Abstract
Aims
Older and disabled rheumatoid arthritis (RA) patients are often not present in large numbers in clinical trials or registries. A novel, claims‐based clinical effectiveness algorithm provides the potential to compare the effectiveness of different biologics among this population using large administrative databases.
Method
Using Medicare 2006–2010 data for 100% of patients with RA, we identified biologic naïve users of abatacept, adalimumab, etanercept and infliximab, defined as no biologic use during the 12 months before the biologic initiation. The effectiveness was evaluated at 365 days after biologic initiation, determined using a validated claims‐based algorithm. We compared the proportion meeting effectiveness criteria for each biologic using robust Poisson regression to compute risk ratios (RRs) adjusted for potential confounders. One year cost per effectively treated patient was calculated by different biologics.
Results
The study included biologic naïve users of abatacept (n = 2129), adalimumab (n = 2944), etanercept (n = 3517) and infliximab (n = 5654). The algorithm classified the medications as 26% effective for abatacept, 24% for adalimumab, 28% for etanercept and 23% for infliximab, indicating comparable effectiveness. However, after adjustment and compared with infliximab, the RRs for effectiveness were 1.17 (95% CI 1.06, 1.30) for abatacept, 1.11 (95% CI 1.02, 1.23) for adalimumab and 1.27 (95% CI 1.17, 1.39) for etanercept. Older patients had a higher effectiveness than patients who were disabled (RR = 1.18, 95% CI 1.08, 1.28). Infliximab had highest cost per effectively treated patient.
Conclusion
Abatacept, adalimumab and etanercept are more effective than infliximab among RA patients initiating biologics. Effectiveness was significantly higher among older patients compared with disabled RA Medicare patients.
Keywords: biologics, claims‐based algorithm, comparative effectiveness, medicare, rheumatoid arthritis
What is Already Known About this Subject
The US Medicare programme collects data on medical diagnoses, procedures, hospitalizations, costs, mortality and the use of prescription for older and disabled patients, who are not present in large numbers in clinical trials or registries. One potential obstacle to using this data source for evaluating the effectiveness of specific DMARDs for patients with rheumatoid arthritis is the lack of detailed clinical information, such as disease activity. A novel, claims‐based clinical effectiveness algorithm provides the potential to compare the effectiveness of different biologics among this population using large administrative databases.
What this Study Adds
We evaluated the real world effectiveness of biologic DMARDs in Medicare RA patients using a previously validated claims‐based algorithm and found that users of abatacept, adalimumub and etanercept were associated with higher effectiveness compared with users of infliximab, these associations were stronger when the analyses were limited to disabled patients and 1 year cost per effectively treated patient was lower for etanercept, adalimumab and abatacept than for infliximab. This study supports further use of the claims‐based algorithm in comparative effectiveness research.
Introduction
Rheumatoid arthritis (RA) is a chronic disease affecting two million adults in the United States and can substantially impair physical functioning. Treatment of RA aims to control pain and slow the progression of joint destruction and disability 1, 2. In the treatment of RA, guidelines have changed significantly since the first biologic disease‐modifying antirheumatic drugs (DMARDs) targeting tumour necrosis factor (anti‐TNF) were approved by the Food and Drug Administration (FDA) 3. First line RA biologic treatments include anti‐TNF therapies (e.g. etanercept, adalimumab, infliximab) and newer biologics with different mechanisms of action such as abatacept 4. Achieving a better understanding of the comparative effectiveness of these biologic treatments for patients with RA has been identified as one of the top national priorities recommended by the Institute of Medicine in 2009 5.
Clinical trials and observational studies using registries or administrative data are commonly used approaches for developing evidence for comparative effectiveness research (CER). However, current CER for comparing the effectiveness of biologic DMARDs among RA patients is scant. To date, only a few head‐to‐head RCTs have been conducted that have compared one biologic DMARD directly with another to determine effectiveness 6, 7, 8, and these trial results rarely reflect the availability and effectiveness of medical therapies used in routine medical practice, particularly for those older and disabled patients. Observational studies have been small in size, have yielded mixed results and provided very limited direct evidence regarding the effectiveness and cost differences associated with different biologics 4, 9, 10, 11.
