Abstract
Subcutaneous emphysema (SE) is a condition often causing minimal symptoms, but sometimes it can be severe and even life-threatening. This study is the first great survey about SE. The aim of this study is to classify and evaluate the etiology, signs, symptoms, and management of SE. This retrospective study was performed by reviewing patients who had been diagnosed as having SE in Rasht, between January 2001 and January 2011. We classified the severity of SE in five grades including the (1) base of the neck, (2) all of the neck area, (3) subpectoralis major area, (4) chest wall and all of the neck area, and (5) chest wall, neck, orbit, scalp, abdominal wall, upper limbs, and scrotum. We excluded all patients in grades 1 and 2, because the symptoms and signs were not significant. Statistical analysis was carried out with SPSS 18. We collected 35 cases of SE with the mean age of 53 ± 14.83 (71 % men). The most common cause of SE was pneumothorax with background of COPD and surgery in grade 5, trauma due to rib fracture in grade 4, and iatrogenicity in grade 3. We performed two bilateral 2-cm infraclavicular incisions. In our patients with infraclavicular incisions, expansion of the lung was better, and the patients’ appearance improved. Infraclavicular incisions as a simple method for the management of SE can decrease the severity of SE with no cosmetic problem.
Keywords: Subcutaneous emphysema, Classification, Management, Infraclavicular incisions
Introduction
Subcutaneous emphysema (SE) occurs when air gets into the tissues under the skin and in the soft tissues. This usually occurs in the soft tissues of the chest wall or neck but can also occur in other parts of the body [1]. It can result from a number of processes, including blunt or penetrating trauma, pneumothorax barotrauma, infection, malignancy, or as a complication of surgical procedures and even spontaneous SE [2]. The most common and visible sign and symptom of SE is swelling around the neck accompanied with pain in the chest. Other signs and symptoms include tender sore throat, aching neck, difficulty in swallowing, breathlessness, wheezing, and distension [2]. So, it often causes minimal symptoms, is not dangerous in itself, and requires no specific treatment [2]. If it involves the deeper tissues of the thoracic outlet, chest, and abdominal wall, it will be a severe, stressful, and life-threatening condition. It can be complicated by restriction of full lung re-expansion and can lead to high airway pressure, severe respiratory acidosis, ventilator failure, pacemaker malfunction, airway compromise, and tension phenomena [2]. Diagnosis is made by physical exam (crepitation on palpation) and radiological studies indicating air in the involved area [1]. SE often presents a management dilemma [2]. Its management should begin with a concerted effort to identify the offending cause of the subcutaneous dissection of air [3]. Various approaches have been described, including the use of subcutaneous incisions, needles, drains, or cervical mediastinotomy [3–6]. Two infraclavicular incisions are our option when these interventions do not relieve increasing respiratory distress. In addition, literature does not reveal classification for severity of SE, and so, the aim of this study was to evaluate the etiology, classification, severity, signs, symptoms, management, and outcome of SE with two infraclavicular incisions.
Patients and Method
Patients
Using a prospective operative database over a 10-year period (between January 2001 and January 2011), this retrospective study was performed on patients who are diagnosed with SE at Razi Hospital and Arya Hospital by one surgeon (in the Thoracic Surgery Center of Guilan University of Medical Science). SE was defined as air under the skin and in the soft tissue that was perceptible by the clinician, patient, or family member. Persistent or recalcitrant SE was defined as SE that did not resolve despite the presence of a patent, functional chest tube in the pleural space.
