Abstract
Ledderhose disease, or plantar fibromatosis, is a benign hyperproliferative disorder of the plantar aponeurosis. It presents as one or more round, firm slow-growing plaques or nodules on the plantar surface of the foot, typically on the medial side. The etiology is unknown, though it has been associated with trauma, liver disease, diabetes mellitus, epilepsy and alcoholism. Histopathological examination of plantar fibromatosis reveals dense fibrocellular tissue with parallel and nodular arrays of fibrocytes and fibrillar collagen with a distinctive cork-screw morphology. The differential diagnosis includes various fibroblastic and myofibroblastic proliferations.
Keywords: Ledderhose disease, Plantar fibromatosis, Superficial fibromatosis
A 73-year-old male presented with nodular lesions on the plantar surface of the right foot [Figure 1]. Overlying hyperkeratosis was present. A 6 mm punch biopsy of the plantar surface of the right foot was performed, demonstrating psoriasiform epidermal hyperplasia, hypergranulosis, and hyperkeratosis [Figure 2]. The dermis revealed a spindle cell proliferation featuring fascicles of spindle cells with cork-screw nuclei and fibrillar cork-screw bundles of collagen [Figures 3 and 4]. Immunohistochemical stains were positive for desmin and negative for S-100, CD68, smooth muscle (SM) myosin and h-caldesmon. An immunostain for human papilloma virus was negative.
Figure 1.

Nodular lesion of the plantar surface of the right foot
Figure 2.
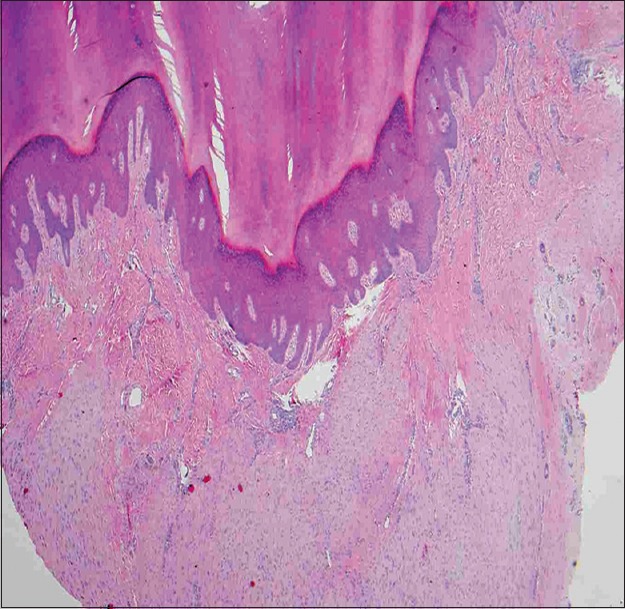
Central invagination of the epidermis with psoriasiform hyperplasia, hypergranulosis, and hyperkeratosis (H and E, ×20)
Figure 3.
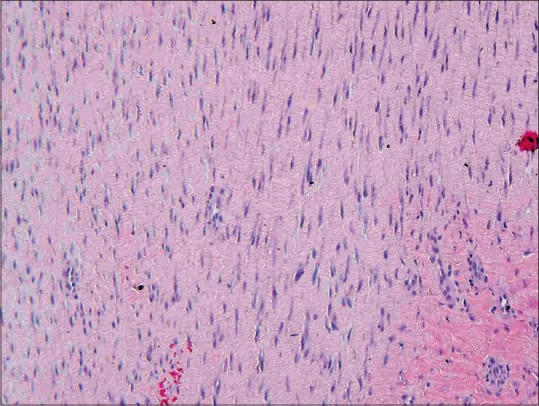
Spindle cell proliferation of dermis with wavy nuclei and fibrillar bundles of collagen (H and E, ×100)
Figure 4.