The US Medicare programme collects data on medical diagnoses, procedures, hospitalizations, costs, mortality and the use of prescription medications 12, 26, thus, providing enormous potential for CER. One potential obstacle to using this data source for evaluating the effectiveness of specific DMARDs for RA is the lack of detailed clinical information, such as disease activity. Recently, a claims‐based algorithm was developed and validated to serve as a proxy for clinical improvement in RA 3, 26, using a linkage between claims data and a large observational registry of RA patients. The gold standard for assessing the validity of the claims‐based algorithm was low disease activity (DAS28ESR ≤3.2) or a meaningful improvement in DAS28ESR by >1.2 units. This gold standard, the DAS28ESR score, is used as an outcome in many clinical trials of RA therapies. Compared with the clinical gold standard, the algorithm's sensitivity (0.75, 95% confidence interval (CI) 0.62, 0.86), specificity (0.90, 95% CI 0.84, 0.94), positive predictive value (0.75, 95% CI 0.62, 0.86), and negative predictive value (0.90, 95% CI 0.84, 0.94) for biologic users were in the range of 75% to 90% 26. Thus, the current study used the claims‐based algorithm to evaluate the effectiveness of etanercept, adalimumab, infliximab and abatacept in Medicare patients with RA. We also estimated the costs per biologic responder, taking a payer perspective to estimate costs to the Medicare programme.
Methods
Study design and eligible population
We conducted a retrospective cohort study using Medicare claims data from 2006–2010 for 100% of RA beneficiaries. The data included the Medicare patient enrolment file, inpatient (Part A) and outpatient medical care (Part B) claims and prescription drug claims (Part D). These files provided patients' demographic information and their claims for inpatient, outpatient, skilled nursing facility, non‐institutional provider, home health and hospice care, for durable medical equipment services and for prescription drugs. This study was approved by a Data Use Agreement from the Centers for Medicare and Medicaid system (CMS) and the Institutional Review Board of the University of Alabama at Birmingham (UAB).
We identified RA patients using the International Classification of Diseases, Ninth Revision, Clinical Modification codes (ICD9‐9‐CM). Eligible patients had at least two RA ICD9‐9‐CM diagnosis codes (714.x) from rheumatologist visits that were separated by greater than 7 days but occurred within 365 days of each other, or they had one ICD‐9‐CM code for RA from a rheumatologist visit, followed by a prescription for, or an infusion of, methotrexate, leflunomide, sulfasalazine, hydroxychloroquine, an anti‐TNF or non‐anti TNF biologic approved for RA. Among RA beneficiaries, we identified biologic naïve users of etanercept, adalimumab, infliximab and abatacept during the study period. Naïve users of a particular drug were defined as having therapy initiated after a baseline period of 12 months, during which there was no prescription for or infusion of any biologic agent. All individuals in this cohort study were required to have continuous enrolment in fee‐for‐service Medicare parts A, B and D, and not be in a Medicare Advantage plan, in the 12 month baseline period and for 365 days after the start of follow‐up. We excluded patients who had a diagnosis of psoriatic arthritis, psoriasis, ankylosing spondylitis or inflammatory bowel disease during the 12 month baseline period. The earliest date for initiation of etanercept, adalimumab, infliximab or abatacept therapy was January 1 2007. The initiation date was defined as the ‘index date’. With this design, each patient contributed one observation to the analysis, classified according to the first biologic initiated.
Main exposures
We identified biologic naïve users of etanercept, adalimumab, infliximab and abatacept using Healthcare Common Procedures Coding System (HCPCS) J codes and pharmacy records that included national drug code (NDC) codes, drug name and days supplied.
