Abstract
The purpose of this study is that to evaluate superiority and results of open technique in the treatment of femoral shaft fracture with interlocking intramedullary nailing. The retrospective study is designed to evaluate results of our technique. In this study, the patients that were admitted to the Orthopedics and Traumatology Department of University Hospital that is third level of trauma center. We claim that open technique is not a disadvantage during union process over closed technique in treatment of femoral shaft fracture with interlocking nailing. In this study, 44 patients that were consulted for adult femoral shaft fracture between January 2008 to July 2010 were included. Patients with open fractures, gunshot wounds, neurovascular injuries, and patients that did not have isolated femoral diaphysis fractures were excluded from the study. Clinical and radiological results of the patients were checked periodically. The open interlocking intramedullary nailing was used in treatment. Complete union rate was 90.9 % in 40 patients who were treated with open interlocking intramedullary nailing for adult femoral shaft fracture, and nonunion rate was 9.1 % in four patients. Mean union time was 18.3 weeks (12–36 weeks). Evaluation of 44 patients according to Thoresen criteria was excellent in 22 patients, good in 6 patients, and bad in 4 patients. We think that open technique is an acceptable technique because all results of our study were similar to results of closed intramedullary nailing technique in literature and some advantages of open technique over closed technique.
Keywords: Open technique, Interlocking intramedullary nailing, Femoral shaft fracture, Nonunion
Introduction
Nowadays, the rate of traffic and work accidents has increased due to the active life created by technological developments. These accidents cause physical, mental, and social issues in terms of patients and society [1]. Femoral shaft fractures are a traumatologic situation that distorts the entirety of the skeletal system. It can result in mortality, extended morbidity, and disability [1–3].
Intramedullary fixation is the most reliable method in comparison to other treatment methods [2]. The purpose of this study was to analyze the advantages and results of using the open reduction technique for interlocking intramedullary fixation, the latest method developed to treat femoral shaft fractures, in comparison to using a closed technique.
Patients and Method
Results obtained from retrospectively monitoring adult patients that underwent open interlocking intramedullary fixation after admitting to our orthopedic and traumatology clinic diagnosed with femoral shaft fractures between January 2008 and July 2010 were analyzed in this study. Forty-four patients that registered with a femoral shaft fracture between these dates and were treated with interlocking intramedullary nails were included in the study. Twenty-eight (63.6 %) of these patients were male, 16 (36.4 %) were female, and the average age of patients was 44 (17–70 years old). Patients with open fractures, Gunshot wounds, neurovascular injuries, and patients that did not have isolated femoral diaphysis fractures were excluded from the study.
Patients underwent a systemic physical examination during their initial visit, and investigations were conducted to find out whether or not they had additional pathologies. Patients were specifically checked for neurological and vascular injuries.
The X-rays (showing both femur, hip, and knee) were taken of every patient admitted to our clinic, in addition to their regular check-ups. Femoral shaft fractures were classified using AO/OTA classification.
Patients spoke about their subjective complaints regarding surgery; their knee range of motion was measured; shortness development and rotational deformities were examined during clinical examinations of patients attending their last check-up appointment; and results were compared to the uninjured side.
The level of bone healing, entirety of the fracture line, continuity of reduction, length of both femurs, heterotrophic bone development, and extensive callus tissue development were investigated during radiological assessment.
Clinical results were assessed based on clinical examination-based evaluation criteria set by Thoresen et al. Results were classified as excellent, good, moderate, and bad.
First-generation cephalosporin was given as prophylactic antibiotic, using intravenous therapy, roughly an hour before surgery. Parenteral antibiotherapy was applied for 3 days during the postoperative period. Patients started receiving low molecular weight heparin (Clexan®, 0.4 IU) before surgery until their postoperative discharge date.
Open reduction without periosteal stripping was the surgical technique used for all patients. A 10-cm skin incision was made for transverse fractures, and a 15-cm skin incision or more depending on the type of the fracture was made for oblique, spiral, and split fractures. The medullar content while the canal was being reamed was left into the fracture region due to the fact that it could cause an osteoinductive effect. Finally, reduction and the position of the nail were checked using an intraoperative x-ray.
