Abstract
The presence of an aortoenteric fistula following aortobifemoral graft repair of an abdominal aortic aneurysm is associated with a high probability of infection leading to clinically significant bacteremia. We report a case of an aortoenteric fistula that developed two years after initial aortic grafting resulting in colonization with the anaerobe, Eggerthella lenta. This dangerous bacterium is difficult to culture, associated with high mortality and the patient may have mild symptoms on presentation.
Keywords: Aortic graft infection, Aortobifemoral graft, Aortoenteric fistula, Eggerthella lenta
INTRODUCTION
Abdominal aortic aneurysms (AAA) can be repaired with an aortic bifemoral bypass graft, which is considered an ideal procedure for aortic aneurysms, aorto-iliac disease or aortic atherosclerosis.[1] Though rare, infections involving the graft can happen, typically,two to five years following implantation.[2] Anaerobic, non-sporulating, Gram-positive bacilli from the normal human gut flora can occasionally be implicated in invasive diseases. Notably, Eggerthella lenta, formerly known as Eubacterium lentum, often causes clinically significant bacteremia with a significant mortality rate.[3,4] Herein we report a case of an aortobifemoral bypass graft with an aortoenteric fistula, giving rise to a very rare bacteremia caused by the species Eggerthella lenta.
CASE REPORT
A 75-year-old male with a past medical history significant for Type 2diabetes mellitus, hypertension, chronic thrombocytopenia and chronic kidney injury underwent resection of a ruptured AAA and placement of an aortobifemoral bypass graft. His postoperative course was eventful for renal failure, which required four cycles of dialysis with improvement.
Twenty-nine months later, the patient was seen in the emergency department with a two-day history of rigors, dysuria, polyuria and burning micturition complicated by fever, weakness and lethargy observed by his family on the day of admission. He denied cough, chest pain, palpitations, nausea, vomiting or constipation. Blood pressure upon examination was 70/35 mmHg, rising to 90/48 mmHg after a fluid bolus; temperature was 101 degrees Fahrenheit; heart rate 90/min; and respiratory rate was 20/min. Blood work was significant for a white blood cell count of 18,000; lactic acid of 4.1, 20 percent bands and platelet count of 20,000.Urinalysis was remarkable for white blood cells, red blood cells and moderate leukocyte esterase. Physical examination revealed diffuse abdominal tenderness, and peri-umbilical tenderness with deep palpation without peritoneal signs.The patient was admitted to the intensive care unit with a diagnosis of severe sepsis secondary to urinary tract infection with high anion gap metabolic acidosis secondary to lactic acidosis. Blood cultures and urine cultures were drawn, which demonstrated Eggerthella lenta septicemia and Escherichia coli Extended spectrum beta-lactamase (ESBL)-positive urinary tract infection. The patient was started on IV antibiotics with etrapenem after infectious diseases consult. A subsequent abdominal computed tomography (CT) with contrast demonstrated induration with inflammatory changes around the aortobifemoral bypass graft. Furthermore, the graft showed stranding around the aorta near the iliac components with presence of an air bubble between these components [Figure 1]. This finding raised the possibility of gas producing infection or an aortoenteric fistula communicating with an adjacent loop of bowel, either of which could have feasibly contributed to the aortic graft harboring Eggerthella lenta. The patient was recommended to have graft replacement surgery with repair of the fistula in order to remove the source of infection; however, he refused, preferring to be treated with IV antibiotics instead, despite the considerable risk. Repeated blood cultures after treatment with antibiotics were negative and the patient was discharged home on antibiotics as an outpatient with the possibility of requiring chronic suppression with antibiotics.
Figure 1.
