Abstract
Right paraduodenal hernia usually occurs in setting of nonrotated small bowel, when small bowel herniates through Waldeyer's fossa (a defect in the first part of jejunal mesentery). It lies behind the superior mesenteric artery and inferior to the transverse colon or third portion of duodenum. We studied two cases of right paraduodenal hernia, an incomplete rotation, and nonrotation of small bowel, respectively, and describe CT abdomen signs, which can give a preoperative diagnosis.
Keywords: Right paraduodenal hernia, Incomplete rotation and nonrotation of small bowel
Introduction
Although internal hernias have an overall incidence of less than 1 %, they constitute up to 5.8 % of all small bowel obstructions [1]. Paramesocolic hernia traditionally known as paraduodenal hernias were described for the first time by Neubauer in 1786 and were classified by Treitz in 1857. Klob, Jonnesco, and Moynihan proposed the terms mesenteric–parietal, retroperitoneal, or transmesocolic hernia for right paraduodenal hernia, which were closely related to intestinal malrotation [2]. Midgut malrotation is diagnosed on barium studies with depression of the duodenojejunal (DJ) flexure, absence of the normal horizontal third part of duodenum, right-sided small bowel, and left-sided colon. Only rarely is an internal hernia correctly diagnosed preoperatively. Discovery of a congenital internal hernia at laparotomy may be confusing to a surgeon, and appropriate management may be compromised [3].
Clinical Case Reports
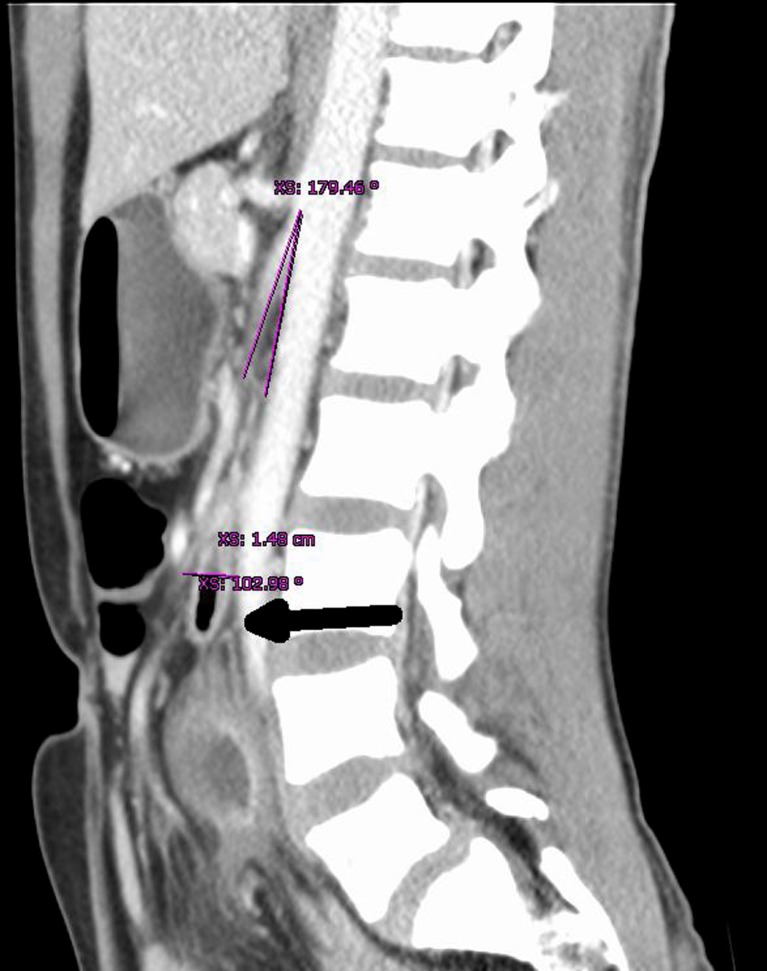
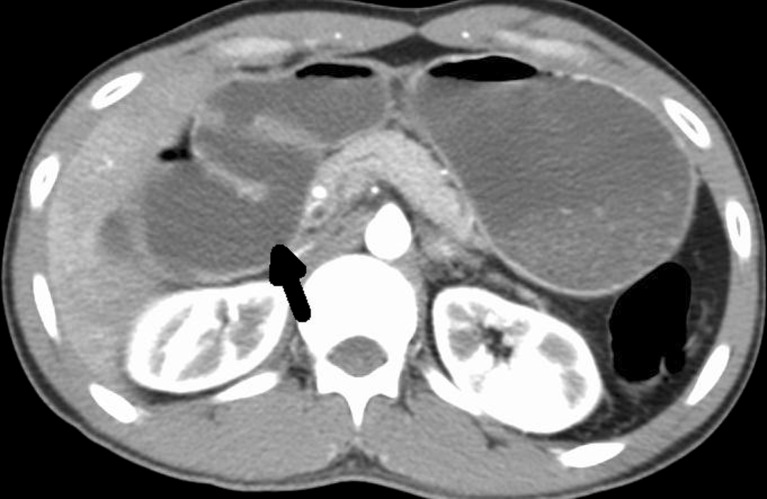
Our first case computed tomography (CT) scan abdomen showed a distended stomach and duodenum with midline focal compression of third part of duodenum between the aorta and superior mesenteric artery (SMA) (Fig. 1). We suspected SMA syndrome. On exploration, it revealed an incomplete malrotation of midgut, depression of DJ junction, which was to the right of midline, mesocolic herniation of third part of duodenum through SMA and aortic gap, and Ladd's band connecting the caecum and duodenum with proximal jejunal stricture (Fig. 2). Ladd's band were released, the third and fourth part of duodenum was mobilized to supracolic compartment, and a side to side retrocolic anastomosis of the jejunum and third part of the duodenum was done, bypassing jejunal stricture with appendectomy (Fig. 3).
