specify indications and limitations of these two methods.
Material and methods
Temperature-induced injuries due to laser light application, possibility of post-operative histopathological evaluation of the removed tissue, efficacy of the cut and coagulation, healing process and completeness of laser surgeries give rise to our special concern.
Results
The main asset of the CO2 laser comparing to Er:YAG laser is an effective coagulation while thermal injury to the tissues is its limitation, especially with multiple passage of the beam and too high power applied. Er:YAG laser application does not exclude histopathological examination of the removed lesion tissue which is its advantage over CO2 laser.
Conclusions
Still, insufficient coagulation is a limitation ofits use in the case of richly vascularized lesions.
Keywords: CO2 laser, Er:YAG laser, oral benign lesions, oral hyperplastic lesions, surgical laser
Introduction
Benign neoplasms and hyperplastic tumorous lesions are common oral pathologies. Predisposing factors are prolonged mechanical irritation, habitual biting on the soft tissues, and injuries under the denture base. They are characterized by slow growth and clearly defined border. They are most common on the mucosa of the cheeks, tongue, alveolar processus of the maxilla and the A-H line on the palate. They are covered with acanthotic or hyperplastic epithelium which often becomes superinfected with bacteria or fungi. These lesions require to be surgically removed with conventional methods, lasers or electrosurgery. Surgical treatment aims at complete removal of pathological lesions and ensuring proper healing of the tissues to minimize the risk of lesion recurrence [1–3]. Though conventional surgery ensures complete removal of the lesion and makes histopathological evaluation of the removed tissue possible, post-operative tissue formation may promote recurrence of the lesions in some cases. Due to coagulation, laser surgery does not require post-operative suturing of the wound and thus does not produce any tissue changes.
Aim
The aim of the paper was to present and compare the results of treatment of benign neoplasms and tumorous lesions developing on the oral mucosa using Er:YAG and CO2 lasers. Basing on the photographic records of the chosen clinical cases, advantages and disadvantages of both lasers were described and indications for their use specified.
Material and methods
In the paper, clinical data of 75 patients (45 women and 30 men) aged 23–79 years (mean: 56.01) affected by benign neoplasms and tumorous lesions on the oral mucosa were used. The patients were qualified to a laser surgery, either with Er:YAG or CO2 laser. In 35 patients, procedures were performed using Er:YAG laser named 1243 K.E.Y. Laser 3 manufactured by (KaVo) (Germany) and a 2060 hand piece. K.E.Y. Laser 3 is Er:YAG laser of a 2.94 µm wave length, pulse energy up to 600 mJ, and pulse frequency of 1–25 Hz.Pilot beam emits the energy of 655 nm/1 mW. In the presented cases, multi-impulse radiation beam was used as well as energy of 300 mJ and frequency of 15 Hz designed for the extensive ablation program. The other laser type applied in 40 patients was CO2 laser, CTL 1401 model, manufactured by (Laser instruments Laser Technology Centre) (Poland). It emits 10600 nm wave length radiation in a continuous, single- or multi impulse mode, depending on the operator's needs. The beam power may be set from 0.5 to 12.0 W. A single impulse may last for 0.1 s or its multiple and may be repeated depending on the set frequency. In the presented cases, multi impulse radiation beam was used of the 0.1–0.2 s impulse wave, 2–4 Hz frequency and 5.0 W power to eliminate thermal injury to the surrounding tissues. All patients were operated on under local anesthesia with articaine (4% Ubistesin) or mepivacaine (3% Scandonest).
