Abstract
Background.
Assessing volume of physical activity (PA) in older adults is critical to understanding the role that PA has on health outcomes and the effectiveness of treatment interventions to increase PA. The purpose of this study was to investigate the psychometric properties of a novel computer-animated self-report questionnaire designed to assess walking activity of older adults: the Mobility Assessment Tool for Walking—the MAT-W.
Methods.
We recruited 249 older adults (66.9±4.7 years, 71% female, 32% black) with cardiovascular disease and/or metabolic syndrome as part of the Cooperative Lifestyle Intervention Program-II study. Participants completed the MAT-W at baseline and after 6 months of a walking and weight loss (n = 78) or weight loss only (n = 69) intervention. Test–retest reliability was assessed in 31 participants. Walking speed at usual and fast pace was measured using a GAITRite mat, and 7-day accelerometry data were collected at baseline and 6 months. The mCHAMPS5, a modified version of a widely used self-report PA questionnaire, was completed at baseline.
Results.
The test–retest reliability of MAT-W was excellent (intraclass correlation coefficient > .85). The MAT-W was correlated with mCHAMPS5 (Spearman r = .66, p < .001) and moderate/vigorous levels of PA as assessed by accelerometry (Spearman r = .65, p < .001) and was responsive to an intervention-induced change in PA at 6 months when comparing the Cooperative Lifestyle Intervention Program-II walking and weight loss group with the weight loss only group (p < .001).
Conclusion.
The MAT-W is a brief, reliable, and valid tool to assess PA and has promise for the assessment of walking behavior in older adults under free-living conditions.
Key Words: Physical activity assessment, Self-report measure, Exercise, Mobility
Reductions in the volume of physical activity (PA) play a central role in the progression of chronic disease, mobility disability, and obesity in older adults (1). Accurate assessment of the volume of PA is critical to our understanding of the role that it has on various health outcomes and the efficacy or comparative effectiveness of treatment interventions designed to increase PA. PA is most commonly assessed using self-report measures or objective activity monitoring using accelerometry (2–4). In this article, we examine self-reported walking activity because walking is, by far, the most common form of PA undertaken by older adults (5–7). Walking is associated with positive health benefits and can be done by older adults with a wide range of functional abilities (1). The current article focuses on the description and psychometric evaluation of a novel measure for assessing walking behavior in older adults, the Mobility Assessment Tool for Walking—MAT-W.
Assessing volume of PA by accelerometry has become a widely used objective method. However, accelerometry does have its limitations. Although unit cost and burden on both research staff and participants can be prohibitive, more importantly, when using accelerometry, there is no simple method to determine cut points for identifying moderate levels of PA in older adults, who frequently have a wide range of functional capacity (8–10). To further complicate assessment, existing self-report measures of PA designed for older adults rely on verbal descriptions of activities, which can be misleading. For example, how are phrases such as “walking for exercise” or “brisk walking” interpreted by an older adult? Can a researcher assume that two people who say they walk briskly for 30 minutes each day actually engage in the same behavior?
The MAT-W was designed as a self-report measure for older adults to address these limitations. This measure builds on our previous work where we have used video animations to reduce the ambiguity inherent in verbal descriptions of mobility. Our intent with the MAT-W was to capture the volume of walking behavior that older adults engage in each week by assessing both usual-paced and fast-paced walking. The MAT-W displays video animations of a mannequin walking at a range of speeds and the user selects a pace that they perceive to be representative of their usual or fast pace. Knowing the speed, and the amount of time spent in usual and fast walking, we can compute total volume by combining a novel assessment of intensity (walking speed in this case) together with duration and frequency. Our rationale for this approach is to provide a method that would assist an older adult to make the complex judgment about walking intensity (speed) that can vary widely in older adults with compromised function or disease burden (10).
The specific aims of this study are to describe the MAT-W and to examine the psychometric properties of the instrument. In particular, we hypothesized that (a) the MAT-W will have suitable test–retest reliability (an intraclass correlation coefficient > .70), (b) the usual and fast speeds chosen by participants in the MAT-W will be similar to their measured usual and fast walking speeds, (c) the MAT-W will exhibit moderate to strong relationships with accelerometer-derived and self-report measures of PA, and (d) the MAT-W will be sensitive to change within the context of an ongoing study where one goal of the study design is to increase walking activity in older adults with cardiovascular disease or metabolic syndrome.