Outcomes
The outcome of interest was effectiveness as of the end of the 365 day follow‐up period, as determined by the claims‐based effectiveness algorithm applied to Medicare data 26. The effectiveness algorithm required six criteria to be met: 1) no switching to a different biologic, 2) high adherence to the index biologic, 3) no addition of a new non‐biologic DMARD that the patient had not been on in the 6 months prior to the index date, 4) no biologic dose increase compared with the starting dose, 5) for patients not using oral glucocorticoids during the 6 months prior to the index date, they cannot receive more than 30 days of oral glucocorticoids during follow‐up. For patients using glucocorticoids during the 6 months prior to the index date, the cumulative glucocorticoid dose in the second 6 months of follow‐up must be similar to the cumulative dose in the 6 months prior to the index date ( maximum 120% of initial dose ) and 6) no more than one joint injection on a unique day after the patient had been receiving the new treatment for more than 3 months. Each of the components was treated as dichotomous. For treatment to be classified as effective, patients must have satisfied all conditions.
Potential confounders
From Medicare patient enrolment files, we defined each patient's gender, race, region and age on the index date. We identified the patient's disability status based upon their original reason for Medicare enrolment. From claims in the 12 months preceding the index date, we determined if the patient had low socio‐economic status and if the patient was a nursing home resident. Low socioeconomic status was defined as receipt of a low income subsidy or Medicaid eligibility during the baseline period. Nursing home residents were identified using a validated algorithm with high sensitivity and specificity 13. To control better for patients' RA activity and disease severity during baseline, we used baseline period claims data on diagnoses of RA related conditions (e.g. orthopaedic surgery, baseline infection related hospitalization and rheumatoid factor laboratory test), outpatient infections and on use of narcotics, antibiotics and RA medications (e.g. glucocorticoids, methotrexate, leflunomide, sulfasalazine and hydroxychloroquine). Glucocorticoid doses were calculated as prednisone equivalents (categorized as none, ≤7.5 mg day–1 and >7.5 mg day–1). We further determined each patient's use of health services during the baseline period, including non‐infection related hospitalization, ambulatory physician visits, number of outpatients visits and other comorbidities (chronic obstructive pulmonary disease (COPD), diabetes, cerebrovascular disease, peptic ulcer disease, prior fractures, hypertension, heart failure, acute myocardial infarction, liver disease, cancer, depressive illness), and calendar year of biologic initiation.
Statistical analysis
Patient demographic and baseline characteristics were compared among the four cohorts of biologic users using means and SDs for continuous variables and percentages for categorical variables. Using infliximab as the reference group, we calculated the standardized mean differences (SMD) between groups for each variable. SMD with a value of <0.1 were considered as unimportant 14. For each biologic cohort, we estimated the incidence proportion for effectiveness as the number of patients who met all six effectiveness criteria during the 365 day follow‐up period, divided by the total number of patients in the specific cohort.
Poisson regression models with robust parameters were used to obtain crude and adjusted risk ratios (RRs) for effectiveness of different biologic agents with infliximab used as referent. Multivariable adjustment included all potential confounders. We conducted subgroup analyses stratified according to patient disability status, low socio‐economic status and baseline glucocorticoid dosage categories (none, <=7.5 mg day–1 and >7.5 mg day–1). Because the effectiveness algorithm used in the current study did not require a rheumatologist visit during follow‐up (as did the original validation study, in order to assess the clinical outcome), we also conducted a sensitivity analysis by restricting each biologic cohort to patients who had 14 months of follow‐up and had an outpatient rheumatologist visit at any time during follow‐up months 10 and 14. To evaluate the potential effect of unmeasured confounding, such as baseline disease activity, on the comparative effectiveness, we conducted an additional rule‐out sensitivity analysis 15. To evaluate further the robustness of our results, abatacept vs. infliximab was used as an example because of their smallest and largest sample sizes in the current study. Based on the distribution of the clinical disease activity index (CDAI) reported in a previous study 4, we assumed the prevalence of high disease activity (Pc) (vs. moderate or lower) among biologic naïve users is 0.20. Since there were 2129 and 5654 abatacept and infliximab naïve users, respectively, we assumed the prevalence of drug exposure was 0.27 (Pe) in the sensitivity analysis. According to these assumptions, we evaluated the set of conditions that unmeasured disease activity would make the current significant association back to null. Finally we calculated the average 1 year treatment cost of therapy with each biologic by summing the amounts paid by Medicare and amounts paid by patients for all medical and pharmacy claims for that agent. The mean cost of each intravenous biologic also included infusion‐related procedure costs. Cost per effectively treated patient was calculated as the total cost of the index biologic divided by the number of patients classified as effectively treated by that biologic, according to the claims‐based algorithm. All costs were converted to constant 2010 dollars using the health care inflation rate. All analyses were conducted using SAS version 9.3 (SAS Institute, Cary, North Carolina, USA).