Results
Both types of lasers presented are an effective alternative to conventional surgical treatment. An important indication for their use is the removal of lesions located on such hard or otherwise difficult areas as the hard palate or maxillary alveolar process. Cutting the tissues, dissecting a flap and wound suturing are hard to perform there; however, post-operative tissue adaptation is greatly expected. Laser application shortens post-operative healing time and provides fast and good adaptation of soft tissues despite causing more extensive wounds than those which follow conventional surgery. The technique does not change the tissue profile and prevents post-operative scars formation what is of special importance in the case of prolonged irritation and habitual biting on the tissues. It may be considered a method of preventing formation and recurrence of benign tumors and tumorous lesions in the mouth. The best quality incision is achieved with the possibly highest frequency and lowest power of the laser beam. CO2 laser provides perfect hemostasis but with high power and multiple passage induces deep thermal injury to the tissues. The degree of thermal damage is increased inversely proportionally to the extent of lesion. Removal of very small changes carries the risk of such a significant thermal damage or defragmentation that their subsequent histopathological evaluation is not possible. For this reason, the use of CO2 laser requires very careful pre-operative macroscopic evaluation of the changes and should be performed by experienced clinicians. Therefore, the use of additional diagnostic methods such as dermatoscopy is advisable. Er:YAG laser compared to the CO2 laser does not always provide effective hemostasis but still does not cause such significant thermal damage even after repeated passage. Basing on evaporation, it is safe for the tissues undergoing surgery. Its low coagulatory properties hinder intraoperative assessment of changes and lengthen its duration. Worse insight into the operative field may adversely affect the completeness of the procedure. Constraints to its use include lesions of big diameters, richly vascularized ones, or those located in the richly vascularized regions such as the tongue or lips (Figures 1–6).
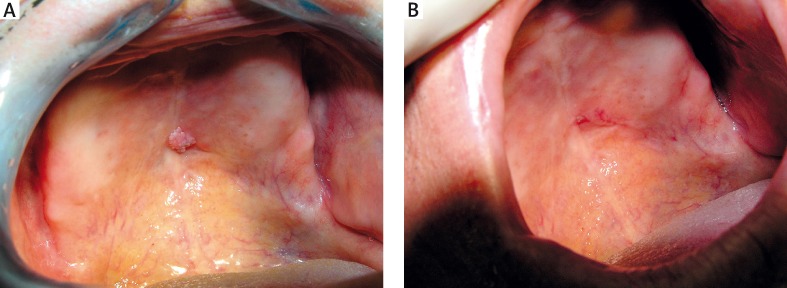
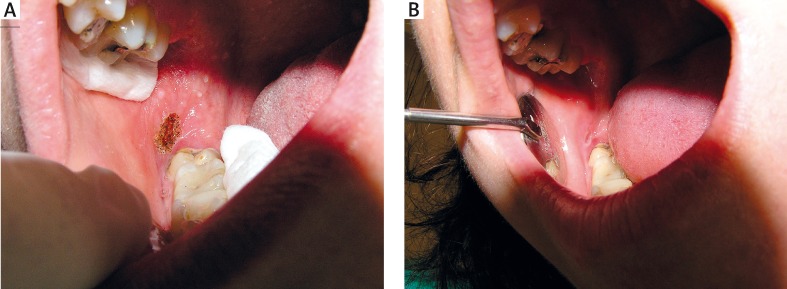
Figure 1.
A – Lesion on the palate. B – Seven days following CO2 laser surgery
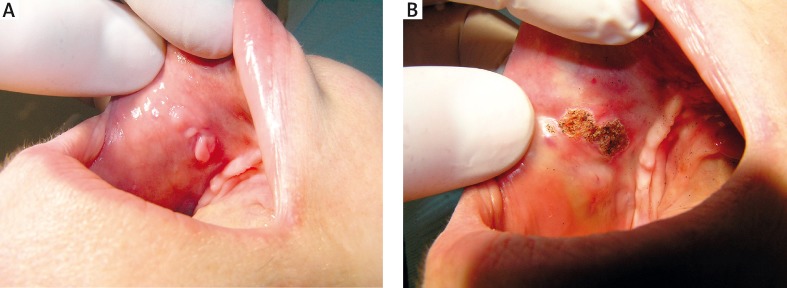
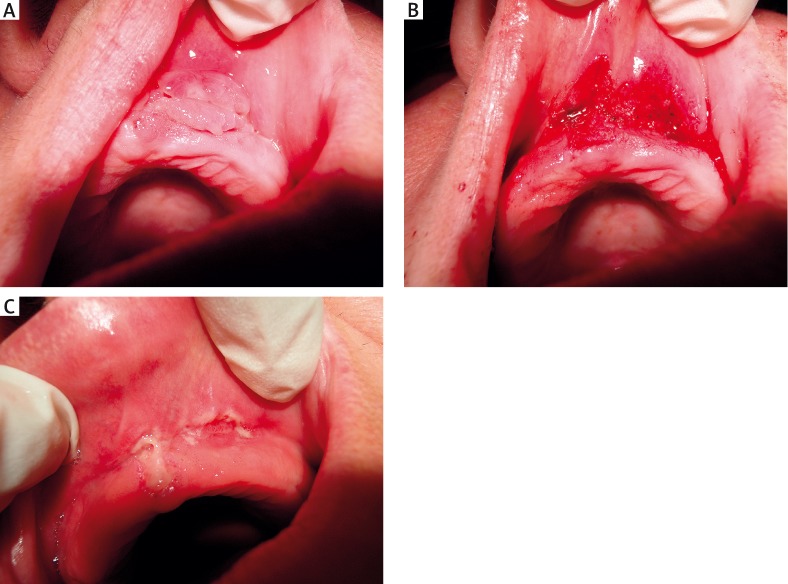
Figure 6.
