Abstract
The immediate hip spica casting is a popular treatment method for femoral fractures in the pediatric age group. Femoral shortening is the unacceptable result for the treatment. In this technique, we tried to describe the immediate spica casting technique pinning with double K-wire in preschool children and evaluate the results with this method. Sixteen patients (ten boys and six girls) are treated with this technique. Patients were treated under general anesthesia in the operating room. K-wire was introduced in the supracondylar area of the femur passing from the lateral to the medial side through both cortexes, and removed from the skin in the medial section. A second K-wire was introduced through the lateral side of the proximal fragment. While an assistant was applying traction to the pin to maintain the reduction, the lower extremity was put in a spica cast on the fractured side, while the knee joint on the other side was excluded from the spica casting process. The angulation after hip spica cast applied was 9.1° (range 7°–12°) on the frontal plane and 8.9° (range 5°–17°) on the sagittal plane. After spica cast removal, it was 8.5° (range 5°–13°) on the frontal plane and 9° (range 5°–17°) on the sagittal plane. No significant difference was found. The final mean leg length discrepancy was 4.8 mm (range 0–10 mm) at the time of cast removal. This technique may be effective for femoral diaphyseal fractures in preschool children to combine the spirits of external fixation with hip spica casting in one construct in order to correct angular deformities and length discrepancies.
Keywords: Femoral fractures, Hip spica cast, Children, Treatment
Introduction
Diaphyseal femur fractures are frequently seen injuries in children and constitute 1.6 % of all fractures [1–5]. These fractures have been treated adequately by several methods: skeletal traction, early or immediate spica cast, incorporated early spica cast, intramedullar elastic nailing, plate fixation, and external fixation [1–3, 6, 7]. Each of these methods has advantages or disadvantages [4, 8].
Immediate or early spica cast is used in order to shorten hospital admissions, to reduce treatment costs, and to allow the patient to return to his/her family earlier [1, 2, 8, 9]. However, reduction loss has been developed. The angulation and shortness is unacceptable important result of this method [1, 3, 9, 10]. Incorporated spica casting is recommended for reducing correction loss and shortness [11, 12]. This method can be reduced or prevented only by axial movement of the distal fragment on the frontal and sagittal planes, but cannot be prevented to the movement of the proximal fragment [12–15]. We hypothesize that reduction loss and shortness can be prevented or reduced more effectively by reducing the movement of both proximal and distal fragments within the spica cast. According to this hypothesis, we applied a new technique that prevented the movement of the fragments with a K-wire introduced through both proximal and distal fragments in addition to early spica casting, considering that this would help in preventing the development of angulations and shortness.
In this study, we describe an immediate spica casting technique with double pinning in children and evaluate the results obtained from patients treated with this method.
Materials and Methods
Approval from the local ethical committee was obtained for the study. Children 3–8 years old with isolated femur fractures were included. Patients with additional organ injuries, multiple fractures, and/or open fractures were excluded. Fractures were classified according to their shapes and locations in plain radiographs. After all the patients had been assessed by other clinics in the emergency trauma room, those of appropriate general status were admitted to the operating room.
Surgical Technique
Patients underwent surgery under general anesthesia in the emergency operating room. The fractured extremity was covered after a thorough skin cleaning process. A K-wire of 2.5 mm was introduced in the supracondylar area passing from the lateral to the medial side through both cortexes, and removed from the skin in the medial section. A second K-wire of 2.5 mm was introduced through the lateral side of proximal fragment, and it was allowed to pass 1–2 mm in the second cortex. In order to avoid damaging soft tissues, the wire was not passed further through the medial section. Then reduction was achieved by means of traction of the K-wire passing through the supracondylar area. At that time, reduction was checked under fluoroscopic control. The cast was applied after the reduction was found to be appropriate. While an assistant was applying traction to the pin to maintain the reduction, the lower extremity was put in a spica cast on the fractured side, while the knee joint on the other side was excluded from the spica casting process. Then, the cast was allowed to settle, and the reduction was checked again. The cast was applied with 40° hip-and-knee flexion and 30° hip abduction with slight external rotation and was incorporated to the traction pin. Anesthesia was stopped after spica casting. A single dose of cephazoline sodium of 100 mg/kg IV was administered for prophylaxis. The patients were usually discharged the day after the application of the cast.