Results
From the total population of Medicare patients with autoimmune disease during 2006–2010, we identified 579 474 RA patients with at least two RA diagnosis codes from rheumatologists or one diagnosis code followed by a prescription or infusion of a biologic or DMARD (Figure 1). After excluding patients who never took biologics and prevalent biologic users, we identified 168 274 new qualifying biologic users who had not taken any biologics in the prior 12 months. After further excluding patients who did not have continuous full Medicare fee‐for‐service coverage (enrolled in Medicare Part A and Part B, but not in a Medicare advantage plan) and Part D pharmacy coverage during the 12 months before and 365 days after the index date, and patients who had diagnosis of psoriasis, psoriasis arthritis, inflammatory bowel disease or ankylosing spondylitis during baseline, the final cohort was reduced to 14 244 patients and included naïve biologic users of abatacept (n = 2129), adalimumab (n = 2944), etanercept (n = 3517) and infliximab (n = 5654).
Figure 1.
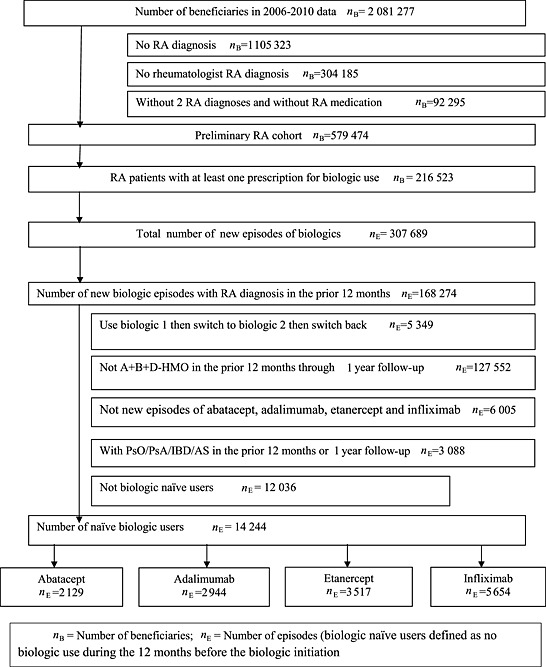
Flowchart for cohort selection. n B, number of beneficiaries; n E, number of episodes (biologic naïve users defined as no biologic use during the 12 months before biologic initiation; PsO, psoriasis; PsA, psoriatic arthritis; IBD, inflammatory bowel disease; AS, ankylosing spondylitis
Baseline characteristics of the four biologic cohorts are shown in Table 1. Compared with users of adalimumab and etanercept, abatacept and infliximab users were more likely to be White, older but non‐disabled, and have higher incomes. The cohorts were similar with respect to RA related conditions, health services utilization including baseline non‐infection related hospitalizations and baseline ambulatory physician visits, comorbidities (including diabetes, liver disease, dementia and renal disease), and other medications (including average glucocorticoid dose, narcotics, antibiotics and anti‐depressive medications during baseline). Histories of coronary heart disease (CHD), heart failure and/or peripheral vascular disorder were more common among abatacept users than for other cohorts.
Table 1.