A – Fibroma in A-H line of the palate. B – The condition following removal of fibroma with Er:YAG laser. C – Seven days after Er:YAG laser surgery of fibroma located in A-H line of the palate
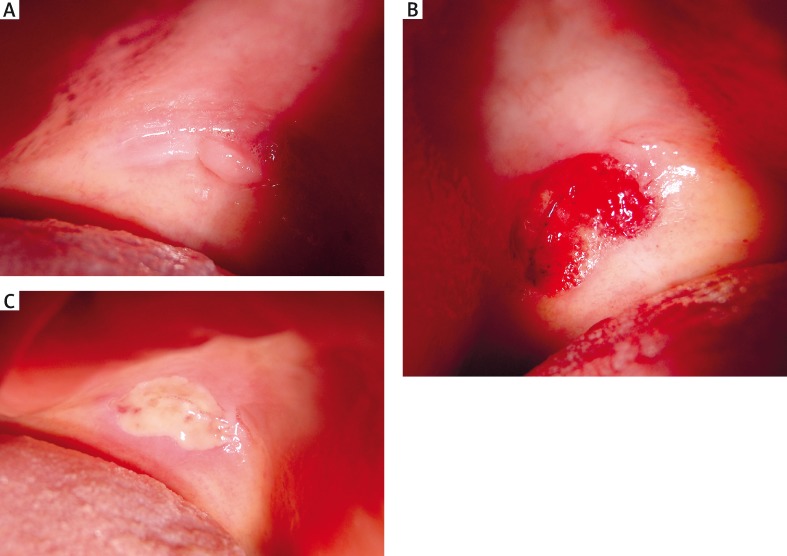
Figure 2.
A – Papilloma on the maxillary alveolar process. B – The condition after tissue removal with CO2 laser. C – The condition 7 days following surgery
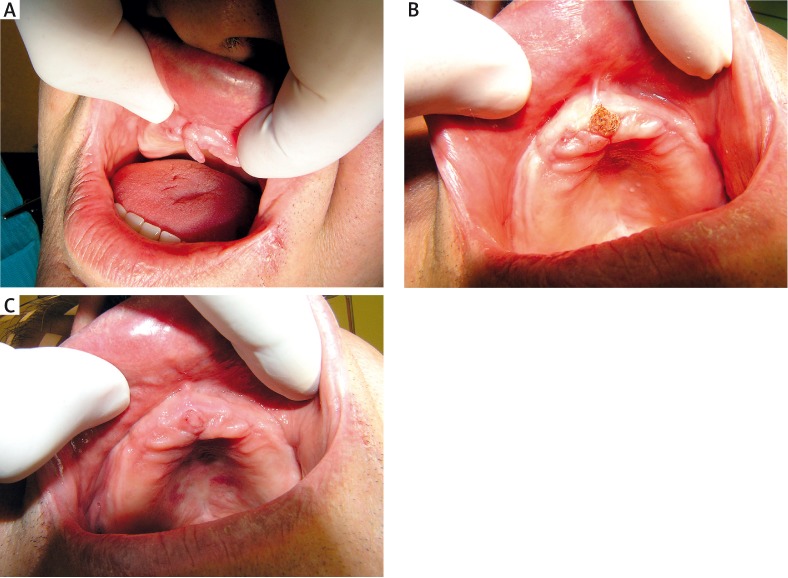
Figure 3.
A – Buccal fibroma. B – The condition following removal of tissues with CO2 laser
Figure 4.
A – The condition following removal of buccal lesion with CO2 laser. B – Seven days following surgery
Figure 5.