Methods
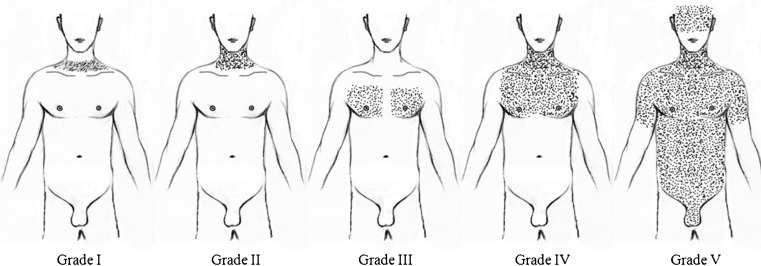
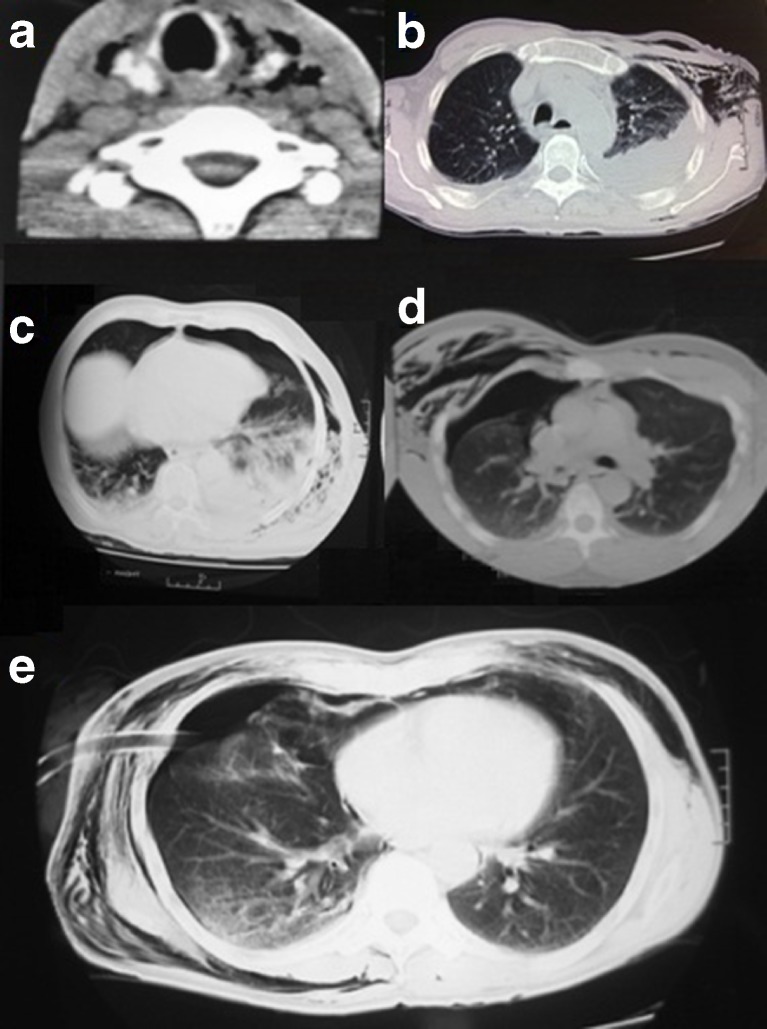
Diagnosis of SE is confirmed by the detection of thoracic, cervical, and abdominal crepitus and presence of air inside the soft tissue by chest X-ray and/or thoracic computed tomography. We cannot find any classification for severity of SE in review of the literature. So, we classified the severity of SE based on anatomical extension into five grades including the (1) base of the neck, (2) all of the neck area, (3) subpectoralis major area, (4) chest wall and all of the neck area, and (5) chest wall, neck, orbit, scalp, abdominal wall, upper limbs, and scrotum (Figs. 1 and 2). Patients who had SE that was only grades 1 and 2 were not included in this study. These grades of SE are not clinically important. Patients were managed by two infraclavicular incisions and then by milking those for evacuating air (Fig. 3). We also insert a unilateral or bilateral chest tube in the pleural space for patients who did not have a chest tube previously, with or without pneumothorax. We followed up patients for improvement of SE and re-expansion of the lungs. All data of the included patients such as demographic information and the etiology, classification, severity, signs, symptoms, and management of patients were recorded in a computerized database. Statistical analysis was performed with SPSS (version 18). Descriptive statistics were mean and standard deviation (SD) for the quantitative variables and frequencies for the qualitative variables.
Fig. 1.
Classification for severity of SE
Fig. 2.
Five classifications of SE were shown respectively: a grade 1, b grade 2, c grade 3, d grade 4, and e grade 5
Fig. 3.

Grade 5 of SE. This patient was managed with two infraclavicular incisions
Result
Thirty-five patients who had clinically noticeable SE (grades 3, 4, and 5) were included in this study. In each grade, men were of prominent gender (Table 1). The mean age of patients was 54.4 ± 14.5 (range, 16–75), and 68.6 % of them were men.
Table 1.
