Abstract
Despite success in expanded program immunization for an increase in vaccination coverage in the children of world, timeliness and schedule of vaccination remains as one of the challenges in public health. This study purposed to demonstrate the related factors of delayed diphtheria-tetanus-pertussis (DTP) vaccination using life table approach. A historical cohort study conducted in the poor areas of five large Iran cities. Totally, 3610 children with 24-47 months old age who had documented vaccination card were enrolled. Time of vaccination for the third dose of DTP vaccine was calculated. Life table survival was used to calculate the proportional probability of vaccination in each time. Wilcoxon test was used for the comparison proportional probability of delayed vaccination based on studies factors. The overall median delayed time for DTP3 was 38.52 days. The Wilcoxon test showed that city, nationality, education level of parents, birth order and being in rural areas are related to the high probability of delay time for DTP3 vaccination (P < 0. 001). Moreover, child gender and parent's job were not significant factors (P > 0.05). Being away from the capital, a high concentration of immigrants in the city borders with a low socioeconomic class leads to prolonged delay in DTP vaccination time. Special attention to these areas is needed to increase the levels of parental knowledge and to facilitate access to the health services care.
Keywords: Children, Immunization, Iran, life table, Survival time, Vaccine
INTRODUCTION
Vaccination is the most effective and economical means of combating the disease.[1] Considerable progress has been made in increasing immunization coverage of children around the world through Expanded Immunization Program (EPI) of World Health Organization (WHO).[2] Before the implantation of universal EPI by WHO in 1974, <5% of children were vaccinated against the vaccine-preventable diseases worldwide.[3] Until 2013, global coverage with the four core vaccines especially diphtheria-tetanus-pertussis (DTP), polio and measles has reached more than 84%.[4] Therefore, a considerable success in eradication or noticeable reduction in the incidence and mortality of childhood diseases occurred.[5,6,7]
Despite good achievement and increasing immunization coverage, timely vaccination has become an important challenge in many countries.[8,9] To achieve the highest level of immunity against the target diseases evermore, children should receive all recommended vaccines on the schedule.[10] The only accomplished studies in Iran showed that 42-67.6% of children received vaccines out of time[11] and this rate in outskirt of Iranian cities is 56.6-93.2% for hepatitis1 and measles, mumps, and rubella vaccines.[12] Delayed administration of vaccination is a powerful risk factor for fatal childhood diseases and can create epidemic and menace international elimination disease programs.[13,14] Therefore, after the high immunization coverage in Iran[9,12] recognizing the predictor of delayed time vaccination is necessary due to little information about timely immunization. Delayed vaccination against the pertussis increases the risk of disease and up to four-fold increased the risk of hospitalization.[15] Moreover, due to the importance of third dose of DTP vaccine (DTP3) as one of the most important indicators of public health,[4] the current study aimed to evaluate the predictors of untimely DTP3 vaccination in children of suburbs of five big Iranian cities.
MATERIALS AND METHODS
A historical cohort study was conducted in suburbs of Iran's cities including Tehran, Isfahan, Mashhad, Zahedan, and Arak in June 2013.The target population was children 24-47 months old that lived in these areas at the time of the survey. The delay time in DTP3 vaccination was calculated according to the time of vaccination and national immunization schedule. Due to the excluding children without the vaccination card, 3610 were analyzed in study finally. Trained interviewers collected data using the WHO standard questionnaire and interviews conducted with the child's mother or nurse. The more details about sampling schedule, study setting, and data collection described in another study.[9]
The data were analyzed by the SPSS software (Chicago Inc.). Since DTP3 vaccine coverage is one of the most important indicators of the public health and for childhood immunization program,[4,10] the delay time of third dose of DTP vaccine was considered as the outcome variable. Independent variables were demographic characteristics including child sex, parent's education and job, living city, prior rural residency, birth order, and nationality. Life table approach used for the survival analysis to estimate the median and proportional probability of vaccination in each month periods intervals of delay in DTP vaccination. Wilcoxon test (Gehan statistics) was used for overall and pairwise comparison. Significance level considered as 0.05.
