Abstract
There are many differential diagnoses in investigating patients who present with retinal vasculitis, and the laboratory investigations used to investigate this have low-to-moderate sensitivity and/or specificity. Diagnoses include conditions such as tuberculosis or sarcoidosis, which may require long courses of antibiotics or immunosuppression. Influenza vaccination has been recognised as a cause of vasculitis for decades, although a purely ocular presentation is rare. We present a case of a 78-year-old Caucasian woman presenting with a single vessel arterial vasculitis of the right eye 8 weeks following influenza vaccination at her local general practitioner practice. We encourage ophthalmologists, rheumatologists and uveitis specialists to consider influenza vaccine as a cause of ocular vasculitis if the vaccine has been recently administered.
Background
It has been long recognised that influenza vaccination is a cause of systemic vasculitis. Ocular vasculitis alone, without systemic involvement, has been previously described following vaccination for other conditions, but we present a case of purely ocular vasculitis resulting from influenza vaccination. Investigating uveitis is notoriously challenging due to the low sensitivity and specificity of the investigations available, and can lead to inappropriate management if the wrong aetiology is suspected. This case was written principally to highlight the importance of asking patients for recent influenza vaccination if they present with ocular vasculitis, as they may not readily admit this information in their medical history.
Case presentation
A 78-year-old Caucasian woman presented to the University Hospital of Wales eye casualty with a 2-day history of blurred vision in her right eye as well as a right-sided headache. There was no associated eye pain, jaw claudication, photopsia or other feature that might suggest giant cell arteritis, although she did have a medical history of polymyalgia rheumatica (PMR), which is an association. In addition to this, she had a history of atrial fibrillation and a previous mitral valve replacement. She took warfarin for this, as well as 9 mg of prednisolone for the PMR, along with digoxin, omeprazole and calcichew. She had no family history of note. The only history of note beyond this was an injection of a yearly influenza vaccine (Influvac 0.5 mL) at her local general practitioner practice 8 weeks prior to the symptoms starting.
Examination revealed a Snellen visual acuity of 6/18 in the affected right eye and 6/9 in the left. There was vasculitic inflammation of a single branch retinal artery seen in the inferonasal quadrant of the right eye (figure 1), and a few scattered intraretinal haemorrhages in all four quadrants as well as mild anterior uveitis consisting of flare+ and cells+. The left eye was entirely unaffected.
Figure 1.
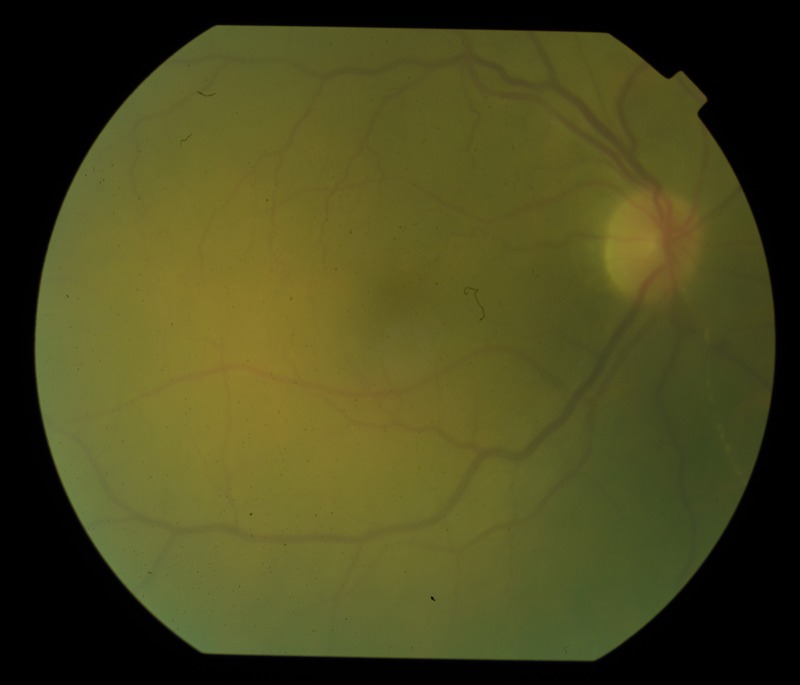
Colour fundus photograph of the right eye demonstrating retinal arterial vasculitis affecting an inferonasal branch retinal artery.