Evaluation of the Results
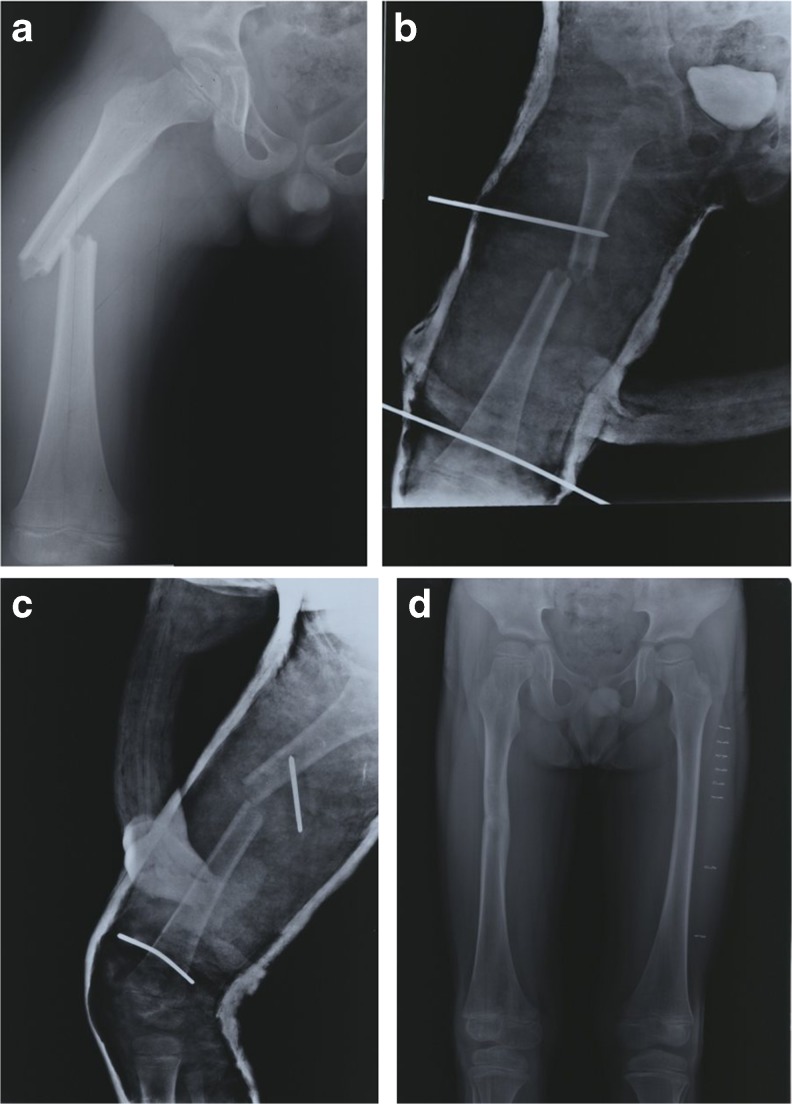
On the anterior–posterior (AP) and lateral radiographs obtained after spica casting on the patients (Fig. 1a–d), the degrees of angulations and overriding on the frontal and sagittal planes were evaluated; patients were controlled with radiograph imaging once a week for the first 2 weeks after being discharged from the hospital, and then once every 4 weeks. If callus formation was satisfactory, the pins were removed. In the radiographs obtained, it was checked whether reduction loss and changes in angulations of the frontal and sagittal planes had occurred. Fracture healing was evaluated in the radiographs in the 7th and 8th weeks. Appearance of callus tissue in at least three cortexes as observed in the radiographs was regarded as recovery, and the spica casts were removed, with the patients instructed to apply controlled load for at least another 2 weeks. After the removal of the spica casts, the distance between the SIAS and the medial malleolus was measured and recorded. It was determined whether there was a difference in length compared to the other extremity. Femoral malrotation was defined as a difference in the internal rotation of the hip of more than 10° between the injured and uninjured sides, and shortness of less than 1 cm was considered acceptable. In the radiographs, angulations of 10° or less on the frontal plane were considered excellent, with 11°–20° acceptable. Moreover, 20° or less on the sagittal plane was considered an excellent result, while angulations of 21°–30° were acceptable. Angulations larger than 20° on the frontal plane and greater than 30° on the sagittal plane were assessed as malunion [5].
Fig. 1.
Radiographs of a 6-year-old boy after a vehicle accident. a X-rays after fracture. b AP radiograph after immediate spica casting with double K-wire. c Lateral radiograph after immediate spica casting with double K-wire. d Radiograph after removal of the spica cast
Statistical Analysis
Mean and standard deviation were calculated for descriptive statistics of continuous variables and median values for discrete variables. The Kolmogorov–Smirnov test was used to analyze the normality of data. The Wilcoxon signed ranks test was used to compare the values of frontal and sagittal plane angulations at early postoperative time and cast removal. Two-tailed hypothesis was considered in the analyses, and the significant differences was accepted while p ≤ 0.05. SPSS 15.0 Software for Windows (SPSS Inc., Chicago, IL, USA) was used in the evaluation of statistical analyses.