Distribution of biologic naïve users by selected baseline characteristics among rheumatoid arthritis patients in US Medicare population
| Abatacept | Adalimumab | Etanercept | Infliximab | ||||
|---|---|---|---|---|---|---|---|
| Total population | 2129 | SMD | 2944 | SMD | 3517 | SMD | 5654 |
| Demographic covariates: | |||||||
| Age * , years (SD) | 69.9 (11.2) | 0.06 | 63.0 (12.9) | 0.55 | 63.7 (13.0) | 0.48 | 69.3 (10.1) |
| Female, % | 83.5 | 0.11 | 83.0 | 0.08 | 82.5 | 0.07 | 79.8 |
| Race, % | |||||||
| White | 82.3 | 0.05 | 72.3 | 0.30 | 76.3 | 0.21 | 84.5 |
| Black | 9.4 | 0.01 | 17.3 | 0.23 | 13.1 | 0.11 | 9.6 |
| Other | 8.3 | 0.08 | 10.4 | 0.16 | 10.6 | 0.17 | 5.9 |
| Urban, % | 75.2 | 0.10 | 68.2 | 0.08 | 71.3 | 0.03 | 70.0 |
| Receipt of lower income subsidy, % | 23.8 | 0.07 | 49.7 | 0.82 | 46.2 | 0.68 | 22.7 |
| Nursing home/community dwelling | 5.1 | 0.02 | 4.4 | 0.03 | 5.2 | 0.01 | 5.1 |
| Original reason for Medicare entitlement, % | |||||||
| Old age and survivors insurance | 72.6 | 0.16 | 50.1 | 0.57 | 55.1 | 0.45 | 77.9 |
| Disabled or ESRD | 27.4 | 0.16 | 49.9 | 0.56 | 44.9 | 0.43 | 22.1 |
| RA related conditions, % | |||||||
| Orthopaedic surgery | 8.8 | 0.01 | 7.8 | 0.10 | 8.7 | 0.03 | 9.1 |
| Baseline infection related hospitalization | 10.3 | 0.14 | 9.0 | 0.06 | 9.7 | 0.13 | 8.1 |
| Any rheumatoid factor laboratory test | 47.0 | 0.22 | 50.8 | 0.09 | 52.0 | 0.07 | 55.4 |
| Health service utilization, % | |||||||
| Baseline non‐infection related hospitalization | 27.7 | 0.14 | 24.4 | 0.01 | 27.8 | 0.07 | 24.7 |
| Ambulatory physician visit during baseline * | 21.2 (13.3) | 0.16 | 18.9 (12.8) | 0.04 | 19.9 (13.8) | 0.04 | 19.4 (12.0) |
| Comorbidity covariates, % | |||||||
| Chronic pulmonary disease (COPD) | 20.3 | 0.05 | 22.0 | 0.11 | 23.1 | 0.16 | 19.1 |
| Diabetes | 21.1 | 0.05 | 23.5 | 0.19 | 22.1 | 0.12 | 19.6 |
| Diabetes with chronic complications | 4.1 | 0.09 | 4.2 | 0.11 | 4.0 | 0.09 | 3.1 |
| Cerebrovascular disease | 5.8 | 0.11 | 4.5 | 0.04 | 4.9 | <0.01 | 4.9 |
| Prior fractures | 8.5 | 0.13 | 6.4 | 0.04 | 8.1 | 0.10 | 6.8 |
| Hypertension | 56.7 | 0.06 | 50.2 | 0.07 | 51.2 | 0.06 | 53.6 |
| Heart failure | 9.0 | 0.26 | 5.5 | <0.01 | 6.7 | 0.09 | 5.5 |
| Acute myocardial infarction | 3.1 | 0.08 | 2.1 | 0.06 | 2.8 | 0.03 | 2.6 |
| Cancer | 6.3 | 0.04 | 3.5 | 0.17 | 5.1 | 0.02 | 5.4 |
| Other medication use, % | |||||||
| Narcotic use (%), | 76.5 | 0.18 | 76.8 | 0.19 | 77.6 | 0.23 | 72.6 |
| Average glucocorticoid use | |||||||
| None | 40.0 | 0.06 | 39.1 | 0.06 | 37.8 | 0.03 | 36.3 |
| <7.5 mg day–1 | 44.8 | 0.04 | 45.4 | 0.04 | 44.8 | 0.05 | 47.4 |
| > = 7.5 mg day–1 | 15.2 | 0.03 | 15.6 | 0.02 | 17.4 | 0.03 | 16.4 |
| Antibiotic | 74.2 | 0.07 | 72.6 | 0.03 | 73.6 | 0.05 | 71.2 |
| Anti‐depressive medication | 38.1 | 0.12 | 43.3 | 0.32 | 42.3 | 0.28 | 35.5 |
All factors measured during baseline and displayed as column %, except age and ambulatory physician visit during baseline expressed as mean (SD).