Demographic characteristics of each grade
| Grade | Male/female | Age (mean ± SD) and range |
|---|---|---|
| 3 | N = 6 (50 %)/N = 6 (50 %) | 51.5 ± 15.24 (16–75) |
| 4 | N = 8 (67 %)/N = 4 (33 %) | 50.2 ± 15.7 (20–70) |
| 5 | N = 10 (91 %)/N = 1 (9 %) | 62.1 ± 9.6 (40–75) |
We detected and classified four main causes for SE in our experience (35 patients) including trauma in 11 cases (31 %), pneumothorax with background of chronic obstructive pulmonary disease (COPD) in 12 cases (34 %), iatrogenicity in 9 cases (26 %), and barotrauma in 3 cases (9 %). The cause of SE was shown in Table 2. The most common cause of SE in grade 3 was pneumothorax with background of COPD (42 %). In the grade 4, trauma due to rib fracture (50 %) was detected as the most common cause. The most common cause of SE in grade 5 was iatrogenicity [surgical procedure such as coronary artery bypass graft surgery (CABG) and lobectomy] (55 %).
Table 2.
Causes of SE in grades 3 to 5
| Etiology | Pneumothorax with background of COPD | Trauma due to rib fracture | Iatrogenicity | Barotrauma |
|---|---|---|---|---|
| Grade 3 | N = 5 (42 %) | N = 4 (33 %) | N = 2 (17 %) | N = 1 (8 %) |
| Grade 4 | N = 5 (42 %) | N = 6 (50 %) | N = 1 (8 %) | N = 0 |
| Grade 5 | N = 2 (18 %) | N = 1 (9 %) | N = 6 (55 %) | N = 2 (18 %) |
In all grades, swelling, dyspnea, crepitus, and pneumothorax were the most common signs and symptoms, and in a few cases, hypoxemia, pain, and cough were accompanied with SE. For management, two bilateral 2-cm infraclavicular incisions deep to external thoracic fascia were performed for all patients, and chest tube was inserted in patients without a chest tube. Thereafter, milking was done for evacuating air. Bilateral chest tubes were inserted in seven cases in the grade 3 (25 %), and three cases in both grades 4 (30 %) and 5 (33 %) because of the severity of patient’s condition, and in the other patients, unilateral chest tubes were used. All patients’ data are shown in Table 1. The mean period of hospitalization was 16 days (12 to 24 days). We did not record any mortality. In our follow-up survey, the patients’ appearance had improved. The lungs were re-expanded. The most complications of infraclavicular incision in our patients was occlusion of incision by clot (four patients), bleeding (three patients), insufficient depth of incision in thoracic fascia (five patients), and cosmetic problem (four patients).
Discussion
Although SE is a nonlethal condition, it is often troubling to patients and their families. Once air enters the subcutaneous space of the chest wall, it dissects into the soft tissues of the face, neck, upper chest, and shoulders. That results in cosmetic deformities but rarely results in any physiologic problems such as tension pneumomediastinum, pneumothorax, or pneumopericardium [7].
We did not find any article about classification and large case series of SE in the literature. However, we found multiple case reports with different causes and management. Chest trauma, as a major cause of SE, can cause air to enter the skin of the chest wall from the neck or lung [8]. Conditions that cause SE may result from both blunt and penetrating trauma [9]; the trachea may be injured by tracheostomy or tracheal intubation. Overall, in cases of tracheal injury, large amounts of air can enter the subcutaneous space [10]. An endotracheal tube can puncture the trachea or bronchi and can cause SE [11]. Another main cause of SE, along with pneumothorax, is improper functioning of the chest tube [10]. Thus, SE is often a sign that shows something is wrong with a chest tube; it may be clogged, clamped, or out of place [10]. The tube may need to be replaced, or when large amounts of air are leaking, a new tube may be added [10]. Mechanical ventilation can force air into the tissues and worsen a pneumothorax. Occurrence of SE in mechanically ventilated patients may signify the presence of the pneumothorax [10].
