Abstract
Aim:
To evaluate the sealing ability of ProRooT MTA, RetroMTA, and Biodentine as furcation repair materials using dye extraction leakage method.
Materials and Methods:
Thirty-five mandibular molars were randomly divided into four groups according to the material used for perforation repair. Group I — ProRoot MTA (10 samples), Group II — RetroMTA (10 samples), Group III — Biodentine (10 samples), and Group IV (Control) — left unrepaired (5 samples). All samples were subjected to orthograde and retrograde Methylene blue dye challenge followed by dye extraction with concentration 65% nitric acid. Samples were then analyzed using ultraviolet-visible spectrophotometer using 550 nm wave lengths.
Statistical Analysis:
One-way analysis of variance, Tukey-Kramer multiple comparisons test.
Results:
Biodentine showed least dye absorbance while RetroMTA showed highest dye absorbance values when compared with other repair materials.
Conclusion:
Within the limitations of this study, it was observed that Biodentine showed better sealing ability when compared with other root repair materials.
Keywords: Dye-extraction, furcation repair, perforation, ultraviolet spectrophotometer
INTRODUCTION
The goal of endodontic therapy is to maintain the integrity of the natural dentition to proper form, function, and esthetics. In endodontic practice, procedural accidents are commonly encountered, which affect the prognosis of the root canal treatment. A furcation perforation is one such complication that refers to mid-curvature opening into the periodontal ligament (PDL) space and leads to worst possible treatment outcome.[1] According to Seltzer, perforations were the second greatest cause of failure in endodontic therapy.[2] For long-term success, perforations should be repaired as quickly as possible with a biocompatible material to prevent bacterial contamination. An ideal perforation repair material should provide an adequate seal, be biocompatible, not affected by blood contamination, bactericidal, should induce bone formation and healing, radiopaque, induce mineralization, cementogenesis, and easy in manipulation and placement.[3] Several materials such as intermediate restorative material, composite resin, super ethoxy benzoic acid, resin-modified glass ionomer cement, calcium hydroxide, Gutta-percha, and mineral trioxide aggregate (MTA) were the most commonly used repair materials. However, the divergent outcomes suggest that so far no material has satisfied all the ideal requirements.[4]
The most preferred furcation repair material used is MTA. Despite the favorable properties of MTA that supports its clinical use, it has several clinical drawbacks such as prolonged setting time, difficult handling characteristics, and potential discoloration.[5] Hence, in an attempt to modify the properties of MTA and to overcome the shortcomings, a variety of new Calcium-silicate based materials have been formulated which includes Biodentine, BioAggregate, RetroMTA, and EndoSequence root repair material.
Biodentine (Septodont, France) is a high purity calcium-silicate based dental material composed of tricalcium silicate; calcium carbonate, zirconium oxide, and water-based liquid containing calcium chloride (CaCl2) as the setting accelerator and water-reducing agent. Biodentine is recommended for use as a dentin substitute and an endodontic repair material because of its good sealing ability, high compressive strengths, short setting time[6,7] biocompatibility, bioactivity and biomineralization properties.[8]
A novel RetroMTA® (BioMTA, Seoul, Korea) material was recently introduced, which is a mixture of hydrophilic powders that are not derived from Portland cement. It consists of calcium carbonate, silicon dioxide, aluminum oxide, hydraulic calcium zirconia, and it has an initial setting time of only 150 s.[9] Hence, it is recommended as a furcation repair material.
Thus, the present study was designed to evaluate the sealing ability of ProRoot MTA, RetroMTA, and Biodentine in the repair of furcation perforations.
MATERIALS AND METHODS
Thirty-five extracted, intact human mandibular molars with non-fused and well-developed roots were used in this study. The teeth were stored in 3% sodium hypochlorite until further use. Molars were decoronated 3 mm above the cemento-enamel junction and roots were amputated 3 mm below the furcation. A standardized endodontic access opening was prepared in all 35 samples. Sticky wax was placed over the orifice of each canal. It was then coated with two layers of nail varnish.
To ensure each perforation was centered between the roots, a black marker pen was used to mark the location of the defect. A defect 1 mm in diameter was made from the external surface of the tooth with a number 2 round carbide bur mounted on a high-speed handpiece with air water coolant. The chamber and perforation were flushed with water and dried. The teeth were kept in an incubator at 37°C for 24 h for simulating clinical conditions.
Perforation repair
Teeth were randomly divided into four groups with 10 samples each for the experimental group and 5 samples in the control group. Group I was repaired with ProRoot MTA (Dentsply Tulsa, Tulsa, OK, USA), Group II with RetroMTA (BioMTA, Daejeon, Korea), Group III with Biodentine (Septodont, France) and Group IV, that is, control group was left unrepaired (positive control). All the teeth in each group were allowed to set for 24 h.