RESULTS
A total of 3610 children was entered into the analysis, of which 1754 (48.6%) were female, and 1851 (51.3%) were male. The mean ± standard deviation of children age was 36.02 ± 7.11 months. The overall delayed time for DTP3 was 38.52 days. The probability (cumulative incidence) of vaccination at the end of 1st, 2nd, and 3rd months after recommended age for DTP3 vaccination were 0.23, 0.07, and 0.02, respectively. The Wilcoxon test showed a significant difference, as presented in Table 1, in median delay time among under study living cities, nationality, education level of parents, birth order, and prior rural residency (P < 0.001). Nevertheless, there was no significant difference between the delay time of DTP3 vaccination in children based on parents' jobs and child gender. Figures 1 and 2 showed a higher probability of delayed vaccination in non-Iranian children based on life table and Kaplan-Mayer approaches.
Table 1.
Median delay time and proportional probability (SE) of DTP vaccination at 1st, 3rd and 6th months after immunization schedule according to related factors
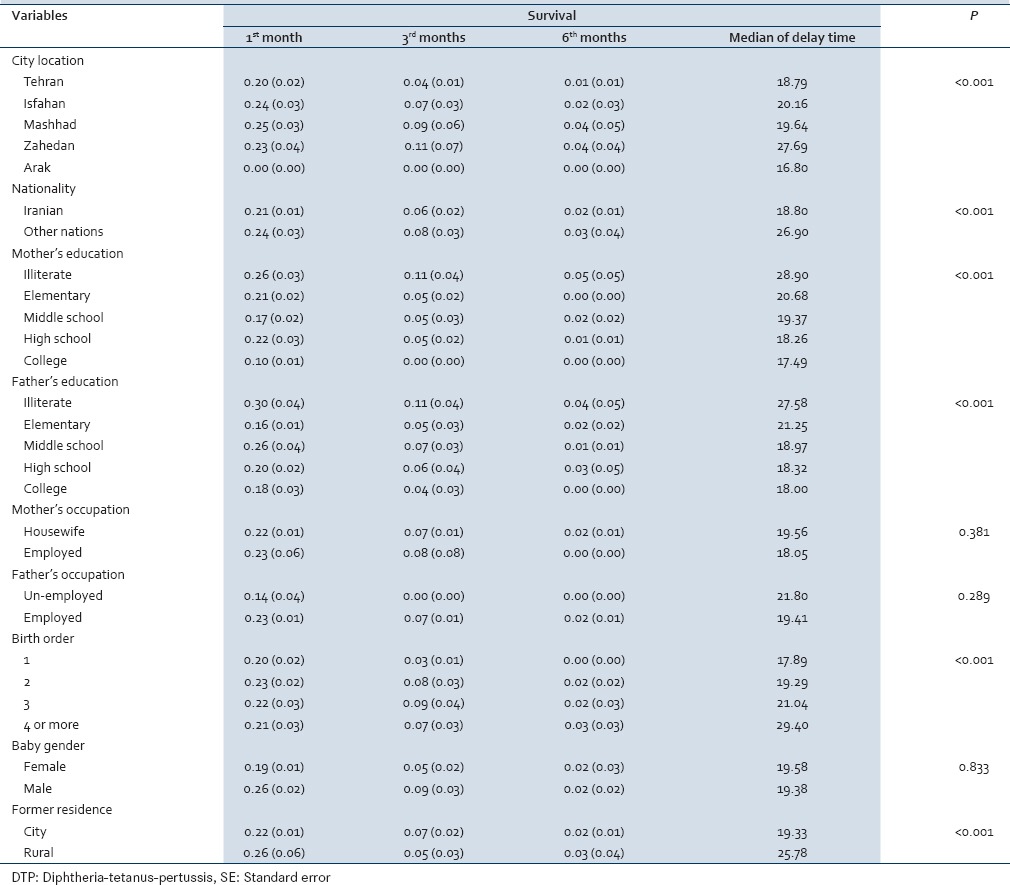
Figure 1.