In our patients, the causes of SE are classified into main grade 4 or >5, and overall, trauma was the most common, but it was different in each grade. The most common cause of SE was pneumothorax with background of COPD in grade 3, trauma due to rib fracture in grade 4, and iatrogenicity in grade 5. Barotrauma was the other cause of SE, but it was seen rarely. In a case report by Beck and colleagues [2], the cause of SE was community-acquired pneumonia with background of COPD. In addition, the cause was iatrogenicity and trauma in some other case reports [1, 3, 12]. Significant cases of SE are easy to diagnose because of the characteristic signs and symptoms. On a chest X-ray, SE may be seen as radiolucent striations in the pattern which outlined the pectoralis major muscle fibers. Air in the subcutaneous tissues may interfere with radiography of the chest, potentially obscuring serious conditions such as pneumothorax [13]. It can also reduce the effectiveness of chest ultrasound [14]. On the other hand, SE may become apparent in chest X-rays before a pneumothorax [15]. SE can also be seen in CT scans, with the air pockets appearing as dark areas [15]. Diagnosis in our patients was performed by detection of thoracic crepitus; swelling of the neck, chest wall, eyelid, scalp, and abdomen; and presence of air inside the soft tissue confirmed by combinations of chest roentgenogram and thoracic computed tomography. SE does not need treatment in the majority of cases. However, if the amount of air is large, it can interfere with breathing and be intolerable for the patients, so it occasionally progresses to a state of “massive SE” which is quite uncomfortable and requires surgical drainage [16]. When the amount of air pushed out of the airways or lung becomes massive, usually due to positive pressure ventilation, the eyes will be obscured by the swollen eyelids, making the patient sightless [2]. Also, the pressure of the air may impede the blood flow to the areolae of the breast and skin of the scrotum or labia. This can lead to necrosis of the skin in these areas, so it is an urgent situation and requires rapid and adequate decompression [17]. In severe cases, it can compress the trachea and requires emergency intervention [18]. Various approaches have been described, including the use of subcutaneous incisions, needles, or drains [3–6, 9]. Cervical mediastinotomy is another option and used when these interventions do not relieve increasing respiratory distress [19].
In severe cases of SE, catheters can be placed in the subcutaneous tissue to release the air [2]. Small cuts, or “blow holes,” may be made in the skin to release the gas [20, 21]. When SE occurs due to pneumothorax, a chest tube is frequently used, which controls and eliminates the source of the air entering the subcutaneous space [10]. If the volume of subcutaneous air increases, the chest tube cannot remove air from pleural space, so it seems the chest tube should be replaced by a larger one [19]. Suction may also be applied to the tube to remove air faster [19]. Since treatment usually involves dealing with the underlying condition, cases of spontaneous SE may require nothing more than bed rest, control of pain, and perhaps supplemental oxygen [9]. Breathing oxygen may help the body to absorb the subcutaneous air more quickly [20]. Reassurance and observation are also part of the treatment in a mild form of SE [22].
SE in our patients was managed by two infraclavicular incisions for all patients and chest tube insertion in patients without chest tube. In a report by Herlan and colleagues [3], four patients with SE were managed with bilateral 3-cm infraclavicular incisions down to the pectoralis fascia. Then, the progressive subcutaneous dissection was acutely decompressed, and SE was resolved in all four patients without any additional invasive therapy.
Most complications of infraclavicular incision include occlusion of incision by clot, bleeding, insufficient depth of incision in thoracic fascia, and cosmetic problem. The advantages of infraclavicular incisions are rapid resolution of SE, improvement in appearance of patients and releasing the patients, and their entourage from stress.
Conclusion
In the literature, we did not find the classification of SE. We classified SE into five grades. These approaches are performed easily at the bedside. Several techniques have been used to treat SE, but many of those techniques are inefficient and intolerable. For management of patient, we used infraclavicular incision to decrease the severity of emphysema, so that these incisions improved the status of the patients.
Acknowledgments
Conflict of Interest
None declared.
Abbreviation
- SE
Subcutaneous emphysema
Contributor Information
Manouchehr Aghajanzadeh, Email: maghajanzadeh2012@yahoo.com.
Anosh Dehnadi, Email: dehnadi@gtrc.ir.
Hannan Ebrahimi, Phone: +98-131-5542460, FAX: +98-131-5530169, Email: hannan_1367@yahoo.com.
Morteza Fallah Karkan, Email: morteza_brilliant@yahoo.com.
Sina Khajeh Jahromi, Email: sina.khajehjahromi@gmail.com.
Alireza Amir Maafi, Email: alireza_am427@yahoo.com.
Gilda Aghajanzadeh, Email: gilda.aghajanzadeh@yahoo.com.