Dye extraction microleakage evaluation
Each group was placed in separate Petri dishes containing 2% methylene blue such that all teeth were immersed in dye up to the cemento-enamel junction for retrograde dye challenge and dye was added to access chamber of each teeth so that it was filled for orthograde dye challenge. All samples were stored similarly for 48 h.
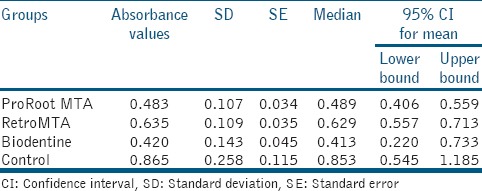
After removal of the dye, teeth were rinsed under tap water for 30 min and varnish removed with a polishing disc. Each tooth was stored in a vial containing 5 ml of concentration nitric acid (65 weight %) for 3 days. The solutions thus obtained were centrifuged at 3500 rpm for 5 min. Four milliliters of the supernatant liquid was then analyzed in an ultraviolet (UV) visible spectrophotometer at 550 nm wavelength with concentrated nitric acid as the blank and readings were recorded as absorbance units [Table 1]. The obtained readings were statistically analyzed using one-way analysis of variance and Tukey multiple comparisons tests.
Table 1.
Mean values for four different experimental groups
RESULTS
The mean absorbance values [Figure 1] of experimental groups and control group in the current study showed that the positive control samples (Group IV) in which perforations were left unrepaired had the highest dye absorbance (0.86 ± 0.258) of all groups denoting the accuracy of the technique. This was followed by RetroMTA (Group II) which had dye absorbance values (0.63 ± 0.109) significantly higher than ProRoot MTA (Group I) and Biodentine (Group III) showed least dye absorbance than remaining groups.
Figure 1.
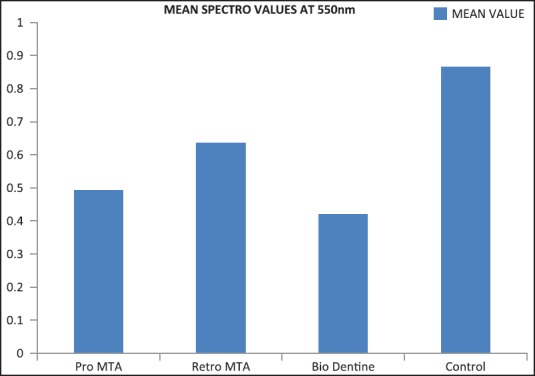
Mean spectrophotometric dye absorbance values of the groups
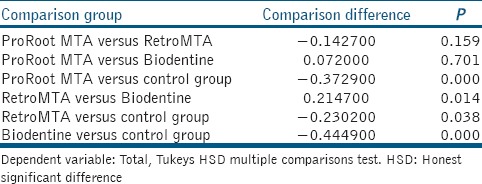
There was a significant difference in the mean dye leakage among four groups (P < 0.005). Hence, Tukey's HSD Multiple comparison test was done. It was seen that there was no statistically significant difference between ProRoot MTA and Biodentine groups. Similarly, there was no significant difference between ProRoot MTA and RetroMTA groups either. However, there was a statistically significant difference seen between the RetroMTA and Biodentine groups [Table 2].
Table 2.
Comparison between individual groups
DISCUSSION
The perforations irrespective of location or etiology may interfere with the prognosis of endodontic treatment. This iatrogenic, mechanical, or pathologic communication between root canal system and external root surface should be sealed immediately with a biocompatible material. The present study evaluated the sealing ability of MTA, RetroMTA, and Biodentine as furcation repair materials in mandibular molars using a dye extraction leakage method.
Several methods have been used to assess microleakage. These include methods such as fluid filtration, dye penetration, dye extraction, bacterial, and protein leakage models. Recent methods include by using radioactive isotopes, artificial caries, scanning electron microscopy, neutron activation analysis, and electrical conductivity.[10] In this study, dye extraction methodology was employed which according to Camps and Pashley[11] gave similar results to the fluid filtration technique as both are based on quantitative measurements of liquid passage within interfaces. Dye penetration techniques are also one of the commonly used techniques for evaluation of the sealing ability of dental materials. Despite its popularity, dye penetration relies on randomly cutting the root into two pieces, without knowing if the section goes through the deepest dye penetration. This drawback is avoided by dye extraction method, which involves recovering all of the dye that penetrated the apex, thereby avoiding limitations of sectioning the root. Moreover, it is easy to perform and does not require an elaborate equipment set up.[12] Spectrophotometers are instruments designed to produce the most accurate color measurements.[13] UV-visible spectrophotometry refers to absorption spectroscopy or reflectance spectroscopy in the UV-visible spectral region. This means it uses light in the adjacent (near-UV and near-infrared) ranges. The absorbance or reflectance in the visible range directly affects the perceived color of the chemicals involved.