ESRD, end‐stage renal disease.
The algorithm classified the medication as effective for 26% of abatacept users, 24% of adalimumab users, 28% of etanercept users and 23% of infliximab users (Table 2). For users of abatacept, adalimumab and etanercept, the most common reason for failing the effectiveness algorithm was low adherence to the index medications, whereas for users of infliximab, the most common reason for failure was dose escalation during follow‐up. The percentages of patients who failed other criteria of the algorithm were very similar across biologic cohorts.
Table 2.
Components of the effectiveness algorithm† for adalimumab, etanercept, infliximab and abatacept at 1 year*
| Abatacept | Adalimumab | Etanercept | Infliximab | |
|---|---|---|---|---|
| Total number of patients | 2129 | 2944 | 3517 | 5654 |
| Satisfied all six effectiveness criteria, % | 26 | 24 | 28 | 23 |
| No switch to a different biologic | 89 | 86 | 84 | 88 |
| High adherence to the index drug | 54 | 52 | 55 | 73 |
| No addition of a new non‐biologic DMARD | 88 | 89 | 89 | 89 |
| No biologic dose increase compared with starting dose | 92 | 95 | 99 | 65 |
| For patients not using glucocorticoids at baseline, no initiation of glucocorticoids; for patients using glucocorticoids at baseline, no increase in dose | 87 | 85 | 88 | 86 |
| No more than one joint injection on unique days after the 3 months of new treatments | 85 | 89 | 90 | 88 |
assessed between the first exposure date and 365 days after the drug initiation.
DMARD = disease‐modifying antirheumatic drug
After adjusting for potential confounders and compared with infliximab, abatacept (RR 1.17, 95% CI 1.06, 1.29), adalimumab (RR 1.11, 95% CI 1.01, 1.21) and etanercept (RR 1.26, 95% CI 1.16, 1.37) exhibited elevated relative benefit for effectiveness (Table 3). The effectiveness of biologics was greater among non‐disabled persons compared with disabled patients (RR 18, 95% CI 1.08, 1.28). Effectiveness of biologics was greater among patients who were on infusions compared with subcutaneous self‐injected biologics (RR 1.26, 95% CI 1.15, 1.39) (Table 3). Factors associated with lower effectiveness included being African‐American or of other race/ethnicity groups, residency in a nursing home, and use of antidepressants, narcotics and/or glucocorticoids greater than 7.5 mg day–1 during baseline.
Table 3.