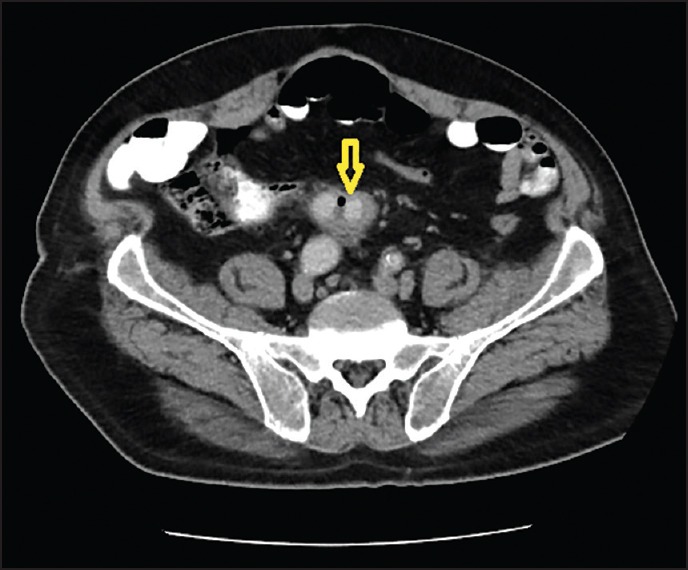
CT scan of the abdomen and pelvis showing an induration with inflammatory changes around the aorto-iliac graft and an small air bubble (yellow arrow) between the two legs of the graft, possibly caused by a fistulous communication with the bowel
DISCUSSION
Aortoenteric fistulas can involve any part of the small or large bowel, but it is more common to find them in the third and fourth portions of the duodenum. Mucosal bleeding can be one of the signs as erosions of the graft into the intestines can precede massive gastrointestinal bleeding from an established aortoenteric fistula. Staphylococcus aureus and Gram-negative bacilli, accompanied by fever, signs of infection and leukocytosis, typically cause early infections (less than four months after repair). The presentation of late-onset infections can be subtle without any specific signs or symptoms with an absence of fever being common. In fact, in few studies, the absence of fever and stay in the intensive care unit (ICU), was associated with an increased risk of mortality.[5,6] They can also present with complications of the graft infection, such as a pseudoaneursym, sepsis or bleeding.[7] Our patient did have fever, leukocytosis and hypotension, but thiscould have been caused by his concurrent urinary tract infection with E. coli. It is possible that had this patient not had symptoms from his urinary tract infection, his bacteremia may have been missed.
The use of graft devices for repair of an AAAmay require a complex, open-air procedure with exposure of the compromised vessel. This, of course, increases the risk of an infectionfrom the device as well as the wound. The incidence of AAA graft infection is low (0.4% to 3%),[8] with one-third of those infections manifesting as aortoenteric erosions/fistula.[9] The management of an aortoenteric fistula has typically required replacement of the affected graft and repair of the fistulae, a surgery with a mortality risk of 20 to 30 percent.[5] Bacteremia associated with the aortoenteric fistula has also been reported to have a high mortality risk.[3,10] In our case, the CT scan of the patient raised the possibility of an aortoenteric fistula that was likely to be the source of the patient's infection with Eggerthella lenta. After being explained the risk of the surgery, as well as the possibility of not being able to resolve the infection without surgery, the patient declined to move forward with the procedure.
Anaerobic bacteria are the predominant normal flora of the mucous membranes.[11,12,13] Although Lactobacillus, Clostridium and Propionibacterium species are more commonly encountered, many other lesser known anaerobic Gram-positive bacilli can be involved in clinical infections as well. Eggerthella is a bacterial genus of Actinobacteria, in the family Coriobacteriaceae. Members of this genus are anaerobic, non-sporulating, non-motile, Gram-positive bacilli that grow singly, as pairs or in short chains.[10] Classification and identification of this bacterium is reliably achieved through specialized cultured blood samples identifying the Gram-positive bacilli as Eggerthella lenta with 94% and 99% probability and confirmed by 16sRNA PCR gene sequencing. Eggerthella lenta can be found in many different parts of the body, most commonly in the colon and feces. Bacteremia associated with this bacterium carries a high mortality rate (20-40%) especially if it is found to be the only pathogen in the blood. It is thereforecritical to locate the source of the bacteremia and initiate antibiotic treatment.[3,4,14] Eggerthella lenta has been linked with many conditions such as ulcerative colitis, Crohn's disease, sinusitis, abscesses, pelvic inflammatory disease, malignancy and pancreatic abscesses among others.[14,15] Nearly all infections with anaerobic bacteria originate from the patient's own microflora; therefore, we can conclude that this patient's bacteremia was from his own flora, with the likely source to be the aortoenteric fistula.[11] Due to the fastidious nature of these organisms, it can be exceedingly difficult to isolate these anaerobes from the site of an infection and easy to miss. Isolating them requires the appropriate method of collection, transportation and cultivation of specimens, which requires a laboratory capable of performing 16S rRNA gene analysis. At times it can take two to six weeks for identification.[9,16] For our patient, it took three days in order to get a positive blood culture and another three days to identify the organism and get antibiotic susceptibility. Treatment with etrapenem proved to be successful as repeat cultures were negative.