MTA was actually introduced as a root-end filling material; however because of its biocompatibility, it is now also considered as a material of choice to seal perforations.[14] However, MTA shows certain drawbacks such as difficulty in handling and very slow setting reaction. In order to overcome these difficulties, new materials have been formulated.
RetroMTA is a hydraulic bioceramic material newly formulated for application in perforation repair and vital pulp therapy. It is a powder consisting of fine, hydrophilic particles that set in the presence of water. It is claimed to have comparatively shorter setting time than ProRoot MTA, good handling properties, no cell toxicity, setting reaction initiated by moisture, no heavy metals, and greater washout resistance than ProRoot MTA.[9]
Hence, this new bioactive material RetroMTA was taken as one of the furcation perforation sealer in comparison with MTA. However, such RetroMTA showed high dye absorbance values than MTA.
The current study is perhaps the first attempt to adapt the use of RetroMTA into the field of endodontics where the search for the ideal repair material is a continuous process. However, further studies involving RetroMTA will be necessary to examine its clinical applications.
ProRoot MTA showed dye absorbance values comparable to the remaining materials. The excellent and unique property of MTA is its ability to promote regeneration of cementum, thus facilitating the regeneration of the periodontal apparatus. The enhanced proliferation of PDL fibroblasts on MTA compared with other root end filling materials has been reported. It was found that the presence of moisture in perforations during the placement of MTA increases its adaptation to perforation walls.[15]
Biodentine is a calcium silicate-based material that has polycarboxylate based hydro-soluble polymer system described as water-reducing agent to reduce the overall water content of the mix, along with CaCl2 as setting accelerator.[12] Biodentine bonds chemomechanically with the tooth and composite. This has high compressive and flexural strength.[3]
In addition, biodentine can induce the synthesis of a dentin-like matrix by human odontoblast-like cells in the form of mineralization nodules that have the molecular characteristics of dentine.[16] This material can also stimulate cell growth and induces Hydroxyapatites (HA) formation on the surface of the material when exposed to simulated body fluid.[17,18] HA have been shown to induce bone formation, growth, and maintenance at the bone material interface.
Han and Okiji compared calcium and silicon uptake by adjacent root canal dentine in the presence of phosphate buffered saline using Biodentine and ProRoot MTA.[6] The results showed that both materials formed a tag-like structure composed of the material itself or calcium or phosphate rich crystalline deposits. The thickness of the calcium and silicon-rich layers increased over time, and the thickness of the calcium and silicon-rich layer was significantly larger in biodentine compared to MTA after 30 and 90 days, concluding that the dentine element uptake was greater for Biodentine than for MTA.
Kokate and Pawar conducted a study that compared the microleakage of glass ionomer cement, MTA and Biodentine when used as a retrograde filling material and concluded that Biodentine exhibited the least microleakage when compared to other materials used.[19]
Based on the results of this study, RetroMTA showed highest dye absorbance, followed by ProRoot MTA and Biodentine, which showed the least dye absorbance.
The biomineralization ability of Biodentine, most likely through the formation of tags, greater calcium and silicon uptake from adjacent root canal dentine and least microleakage when compared with other retrograde filling materials are the probable reasons for its least dye absorbance.
CONCLUSION
Within the limitations of this study, it can be concluded that ProRoot MTA, RetroMTA, and Biodentine showed sealing ability comparable to each other. However, the best seal was provided by Biodentine. Still further research with more number of samples along with the application of different techniques would be helpful.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
Contributors of this study sincerely acknowledge the efforts taken by Dr. Gavhale, (HOD, Biochemistry Department) and Mr. Swapnil Sinkar for the statistical analysis.