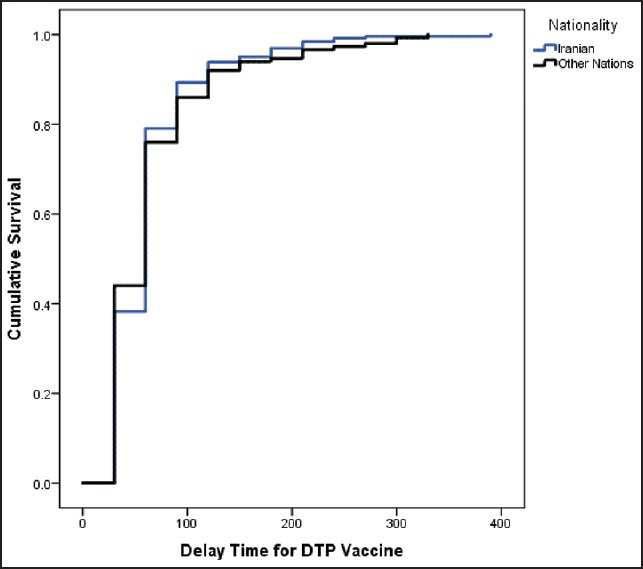
Life table approach of cumulative proportional probability of diphtheria-tetanus-pertussis 3 vaccination for nationality after recommended age of vaccination based on immunization schedule
Figure 2.
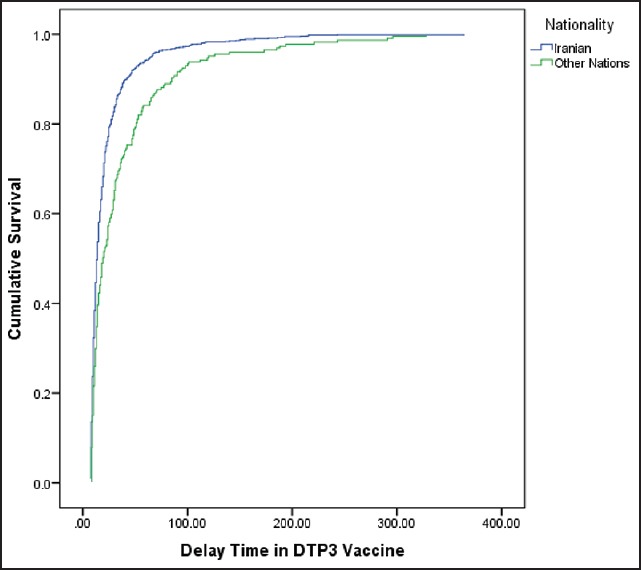
Kaplan-Mayer approach of cumulative proportional probability of diphtheria-tetanus-pertussis 3 vaccination for nationality after the recommended age of vaccination based on immunization schedule
DISCUSSION
According to the results, more than 95% of children are vaccinated 3 months after the recommended age for immunization according to the national schedule program. However, based on some related factors this rate was increased or decreased. Prior residency in the rural area, higher birth order, and more distance from the capital are the risk factors for increasing the delayed vaccination rate. Nevertheless, Iranian nationality and high parent's education are protective factors for delayed vaccination rate that caused earlier vaccination.