Fig. 1.
Compression of duodenum between SMA and aorta with dilated proximal duodenum
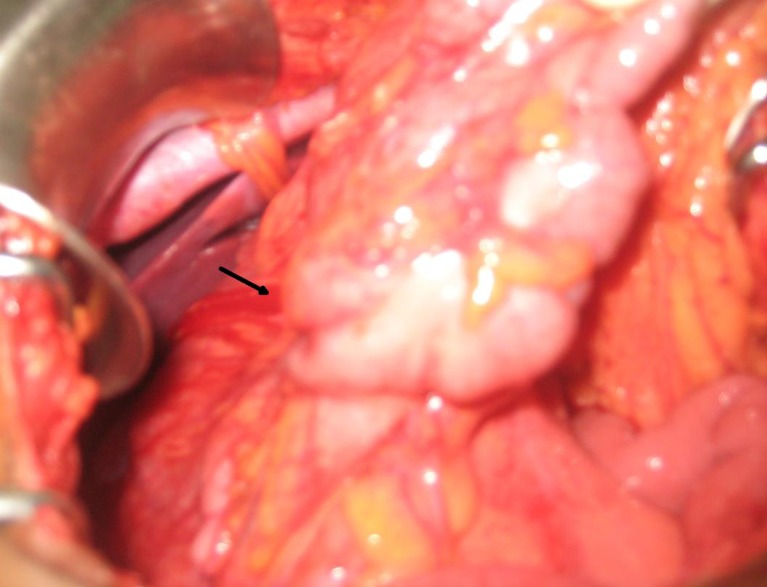
Fig. 2.
Showing Ladd's bands connecting the right colon and duodenum
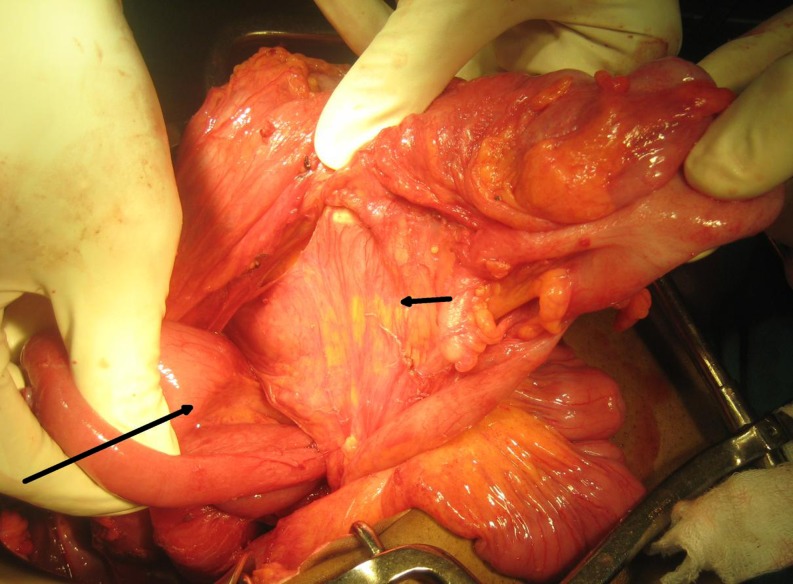
Fig. 3.