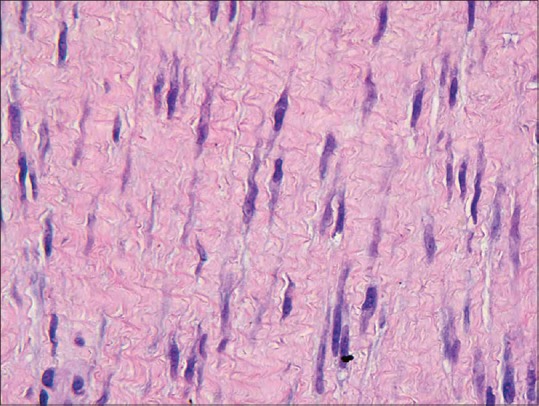
Spindle cell proliferation of dermis with wavy nuclei and fibrillar bundles of collagen (H and E, ×600)
The lesion most likely represents:
Nodular fasciitis
Ledderhose disease (plantar fibromatosis)
Low grade fibromyxoid sarcoma
Neurofibroma
Cutaneous Leiomyosarcoma
ANSWER
B. Ledderhose disease (plantar fibromatosis)
DISCUSSION
Ledderhose disease, or plantar fibromatosis, is a benign hyperproliferative disorder of the plantar aponeurosis first described by George Ledderhouse in 1894.[1] It is part of a heterogeneous group of fibromatoses, including Dupuytren's contracture of the hand and Peyronie's disease of the penis, featuring a proliferation of fibroblasts and collagen. It presents as one or more round, firm slow-growing nodules on the plantar surface of the foot, typically on the medial side, and has bilateral involvement in 25% of cases.[2] Lesions are often asymptomatic, but may become symptomatic when invasion of adjacent neurovascular bundles, muscles, or tendons occurs. Patients may have pain with weight bearing that affects the patient's ability to stand or walk. Ledderhose disease generally appears in middle-aged and elderly adults, though cases have been described in children.[3] Men are affected approximately 10 times more than women.
The etiology of plantar fibromatosis is unknown, though it has been associated with trauma, liver disease, diabetes mellitus, epilepsy and alcoholism.[1] It is often found in association with other fibromatoses such as Dupuytren's contracture. In contrast to fibromatoses associated with Gardner syndrome, plantar fibromatosis is not associated with somatic mutations in the beta-catenin or adenomatous polyposis coli gene.[4]
Histopathological examination of plantar fibromatosis reveals dense fibrocellular tissue with parallel and nodular arrays of fibrocytes and fibrillar collagen with a distinctive cork-screw morphology, evidence of myofibroblastic differentiation. There are variable amounts of extracellular myxoid matrix and compressed and elongated vessels. Three histologic phases occur: The proliferative phase with numerous fibroblasts associated with a small amount of collagen; the active phase with more mature fibroblasts and collagen; and the maturation phase with larger bundles of collagen fibers and fewer bland fibroblasts.[5] All three phases are commonly present together, and the disease is slowly progressive. Atypical cellular features and abnormal mitotic activity are absent, though mitotic figures may be seen. Multinucleated giant cells may be present.[6]
The differential diagnosis of Ledderhose disease includes various spindle cell proliferations. Nodular fasciitis is a reactive proliferation of spindle cells typically found on the extremities of young adults. Lesions feature spindle cells loosely arranged in a mucinous stroma with erythrocyte extravasation and stellate “tissue culture” fibroblasts. Low grade fibromyxoid sarcoma presents as a deep mass involving the trunk and deep extremities (most commonly the thigh) of a young to middle-aged adult. The clinical course is often aggressive and wide excision may not prevent subsequent metastasis. The tumors have a deceptively bland appearance with moderate cellularity and bland fusiform or spindled cells in a heavily collagenized stroma with abrupt transition to myxoid areas. S–100, desmin and caldesmon will be negative and CD34 will be positive. Neurofibromas are characterized by spindle cells with sinusoidal wavy nuclei that stain positive for S–100. The stroma is amphophilic and contains numerous mast cells. Cutaneous leiomyosarcomas present as solitary tender subcutaneous nodules on the extremities of older adults. Histologically, they show a proliferation of spindle cells with cigar-shaped, blunt-ended nuclei arranged in interlacing hypercellular fascicles. They demonstrate a high nuclear to cytoplasmic ratio, variable mitotic figures and pleomorphism, and will also stain positive for caldesmon.
The antidesmin positivity encountered in the presented case is unusual but not uncommon in fibromatoses. Polyclonal antidesmin antibody reacts focally with myofibroblasts that possess cytoskeletons resembling SM cells.[7] Desmin-positive cells likely occur predominantly in the proliferative phase, with a significant decrease during the later fibrous phase, and will make up <25% of tumor cells.[8,9] SM proliferations that typically stain positive for desmin, like leiomyosarcoma and angioleiomyoma, must nonetheless be considered in the differential, though staining is more diffuse in these tumors and will affect 25–>75% of cells.[9] Careful attention to cytological details, architecture and additional muscle stains are also needed to differentiate SM and myofibroblastic tumors. Studies looking at the expression of immunohistochemical markers in various myofibroblastic and SM lesions demonstrated positive and diffuse staining for antimuscle actin, anti-SM actin, anticalponin, anti-SM myosin, and h-caldesmon in leiomyosarcoma cases. Fibromatosis cases demonstrated positive, but more focal, staining for antimuscle actin, anti-SM actin, and anticalponin, but mostly negative reactivity for anti-SM myosin. Furthermore, anti-h-caldesmon is a reliable and specific marker of SM differentiation that demonstrates no reactivity with myofibroblastic cells and thus should be included in questionable cases.[9,10]
Magnetic resonance imaging (MRI) is a useful diagnostic imaging study in the detection of plantar fibromatosis. Lesions typically grow along the aponeurosis and show intensity heterogeneity and infiltrative margins.[11] MRI and clinical findings are similar to clear cell sarcoma, which histologically features clear cytoplasm, nuclear atypia, and S-100 positivity.