Methods
Participants and Testing Procedures
Older adults in this study were part of the Cooperative Lifestyle Intervention Program-II (CLIP-II), an 18-month duration community-based randomized controlled trial investigating the effects of exercise and weight loss on mobility in older adults with cardiovascular disease and/or metabolic syndrome. The research design, inclusion/exclusion criteria, and methods including the interventions have been reported in detail (11). Briefly, participants were aged 60–79 years, community-dwelling, sedentary, had documented evidence of a myocardial infarction, angioplasty, chronic stable angina, cardiovascular surgery or an Adult Treatment Panel II diagnosis of metabolic syndrome, and self-reported difficulty with mobility. We excluded individuals with severe or uncontrolled chronic disease. In this study, we assessed 249 participants at baseline. At 6 months, we assessed 147 participants, 69 of whom were randomized to a weight loss only control and 78 who were randomized to a walking and weight loss intervention. Participants were recruited via targeted mailings to the greater Winston-Salem, North Carolina community.
Participants completed three baseline assessment sessions for the CLIP-II study and here we report only those assessments relevant to the current analyses. At the first session, the MAT-W was administered along with the mCHAMPS5, a modified version of a widely used self-report PA questionnaire (see description below). At the second session, usual and fast walking speeds were measured on the GAITRite mat, and an accelerometer was provided to the participant with detailed instructions on proper placement and use for a 7-day period. All the assessments were repeated at the 6-month follow-up visits for 147 participants. A subset of participants (n = 31) completed test–retest sessions on the MAT-W to assess reliability of the instrument after they were engaged in the intervention so that there was some heterogeneity in responses. These sessions were 7–12 days apart to accommodate individual participant schedules.
Mobility Assessment Tool for Walking
The MAT-W is a computer-based self-report walking activity questionnaire adapted from the technology used in the MAT-sf, a validated tool that assesses mobility in older adults using animations of tasks to reduce measurement error (12,13). The MAT-W uses animated video clips of walking and was designed to provide a detailed assessment of walking activity (Figures 1 and 2). Participants are instructed to recall their walking activity for a typical week in the past month. The questionnaire was administered in a supervised setting with a staff member available to answer questions as needed. In our testing with the current sample, the MAT-W took approximately 3.5 minutes (range: 2–6 minutes).
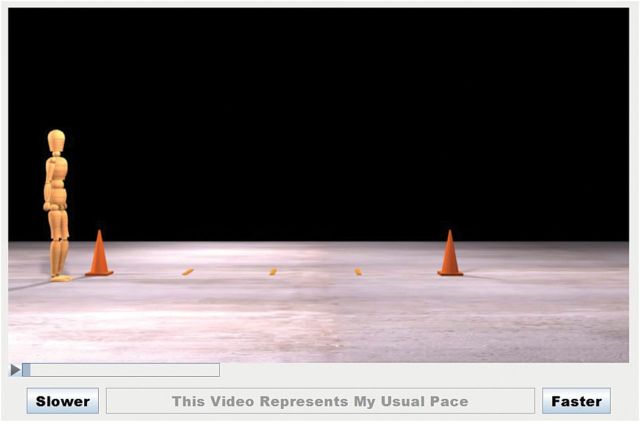
Figure 1.
Screenshot of Mobility Assessment Tool for Walking speed animation.
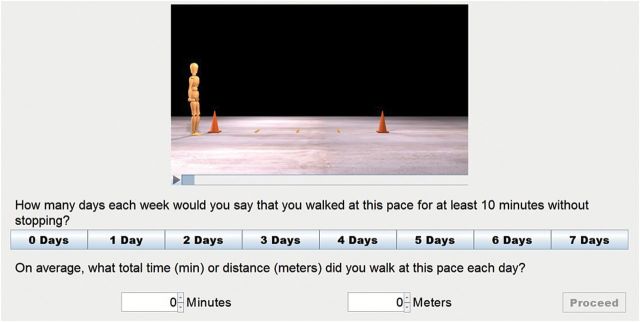
Figure 2.
Screenshot of Mobility Assessment Tool for Walking volume items.