The results of our study showed a significant relationship among under study living cities and probability vaccination after recommended schedule time in specified intervals. Several studies have been shown that geographical variation is related factors of vaccination quality.[16,17,18] It is due to the inequity in the distribution of health care facilities, socioeconomic, and cultural differences among different studied cities. So that, the pairwise comparison showed that the probability of delayed vaccination in children living in Zahedan is higher than other cities. Moreover, Arak had the lower probability of delayed vaccination. Zahedan is away from the capital with lower socioeconomic standards and more concentrated illegal immigrant, especially from Afghanistan. On the other hand, children in Arak have the best condition with the lowest median of delayed vaccination time due to the small size of the town and easier access to health centers. In addition, according to the results, the probability of early vaccination in Non-Iranian children is lower than Iranian. Pavlopoulou et al. conducted a study on preschool children in Athens, Greece and showed that incomplete vaccination is more prevalent in immigrants and other minority. This factor leads to lower vaccination worldwide.[19] Therefore, a special intervention on minorities and immigrants seemed to be necessary. Moreover, several studies similar to our study have shown that with increase family size, the timely vaccination decreases.[16,20,21,22,23] Because usually in crowded families, parents' education level and socioeconomic status is low, and the attention of parent for immunization of children decreases. This study showed that the median of delay time for DTP3 vaccine in three intervals (1st month, 2nd to 3rd and 4th to 6th month) is longer in children that lived in the rural area. Similar results presented in another study in India.[22]
It is shown that parent's education have a significant effect on the probability of un-time vaccination and low levels of education inversely related to the increasing probability of delayed vaccination. Pairwise comparison showed that illiterate parent had more delay time for DTP3 vaccination in all intervals. It has been shown in various studies that mother job and education is related to health care utilization and health disparities.[21,24,25,26,27,28,29,30,31] Since, literate mothers have more knowledge about the childhood diseases and are oriented regarding the importance of vaccination at the recommended age. In addition, gender difference did not observe regarding earlier vaccination in boys, unlike some studies.[23,32] Moreover, we did not find a significant association between parent job status and timely vaccination of children. It is similar to the studies conducted in Ethiopia, India, and Brazil.[22,33,34] But the two studies showed that women's occupation related with vaccination status and children whose mothers work out of home were better vaccinated.[18,23] However, in the view point of health policy, the probability of vaccination in each period after recommended age for DTP is calculated. Therefore, more attempts are needed for increasing the timeliness of vaccination as high immunization coverage.
CONCLUSION
The overall median time of children with delayed vaccination was 36.02 days. The delay time in DTP vaccination is increased with distance from the capital, lower levels of parent education, increasing foreign population, and busy families. Therefore, increasing awareness of parents by educational intervention programs should be considered especially for mothers in crowded families. In addition, more attention should be taken for an increase of welfare of families in poor areas.
Financial support and sponsorship
Qom University of Medical Sciences.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors wish to express their gratitude to all health experts who collaborated in data collection in the selected cities, as well as the Qom University of Medical Sciences for the financial support of this study.
REFERENCES