Early treatment of plantar fibromatosis includes stretching, orthotics, antiinflammatory drugs, intralesional corticosteroid injections, and physical therapy. For patients with persistent pain, surgical treatment typically requires wide fasciectomy. Postsurgical radiotherapy may diminish the rate of recurrence.[12]
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Ledderhose G. Über zerreisungen der plantarfascie. Arch Klin Chir. 1894;48:853–6. [Google Scholar]
- 2.Goldblum JR, Fletcher JA. Superficial fibromatoses. In: Fletcher CD, Unni KK, Mertens F, editors. Pathology and Genetics of Tumours of Soft Tissue and Bone. 2nd ed. Lyon, France: International Agency for Research on Cancer; 2002. pp. 81–2. [Google Scholar]
- 3.Fetsch JF, Laskin WB, Miettinen M. Palmar-plantar fibromatosis in children and preadolescents: A clinicopathologic study of 56 cases with newly recognized demographics and extended follow-up information. Am J Surg Pathol. 2005;29:1095–105. [PubMed] [Google Scholar]
- 4.Montgomery E, Lee JH, Abraham SC, Wu TT. Superficial fibromatoses are genetically distinct from deep fibromatoses. Mod Pathol. 2001;14:695–701. doi: 10.1038/modpathol.3880374. [DOI] [PubMed] [Google Scholar]
- 5.Farsetti P, Tudisco C, Caterini R, Bellocci M. Ledderhose's disease: Case study with histologic and ultrastructural analysis. Ital J Orthop Traumatol. 1992;18:129–33. [PubMed] [Google Scholar]
- 6.Evans HL. Multinucleated giant cells in plantar fibromatosis. Am J Surg Pathol. 2002;26:244–8. doi: 10.1097/00000478-200202000-00012. [DOI] [PubMed] [Google Scholar]
- 7.Hasegawa T, Hirose T, Kudo E, Abe J, Hizawa K. Cytoskeletal characteristics of myofibroblasts in benign neoplastic and reactive fibroblastic lesions. Virchows Arch A Pathol Anat Histopathol. 1990;416:375–82. doi: 10.1007/BF01605141. [DOI] [PubMed] [Google Scholar]
- 8.Shum DT, McFarlane RM. Histogenesis of Dupuytren's disease: An immunohistochemical study of 30 cases. J Hand Surg Am. 1988;13:61–7. doi: 10.1016/0363-5023(88)90202-x. [DOI] [PubMed] [Google Scholar]
- 9.Ceballos KM, Nielsen GP, Selig MK, O’Connell JX. Is anti-h-caldesmon useful for distinguishing smooth muscle and myofibroblastic tumors? An immunohistochemical study. Am J Clin Pathol. 2000;114:746–53. doi: 10.1309/K5JP-A9EN-UWN7-B5GG. [DOI] [PubMed] [Google Scholar]
- 10.Perez-Montiel MD, Plaza JA, Dominguez-Malagon H, Suster S. Differential expression of smooth muscle myosin, smooth muscle actin, h-caldesmon, and calponin in the diagnosis of myofibroblastic and smooth muscle lesions of skin and soft tissue. Am J Dermatopathol. 2006;28:105–11. doi: 10.1097/01.dad.0000200009.02939.cc. [DOI] [PubMed] [Google Scholar]
- 11.Bancroft LW, Peterson JJ, Kransdorf MJ. Imaging of soft tissue lesions of the foot and ankle. Radiol Clin North Am. 2008;46:1093–103. doi: 10.1016/j.rcl.2008.08.007. vii. [DOI] [PubMed] [Google Scholar]
- 12.Wapner KL, Ververeli PA, Moore JH, Jr, Hecht PJ, Becker CE, Lackman RD. Plantar fibromatosis: A review of primary and recurrent surgical treatment. Foot Ankle Int. 1995;16:548–51. doi: 10.1177/107110079501600906. [DOI] [PubMed] [Google Scholar]