Crude and adjusted risk ratio for medication effectiveness using robust Poisson analysis
| Crude | Adjusted | |||
|---|---|---|---|---|
| Baseline biologic use | RR | 95% CI | RR | 95% CI |
| Abatacept | 1.13 | 1.02, 1.25 | 1.17 | 1.06, 1.30 |
| Adalimumab | 1.05 | 0.95, 1.14 | 1.11 | 1.02, 1.23 |
| Etanercept | 1.19 | 1.09, 1.29 | 1.27 | 1.17, 1.39 |
| Infliximab | Ref | Ref | ||
| Demographic covariates | ||||
| Aged vs. Disabled | 1.18 | 1.10, 1.27 | 1.18 | 1.08, 1.28 |
| Male vs. Female | 1.10 | 1.02, 1.20 | 1.07 | 0.98, 1.16 |
| Black vs White | 0.88 | 0.79, 0.98 | 0.89 | 0.80, 0.99 |
| Other vs. White | 0.79 | 0.69, 0.90 | 0.77 | 0.68, 0.88 |
| Receipt of higher income subsidy vs. receipt of lower or no income subsidy | 1.08 | 1.00, 1.15 | 0.95 | 0.87, 1.04 |
| Rural vs. urban | 1.03 | 0.96, 1.10 | 1.00 | 0.94, 1.09 |
| Nursing home vs. community dwelling | 0.60 | 0.47, 0.72 | 0.67 | 0.55, 0.81 |
| Calendar year | ||||
| 2008 vs. 2007 | 1.02 | 0.94, 1.10 | 1.02 | 0.94, 1.10 |
| 2009 vs. 2007 | 1.02 | 0.94, 1.11 | 1.06 | 0.96, 1.16 |
| RA related conditions | ||||
| Orthopaedic surgery | 0.88 | 0.78, 0.99 | 1.04 | 0.91, 1.18 |
| Intra‐articular injection | ||||
| Baseline infection related hospitalization | 0.78 | 0.69, 0.88 | 1.03 | 0.88, 1.19 |
| Any rheumatoid factor laboratory test | 0.89 | 0.84, 0.95 | 0.94 | 0.88, 1.01 |
| Health Service utilization: | ||||
| Baseline non‐infection related hospitalization | 0.80 | 0.74, 0.87 | 0.97 | 0.87, 1.08 |
| Ambulatory physician visit during baseline | 0.99 | 0.98, 0.99 | 0.99 | 0.98, 0.99 |
| Comorbidity covariates | ||||
| Chronic pulmonary disease (COPD) | 0.82 | 0.75, 0.89 | 0.93 | 0.85, 1.02 |
| Diabetes | 0.89 | 0.82, 0.97 | 0.99 | 0.90, 1.08 |
| Diabetes with complications | 0.74 | 0.61, 0.90 | 0.88 | 0.71, 1.09 |
| Cerebrovascular disease | 1.02 | 0.87, 1.18 | 1.14 | 0.98, 1.34 |
| Prior fractures | 0.90 | 0.79, 1.03 | 1.05 | 0.91, 1.20 |
| Hypertension | 0.93 | 0.97, 0.99 | 1.02 | 0.95, 1.09 |
| Heart failure | 0.83 | 0.72, 0.96 | 1.00 | 0.86, 1.17 |
| Acute myocardial infarction | 0.86 | 0.69, 1.07 | 1.03 | 0.82, 1.30 |
| Cancer | 1.03 | 0.89 | 1.06 | 0.91, 1.23 |
| Other medication use | ||||
| Narcotic use (%), | 0.73 | 0.68, 0.78 | 0.82 | 0.76, 0.88 |
| Average glucocorticoid use | ||||
| <7.5 mg day–1vs. none | 0.87 | 0.81, 0.93 | 1.00 | 0.91, 1.10 |
| >7.5 mg day–1vs. none | 0.91 | 0.82, 1.00 | 0.90 | 0.84, 0.97 |
| Antibiotic | 0.85 | 0.79, 0.91 | 0.97 | 0.90, 1.05 |
| Antidepressants | 0.78 | 0.73, 0.84 | 0.88 | 0.82, 0.94 |
The adjusted risk ratios of biologic effectiveness in subgroup and sensitivity analyses stratified by patients' initial Medicare entitlements are presented in Figure 2. Among non‐disabled patients, etanercept had the highest effectiveness. Among patients who received Medicare benefit due to disability, etanercept had the highest effectiveness with greater estimated risk ratio. The risk ratios of effectiveness for abatacept, etanercept and adalimumab were greater compared with the main analysis. The result of the rule‐out sensitivity analysis is shown in the Supplementary Figure S1. We found out that the association between drug use and high disease activity (OREC) or the association between high disease activity and effectiveness (RRCD) must be very strong to move the adjusted exposure relative risk to null. As it is very unlikely for OREC to be greater than 2 and RRCD to be greater than 3, our results are robust in most cases.