Though bacteremia caused by Eggerthella lenta is rare, if it is present, it is almost always clinically significant and requires prompt diagnosis and treatment. We believe that patients, who have had repair of an AAA and present with abdominal pain with or without fever, should have their blood appropriately cultured for anaerobic bacteria. It should be noted that patients who undergo this procedure are recommended to have yearly CT scans performedto rule out infections or fistulas that can lead to dangerous bacteremia.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.West CA, Jr, Johnson LW, Doucet L, Caldito G, Heldman M, Szarvas T, et al. A contemporary experience of open aortic reconstruction in patients with chronic atherosclerotic occlusion of the abdominal aorta. J Vasc Surg. 2010;52:1164–72. doi: 10.1016/j.jvs.2010.05.112. [DOI] [PubMed] [Google Scholar]
- 2.Farkas JC, Fichelle JM, Laurian C, Jean-Baptiste A, Gigou F, Marzelle J, et al. Long-term follow-up of positive cultures in 500 abdominal aortic aneurysms. Arch Surg. 1993;128:284–8. doi: 10.1001/archsurg.1993.01420150038007. [DOI] [PubMed] [Google Scholar]
- 3.Lau SK, Woo PC, Fung AM, Chan KM, Woo GK, Yuen KY. Anaerobic, non-sporulating, Gram-positive bacilli bacteraemia characterized by 16S rRna gene sequencing. J Med Microbiol. 2004;53:1247–53. doi: 10.1099/jmm.0.45803-0. [DOI] [PubMed] [Google Scholar]
- 4.Venugopal AA, Szpunar S, Johnson LB. Risk and prognostic factors among patients with bacteremia due to Eggerthella lenta. Anaerobe. 2012;18:475–8. doi: 10.1016/j.anaerobe.2012.05.005. [DOI] [PubMed] [Google Scholar]
- 5.Kan CD, Lee HL, Yang YJ. Outcome after endovascular stent graft treatment for mycotic aortic aneurysm: Asystematic review. J Vasc Surg. 2007;46:906–12. doi: 10.1016/j.jvs.2007.07.025. [DOI] [PubMed] [Google Scholar]
- 6.Laupland KB, Zahar JR, Adrie C, Schwebel C, Goldgran-Toledano D, Azoulay E, et al. Determinants of temperature abnormalities and influence on outcome of critical illness. Crit Care Med. 2012;40:145–51. doi: 10.1097/CCM.0b013e31822f061d. [DOI] [PubMed] [Google Scholar]
- 7.Valentine RJ. Diagnosis and management of aortic graft infection. Semin Vasc Surg. 2001;14:292–301. doi: 10.1053/svas.2001.27874. [DOI] [PubMed] [Google Scholar]
- 8.Sharif MA, Lee B, Lau LL, Ellis PK, Collins AJ, Blair PH, et al. Prosthetic stent graft infection after endovascular abdominal aortic aneurysm repair. J Vasc Surg. 2007;46:442–8. doi: 10.1016/j.jvs.2007.05.027. [DOI] [PubMed] [Google Scholar]
- 9.Riesenman PJ, Farber MA, Mauro MA, Selzman CH, Feins RH. Aortoesophageal fistula after thoracic endovascular aortic repair and transthoracic embolization. J Vasc Surg. 2007;46:789–91. doi: 10.1016/j.jvs.2007.05.036. [DOI] [PubMed] [Google Scholar]
- 10.Lau SK, Woo PC, Woo GK, Fung AM, Wong MK, Chan KM, et al. Eggerthella hongkongensis sp. nov. and eggerthella sinensis sp. nov., two novel Eggerthella species, account for half of the cases of Eggerthella bacteremia. Diagn Microbiol Infect Dis. 2004;49:255–63. doi: 10.1016/j.diagmicrobio.2004.04.012. [DOI] [PubMed] [Google Scholar]
- 11.Hentges DJ. The anaerobic microflora of the human body. Clin Infect Dis. 1993;16:S175–80. doi: 10.1093/clinids/16.supplement_4.s175. [DOI] [PubMed] [Google Scholar]
- 12.Liderot K, Larsson M, Boräng S, Özenci V. Polymicrobial bloodstream infection with Eggerthella lenta and Desulfovibrio desulfuricans. J Clin Microbiol. 2010;48:3810–2. doi: 10.1128/JCM.02481-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brook, Frazier EH. Significant recovery of nonsporulating anaerobic rods from clinical specimens. Clin Infect Dis. 1993;16:476–80. doi: 10.1093/clind/16.4.476. [DOI] [PubMed] [Google Scholar]
- 14.Thota VR, Dacha S, Natarajan A, Nerad J. Eggerthella lenta bacteremia in a Crohns disease patient after ileocecal resection. Future Microbiol. 2011;6:595–7. doi: 10.2217/fmb.11.31. [DOI] [PubMed] [Google Scholar]
- 15.Lattuada E, Zorzi A, Lanzafame M, Antolini D, Fontana R, Vento S, et al. Cutaneous abscess due to Eubacterium lentum in injection drug user: A case report and review of the literature. J Infect. 2005;51:E71–2. doi: 10.1016/j.jinf.2004.08.026. [DOI] [PubMed] [Google Scholar]
- 16.Woo PC, Lau SK, Teng JL, Tse H, Yuen KY. Then and now: Use of 16S rDNA gene sequencing for bacterial identification and discovery of novel bacteria in clinical microbiology laboratories. Clin Microbiol Infect. 2008;14:908–34. doi: 10.1111/j.1469-0691.2008.02070.x. [DOI] [PubMed] [Google Scholar]