Following a welcome page with instructions for the test, participants self-selected their usual walking pace from a series of animations described as “the pace that you typically walk if there is no rush to get somewhere.” The five animations spanned a range of speeds that older adults may potentially walk: 0.72 mph (0.32 m/s), 1.52 mph (0.68 m/s), 2.24 mph (1.00 m/s), 2.68 mph (1.20 m/s), and 3.36 mph (1.50 m/s). The first animation presented on screen shows a 4-m walk at a speed of 1 m/s. Participants are instructed to decide if the walking speed shown represents their usual walking pace, or whether they perceive their usual walking pace is faster, or slower. The participant can then select another animation by using the “Slower” and “Faster” buttons (Figure 1). Adjustments are allowed until the participant believes the pace shown in the animation represents their usual walking pace. They then select a button labeled: “This Video Represents My Usual Walking Pace.”
After the participant selects their usual walking pace, they indicate the number of days (0–7) during the past week in which they walked more than 10 minutes at that pace, along with the total amount of time walked at that pace on those days (Figure 2). If desired, their usual-pace walking speed can be viewed at this time as a reminder to the participant what they meant by their usual walking speed.
The process of selecting walking speed, frequency, and duration as described above is repeated for the participant’s fast walking pace, described as “a pace that would cause sweating, a faster heart rate, or more rapid breathing.” The animations of walking that are shown to the participant in this condition, including the initial clip of a 4-m walk, are the same as those used for the usual walking pace.
The volume of walking in meters per week was calculated as the product of the speed at which participants walked at their usual or fast pace, the duration of walking at each pace, and the frequency of walking at each pace (d/wk). Therefore, we take advantage of the different speeds of movement of both the usual- and fast-paced conditions—an innovation made possible by the inclusion of video of different walking speeds into the MAT-W. The volume measure is used in subsequent analyses related to reliability, validity, and sensitivity to change.
Modified CHAMPS Questionnaire
The mCHAMPS5, a modified version of the Community Health Activities Model Program for Seniors (CHAMPS) PA self-report questionnaire (14), was administered on a computer with the assistance of assessment staff, if necessary. It consists of five items (heavy gardening, fast/brisk walking for exercise, jogging/running, other moderate/vigorous aerobic activities [cycling, step machine], moderate-to-vigorous aerobic dancing) that focus on moderate-to-vigorous intensity activities that are common types of PA performed by older adults. Consistent with the original CHAMPS instrument, participants are asked to recall these activities in a typical week during the past month. The mCHAMPS5 was processed to provide an aggregate duration in minutes of PA on these five items per week. We also looked at the single item of fast/brisk walking for exercise.
Accelerometry
At baseline, prior to randomization and at the 6-month testing visit, participants were given a logbook and an accelerometer (Lifecorder EX, Kenz, Japan), a small hip-mounted uniaxial device that provides data that is comparable with a widely used accelerometer (15,16). Along with verbal instructions, a handout describing use of the accelerometer and logbook for collecting dates and times the device was worn were provided. The LIFEcorder samples vertical acceleration at 32 Hz and assesses values ranging from 0.06 to 1.94g. The acceleration signal is filtered by an analog bandpass filter and digitized. Based on the accelerometer signal, the LIFEcorder categorizes the intensity of the movement into 1 of 9 activity levels every 4 seconds. The signal is categorized into 11 activity levels (0.0, 0.5, and 1.0–9.0; level 0.0 corresponds to <0.06g). The LIFEcorder software considers moderate/vigorous physical activity (MVPA) as a level of four and above. The participant was directed to wear the device during all waking hours for the following 7 days and to return it, together with the logbook, using a stamped addressed envelope.
Accelerometry data were uploaded into the Kenz Physical Activity Analysis Software Lifestyle Coach V1.21 where the data were reviewed, together with the log book, and the wear time period was manually selected. Our goal was to collect a minimum of 5 days of data, each with at least 10 hours of wear time per day (2,17,18). If these criteria were not met (due to either equipment malfunction or inadequate wear time), the participant was given another accelerometer to be worn for the following 7 days. If we were unable to obtain sufficient accelerometry data again, the individual was excluded from analyses involving accelerometry. Accelerometry files were processed to provide minutes of MVPA. Eligible days were then averaged to create the summary accelerometry data used in our analyses.
Objectively Assessed Walking Speed
GAITRite
The usual and fast walking speed was measured using a GAITRite instrumented mat (CIR Systems Inc.). It has good to excellent reliability in a range of cohorts and demonstrates good agreement with spatiotemporal parameters collected using 3-D motion analysis systems (19–21).