All patients were started on isometric quadriceps exercises on post-op day 2, and passive hip and knee movements on post-op day 3. Mobilization without load was allowed for patients within the week before discharge. Patients were given a home program and discharged within 7 to 14 days after starting their physiotherapy program and when they reached a 90° knee flexion. Patients were asked to attend check-up appointments every fortnight during the first month, a check-up appointment once a month during the following 6 months, and after that a check-up appointment every 3 months.
The range of motion of the knee, the state of the wound, and the level of pain in the fracture region were examined at check-up. In terms of radiology, the reduction, fracture union, and the configuration of the nail were checked in the x-rays. During their final check-up, patients were given the chance to talk about their subjective complaints such as pain and restricted movement; the distance between the spina iliaca anterior superior and medial malleolus was measured for both lower extremities to calculate the difference in distance. The range of motion for the knee was recorded in degrees using a goniometer. Rotational defects were looked at by clinical examination (comparing with normal side). The union level of the fracture and the continuity of the reduction were checked from the x-rays, and at least three cortices union was accepted as union.
Results
Twenty-eight (63.6 %) patients were male and 16 (36.4 %) were female. The average age of patients was 44 (17–70 years old). The mean follow up time for patients was 30.9 months (15–48 months).
Eight (18.1 %) of the femoral shaft fractures were in the proximal 1/3 part, 34 (77.2 %) of the femoral shaft fractures were in the middle 1/3 part, and 2 (4.7 %) of the femoral shaft fractures were in the distal 1/3 part. According to AO/OTA morphological classification, 10 (22.7 %) patients had type B femoral shaft fractures, and 34 (77.3 %) patients had type A femoral shaft fractures.
Sixteen (36.4 %) patients had a femoral shaft fracture in their left side, and 28 (63.6 %) had a femoral shaft fracture in their right side. All patients had closed fractures.
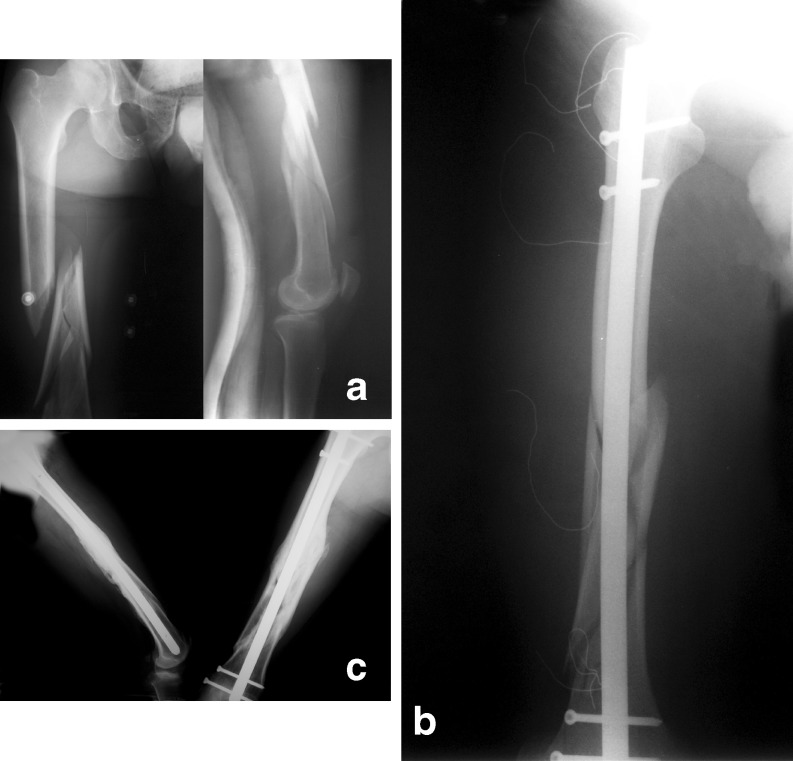
The fractures of 40 (90.9 %) patients healed completely, and nonunion was seen in 4 (9.1 %) patients (Fig. 1a–c).