Results
Sixteen patients including ten boys and six girls were treated with this technique and were followed up for an average of 29.7 months (range 22–38 months). The average age was 5.4 years (range 3–8 years), and 11 fractures were on the right side and five on the left side. The fractures in nine patients occurred as a result of car accidents, and the other seven after a fall. The duration of hospitalization was 1.3 days (range 1–2 days). With respect to type of the 16 fractures, 7 were spiral, 5 were oblique, and 4 were transverse, while 12 fractures were located at 1/3 mid-diaphysis, 2 were at 1/3 proximal, and 2 were at 1/3 distal part of the femur (Table 1).
Table 1.
Demographics of the patients
| Patient no. | Sex | Age | Fracture type | Fracture level | Cause | Side |
|---|---|---|---|---|---|---|
| 1 | M | 6 | Spiral | Mid-shaft | MVA | R |
| 2 | M | 6 | Spiral | Mid-shaft | MVA | R |
| 3 | F | 5 | Transverse | Proximal | Fall | R |
| 4 | M | 8 | Oblique | Mid-shaft | MVA | R |
| 5 | F | 7 | Spiral | Mid-shaft | Fall | R |
| 6 | M | 4 | Oblique | Mid-shaft | MVA | L |
| 7 | F | 6 | Transverse | Distal | Fall | L |
| 8 | F | 6 | Spiral | Mid-shaft | Fall | L |
| 9 | M | 3 | Oblique | Mid-shaft | Fall | L |
| 10 | M | 4 | Spiral | Mid-shaft | MVA | R |
| 11 | M | 5 | Transverse | Distal | MVA | R |
| 12 | M | 4 | Spiral | Mid-shaft | Fall | R |
| 13 | F | 5 | Spiral | Mid-shaft | MVA | L |
| 14 | M | 6 | Transverse | Mid-shaft | MVA | R |
| 15 | M | 5 | Oblique | Proximal | MVA | R |
| 16 | F | 6 | Oblique | Mid-shaft | Fall | R |
M male, F female, MVA motor vehicle accident, Mid-shaft mid-diaphyseal, R right, L left
In radiographs obtained after spica casting, the angulation was 9.1° (range 7°–12°) on the frontal plane and 8.9° (range 5°–17°) on the sagittal plane. In radiographs after spica cast removal, values were 8.5° (range 5°–13°) on the frontal plane and 9° (range 5°–17°) on the sagittal plane. With respect to both the frontal and sagittal planes, there were no statistically significant differences between the radiographs obtained after spica casting and after spica cast removal (p = 0.193 for frontal plane; p = 0.684 for sagittal plane). The mean leg length discrepancy after treatment was 4.8 mm (range 0–10 mm) (Table 2).
Table 2.
Results of the patients
| Patients | Stay (day) | Frontal angulations (deg) | Sagittal angulations (deg) | Final leg length discrepancy (mm) | ||
|---|---|---|---|---|---|---|
| After spica cast | After removed of spica cast | After spica cast | After removed of spica cast | |||
| 1 | 1 | 7 | 5 | 6 | 6 | 2 |
| 2 | 2 | 9 | 10 | 13 | 16 | 4 |
| 3 | 1 | 10 | 7 | 17 | 15 | 0 |
| 4 | 1 | 12 | 12 | 5 | 6 | 5 |
| 5 | 2 | 10 | 13 | 14 | 17 | 5 |
| 6 | 1 | 11 | 9 | 10 | 12 | 4 |
| 7 | 1 | 10 | 10 | 8 | 10 | 8 |
| 8 | 2 | 8 | 8 | 5 | 5 | 5 |
| 9 | 1 | 7 | 5 | 6 | 5 | 7 |
| 10 | 1 | 9 | 5 | 6 | 6 | 0 |
| 11 | 1 | 7 | 7 | 8 | 6 | 5 |
| 12 | 2 | 10 | 12 | 8 | 8 | 0 |
| 13 | 1 | 8 | 7 | 6 | 5 | 5 |
| 14 | 2 | 9 | 9 | 12 | 10 | 6 |
| 15 | 1 | 10 | 9 | 13 | 12 | 10 |
| 16 | 1 | 9 | 8 | 5 | 5 | 10 |
| Mean | 1.3 | 9.1 | 8.5 | 8.9 | 9.0 | 4.8 |
Thirty-two pins in total were used in 16 patients. No pin tract infections, soft tissue infections, or deep infections were observed in the follow-ups. No iatrogenic nerve injury developed.