Investigations
Blood tests, specifically looking for inflammatory markers, and a vasculitic screen were performed, all of which returned no abnormality. A chest X-ray did not demonstrate any features of sarcoidosis and was otherwise normal, as were a Mantoux test, ocular coherence tomography of the eye and blood pressure. A fluorescein angiogram of the right eye demonstrated a single affected arterial branch vessel in the inferonasal quadrant and three separate loci of perivascular staining within that vessel (figure 2), indicating a single vessel arterial vasculitis.
Figure 2.
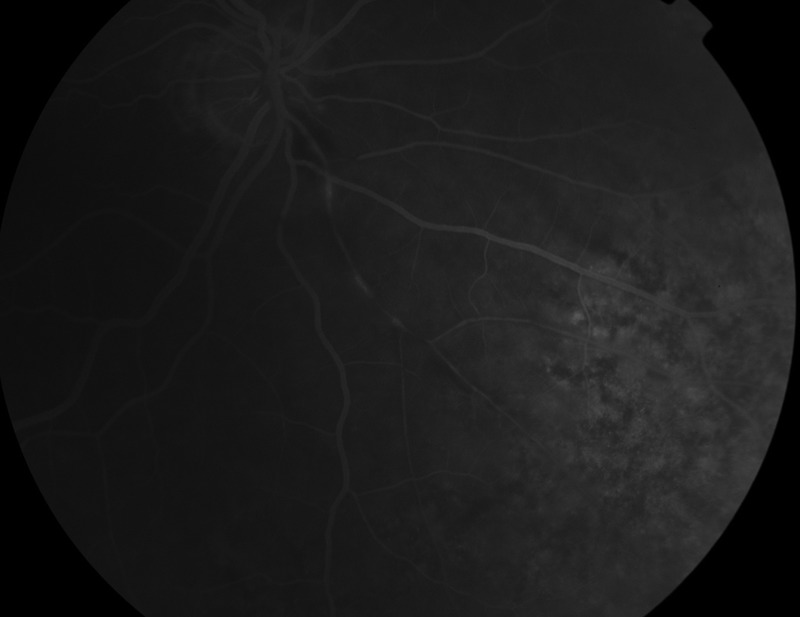
Fundus fluorescein angiogram of the right eye demonstrating three foci of hyperfluorescence in a single branch retinal artery indicative of vasculitis.
Differential diagnosis
Causes of both anterior uveitis and vasculitis include sarcoidosis, tuberculosis, syphilis and Wegener's granulomatosis, although testing was negative for all these diseases. Causes of visual loss associated with headache include giant cell arteritis, although both erythrocyte sedimentation rate and C reactive protein tests were normal. It is possible for a localised ocular form of sarcoidosis to occur in the absence of any normal testing, although this method of presentation is highly atypical of this.
Of note was the recent history of influenza vaccination, as there have been a few rare published cases of vaccination causing retinal vasculitis, though not the influenza vaccination. The negative investigations and the nature of the vasculitis were highly suggestive of a retinal arterial vasculitis secondary to influenza vaccination.
Treatment
As the patient had only one vessel involvement in the retina of one eye as well as entirely negative investigation results returned, it was decided to treat her with a course of topical steroid drops for the anterior uveitis (Predforte six times a day, reducing over 6 weeks). As the vasculitis was secondary to a transient insult to the immune system as opposed to a rheumatic inflammatory disease, no systemic immunosuppression was needed on top of the patient's pre-existing 9 mg of daily prednisolone and no orbital floor, subTenon or intravitreal steroid therapy was required.
Outcome and follow-up
Over the course of 6 weeks, the anterior uveitis cleared up completely so that the topical steroid drops could be discontinued. No further vessels became affected in either eye, and no systemic symptoms or signs became apparent. The intraretinal haemorrhages cleared from the right eye over the course of the 6 weeks, and although the affected vessel still appeared sheathed, there was no further progression over the following 3 months. The patient is followed up at three-month intervals to assess for reactivation of the inflammation and any neovascular sequelae secondary to the patch of ischaemic retina that resulted from reduced flow through the affected retinal artery. None have been found thus far and, 9 months following the event, no further treatment has been needed.