The participant started walking 4 m prior to the beginning of the instrumented mat so that they were walking at a constant walking speed. Data were collected on four consecutive trials at a usual walking pace and four consecutive trials at a fast walking pace with a brief rest in between trials while data were saved. The descriptions for the usual and fast walking paces were the same as provided during the MAT-W. Trials where the participant altered their stride to target the beginning or end of the mat were repeated. The walks were grouped as either “usual walking pace” or “fast walking pace” to compute the average walking speed for the four usual-pace and four fast-pace trials.
Statistical Analyses
Tests for normality were performed to determine whether data transformations were appropriate and if nonparametric analyses would be required. The MAT-W was transformed using a square root function to normalize the data. Test–retest reliability of MAT-W walking activity was assessed with intraclass correlation coefficient. Construct validity for the MAT-W self-reported walking speeds was determined using Spearman’s correlations examining MAT-W usual and fast walking speeds and the average walking speeds from the respective GAITRite walking speed trials. MAT-W assessed at baseline was used for walking speed validity analyses.
Validity of the MAT-W walking PA measure was determined using Spearman’s correlations of the MAT-W with accelerometry-derived MVPA and mCHAMPS5 minutes of PA. For the walking PA analysis, we used MAT-W 6-month follow-up scores because the distribution was more heterogeneous at this point in time, that is, at baseline, the majority of participants were reporting no PA. Difference scores between baseline and 6-month values for both the MAT-W and MVPA were computed with Spearman’s correlation to examine the relationship between the changes in these measures.
General linear models were used to explore the MAT-W total, usual, and fast walking volumes at 6 months with treatment (walking and weight loss vs weight loss only) using the baseline MAT-W variable as the covariate in each analysis.
Results
Of the 249 participants tested at baseline, 248 completed the MAT-W and 231 had valid accelerometry data. Three participants had missing data on the GAITRite due to technical issues. Of the 147 participants who completed 6-month testing, 147 completed the MAT-W and 133 had valid accelerometry data. The mean age of our sample was 67 years, most were white females, although 30% of our sample were African American (Table 1). The cognitive function of the sample was relatively high as indicated by the Montreal Cognitive Assessment scores.
Table 1.
Demographic Data at Baseline for All Randomized Participants and for Participants Randomized to the Walking and Weight Loss Group or Weight Loss Group
| All Participants Baseline | Walking and Weight Loss Baseline | Weight Loss Baseline | |
|---|---|---|---|
| N = 248 | N = 86 | N = 82 | |
| Age at baseline (y) | 66.9±4.7 | 67.4±5.1 | 66.3±4.5 |
| BMI (kg/m2) | 34.4±3.7 | 33.9±3.5 | 34.7±4.0 |
| Female sex (n, %) | 177, 71.1% | 62, 72.1% | 59, 72.0% |
| Race (n, %) | |||
| White | 162, 65.1% | 55, 64.0% | 49, 59.8% |
| AA | 80, 32.1% | 30, 34.9% | 30, 36.6% |
| Other | 7, 2.8% | 1, 1.2% | 3, 3.6% |
| MOCA (0–30) | 25.8±2.4 | 25.9±2.4 | 25.9±2.8 |
Notes: AA = African American; BMI = body mass index; MOCA = Montreal Cognitive Assessment. Values are mean ± SD or number and percentage.
Table 2 provides data on usual- and fast-paced walking speed assessed using the GAITRite and minutes of moderate PA reported on the mCHAMPS5, together with the mCHAMPS5 item on minutes of fast/brisk walking, and MVPA measured with accelerometry. At baseline, the accelerometry data indicated that participants in CLIP-II were involved in only an average of 49.5 minutes per week of MVPA, that is, less than an hour out of an estimated ~100h/wk of awake time. These data highlight the sedentary nature of the study cohort. These measures are used to examine the validity of the MAT-W.
Table 2.