Showing right paraduodenal hernia (large arrow) through mobile right mesocolon (small arrow) seen after releasing Ladd's bands
The second case was a boy referred after abdominal exploration and appendectomy with unrelieved intestinal obstruction. CT abdomen revealed small bowel loops on right side and large bowel on left side of abdomen with superior mesenteric artery lying to the right of superior mesenteric vein (Fig. 4). Exploration revealed nonrotation of small bowel (Fig. 5). Releasing Ladd's bands and adhesiolysis relieved obstruction.
Fig. 4.
CT abdomen showing SMV lying on left ventral aspect of SMA suggesting nonrotation of small bowel
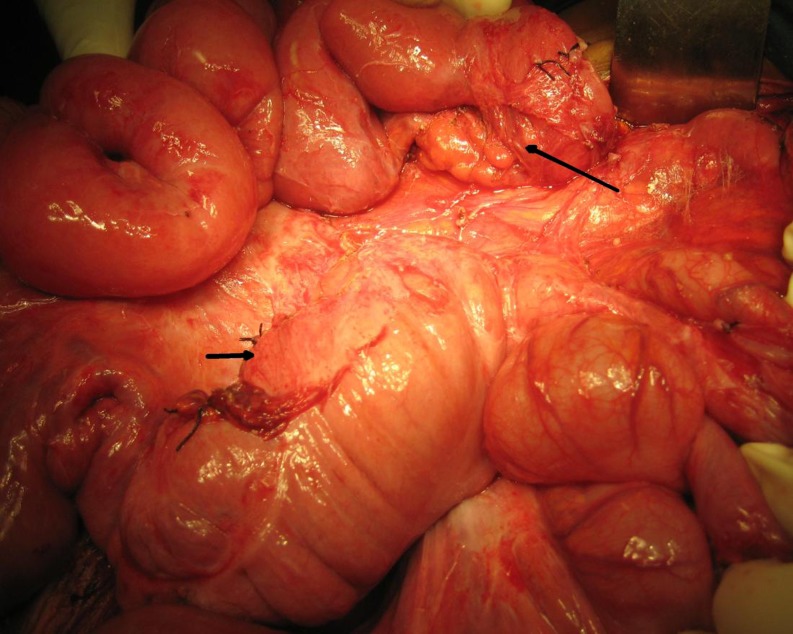
Fig. 5.
Duodenal third part (large arrow) going straight and downwards and colon (small arrow) on left side of abdomen
Discussion
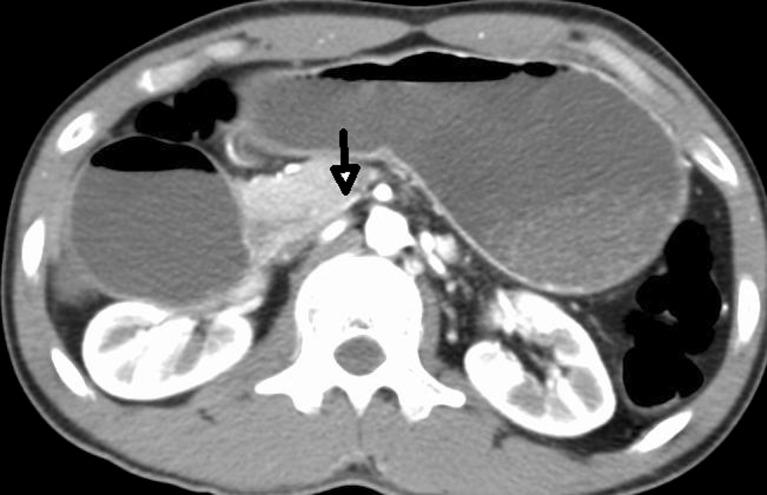
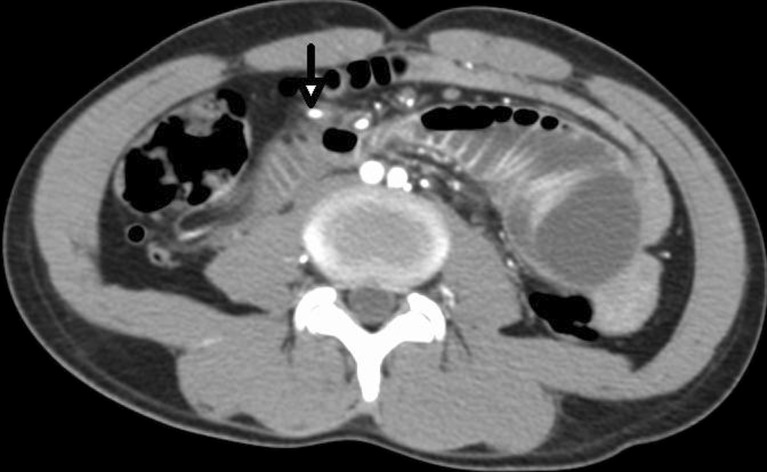
Andrews postulated abnormalities in second phase of embryonic intestinal rotation as cause for right paraduodenal hernias [2]. Normally, the prearterial or DJ limb rotates through an arch of 270° around an axis formed by the SMA in a counterclockwise direction. This results in the normal location of the second portion of the duodenum to the right of the SMA, the third portion of the duodenum posterior to the SMA, and the DJ junction to the left and posterior to the SMA. Failure of rotation during this stage may result in incomplete rotation/nonrotation with right paraduodenal hernia. In incomplete rotation, the duodenal loop lacks 90° of its normal 270° rotation, and the cecocolic loop lacks 180° of its normal rotation as was seen in the first case (Figs. 1, 2, and 3). Nonrotation occurs when the duodenum descends straight down to the right of the SMA. The small bowel lies entirely on the right side of the abdomen, and the colon lies on the left, as our second case [4] (Figs. 4, and 5). The normal arrangement of superior mesenteric vein (SMV) and the SMA in upper mesenteric root is the result of complete 270° counterclockwise rotation of the midgut. The final position of the SMV relative to the SMA reflects the degree of rotation that has occurred [5]. CT findings of right paraduodenal hernia in our cases were the absence of normal horizontal third part of duodenum, which goes towards right and downwards (Fig. 6), caudal displacement of the DJ junction than at the level of duodenal bulb (Fig. 7) [6], jejunal arteries which arise from left side of the