Fig. 1.
a Preoperative view from one of the patients. b Early postoperative view of the same patient. c Late postoperative view of the same patient
The average healing period was 18.3 weeks (ranging between 12 and 36 weeks). No pain in the fracture region was recorded, and the formation of a callus bridge was interpreted as good healing.
During their last check-up appointment, 28 patients had a knee flexion of 120° and above, 12 patients had a knee flexion between 90° and 120°, and 4 patients had a knee flexion below 90°.
A 10-mm shortening was observed in six patients, and a 20-mm shortening was observed in six patients. According to rotational deformity measurements, two patients had a 10° internal rotation varus deformity, six patients had a 10° external rotation varus deformity, and six patients had a varus deformity below 10°. Internal or external deformities were measured using a goniometer while the patient was in “prone” position, and their knee was at a 90° flexion after fracture healed.
Four patients developed a surface infection in the entrance region of the nail in the hip after discharge; the infection was controlled with oral antibiotherapy.
According to the Thoresen measurements of the 44 patients monitored, 22 patients were “excellent,” 6 patients were “good,” 12 patients were “moderate,” and 4 patients were bad.
Discussion
Numerous methods can be used to treat femoral shaft fractures. Orthopedic surgeon should be aware of the advantages, disadvantages, and restrictions of these various methods. The position of the fracture, the extent of fragmentation, the age of the patient, the social and economic demands of the patient, and other factors help to determine the treatment method [4].
Literature states that the average clinical and radiological recovery period after standard fixation of femoral diaphysis is between 12 and 24 weeks [5]. Numerous studies report that a healing rate of 97–100 % takes place within this period with interlocking intramedullar fixation [3]
Rascher et al. reported that 42 femoral fractures treated with closed intramedullary fixation healed completely [6]. Although closed method has been studied well in literature, there are a few comparative studies between open and closed methods. The advantages of closed nailing over open operation continue to be debated. In theory, if one disturbs the fracture hematoma by exposing the fracture site, healing will be delayed and the risk of infection will be increased. Rokkanen reports slightly better results for closed nailing over open nailing [7], but in a more recent and better controlled study, Leighton did not find any significant difference between open versus closed intramedullary nailing for femoral shaft fractures [8]. Harper reported that open and closed groups had similar incidence of postoperative complications accept for rational malunion, which occurred more frequently in closed nailing group. The other results were similar in both groups [9].
Due to the reasons stated below, we used the open intramedullar fixation method in all our patients.
Less and cheaper equipment was required to those used in closed fixation.
No requirement for a special fracture or operating table.
Fluoroscopy was only required for distal interlocking; scopy is not even required for some of the new-type nail designs.
No requirement for preoperative traction and distraction for the reduction of the fracture.
Achieving total anatomic reduction is easier using the open technique.
Being able to see the fracture line directly helps to discover displaced pieces, or pieces not indentified from the X-ray.
Being able to bring the fragments together increases rotational stability. Rotational malalignment is a complication that rarely develops after open reduction.
The middle segment is stabilized easier for segmental fractures using the open method. This can prevent the rotation and bending caused by closed reduction and medullar reaming.
A fracture may occur in the femur neck when nailing during the closed technique.
As reaming is easier in the open method, it is easier to designate the correct length and diameter for the nail.
In comminuted fractures, bone fragments can be stopped from escaping to the medulla.
The risk of disruption of blood supply of the femoral head based on unsuitable entrances and additional femoral fracture is lower in the open method in comparison to the closed method.
The risk of superior gluteal nerve damage is lower.
As the medulla is reamed when open, the risk of reaming-based emboli is lower in comparison to the closed method.
The fact that the surgery lasts longer and the excessive amount of radiation that the surgeon is exposed are among the most important disadvantages of closed interlocking intramedullar fixation surgery. Studies report that the radiation that surgeons are exposed cause leukemia, bone sarcoma, brain tumors, thyroid carcinoma, skin cancer, and lung cancer [10, 11].
In terms of the amount of radiation exposed to, Levin et al. report that the amount of radiation exposed to is 12.6 min, while Sugarman et al. report that this period is 12.08 min [12–14]. One dose of scopy was only used to identify the fracture line of cases that did not experience any difficulties during the application of distal interlocking screws.