A – Fibroma on the maxillary alveolar processus before surgery. B – The condition following removal of fibroma with Er:YAG laser. C – Seven days after removal of fibroma with Er:YAG laser
Discussion
Since laser techniques were introduced, the number of indications for their use has been constantly growing. With the availability of numerous modifications, the number of contraindications and limitations to their use has significantly dropped. The greatest asset of CO2 laser was an effective coagulation of the operating field. However, significant thermal damage to the surrounding tissues limited the scope of its use. Oral soft tissues composed in 80% of water intensely absorb the light emitted by CO2 laser and prevent their deeper penetration. A recommended power of the laser light is 5–10 W for the oral mucosa as higher values may promote formation of scars, connective tissue adhesions and thermal damage [1]. Thermal damage results from conversion of light into heat, transmission of heat and tissue reaction to heat as well as exposure time. It also depends on the light power, wave length, exposure time and emission mode, beam profile, extent of lesion and its chemical and physical features [3]. Introducing high energy pulsed CO2 lasers (HEPCO2) has expanded the range of their use and minimized adverse thermal effects. The continuous laser enabled simultaneous cutting and coagulation. Its pulse mode promoted more extensive use of the ablation phenomenon in therapeutic and cosmetic procedures on the skin. To limit thermal damage to the tissues, laser target cells should absorb the emitted light better than the cells of the surrounding tissues. Laser light exposure time to the tissue undergoing surgery must be shorter than relaxation time defined as the time needed for the tissue to lose 50% of the heat. The third indispensable condition to counteract thermal damage is providing the target cells with an adequately high level of energy to induce ablation [4]. Minimizing thermal damage is of utmost importance for the long-lasting therapeutic effect as it counteracts scar and pigment changes formation. Comparing the extent of the skin thermal damage and the ablation extent of high energy pulsed CO2 laser and of pulse Er:YAG laser, similar ablation values were achieved – from 20 to 75 µm. As to the difference in the extent of thermal damage, the values of 10 to maximum 50 µm for Er:YAG laser and of 50 to 200 µm for CO2 laser were achieved. Er:YAG laser emits light of 2949 nm wavelength which is similar to the water absorption value (3000 nm), what results in almost complete absorption of light and significantly smaller thermal damage. Even multiple passage of the laser light emitted by Er:YAG laser through the tissues during surgery does not produce an increase in the thermal damage area. Water vaporization by Er:YAG laser reduces the temperature of the surrounding tissues, preventing collagen fiber shrinkage which appears at 55–60°C [4]. This desired feature of eliminating thermal damage was used in otosurgery. During stapedectomy, Er:YAG laser produced neither an increase in temperature of the inner ear fluid nor damage to the ciliated cells of the cochlea [5, 6]. It may be an effective alternative to CO2 laser in the middle ear surgery. Apart from high values of absorption and ablation, another feature of the CO2 laser is producing a change in the collagen fibers structure. On one hand, it negatively affects a long-term therapeutic effect by promoting scars, changes in pigmentation and adhesions of connective tissue. Still on the other hand, this feature is favorable when it comes to the oral mucosa as collagen fibers affected by laser light form a layer isolating the wound from irritation by oral fluids [1, 7, 8]. An advantage of lasers over conventional surgery is reducing pain during and after the procedure. It is due to insulating the nerve endings in the operative field, wound isolation, and prevention of tissue fluids penetration which initiate and back up the inflammatory phase [1, 2]. Elimination of pain in the postoperative period is also related to reduction in bacteremia and to laser cutting sterility [9]. Many hyperplastic changes operated on by us were caused by chronic irritation, or bad fitting removable prosthetic restorations. In such cases, the use of laser technology was the method of choice as it provided the best adaptation of the tissues operated on and minimal loss of the denture bearing area, especially in the vestibule of the mouth [1]. After conventional surgery of hyperplastic lesions, the biggest loss of the denture bearing area takes place within 6 weeks following a new prosthetic restoration. Within 72 h after CO2 laser surgery, a fibrin purulent membrane is formed that replaces the layer of radiation necrosis. After 2 weeks, the wound epithelium begins to form, gradually covering the entire circumference of the wound. The resulting epithelium is thinner and parakeratotic comparing to the tissue produced by a conventional surgery incision [1]. Advantages of CO2 laser were effective