- 1.Koumaré AK, Traore D, Haidara F, Sissoko F, Traoré I, Dramé S, et al. Evaluation of immunization coverage within the expanded program on immunization in kita circle, mali: A cross-sectional survey. BMC Int Health Hum Rights. 2009;9(Suppl 1):S13. doi: 10.1186/1472-698X-9-S1-S13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kruger C, Olsen OE, Mighay E, Ali M. Immunisation coverage and its associations in rural Tanzanian infants. Rural Remote Health. 2013;13:2457. [PubMed] [Google Scholar]
- 3.Hornshøj L, Benn CS, Fernandes M, Rodrigues A, Aaby P, Fisker AB. Vaccination coverage and out-of-sequence vaccinations in rural Guinea-Bissau: An observational cohort study. BMJ Open. 2012;2:pii: e001509. doi: 10.1136/bmjopen-2012-001509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Harris JB, Gacic-Dobo M, Eggers R, Brown DW, Sodha SV. Centers for disease control and prevention (CDC).Global routine vaccination coverage, 2013. MMWR Morb Mortal Wkly Rep. 2014;63:1055–8. [PMC free article] [PubMed] [Google Scholar]
- 5.Sanou A, Simboro S, Kouyaté B, Dugas M, Graham J, Bibeau G. Assessment of factors associated with complete immunization coverage in children aged 12-23 months: A cross-sectional study in Nouna district, Burkina Faso. BMC Int Health Hum Rights. 2009;9(Suppl 1):S10. doi: 10.1186/1472-698X-9-S1-S10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cutts F, Soares A, Jecque AV, Cliff J, Kortbeek S, Colombo S. The use of evaluation to improve the Expanded Programme on Immunization in Mozambique. Bull World Health Organ. 1990;68:199–208. [PMC free article] [PubMed] [Google Scholar]
- 7.Choe YJ, Yang JJ, Park SK, Choi EH, Lee HJ. Comparative estimation of coverage between national immunization program vaccines and non-NIP vaccines in Korea. J Korean Med Sci. 2013;28:1283–8. doi: 10.3346/jkms.2013.28.9.1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hu Y, Li Q, Luo S, Lou L, Qi X, Xie S. Timeliness vaccination of measles containing vaccine and barriers to vaccination among migrant children in East China. PLoS One. 2013;8:e73264. doi: 10.1371/journal.pone.0073264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zahraei SM, Eshrati B, Gouya MM, Mohammadbeigi A, Kamran A. Is there still an immunity gap in high-level national immunization coverage, Iran? Arch Iran Med. 2014;17:698–701. [PubMed] [Google Scholar]
- 10.Sadoh AE, Eregie CO. Timeliness and completion rate of immunization among Nigerian children attending a clinic-based immunization service. J Health Popul Nutr. 2009;27:391–5. doi: 10.3329/jhpn.v27i3.3381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Poorolajal J, Khazaei S, Kousehlou Z, Bathaei S, Zahiri A. Delayed Vaccination and Related Predictors among Infants. Iran J Public Health. 2012;41:65–71. [PMC free article] [PubMed] [Google Scholar]
- 12.Rejali M, Mohammadbeigi A, Mokhtari M, Zahraei SM, Eshrati B. Timing and delay in children vaccination; evaluation of expanded program of immunization in outskirt of Iranian cities. J Res Health Sci. 2015;15:54–8. [PubMed] [Google Scholar]
- 13.Fadnes LT, Nankabirwa V, Sommerfelt H, Tylleskär T, Tumwine JK, Engebretsen IM. PROMISE-EBF Study Group. Is vaccination coverage a good indicator of age-appropriate vaccination. A prospective study from Uganda? Vaccine. 2011;29:3564–70. doi: 10.1016/j.vaccine.2011.02.093. [DOI] [PubMed] [Google Scholar]
- 14.Heininger U, Zuberbühler M. Immunization rates and timely administration in pre-school and school-aged children. Eur J Pediatr. 2006;165:124–9. doi: 10.1007/s00431-005-0014-y. [DOI] [PubMed] [Google Scholar]
- 15.Grant CC, Roberts M, Scragg R, Stewart J, Lennon D, Kivell D, et al. Delayed immunisation and risk of pertussis in infants: Unmatched case-control study. BMJ. 2003;326:852–3. doi: 10.1136/bmj.326.7394.852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fadnes LT, Jackson D, Engebretsen IM, Zembe W, Sanders D, Sommerfelt H, et al. Vaccination coverage and timeliness in three South African areas: A prospective study. BMC Public Health. 2011;11:404. doi: 10.1186/1471-2458-11-404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention (CDC). National, state, and local area vaccination coverage among children aged 19-35 months - United States, 2012. MMWR Morb Mortal Wkly Rep. 2013;62:733–40. [PMC free article] [PubMed] [Google Scholar]