Özsoy et al. proved that there is a risk that the superior gluteal nerve is damaged due to the different flexion positions of the hip during the closed intramedullar fixation procedure [15].
The issues of the correct entry point for antegrade nailing remains a matter of controversy, and the literature is confusing. Kale et al. [16] reviewed the opinions of 100 orthopedic surgeons by means of questionnaires. Only four surgeons were able to identify and label their respective entry points of femoral nailing correctly. Although the piriformis fossa appears to be the ideal entry point, the importance of exact localization in the sagittal plane, centered over the axis of medullary canal, cannot be overlooked.
One of basic problem during antergrade nailing is not to determine correct entry point. Correct entry point will prevent problems that can cause a lot of complications of entry point. Even if described entry point will be chosen at proximal end, femoral anatomic variations can be possible distally. Each femoral canal architecture and curve is different. Therefore, retrograde nailing will provide optimal entry point for each patient individually. A fracture may occur in the femur neck when incorrect entry point was chosen at the closed technique. Wild et al. reported that the total rate of complications for intramedullary femoral nailing was low (4.9 %), but a high rate of intraoperative femoral neck fractures was observed (1.4 %) [17].
Literature refers to complications such as damage to the sciatic, peroneal, and pudendal nerves as a result of treating femoral shaft fractures with the interlocking intramedullar fixation method under traction. Pudendal nerve paralysis is a known complication of femoral nailing. This situation appears in the form of labial sensory change in women, and scrotal and penile sensory change in men, sometimes together with erection disorders. Pudendal nerve paralysis can be prevented by decreasing traction-based pressure [18]. None of our cases developed a nerve paralysis as we did not use a traction table for all our cases.
According to literature, the rate of infection after femoral fixation is significantly low. This rate is higher in open fractures. Different references in literature state that the rate of deep infection in closed intramedullar fixation is below 2 %, and between 1.5 and 10 % in open intramedullary fixation [5, 18–20].
Rothwell et al. reported significance shortness for all femoral fractures regardless of the treatment method. However, they emphasized that the rate of complication was lower for interlocking intramedullar nails [21]. Winquist et al. reported that the rate of shortness above 2 cm was 2 % [22]. They reported that shortness was rarely seen in type 1 stabile, short oblique, or transverse fractures, and that shortness less than 2 cm rarely caused leg or back pain. Accordingly, they identified that shortness of 1.5 cm was acceptable for young patients, and shortness of 2.5 cm was acceptable for patients that were 65 and over. In our study, 27.2 % of the patients had shortness between 1 and 2 cm.
Winquist and Hansen published the results for closed intramedullar fixation technique applied to 520 cases with femoral shaft fractures. Eighty-five patients had a proximal fracture, 325 patients had a middle diaphysis fracture, and 110 patients had a distal diaphysis fracture. They concluded that 87 % of these patients displayed solid union in 3 months, and there were only eight patients (1.5 %) that had a knee flexion below 125°. In terms of complications, they reported that 0.7 % (4 patients) of patients developed an infection, 0.7 % (4 patients) of nonunion, 2 % of cases had shortness more than 2 cm, 7 % of cases had shortness between 1 and 2 cm, 2.3 % (12 patients) of cases developed malunion more than 20°, and 8.2 % (43 patients) of cases union at an external rotation of 10° [22].
Klemm and Borner investigated using the interlocking nailing method of 266 patients with femoral fractures, of which 84 % were closed. According to the functional criteria they used in their study, 79.3 % of cases were excellent, and 97 patients were excellent or good. Fourteen patients did not develop any complications. Four patients (1.5 %) experienced nonunion, seven patients (2.6 %) developed a deep infection, and one patient (0.3 %) suffered peroneal nerve paralysis [23].