coagulation and no perioperative bleeding [10]. CO2 laser allows for closing blood vessels up to 0.5 mm in diameter, but it is also effective in the treatment of Osler-Weber-Rendu syndrome [3]. Coagulation achieved by the patients undergoing surgeries enabled no wound suturing and did not change the shape of the surrounding tissues. Er:YAG laser did not provide equally effective coagulation, what poses a significant inconvenience during the surgery. Large or richly vascularized changes limited the use of Er:YAG laser. Removing large, richly vascularized or non-stalked lesions required additional measures such as pressing or sewing, to ensure hemostasis in our patients. The most advanced effect of thermolysis is charring and melting of tissues. While comparing how effective both lasers were in removing neoplastic changes of the larynx, diffused charring of the tissue was found along the CO2 laser incision and no collagen fibers changes after Er:YAG laser application [11]. Summing up, Er:YAG laser was characterized by limited thermal damage, possibility of multiple passage through the tissues with complete light absorption and ablation value similar to that achieved with CO2 laser. Clinically, it results in shortening of post-operative healing time, reducing redness and swelling, and accelerating reepithelization. Mean reepithelization time for Er:YAG laser was 5.1 days and for CO2 laser 5.5 days [12–14]. Histological evaluation confirms a similar degree of thermal damage to produce similar mean tissue healing time and long-term effectiveness of the procedure. Our observations show that there were no differences in post-operative healing time except that the inflammatory phase was slightly more intense locally in the case of CO2 laser. It showed as swelling and wound margins reddening. Another important issue was surgery completeness and the ability to perform histopathological evaluation. Laser incision and thermal damage area did not exclude histopathological evaluation. The lesions removed by us were microscopically evaluated. However, our observations showed that in the case of small size lesions, their thermal damage and defragmentation did not allow histopathological evaluation to be performed. The greatest changes in the epithelium and interstitium were found in lesions not bigger than 7 mm in the diameter. The best quality cut and the least thermal damage was achieved with a high frequency and low power [3]. CO2 laser is used to prevent and treat non-pigmented skin neoplasms. Its efficacy to reduce atypia is limited by keratinocytes overgrowth beyond ablation depth and their growth during healing. Better effects are achieved with retinoids applied prior to a laser surgery. It has been noted that after a laser removal, there were fewer relapses of basal cell carcinomas than spinocellular carcinomas. It may be due to a smaller content of water in keratinocytes of the latter than the former. Laser light is also used to remove pigmented moles [4, 15, 16]. Both laser types provide surgery completeness and similar percentage of relapse. The possibility of multiple passage of the light emitted by Er:YAG laser is an advantage in pigmented moles removal. On the other hand though, CO2 laser enables excision of richly vascularized lesions. It is also beneficial in patients in whom hemostasis might be difficult, for example during anticoagulants therapy [16]. It was of significant importance to our patients undergoing surgery. We achieved surgery completeness in all of them and could avoid suturing in many cases for post-operative scars and changes in the tissue profile as suturing may bring about chronic irritation, pathological biting on the tissues and therefore promote lesions relapse.
Conclusions
Both, Er:YAG and CO2 lasers may be effective in the treatment of benign neoplastic and tumorous lesions of the oral soft tissues being an alternative to conventional surgery. They shorten post-operative healing time, eliminate or soothe inflammation, reduce perisurgical pain. Thanks to effective hemostasis, CO2 laser may be used to remove richly vascularized lesions and in compromised patients. Healing neither changes the tissue profile nor causes its loss, ensures fast and good adaptation of the changes. A major limitation of the laser technique application is thermal injury to the surrounding tissues, charring and melting of wound margins with CO2 laser, especially during multiple passage of the beam and with excessive power for a small lesion. This may promote tissue defragmentation and thus frequently makes histopathological evaluation impossible. Changes in the healing tissues profiles following laser beam application are not observed. Good and fast adaptation of prosthetic restoration to the operated area is visible. CO2 laser is contraindicated for lesions smaller than 3 mm in diameter as they may get defragmented making histopathological evaluation impossible. Therefore, for the majority of minor oral surgeries Er:YAG laser is a better choice.
Conflict of interest
The authors declare no conflict of interest.