REFERENCES
- 1.Balachandran J, Gurucharan Comparison of sealing ability of bioactive bone cement, mineral trioxide aggregate and Super EBA as furcation repair materials: A dye extraction study. J Conserv Dent. 2013;16:247–51. doi: 10.4103/0972-0707.111326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Seltzer S, Bender IB, Smith J, Freedman I, Nazimov H. Endodontic failures - An analysis based on clinical, roentgenographic, and histologic findings. II. Oral Surg Oral Med Oral Pathol. 1967;23:517–30. doi: 10.1016/0030-4220(67)90547-6. [DOI] [PubMed] [Google Scholar]
- 3.Aggarwal V, Singla M, Miglani S, Kohli S. Comparative evaluation of push-out bond strength of ProRoot MTA, Biodentine, and MTA Plus in furcation perforation repair. J Conserv Dent. 2013;16:462–5. doi: 10.4103/0972-0707.117504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.EI-Tawil SB, EI-Dokkyl NA, EI-Hamid DA. Sealing ability of MTA versus Portland cement in the repair of furcal perforations of primary molars: A dye extraction leakage model. J Am Sci. 2011;7:1037–43. [Google Scholar]
- 5.Unal GC, Maden M, Isidan T. Repair of Furcal Iatrogenic Perforation with Mineral Trioxide Aggregate: Two Years Follow-up of Two Cases. Eur J Dent. 2010;4:475–81. [PMC free article] [PubMed] [Google Scholar]
- 6.Han L, Okiji T. Uptake of calcium and silicon released from calcium silicate-based endodontic materials into root canal dentine. Int Endod J. 2011;44:1081–7. doi: 10.1111/j.1365-2591.2011.01924.x. [DOI] [PubMed] [Google Scholar]
- 7.Koubi G, Colon P, Franquin JC, Hartmann A, Richard G, Faure MO, et al. Clinical evaluation of the performance and safety of a new dentine substitute, biodentine, in the restoration of posterior teeth — A prospective study. Clin Oral Investig. 2013;17:243–9. doi: 10.1007/s00784-012-0701-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Laurent P, Camps J, About I. Biodentine(TM) induces TGF-ß1 release from human pulp cells and early dental pulp mineralization. Int Endod J. 2012;45:439–48. doi: 10.1111/j.1365-2591.2011.01995.x. [DOI] [PubMed] [Google Scholar]
- 9.RetroMTA Catalogue. [Last accessed on 2014 Dec 29]. Available from: http://www.bioMTA.com .
- 10.Gogna R, Jagadis S, Shashikal K. A comparative in vitro study of microleakage by a radioactive isotope and compressive strength of three nanofilled composite resin restorations. J Conserv Dent. 2011;14:128–31. doi: 10.4103/0972-0707.82609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Camps J, Pashley D. Reliability of the dye penetration studies. J Endod. 2003;29:592–4. doi: 10.1097/00004770-200309000-00012. [DOI] [PubMed] [Google Scholar]
- 12.Reyes-Carmona JF, Felippe MS, Felippe WT. Biomineralization ability and interaction of mineral trioxide aggregate and white portland cement with dentin in a phosphate-containing fluid. J Endod. 2009;35:731–6. doi: 10.1016/j.joen.2009.02.011. [DOI] [PubMed] [Google Scholar]
- 13.Sikri VK. Color: Implications in dentistry. J Conserv Dent. 2010;13:249–55. doi: 10.4103/0972-0707.73381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Biswas M, Mazumdar D, Neyogi A. Non surgical perforation repair by mineral trioxide aggregate under dental operating microscope. J Conserv Dent. 2011;14:83–5. doi: 10.4103/0972-0707.80729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jeevani E, Jayaprakash T, Bolla N, Vemuri S, Sunil CR, Kalluru RS. Evaluation of sealing ability of MM-MTA, Endosequence, and biodentine as furcation repair materials: UV spectrophotometric analysis. J Conserv Dent. 2014;17:340–3. doi: 10.4103/0972-0707.136449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sanghavi T, Shah N, Shah RR. Comparative analysis of sealing ability of biodentine and calcium phosphate cement against mineral trioxide aggregate as a furcal perforation repair material: An in vitro study. Natl J Integr Res Med. 2013;4:56–60. [Google Scholar]
- 17.Malkondu Ö, Karapinar Kazandag M, Kazazoglu E. A review on biodentine, a contemporary dentine replacement and repair material. Biomed Res Int 2014. 2014 doi: 10.1155/2014/160951. 160951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rajasekharan S, Martens LC, Cauwels RG, Verbeeck RM. Biodentine™ material characteristics and clinical applications: A review of the literature. Eur Arch Paediatr Dent. 2014;15:147–58. doi: 10.1007/s40368-014-0114-3. [DOI] [PubMed] [Google Scholar]
- 19.Kokate SR, Pawar AM. An in vitro comparative stereomicroscopic evaluation of marginal seal between MTA, glass ionomer cement and biodentine as root end filling materials using 1% methylene blue as tracer. Endodontics. 2012;2:36–42. [Google Scholar]