Tuzuner et al. reported that all cases except one patient made a full recovery in their study, conducted over an average monitoring period of 14.4 months. They concluded that the average healing time for 30 patients (71.42 %) with Winquist types I and II fractures was 17.6 weeks (8–32 weeks), and the average healing time for 12 patients (28.57 %) with Winquist types III and IV fractures was 19.8 weeks (10–36 weeks). After surgery, the knee flexion of 30 patients was between 90° and 120°, the knee flexion of 10 patients was above 120°, and the knee flexion of four patients was below 90°. In six patients, 10-mm shortness was seen, and 25-mm shortness was seen in one patient. According to rotational deformity measurements, conducted after the fractures were healed, one patient (2.38 %) had a 10° internal rotational varus deformity, four patients (8.52 %) had a 15° external rotational varus deformity, and two patients (4.76 %) had a varus deformity below 10°. The healing rate was 97 %, and the average healing period was 18.22 weeks [24].
A study conducted on 3,243 patients by the AO European Commission concluded that 2.6 % of patients suffered from malunion and malrotation using the open technique, and 7.7 % of patients using the closed technique [25].
Fracture hematoma has a positive effect on the healing of fractures. Therefore, there is a common view that the ideal approach while treating fractures is that fracture hematoma should not be drain out. Studies, conducted in recent years, simply conclude that the number of osteoblast progenitor cells does not only increase in the fracture hematoma but also there is an increase in the osteoblast progenitor cell concentration in circulation. Eghbali-Fatourechi et al. [26] concluded that the number of osteoblast progenitor cells in the circulation of adolescent individuals was higher in comparison to those of adults, and that the number of osteoblast progenitor cells increased in the circulation of adults that had recently suffered a fracture. Clines [27] published a review about osteoprogenitor stem cells in fracture repair and osteoporosis at 2010. He claimed that comparison of adolescent versus aged individuals revealed higher numbers (fivefold) of circulating osteoprogenitor cells in adolescent individuals, probably reflecting the bone growth at that age. Moreover, numbers of circulating osteoprogenitors were also higher in individuals who had experienced a recent fracture. These studies raise the possibility that osteoprogenitors may not only be recruited locally but also from distant sites during times of heightened bone formation or fracture. In light of this information, we do not agree that the open technique has an adverse effect on the healing of a fracture, and we believe that the open technique is more advantageous in comparison to the closed technique, based on the advantages listed above.
One prospective cohort study (CoE level III) and one retrospective cohort study (CoE level II) were summarized by the AO Foundation [28]. There is insufficient high quality evidence to determine treatment superiority. No significant differences between intramedullary nails versus plates were found. We think that fracture hematoma is an orthopedic myth, the key point is periosteum.
In the literature, Christie et al. [29] report that the healing time using the closed technique was 17 weeks, Johnson et al. [30] report that the healing time using the closed technique was 13.8 weeks. Harper reported that healing time of closed and open method was 14.3 and 13.9 weeks, respectively [9]. He concluded that the difference of 0.4 week is not statistically significant. Our study results conclude that the average healing time using the open technique was 18.3 weeks.
The fact that all our study results are close to those stated in literature regarding the closed intramedullar nailing method proves that the open method is an acceptable method based on its advantages, referred to above, in comparison to the closed technique.
Acknowledgments
Conflict of interest
The authors declare that they have no conflict of interest.
Contributor Information
Halil Burç, Phone: +90-532-3527446, FAX: +90-246-2119431, Email: halilburc@gmail.com.
Tolga Atay, Phone: +90-246-2119264, FAX: +90-246-2119431, Email: ataytolga@gmail.com.
Demir Demirci, Phone: +90-246-2119264, FAX: +90-246-2119431, Email: dr.demirdemirci@gmail.com.
Y. Barbaros Baykal, Phone: +90-246-2119268, FAX: +90-246-2119431, Email: barbarosbaykal@yahoo.com.
Vecihi Kirdemir, Phone: +90-246-2119270, FAX: +90-246-2119431, Email: vkirdemir@yahoo.com.
Hüseyin Yorgancigil, Phone: +90-246-2119267, FAX: +90-246-2119431, Email: huseyinyorgancigil@sdu.edu.tr.