Descriptive Data for Measures Used in Validity Assessment and MAT-W Outcomes on Minutes of Walking Activity at Usual or Fast Pace Per Week and Usual and Fast Walking Distance Per Week
| Variable | All Participants | Walking and Weight Loss | Weight Loss | ||
|---|---|---|---|---|---|
| Baseline | Baseline | 6 mo | Baseline | 6 mo | |
| Usual walking speed on GAITRite mat (m/s) | 1.15±0.16 | 1.16±0.17 | 1.21±0.19 | 1.15±0.17 | 1.19±0.20 |
| Fast walking speed on GAITRite mat (m/s) | 1.56±0.20 | 1.57±0.22 | 1.64±0.23 | 1.57±0.21 | 1.63±0.25 |
| mCHAMPS5 (min/wk) | 29.2±91.4 | 25.4±52.9 | 203.7±117.8 | 26.0±69.6 | 79.6±113.7 |
| Fast/brisk walking for exercise item from mCHAMPS5 (min/wk) | 6.7±28.2 | 6.1±17.6 | 187.3±97.9 | 3.1±11.1 | 44.2±82.9 |
| MVPA from accelerometry (min/wk) | 49.5±56.0 | 50.9±60.0 | 174.0±111.8 | 45.5±48.7 | 43.4±43.1 |
| MAT-W | |||||
| Median (25th, 75th percentile) | |||||
| Usual-pace walking duration (min/wk) | 30 (0, 70) | 30 (0, 100) | 145 (70, 202) | 30 (0, 62) | 30 (10, 105) |
| Fast-pace walking duration (min/wk) | 10 (0, 40) | 20 (0, 45) | 160 (60, 225) | 10 (0, 30) | 15 (0, 45) |
| Total walking duration (min/wk) | 50 (0, 120) | 55 (0, 146) | 271 (200, 400) | 34 (0, 116) | 60 (15, 162) |
| Usual-pace distance (m/wk) | 1800 (0, 4200) | 2160 (0, 6345) | 7200 (4200, 13500) | 1440 (0, 3750) | 1800 (600, 7200) |
| Fast-pace distance (m/wk) | 900 (0, 2835) | 1200 (0, 3420) | 12780 (4980, 18450) | 870 (0, 2700) | 1350 (0, 3600) |
| Total distance (m/wk) | 3000 (0, 7725) | 3465 (0, 10035) | 19140 (14100, 28995) | 2205 (0, 6660) | 4260 (930, 12105) |
Notes: MAT-W = Mobility Assessment Tool for Walking; MVPA = moderate/vigorous physical activity. The MAT-W was not normally distributed at baseline because a majority of participants reported no moderate-to-vigorous physical activity (as required by study inclusion criteria). At 6 mo, there was more variability in the data as a result of the differences between the intervention arms (weight loss only, walking and weight loss).
Descriptive data for baseline and follow-up MAT-W outcome variables are provided in Table 2 and include both the amount of time and the distance walked at both the usual- and fast-paced walking speeds. Note that, at baseline, a large number of participants reported no usual- or fast-paced walking because the MAT-W asks participants to indicate the number of days (0–7) during the past week in which they walked more than 10 minutes at that pace, along with the total amount of time walked at that pace on those days.
Using the MAT-W baseline visit, participants reported a median of 50 minutes of walking per week, mainly at their usual walking pace as opposed to their fast pace. At the 6-month follow-up, the total walking time assessed via the MAT-W increased to a median of 200 minutes per week due primarily to changes in the group of older adults that participated in the walking and weight loss intervention (see below).
The reliability of the MAT-W was excellent; the intraclass correlation coefficients were .85 for the usual-pace walking distance, .85 for the fast-pace walking distance, and .89 for the total distance that includes both the usual- and fast-pace data.
To establish the validity of the MAT-W, we first compared the speeds selected in the MAT-W video clips for the usual- and fast-paced walking speeds with the speeds measured during the usual and fast walk trials using the GAITRite mat (Table 3). There were trends for linear increases between speeds selected in the MAT-W and objectively measured walking speed. In addition, we found that the speeds selected for the MAT-W were related to speed data collected using the GAITRite mat for both the usual (Spearman r = .36, p < .001) and fast walking speeds (Spearman r = .45, p < .001).
Table 3.
Baseline Usual and Fast Walking Speed Assessed on the GAITRite Mat and the Number of Participants Who Selected Each MAT-W Animation as Their Usual or Fast Walking Speed
| MAT-W Animation Walking Speed (m/s) | GAITRite Usual Speed (number of participants, average speed in m/s) | GAITRite Fast Speed (number of participants, average speed in m/s) |
|---|---|---|
| 0.32 | 5, 0.93±0.10 | — |
| 0.68 | 50, 1.06±0.13 | 10, 1.39±0.12 |
| 1.00 | 117, 1.16±0.15 | 49, 1.43±0.17 |
| 1.20 | 54, 1.18±0.15 | 97, 1.56±0.21 |
| 1.50 | 19, 1.29±0.18 | 89, 1.66±0.17 |
Notes: MAT-W = Mobility Assessment Tool for Walking. Data are presented as mean ± SD. Note on interpretation: Five participants selected the 0.32 m/s walking speed animation in the MAT-W as their usual walking speed. The measured average usual-pace walking speed for these five individuals was 0.93 m/s. No participant selected the 0.32 m/s animation as their fast speed. Fifty participants selected the 0.68 m/s animation in the MAT-W as their usual walking speed. The measured average usual-pace walking speed for these 50 individuals was 1.06 m/s. Ten participants selected the 0.68 m/s animation in the MAT-W as their fast walking speed. The measured average usual-pace walking speed for these 10 individuals was 1.39 m/s.