References
- 1.Rojas M, Rojas P, Toro C, Pinto D, Cifuentes C, Henríquez I, et al. Subcutaneous emphysema after ultrasonic treatment: a case report. Int J Odontostomatol. 2009;3(1):67–70. [Google Scholar]
- 2.Beck P, Heitman S, Mody C. Simple construction of a subcutaneous catheter for treatment of severe subcutaneous emphysema. Chest. 2002;121(2):647–649. doi: 10.1378/chest.121.2.647. [DOI] [PubMed] [Google Scholar]
- 3.Herlan DB, Landreneau R, Ferson P. Massive spontaneous subcutaneous emphysema. Acute management with infraclavicular ‘blow holes’. Chest. 1992;102(2):503–505. doi: 10.1378/chest.102.2.503. [DOI] [PubMed] [Google Scholar]
- 4.Nair K, Neville E, Rajesh P, Papaliya H. A simple method of palliation for gross subcutaneous surgical emphysema. J R Coll Surg Edinb. 1989;34(3):163–164. [PubMed] [Google Scholar]
- 5.Terada Y, Matsunobe S, Nemoto T, Tsuda T, Shimizu Y. Palliation of severe subcutaneous emphysema with use of trocar-type chest tube as a subcutaneous drain. Chest. 1993;103:323. doi: 10.1378/chest.103.1.323a. [DOI] [PubMed] [Google Scholar]
- 6.Rydell J, Jennings W. Emergency cervical mediastinotomy for massive mediastinal emphysema. Arch Surg. 1955;70:647–653. doi: 10.1001/archsurg.1955.01270110019004. [DOI] [PubMed] [Google Scholar]
- 7.Tonnesen A, Wagner W, Mackey-Hargadine J. Tension subcutaneous emphysema. Anesthesiology. 1985;62:90–99. doi: 10.1097/00000542-198501000-00022. [DOI] [PubMed] [Google Scholar]
- 8.DeGowin R, Brown D. DeGowin’s diagnostic examination. New York: McGraw-Hill Medical; 2004. pp. 388–552. [Google Scholar]
- 9.Parker G, Mosborg D, Foley R, Stiernberg C. Spontaneous cervical and mediastinal emphysema. Laryngoscope. 1990;100(9):938–940. doi: 10.1288/00005537-199009000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Lefor A. Critical care on call. New York: McGraw-Hill Medical Division; 2002. pp. 238–240. [Google Scholar]
- 11.Olive P. Subcutaneous emphysema. Radiol Technol. 2006;77(4):296. [PubMed] [Google Scholar]
- 12.Perraut M, Gilday D, Reed G. Traumatic occurrence of chest wall tamponade secondary to subcutaneous emphysema. CJEM. 2008;10(4):387–391. doi: 10.1017/s1481803500010435. [DOI] [PubMed] [Google Scholar]
- 13.Criner GJ, Barnette RE, D’Alonzo G. Critical care study guide: text and review. Berlin: Springer; 2010. p. 169. [Google Scholar]
- 14.Gravenstein N, Lobato E, Kirby R. Complications in anesthesiology. Hagerstown: Lippincott Williams & Wilkins; 2007. p. 171. [Google Scholar]
- 15.Wicky S, Wintermark M, Schnyder P, Capasso P, Denys A. Imaging of blunt chest trauma. Eur Radiol. 2000;10(10):1524–1538. doi: 10.1007/s003300000435. [DOI] [PubMed] [Google Scholar]
- 16.Abu-Omar Y, Catarino P. Progressive subcutaneous emphysema and respiratory arrest. J R Soc Med. 2002;95(2):90–91. doi: 10.1258/jrsm.95.2.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Maunder R, Pierson D, Hudson L. Subcutaneous and mediastinal emphysema. Pathophysiology, diagnosis, and management. Arch Intern Med. 1984;144(7):1447–1453. doi: 10.1001/archinte.1984.00350190143024. [DOI] [PubMed] [Google Scholar]
- 18.Carpenito-Moyet L. Nursing care plans and documentation: nursing diagnoses and collaborative problems. Hagerstown: Lippincott Williams & Wilkins; 2004. p. 889. [Google Scholar]
- 19.Long B, Phipps W, Cassmeyer V. Adult nursing: nursing process approach. London: Mosby; 1995. p. 328. [Google Scholar]
- 20.Sciortino CM, Mundinger GS, Kuwayama DP, Yang SC, Sussman MS. Case report: treatment of severe subcutaneous emphysema with a negative pressure wound therapy dressing. Eplasty. 2009;9:e1. [PMC free article] [PubMed] [Google Scholar]
- 21.Kubik T, Niewiński G, Wojtaszek M, Andruszkiewicz P, Kański A. The skin incisions (blow holes) for treatment of massive subcutaneous emphysema. Anestezjol Intens Ter. 2011;43(2):93–97. [PubMed] [Google Scholar]
- 22.Jain P, Vanner T (2008) Subcutaneous emphysema with pneumomediastinum during the second stage of labour: a rare intrapartum complication. Int J Gynecol Obstet 9(1)