- 18.Wiysonge CS, Uthman OA, Ndumbe PM, Hussey GD. Individual and contextual factors associated with low childhood immunisation coverage in sub-Saharan Africa: A multilevel analysis. PLoS One. 2012;7:e37905. doi: 10.1371/journal.pone.0037905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pavlopoulou ID, Michail KA, Samoli E, Tsiftis G, Tsoumakas K. Immunization coverage and predictive factors for complete and age-appropriate vaccination among preschoolers in Athens, Greece: A cross-sectional study. BMC Public Health. 2013;13:908. doi: 10.1186/1471-2458-13-908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abbott P, Menzies R, Davison J, Moore L, Wang H. Improving immunisation timeliness in Aboriginal children through personalised calendars. BMC Public Health. 2013;13:598. doi: 10.1186/1471-2458-13-598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Babirye JN, Engebretsen IM, Makumbi F, Fadnes LT, Wamani H, Tylleskar T, et al. Timeliness of childhood vaccinations in Kampala Uganda: A community-based cross-sectional study. PLoS One. 2012;7:e35432. doi: 10.1371/journal.pone.0035432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mathew JL. Inequity in childhood immunization in India: A systematic review. Indian Pediatr. 2012;49:203–23. doi: 10.1007/s13312-012-0063-z. [DOI] [PubMed] [Google Scholar]
- 23.Rahman M, Obaida-Nasrin S. Factors affecting acceptance of complete immunization coverage of children under five years in rural Bangladesh. Salud Publica Mex. 2010;52:134–40. doi: 10.1590/s0036-36342010000200005. [DOI] [PubMed] [Google Scholar]
- 24.Fernandez RC, Awofeso N, Rammohan A. Determinants of apparent rural-urban differentials in measles vaccination uptake in Indonesia. Rural Remote Health. 2011;11:1702. [PubMed] [Google Scholar]
- 25.Dombkowski KJ, Lantz PM, Freed GL. Risk factors for delay in age-appropriate vaccination. Public Health Rep. 2004;119:144–55. doi: 10.1177/003335490411900207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dayan GH, Shaw KM, Baughman AL, Orellana LC, Forlenza R, Ellis A, et al. Assessment of delay in age-appropriate vaccination using survival analysis. Am J Epidemiol. 2006;163:561–70. doi: 10.1093/aje/kwj074. [DOI] [PubMed] [Google Scholar]
- 27.Mbabazi W, Lako AK, Ngemera D, Laku R, Yehia M, Nshakira N. Maiden immunization coverage survey in the republic of South Sudan: A cross-sectional study providing baselines for future performance measurement. Pan Afr Med J. 2013;23(16):110. doi: 10.11604/pamj.2013.16.110.3164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hassanzadeh J, Mohammadbeigi A, Eshrati B, Rezaianzadeh A, Rajaeefard A. Determinants of inequity in health care services utilization in markazi province of iran. Iran Red Crescent Med J. 2013;15:363–70. doi: 10.5812/ircmj.3525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mohammadbeigi A, Hassanzadeh J, Eshrati B, Rezaianzadeh A. Socioeconomic inequity in health care utilization, Iran. J Epidemiol Glob Health. 2013;3:139–46. doi: 10.1016/j.jegh.2013.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mohammadbeigi A, Hassanzadeh J, Eshrati B, Rezaianzadeh A. Decomposition of inequity determinants of healthcare utilization, Iran. Public Health. 2013;127:661–7. doi: 10.1016/j.puhe.2013.01.001. [DOI] [PubMed] [Google Scholar]
- 31.Mohammadbeigi A, Arsangjang S, Mohammadsalehi N, Anbari Z, Ghaderi E. Education-related Inequity in Access and Utilization of Oral Health Care in Iran. J Family Med Prim Care. 2015;4:35–8. doi: 10.4103/2249-4863.152248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ettarh RR, Mutua MK, Kyobutungi C. Ethnicity and delay in measles vaccination in a nairobi slum. Trop Med Health. 2012;40:59–62. doi: 10.2149/tmh.2012-09s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Etana B, Deressa W. Factors associated with complete immunization coverage in children aged 12-23 months in Ambo Woreda, Central Ethiopia. BMC Public Health. 2012;12:566. doi: 10.1186/1471-2458-12-566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Barata RB, Ribeiro MC, de Moraes JC, Flannery B. Vaccine Coverage Survey Group. Socioeconomic inequalities and vaccination coverage: Results of an immunisation coverage survey in 27 Brazilian capitals, 2007-2008. J Epidemiol Community Health. 2012;66:934–41. doi: 10.1136/jech-2011-200341. [DOI] [PMC free article] [PubMed] [Google Scholar]