Discussion
Immediate and early closed reduction and hip spica casting is an accepted nonsurgical treatment method for children with isolated femoral shaft fractures, especially in patients younger than 10 years of age, because it is safe and reliable, and healing is fast [1, 3, 6]. Re-reduction is performed or a wedge is removed in order to correct the angulations and shortness that have developed in patients treated with immediate or early spica casting [3, 6, 9, 10]. In unsuccessful cases, skeletal traction or surgical methods are used [3, 8, 9]. Such repeated interventions increase the treatment costs [16], and both the patient and healthcare professionals are exposed to radiation due to frequent use of X-rays or fluoroscopy. This is a disadvantage of the technique [3].
Unacceptable shortness remains a problem in this method. More than 1.5–2 cm of shortness in children of 2–10 years of age and of more than 1 cm in older children are considered unacceptable [1, 9, 10]. Illgen et al. reported that a shortness of more than 20 mm developed in 20 % of early spica cast applications, while Thompson et al. reported 19 % and Martinez et al., 43 % [1, 9, 10]. Spinner et al. reported that K-wire and incorporation application could control angulations and shortness in children over 3 years of age [13]. Development of shortness was reduced, but it could not be completely prevented using immediate and early spica casting and incorporation methods [8, 14]. Shortness develops due to insufficient stabilization of axial movements of the proximal and distal fragments. Using the incorporation method, the axial movement of the distal fragment could be prevented; however, the shortness that developed due to insufficient stability of the proximal fragment could not be avoided. We think that the double pinning technique prevents the development of shortness after reduction, because the K-wires located in both proximal and distal fragments limit their axial movement.
In immediate and early spica casting, reduction loss occurs and angulations develop on the frontal and sagittal planes [1, 3, 9, 11]. Wright [15] reported that reduction loss and unacceptable angulations developed in 11 % of patients, while Epps et al. [11] reported 6 % and Thompson et al. [9] 6.9 %. Angulations develop due to the influence of muscle power affecting fractured fragments. We think that the double K pinning prevents angulation as it constraints the movement of the proximal and distal fragments on the AP and lateral planes, and this hypothesis is supported with no reduction loss observed in our cases.
Another problem seen in immediate and early spica casting is wedge removal or cast change due to reduction loss. Re-reduction was reported in 20 % of cases by Illgen et al., 8.9 % by Casinelli et al., and 6.9 % by Thompson et al. [1, 3, 6, 9]. Complications occur as a result of the correction of reduction by wedge removal, and both the patient and the treatment staff are exposed to radiation. Both cast changing and wedge removal processes also cause an increase in costs. No wedge removal or cast changing was required in our cases, as no reduction loss or shortness developed. As double pinning requires no second process, we think that this technique will reduce treatment costs.
It was reported that peroneal nerve injury or compartment syndrome developed following a high-energy trauma treated with spica casting, or reduction performed by wedge removal or 90/90 immediate spica casting [6, 8, 14]. Although our number of cases was small, no iatrogenic peroneal nerve injury was observed following the application of this method.
Buehler et al. and Thompson et al. defined and used the telescope test in order to determine unstable fractures [9]. Casinelli et al. do not recommend early spica casting for fractures with an initial shortness of more than 20 mm [3], because displacement will increase in early spica casting. However, displacement remained stable in our technique both in the proximal and distal fragments without regard to the initial shortness or a positivity of over 3 cm as determined in the telescope test. Therefore, the telescope test or evaluation of initial displacement was not required while applying this technique.
One of the most important complications expected due to this technique is pin tract infection. Pin tract infection was reported in patients treated with incorporated immediate spica casting; however, no deep infection or osteomyelitis was observed [12, 16, 17]. No pin tract infections were seen in our cases. However, it is difficult to draw a conclusion due to the small number of cases. We think that the risk of infection may be reduced by paying special attention to sterilization conditions during the penetration of K-wires.
In conclusion, we think that early or immediate spica casting using double pinning is an effective method for femoral diaphyseal fractures in children, although the number of study cases is limited and only early results are reported.
Acknowledgments
Conflict of Interest
The authors did not have any financial and personal relationships with other people or organizations that could inappropriately influence (bias) their work.