References
- 1.Brovvner BD. Pitfalls, errors, and complications in the use of interlocking Kuntscher nails. Clin Orthop. 1986;212:192–208. [PubMed] [Google Scholar]
- 2.Brovvner BD. Interlocking nailing of femoral fractures. In: Brovvner BD, editor. The science and practice of intramedullary nailing. 2. Connecticut: Williams & Wilkins; 1996. pp. 161–183. [Google Scholar]
- 3.Brumback RJ, Uwagie-Ero S, Lakatos RP, et al. Intramedullary nailing of femoral shaft fractures. Part II: Fracture-healing with static interlocking fixation. J Bone Joint Surg Am. 1988;70:1453–1462. [PubMed] [Google Scholar]
- 4.Whittle AP, Wood GW., II . Shaft of femur. In: Canalle ST, editor. ’s Operative Orthopaedics. Philadelphia, Pennsylvania: Int.edn. Mosby; 2003. pp. 2825–2859. [Google Scholar]
- 5.Bucholz RW, Jones A. Fractures of the shaft of the femur. J Bone Joint Surg Am. 1991;73:1561–1566. [PubMed] [Google Scholar]
- 6.Rascher J, Nahigian SH, Macys JR, Brown JE. Closed nailing of femoral shaft fractures. J Bone Joint Surg Am. 1972;54-A(3):534–544. [PubMed] [Google Scholar]
- 7.Rokkanen P, Slgtis P, Vankka E. Closed or open intramedullary nailing of femoral shaft fractures: a comparison with conservatively treated cases. J Bone Joint Surg. 1969;51-B:313–323. [PubMed] [Google Scholar]
- 8.Leighton RK, Waddell JP, Kellam JF, Orrell KG. Open versus closed intramedullary nailing of femoral shaft fractures. J Trauma. 1986;26:923–926. doi: 10.1097/00005373-198610000-00011. [DOI] [PubMed] [Google Scholar]
- 9.Harper MC. Fractures of the femur treated by open and closed intramedullary nailing using the fluted rod. J Bone Joint Surg Am. 1985;67-A(5):699–708. [PubMed] [Google Scholar]
- 10.Cruz M, Coley BL, Stewart FW. Postradiation bone sarcome. Cancer. 1957;10(1):72–88. doi: 10.1002/1097-0142(195701/02)10:1<72::AID-CNCR2820100111>3.0.CO;2-8. [DOI] [PubMed] [Google Scholar]
- 11.Pack GT, Davis J. Radiation cancer of the skin. Radiology. 1965;84:436–442. doi: 10.1148/84.3.436. [DOI] [PubMed] [Google Scholar]
- 12.Levin PE, Schoen RW, Browner BD. Radiation exposure to the surgeon during closed interlocking intramedullary nailing. J Bone Joint Surg Am. 1986;69:761–766. [PubMed] [Google Scholar]
- 13.Angliss RD, Tran TA, Edwards ER, et al. Unreamed nailing of tibial shaft fractures in multiply injured patients. Injury. 1996;27:255–260. doi: 10.1016/0020-1383(96)00059-9. [DOI] [PubMed] [Google Scholar]
- 14.Sugarman ID, Adam I, Bunker TD. Radiation dosage during AO interlocking femoral nailing. Injury. 1988;19:336–338. doi: 10.1016/0020-1383(88)90107-6. [DOI] [PubMed] [Google Scholar]
- 15.Ozsoy MH, Başarır K, Bayramoğlu A, et al. Risk of superior gluteal nerve and gluteus medius muscle injury during femoral nail insertion. J Bone Joint Surg Am. 2007;89:829–834. doi: 10.2106/JBJS.F.00617. [DOI] [PubMed] [Google Scholar]
- 16.Kale SP, Patil N, Pilankar S, Karkhanis AR, Bagaria V. Correct anatomical location of entry point for antegrade femoral nailing. Injury. Int J Care Injured. 2006;37:990–993. doi: 10.1016/j.injury.2006.06.003. [DOI] [PubMed] [Google Scholar]