Second, evidence for convergent and construct validity was established by correlating the total distance walked from the MAT-W with the mCHAMPS5 score and accelerometry minutes of MVPA, respectively. In these analyses, we used data from the 6-month visit because there was greater heterogeneity in the data at this point in time because the sample comprised participants in the walking and weight loss and weight loss only groups. Using Spearman correlation, the MAT-W had a moderate to high relationship with both the mCHAMPS5 score (r = .66, p < .001) and minutes of MVPA assessed by accelerometry (r = .65, p < .001). The Spearman correlation between the mCHAMPS5 and minutes of MVPA from accelerometry was r = .51 (p < .001). We also computed difference scores for both the MAT-W total score and minutes of MVPA by subtracting baseline from 6-month values and found that there was a significant relationship between change in these two measures (Spearman r = .45, p < .001).
To assess whether the MAT-W was sensitive to change after a 6-month walking intervention, we used linear regression to model the MAT-W scores at 6 months predicted by randomization assignment (walking and weight loss vs weight loss only) and baseline MAT-W scores. Table 4 provides the back-transformed least squared means (95% CI) for each variable by group assignment. Results from these analyses produced significant treatment effects for total walking distance (p < .001, Eta2 = 0.38), usual walking distance (p < .001, Eta2 = 0.18), and fast walking distance (p < .001, Eta2 = 0.37). The Eta2, a measure of effect size, suggests that the effects for total and fast walking distance were substantial in magnitude accounting for close to a third of the variance in the 6-month scores.
Table 4.
Least Squared Means (95% CI) for 6-mo MAT-W Scores for the Walking and Weight Loss Group and the Weight Loss Group
| Total Distance* (m/wk) | Usual-Pace Distance* (m/wk) | Fast-Pace Distance* (m/wk) | |
|---|---|---|---|
| Walking and weight loss | 21066 (18014, 24358) | 8430 (6775, 10267) | 10754 (8905, 12778) |
| Weight loss | 4891 (3401, 6651) | 2734 (1779, 3893) | 1671 (958, 2581) |
Notes: MAT-W = Mobility Assessment Tool for Walking. The means are adjusted for baseline MAT-W score and have been back transformed to aid interpretation.
*p < .001 for the between group comparison.
Discussion
The MAT-W was designed to assess self-reported walking activity performed by older adults using video animation. The primary purpose of the current study was to investigate the reliability and validity of the MAT-W. The intraclass correlation coefficients for the outcomes generated by the MAT-W ranged between .85 and .89 and exceeded our target of >.70. Furthermore, we garnered strong initial support for the validity of the MAT-W.
First, the stepwise progression in average walking speed using data from the GAITRite mat across the five MAT-W speeds illustrates that older adults were able to differentiate between the speed that they actually walked at both their usual and fast pace (Table 3). Obviously, the categorical nature of walking speed options in the MAT-W does not allow a perfect match with the continuous measures of usual and fast speed collected on the GAITRite. A more consistent trend for the ability to discriminate between self-reported speeds was observed for fast-paced walking. For usual walking pace, those with slower walking speeds tended to report that they walked slower than they actually did, whereas those with faster usual walking speeds tended to over report their usual walking pace. For the fast walking pace, everyone in our sample actually walked faster than the speed they selected on the MAT-W. Individuals may have walked faster in the GAITRite walking test than they normally would when engaging in fast-pace walking activity because of the controlled, intermittent, and short duration of the GAITRite test. Future iterations of the MAT-W could incorporate faster walking animations particularly when assessing higher functioning older adults who are capable of walking speeds >1.5 m/s.