References
- 1.Borrás MT, Molina ED, Aytés LB, Escoda CG. Removal of hyperplastic lesions of the oral cavity. A retrospective study of 128 cases. Med Oral Patol Oral Cir Bucal. 2005;10:151–62. [PubMed] [Google Scholar]
- 2.Błochowiak K, Sidorowicz K, Sokalski J, Witmanowski H. Er:YAG laser treatment of benign neoplasms and tumorous lesions of the oral mucosa. Postep Derm Alerg. 2012;29:143–7. doi: 10.5114/pdia.2015.48053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vesovi P, Corcione L, Meleti M, et al. Nd:YAG laser versus traditional scalpel. A preliminary histological analysis of specimens from the human oral mucosa. Laser Med Sci. 2010;25:685–91. doi: 10.1007/s10103-010-0770-4. [DOI] [PubMed] [Google Scholar]
- 4.Riggs K, Keller M, Humphreys TR. Ablative laser resurfacing: high-energy pulsed carbon dioxide and erbium:yttrium-aluminum-garnet. Clin Dermatol. 2007;25:462–73. doi: 10.1016/j.clindermatol.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 5.Szyfter W, Mielcarek-Kuchta D, Miętkiewska-Leszniewska D, et al. Comparison between 2 laser system, Er-Yag and CO2 in stapes surgery. Otol Neurotol. 2013;34:29–35. doi: 10.1097/MAO.0b013e31827853c3. [DOI] [PubMed] [Google Scholar]
- 6.Keck T, Burner H, Rettinger G. Prospective clinical study on cochlear function after erbium: yttrium-aluminum-garnet laser stapedotomy. Laryngoscope. 2005;115:1627–31. doi: 10.1097/01.mlg.0000173164.64044.74. [DOI] [PubMed] [Google Scholar]
- 7.Fitzpatrick RE, Rostan EF, Marchell N. Collagen tightening by carbon dioxide versus erbium: YAG laser. Lasers Surg Med. 2000;27:395–403. doi: 10.1002/1096-9101(2000)27:5<395::AID-LSM1000>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 8.Alster TS, Lupton JR. Erbium:YAG cutaneous laser resurfacing. Dermatol Clin. 2001;19:453–66. doi: 10.1016/s0733-8635(05)70286-2. [DOI] [PubMed] [Google Scholar]
- 9.Pick RM, Colvard MD. Current status of lasers in soft tissue dental surgery. J Periodontol. 1996;64:589–602. doi: 10.1902/jop.1993.64.7.589. [DOI] [PubMed] [Google Scholar]
- 10.Hędzelek W, Andrysiak P. The utility of the CO2 laser to create the prosthetic area. Dent Forum. 2005;32:81–5. [Google Scholar]
- 11.Böttcher A, Jowett N, Kucher S, et al. Use of a microsecond Er:YAG laser in laryngeal surgery reduces collateral thermal injury in comparison to superpulsed CO2 laser. Eur Arch Otorhinolaryngol. 2014;271:1121–8. doi: 10.1007/s00405-013-2761-0. [DOI] [PubMed] [Google Scholar]
- 12.Tanzi EL, Alster TS. Single-pass carbon dioxide versus multiple-pass Er:YAG laser skin resurfacing: a comparison of postoperative wound healing and side-effect rates. Dermatol Surg. 2003;29:80–4. doi: 10.1046/j.1524-4725.2003.29012.x. [DOI] [PubMed] [Google Scholar]
- 13.Fitzpatrick RE. Maximizing benefits and minimizing risk with CO2 laser resurfacing. Dermatol Clin. 2002;20:77–86. doi: 10.1016/s0733-8635(03)00047-0. [DOI] [PubMed] [Google Scholar]
- 14.Sapijaszko MJA, Zachary CB. Er:YAG laser skin resurfacing. Dermatol Clin. 2002;20:87–96. doi: 10.1016/s0733-8635(03)00048-2. [DOI] [PubMed] [Google Scholar]
- 15.Hantash BM, Stewart DB, Cooper ZA, et al. Facial resurfacing for nonmelanoma skin cancer prophylaxis. Arch Dermatol. 2006;142:976–82. doi: 10.1001/archderm.142.8.976. [DOI] [PubMed] [Google Scholar]
- 16.Iyer S, Bowes L, Kricorian G, et al. Treatment of basal cell carcinoma with the pulsed carbon dioxide laser: a retrospective analysis. Dermatol Surg. 2004;30:1214–8. doi: 10.1111/j.1524-4725.2004.30378.x. [DOI] [PubMed] [Google Scholar]