References
- 1.Illgen R, 2nd, Rodgers WB, Hresko MT, et al. Femur fractures in children: treatment with early sitting spica casting. J Pediatr Orthop. 1998;18:481–487. [PubMed] [Google Scholar]
- 2.Shapiro F. Fractures of the femoral shaft in children: the overgrowth phenomenon. Acta Orthop Scand. 1981;52:649–655. doi: 10.3109/17453678108992162. [DOI] [PubMed] [Google Scholar]
- 3.Cassinelli EH, Young B, Vogt M, et al. Spica cast application in the emergency room for select pediatric femur fractures. J Orthop Trauma. 2005;19:709–716. doi: 10.1097/01.bot.0000184146.82824.35. [DOI] [PubMed] [Google Scholar]
- 4.Flynn JM, Schwend RM. Management of pediatric femoral shaft fractures. J Am Acad Orthop Surg. 2004;12:347–359. doi: 10.5435/00124635-200409000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Blasier R, Thompson G, Rab G. Hip, pelvis and femur: pediatric aspect. In: Beaty J, editor. Orthopedic knowledge update 6. Rosemont: American Academy of Orthopedic Surgeons; 1999. pp. 409–425. [Google Scholar]
- 6.Weiss AP, Schenck RC, Jr, Sponseller PD, et al. Peroneal nerve palsy after early cast application for femoral fractures in children. J Pediatr Orthop. 1992;12:25–28. doi: 10.1097/01241398-199201000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Kesemenli CC, Subasi M, Arslan H, et al. Is external fixation in pediatric femoral fractures a risk factor for refracture. J Pediatr Orthop. 2004;24:17–20. doi: 10.1097/01241398-200401000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Czertak DJ, Hennrikus WL. The treatment of pediatric femur fractures with early 90–90 spica casting. J Pediatr Orthop. 1999;19:229–232. doi: 10.1097/01241398-199903000-00018. [DOI] [PubMed] [Google Scholar]
- 9.Thompson JD, Beuhler KC, Sponseller PD, et al. Shortening in femoral shaft fractures in children treated with spica cast. Clin Orthop Relat Res. 1997;338:74–78. doi: 10.1097/00003086-199705000-00010. [DOI] [PubMed] [Google Scholar]
- 10.Martinez AG, Carroll NC, Sarwark JF, et al. Femoral shaft fractures in children treated with early spica cast. J Pediatr Orthop. 1991;11:712–716. doi: 10.1097/01241398-199111000-00002. [DOI] [PubMed] [Google Scholar]
- 11.Epss HR, Molenaar E, O'Conner DP. Immediate single-leg spica cast for pediatric femoral diaphysis fractures. J Pediatr Orthop. 2006;26:491–496. doi: 10.1097/01.bpo.0000217724.08794.e4. [DOI] [PubMed] [Google Scholar]
- 12.Çeliker O, Cetin I, Sahlan S, et al. Femoral shaft fractures in children: technique of immediate treatment with supracondylar Kirschner wires and one and a half spica cast. J Pediatr Orthop. 1998;8:580–584. doi: 10.1097/01241398-198809000-00017. [DOI] [PubMed] [Google Scholar]
- 13.Spinner M, Freundlich BD, Miller IJ. Double spica technic for primary treatment of fractures of the shaft of the femur in children and adolescents. Clin Orthop Relat Res. 1967;53:109–114. doi: 10.1097/00003086-196707000-00012. [DOI] [PubMed] [Google Scholar]
- 14.Mubarek SJ, Frick S, Sink E, et al. Volkmann contracture and compartment syndromes after femur fractures in children treated with 90/90 spica casts. J Pediatr Orthop. 2006;26:567–572. doi: 10.1097/01.bpo.0000230329.06460.f7. [DOI] [PubMed] [Google Scholar]
- 15.Wright JG. The treatment of femoral shaft fractures in children: a systematic overview and critical appraisal of the literature. Can J Surg. 2000;43:180–189. [PMC free article] [PubMed] [Google Scholar]
- 16.Aksahin E, Celebi L, Yüksel HY, et al. Immediate incorporated hip spica casting in pediatric femoral fractures: comparison of efficacy between normal and high-risk groups. J Pediatr Orthop. 2009;29:39–43. doi: 10.1097/BPO.0b013e3181924349. [DOI] [PubMed] [Google Scholar]
- 17.Sahin V, Baktır A, Turk CY, et al. Femoral shaft fractures in children treated by closed reduction and early spica cast with incorporated supracondylar Kirschner wires: a long-term follow-up results. Injury. 1999;30:121–128. doi: 10.1016/S0020-1383(98)00236-8. [DOI] [PubMed] [Google Scholar]