Second, comparisons baseline to 6-month data from the mCHAMPS5, the MVPA from accelerometry, and the MAT-W in Table 2 demonstrate the effect of the walking intervention and together with the analysis presented in Table 4 shows that the MAT-W is sensitive to the effects of the walking intervention. These data suggest that the MAT-W is accurately capturing moderate intensity walking behavior. Also, the strength of the correlation between MAT-W scores and accelerometry-derived minutes of MVPA was stronger than typically reported for construct validation of existing self-report measures of PA. For example, commonly reported relationships between the CHAMPS with accelerometry have been between 0.20 and 0.40 (22). In addition to these analyses, the moderate relationship observed between 6-month change in accelerometry and change in the MAT-W is encouraging. These findings provide strong evidence for the efficacy of using the MAT-W to assess change in PA in walking-based interventions with older adults and suggest that the MAT-W may be a valuable assessment tool for large prospective epidemiological studies.
There are a number of strengths and limitations in the current study. Our sample size of 248 exceeds much of the previous literature investigating measurement properties of older adult PA assessments (23,24). We also compared the MAT-W with an objective assessment of PA (accelerometry) and a modified version of a widely used self-report questionnaire (CHAMPS). We also provided an assessment of the sensitivity of the MAT-W to an intervention focused on increasing walking behavior. However, the psychometric properties of an instrument are dependent on the study sample. We achieved our goal of testing an older adult population; however, comparisons with the broader U.S. older adult population indicate that our sample was relatively young (age range of 60–79). Therefore, we cannot say how those of advanced age (75+) would interact with the MAT-W software. In general, the older adult population is characterized by large variability in levels of both physical and cognitive functioning. The inclusion/exclusion criteria of the CLIP-II study focused on those with established cardiovascular disease or metabolic syndrome and created a relatively homogeneous sample because healthy older adults or those with very low function were excluded from the study (11). Our sample had more females than males, which compromises external validity. CLIP-II inclusion criteria dictated that our sample was sedentary at baseline. Only 37.1% of older adults in the United States currently engage in regular PA and therefore our sample reflects the activity level of a large majority of the older adult population (25).
With the number of older adults increasing, focus must be placed on identifying the best ways to measure volume of PA and in particular walking activity because it is the most common form of PA. The MAT-W was reliable and valid and it was sensitive to change in walking behavior caused by the adoption of a walking PA intervention. The MAT-W is quick and easily administered on a laptop or tablet. An assessment of walking behavior could be accomplished while waiting in a physician’s office and serve as a starting point for discussions about PA and health. Further research on the MAT-W could consider fine-tuning the self-reported walking speed component and assessing its reliability and validity in a range of cohorts.
Funding
This work was supported by National Heart, Lung, and Blood Institute (R18HL076441-06A1 to A.P.M. and W.J.R.); National Institutes for Aging Claude D. Pepper Older Americans Independence Center (P30AG021332); and by the Wake Forest Translational Science Institute’s Clinical Research Unit.
Acknowledgments
The authors would like to acknowledge the significant contributions made to the CLIP-II study by Barbara J. Nicklas, PhD, Denise K. Houston, RD, PhD, Leon Lenchik, MD, Paul J. Laurienti, MD, PhD, Michael P. Walkup, Wesley A. Roberson, Patricia A. Davis, and our YMCA partners and staff.