Discussion
There are many commonly documented local and systemic side effects of vaccination for any disease, including influenza vaccination, although the first ever documented ocular vasculitis secondary to influenza vaccination was in 1980.1 Since then, there has been a handful of published cases of systemic vasculitides following influenza vaccination, although these did not involve ocular tissues.2 3 A recently published series of two cases illustrated how ocular vasculitis can present following vaccination, although neither case specifically involved the influenza vaccination.4 In both described cases the ocular vasculitis presented as an arterial vasculitis alone with no systemic involvement, and the importance of a fluorescein angiogram was highlighted. The symptoms started in these cases approximately 4–6 weeks following administration of the vaccine, a slightly shorter time period to that seen in our patient by 2 weeks, which might be accounted for by the milder symptoms, which might have started earlier but had gone unnoticed by the patient.
Interestingly, this patient had received a yearly influenza vaccination in the past, though without ill effect. It is possible that the influenza vaccine, as it is a new product each year, designed to combat a fast-mutating virus, can induce vasculitis when it has not previously done so due to a differing immune reaction.5 For this reason, we will also be recommending that this patient continue to receive yearly influenza vaccinations, though should any other problem occur, this decision will be reassessed.
This case illustrates how important it is to take a history of vaccination in patients presenting with ocular vasculitis only involving retinal arteries. The differential diagnoses include systemic disorders that can potentially require a long course of antibiotic or immunosuppression with all the attendant side effects. The number of published cases similar in nature is very small, and, to date, this is the only case of retinal arterial vasculitis presenting in this manner following influenza vaccination. Owing to the small number of cases, it is not known what the prevalence of anterior or posterior uveitis is, following influenza vaccination, but it is almost certainly being under-reported, as those seeing and treating such patients may not have asked the patient about recent vaccinations. However, due to increasing usage of influenza vaccination and the notoriously low specificity and sensitivity of tests in investigating uveitis, we recommend a high index of suspicion for a vaccine-based aetiology in arteritic ocular vasculitis, with fluorescein angiography being an essential investigation.6
Learning points.
There are several causes for ocular vasculitis, many of which require some form of long-term therapy.
Influenza vaccination is increasingly used to control winter ’flu outbreaks in developed countries.
Influenza vaccination has previously been described as a cause of systemic vasculitis with ocular involvement.
Other vaccinations have been previously described as being a cause of purely ocular vasculitis.
This is the first report to link influenza vaccination to a purely ocular arterial vasculitis and we encourage ophthalmologists to consider this in the list of differential diagnoses.
Footnotes
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Blumberg S, Bienfang D, Kantrowitz FG. A possible association between influenza vaccination and small vessel vasculitis. Arch Intern Med 1980;140:847–8. 10.1001/archinte.1980.00330180121037 [DOI] [PubMed] [Google Scholar]
- 2.Gavaghan T, Webber CK. Severe systemic vasculitic syndrome post influenza vaccination. Aust NZ J Med 1993;23:220 10.1111/j.1445-5994.1993.tb01824.x [DOI] [PubMed] [Google Scholar]
- 3.Mader R, Narendran A, Lewtas J et al. Systemic vasculitis following influenza vaccination—report of three cases and literature review. J Rheumatol 1993;20:1429–31. [PubMed] [Google Scholar]
- 4.Kwok T, Al-Bermani A. Two rare cases of retinal vasculitis following vaccination. SMJ 2013;58:e10–2. [DOI] [PubMed] [Google Scholar]
- 5.Zafrir Y, Afmon-Levin N, Shoenfeld Y. Post influenza vaccination vascultides: a possible new entity. J Clin Rheumatol 2009;15:269–70. 10.1097/RHU.0b013e3181b56177 [DOI] [PubMed] [Google Scholar]
- 6.Dahlberg PJ, Lockhart JM, Overholt EL. Diagnostic studies for systemic necrotizing vasculitis. Sensitivity, specificity and predictive value in patients with multisystem disease. Arch Intern Med 1989;149:161–5. 10.1001/archinte.1989.00390010139019 [DOI] [PubMed] [Google Scholar]