- 17.Wild M, Gehrmann S, Jungbluth P, Hakimi M, Thelen S, Betsch M, Windolf J, Wenda K. (2010) Treatment strategies for intramedullary nailing of femoral shaft fractures. Orthopedics Vol:33(10); doi:10.3928/01477447-20100826-15 [DOI] [PubMed]
- 18.Stambough JL, Hopson CN, Cheeks ML. Stable and unstable fractures of the femoral shaft. Orthop Rev. 1991;20:855–861. [PubMed] [Google Scholar]
- 19.Court-Brown CM, Browner BD. Interlocking nailing of femoral fractures. In: Browner BD, editor. The science and practice of intramedullary nailing. 2. Baltimore: Williams & Wilkins; 1996. pp. 161–182. [Google Scholar]
- 20.Brumback RJ, Ellison PS, Jr, Poka A, et al. Intramedullary nailing of open fractures of the femoral shaft. J Bone Joint Surg Am. 1989;71:1324–1331. [PubMed] [Google Scholar]
- 21.Rothwell AG. Closed Kuntscher nailing for comminuted femoral shaft fractures. J Bone Joint Surg. 1982;64-B(1):12–16. doi: 10.1302/0301-620X.64B1.7068712. [DOI] [PubMed] [Google Scholar]
- 22.Winquist RA, Hansen ST, Jr, Clawson DK. Closed intramedullary nailing of femoral fractures. A report of five hundred and twenty cases. J Bone Joint Surg Am. 1984;66:529–539. [PubMed] [Google Scholar]
- 23.Klemm KW, Börner M. Interlocking nailing of complex fractures of the femur and tibia. Clin Orthop Relat Res. 1986;212:89–100. [PubMed] [Google Scholar]
- 24.Tuzuner T, Subaşı M, Kapukaya A, et al. Femur cisim kırıklarının kilitli intramedüller çivileme ile tedavisi. Acta Orthop Traumatol Turc. 2002;36:211–219. [PubMed] [Google Scholar]
- 25.Giannoudis PV, Pape HC, Schütz M (Updated 2007) Evidence summary: literature overview of femoral shaft fracture. Table: Open versus closed intramedullary nailing. [AO Foundation web site]. Avaliable at: http://www.aofoundation.ch/wps/portal/!ut/p/c1/04_SB8K8xLLM9MSSzPy8xBz9CP0os3hng7BARydDRwN39yBTAyMvLwOLUA93I4MQE6B8JLK8uYElUN7YIzTE0c_AwMSEJN0GFgFuBkZOpv6GJsEBRgbuBgR0-3nk56bqF-SGRpQ7KioCACmtHFM!/dl2/d1/L2dJQSEvUUt3QS9ZQnB3LzZfQzBWUUFCMUEwR0dSNTAySkowOFVIRzIwVDQ!/?contentUrl=%2fsrg%2fpopup%2fevidence_sum%2f32%2f32_es_operative_treatments.jsp&popupStyle=diagnosis&soloState=true&bone=Femur&segment=Shaft&BackMode=true. Accessed December 17, 2012.
- 26.Guiti Z, Eghbali-Fatourechi, Jesse Lamsam MS, Daniel Fraser, David Nagel AB, Lawrence Riggs B, Sundeep Khosla Circulating Osteoblast-Lineage Cells in Humans. N Engl Jj Med. 2005;352:19. doi: 10.1056/NEJMicm040848. [DOI] [PubMed] [Google Scholar]
- 27.Clines GA. Prospects for osteoprogenitor stem cells in fracture repair and osteoporosis. Curr Opin Organ Transplant. 2010;15:73–78. doi: 10.1097/MOT.0b013e328333d52c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Giannoudis PV, Pape HC, Schütz M (Updated 2007) Evidence Summary: Literature overview of femoral shaft fracture [AO Foundation web site]. Avaliable at: https://www2.aofoundation.org/wps/portal/surgery?showPage=diagnosis&bone=Femur&segment=Shaft. Accessed December 17, 2012.
- 29.Christie J, Howie CR, Kinninmonth AW, Court-Brown C. Intramedullary locking nails in the management of femoral shaft fractures. J Bone Joint Surg. 1988;70-B(2):206–210. doi: 10.1302/0301-620X.70B2.3346289. [DOI] [PubMed] [Google Scholar]
- 30.Johnson KD, Tencer A. Mechanics of intramedullary nails for femoral fractures. Unfallchirurg. 1990;93(11):506–511. [PubMed] [Google Scholar]