References
- 1. Nelson ME, Rejeski WJ, Blair SN, et al. Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39:1435–1445. [DOI] [PubMed] [Google Scholar]
- 2. Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40:181–188. [DOI] [PubMed] [Google Scholar]
- 3. Kowalski K, Rhodes R, Naylor PJ, Tuokko H, MacDonald S. Direct and indirect measurement of physical activity in older adults: a systematic review of the literature. Int J Behav Nutr Phys Act. 2012;9:148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Troiano RP, McClain JJ, Brychta RJ, Chen KY. Evolution of accelerometer methods for physical activity research. Br J Sports Med. 2014;48:1019–1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Siegel PZ, Brackbill RM, Heath GW. The epidemiology of walking for exercise: implications for promoting activity among sedentary groups. Am J Public Health. 1995;85:706–710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Eyler AA, Brownson RC, Bacak SJ, Housemann RA. The epidemiology of walking for physical activity in the United States. Med Sci Sports Exerc. 2003;35:1529–1536. [DOI] [PubMed] [Google Scholar]
- 7. Centers for Disease Control and Prevention. Vital signs: walking among adults--United States, 2005 and 2010. MMWR Morb Mortal Wkly Rep. 2012;61:595–601. [PubMed] [Google Scholar]
- 8. Evenson KR, Buchner DM, Morland KB. Objective measurement of physical activity and sedentary behavior among US adults aged 60 years or older. Prev Chronic Dis. 2012;9:E26. [PMC free article] [PubMed] [Google Scholar]
- 9. Ozemek C, Cochran HL, Strath SJ, Byun W, Kaminsky LA. Estimating relative intensity using individualized accelerometer cutpoints: the importance of fitness level. BMC Med Res Methodol. 2013;13:53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Rejeski WJ, Axtell R, Fielding R, et al. ; LIFE Study Investigator Group. Promoting physical activity for elders with compromised function: the lifestyle interventions and independence for elders (LIFE) study physical activity intervention. Clin Interv Aging. 2013;8:1119–1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Marsh AP, Janssen JA, Ambrosius WT, et al. The Cooperative Lifestyle Intervention Program-II (CLIP-II): design and methods. Contemp Clin Trials. 2013;36:382–393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Rejeski WJ, Ip EH, Marsh AP, Barnard RT. Development and validation of a video-animated tool for assessing mobility. J Gerontol A Biol Sci Med Sci. 2010;65:664–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Rejeski WJ, Marsh AP, Anton S, et al. ; LIFE Research Group. The MAT-sf: clinical relevance and validity. J Gerontol A Biol Sci Med Sci. 2013;68:1567–1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Stewart AL, Mills KM, King AC, Haskell WL, Gillis D, Ritter PL. CHAMPS physical activity questionnaire for older adults: outcomes for interventions. Med Sci Sports Exerc. 2001;33:1126–1141. [DOI] [PubMed] [Google Scholar]
- 15. Yoshioka M, Ayabe M, Yahiro T, et al. Long-period accelerometer monitoring shows the role of physical activity in overweight and obesity. Int J Obes (Lond). 2005;29:502–508. [DOI] [PubMed] [Google Scholar]
- 16. Abel MG, Hannon JC, Sell K, Lillie T, Conlin G, Anderson D. Validation of the Kenz Lifecorder EX and ActiGraph GT1M accelerometers for walking and running in adults. Appl Physiol Nutr Metab. 2008;33:1155–1164. [DOI] [PubMed] [Google Scholar]
- 17. Matthews CE, Ainsworth BE, Thompson RW, Bassett DR., Jr Sources of variance in daily physical activity levels as measured by an accelerometer. Med Sci Sports Exerc. 2002;34:1376–1381. [DOI] [PubMed] [Google Scholar]
- 18. Hart TL, Swartz AM, Cashin SE, Strath SJ. How many days of monitoring predict physical activity and sedentary behaviour in older adults? Int J Behav Nutr Phys Act. 2011;8:62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bilney B, Morris M, Webster K. Concurrent related validity of the GAITRite walkway system for quantification of the spatial and temporal parameters of gait. Gait Posture. 2003;17:68–74. [DOI] [PubMed] [Google Scholar]
- 20. Menz HB, Latt MD, Tiedemann A, Mun San Kwan M, Lord SR. Reliability of the GAITRite walkway system for the quantification of temporo-spatial parameters of gait in young and older people. Gait Posture. 2004;20:20–25. [DOI] [PubMed] [Google Scholar]
- 21. van Uden CJ, Besser MP. Test-retest reliability of temporal and spatial gait characteristics measured with an instrumented walkway system (GAITRite). BMC Musculoskelet Disord. 2004;5:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hekler EB, Buman MP, Haskell WL, et al. Reliability and validity of CHAMPS self-reported sedentary-to-vigorous intensity physical activity in older adults. J Phys Act Health. 2012;9:225–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Forsén L, Loland NW, Vuillemin A, et al. Self-administered physical activity questionnaires for the elderly: a systematic review of measurement properties. Sports Med. 2010;40:601–623. [DOI] [PubMed] [Google Scholar]
- 24. Helmerhorst HJ, Brage S, Warren J, Besson H, Ekelund U. A systematic review of reliability and objective criterion-related validity of physical activity questionnaires. Int J Behav Nutr Phys Act. 2012;9:103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Schoenborn CA, Adams PF, Peregoy JA. Health behaviors of adults: United States, 2008–2010. Vital Health Stat 10. 2013:1–184. [PubMed] [Google Scholar]