SMA, abruptly reverse their direction to right (Fig. 8) [7, 8], presence of superior mesenteric artery, and ileocolic artery in the anterior margin of wall of the right paraduodenal hernia (Fig. 9) [9]. Reduction of a right paraduodenal hernia is accomplished by simply cutting the lateral peritoneal attachment of the right side of the colon (Ladd's procedure) and sweeping it to the left, thereby opening the small bowel sac to the free peritoneal cavity [2].
Fig. 6.
CT abdomen showing duodenum going towards right and downwards
Fig. 7.
CT abdomen showing inferior displacement of DJ (small arrow) as compared to duodenal cap (large arrow)
Fig. 8.
CT abdomen showing proximal jejunal arteries (arrow) reversing their direction to right
Fig. 9.
CT abdomen showing superior mesenteric artery and ileocolic branch (arrow) forming anterior margin of hernia. Small bowel traversing to left at the level of bifurcation of aorta
References
- 1.Martin LC, Merkle EM, Thompson WM. Review of internal hernias radiographic and clinical findings. Am J Radiol. 2006;186:703–717. doi: 10.2214/AJR.05.0644. [DOI] [PubMed] [Google Scholar]
- 2.Moran JM, Salas J, Sanjuan S, et al. Paramesocolic hernia: consequences of delayed diagnosis. Report of three new cases. J Pediatr Surg. 2004;39(1):112–116. doi: 10.1016/j.jpedsurg.2003.09.027. [DOI] [PubMed] [Google Scholar]
- 3.Newsom BD, Kukora JS. Congenital and acquired internal hernias: unusual causes of small bowel obstruction. Am J Surg. 1986;152:279–285. doi: 10.1016/0002-9610(86)90258-8. [DOI] [PubMed] [Google Scholar]
- 4.Torres AM, Ziegler MM. Malrotation of the intestine. World J Surg. 1993;17:326–331. doi: 10.1007/BF01658699. [DOI] [PubMed] [Google Scholar]
- 5.Nichols DM, Li DK. Superior mesenteric vein rotation: a CT sign of midgut malrotation. Am J Radiol. 1983;141:707–708. doi: 10.2214/ajr.141.4.707. [DOI] [PubMed] [Google Scholar]
- 6.Blachar A, Federie MP, et al. Radiologist performance in the diagnosis of internal hernia by using specific CT findings with emphasis on transmesenteric hernia. Radiology. 2001;221:422–428. doi: 10.1148/radiol.2212010126. [DOI] [PubMed] [Google Scholar]
- 7.Ghahremani, G.G., and Meyers, M.A.(1981): Hernias. Surgical Radiology vol 1.
- 8.Meyers MA. Paraduodenal hernias: radiologic and arteriographic diagnosis. Radiology. 1970;95:29–37. doi: 10.1148/95.1.29. [DOI] [PubMed] [Google Scholar]
- 9.Berardi RS. Paraduodenal hernias. Surg Gynecol Obstet. 1981;152:99–110. [PubMed] [Google Scholar]