Figure 2.
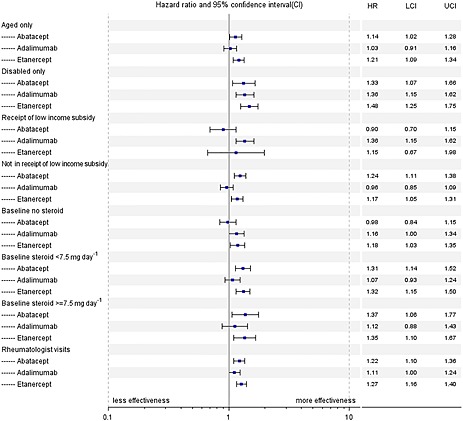
Sensitivity analyses of various subgroup analyses examining effectiveness of biologic treatments referent to infliximab among Medicare enrollees with rheumatoid arthritis
The average 1 year treatment costs per patient were similar for the four different biologic cohorts (Table 4). After considering administration costs and the proportion of effectiveness for patients, the 1 year total cost per patient categorized as effectively treated (in descending order) was $62 666 for infliximab, $55 096 for abatacept, $51, 436 for adalimumab and $45 910 for etanercept. Comparative effectiveness of these biologic DMARDs from the sensitivity analysis restricting patients to those who had rheumatologist visits at approximately 1 year yielded similar results (Supplementary Table S1).
Table 4.
Mean cost related to the index biologic among patients with rheumatoid arthritis
| Abatacept | Adalimumab | Etanercept | Infliximab | |
|---|---|---|---|---|
| Parameter | (n = 2129) | (n = 2944) | (n = 3517) | (n = 5654) |
| Index biologic cost * | ||||
| Mean | 13 506 | 12 859 | 12 855 | 13 573 |
| SD | 7120 | 8286 | 7636 | 11 128 |
| Administration cost † | ||||
| Mean | 1371 | N/A | N/A | 1467 |
| SD | 926 | 1382 | ||
| Total cost | ||||
| Mean | 14 876 | 12 859 | 12 855 | 15 040 |
| SD | 7699 | 8286 | 7636 | 11 939 |
| Effectively treated patients ‡ | ||||
| n (%) | 574 (27%) | 726 (25%) | 989 (28%) | 1346 (24%) |
| Cost per effectively treated patient | ||||
| Mean | 55 096 | 51 436 | 45 910 | 62 666 |
Costs are rounded and adjusted to 2010 dollar in the table for clarity.
Subcutaneous agents have no administration cost because they are self‐administered.
Patients who did not fail any of the six algorithm criteria throughout the 12 month post‐index period.
Discussion
We evaluated the real world effectiveness of biologic DMARDs in Medicare RA patients using a recently published claims‐based effectiveness algorithm. The algorithm classified these biologics as effective for 26% of abatacept, 24% of adalimumab, 28% of etanercept and 23% of infliximab users, respectively. Compared with users of infliximab and with multiple variables adjustment, users of abatacept, adalimumub and etanercept were associated with higher effectiveness. Among disabled patients, etanercept users were associated with 48% higher effectiveness compared with infliximab users. Among patients who used glucocorticoid greater than 7.5 mg day–1 during baseline, abatacept use was associated with 37% higher effectiveness compared with infliximab use.
A few head‐to‐head RCTs have produced evidence for CER among RA patients 16. For example, the AMPLE (Abatacept vs. Adalimumab comparison in Biologic Naïve Subjects with Background Methotrexate) study compared the efficacy and safety of 646 subcutaneous abatacept vs. adalimumab users, with background methotrexate and reported that the ACR20 response rates were 64.8% for abatacept and 63.4% for adalimumab, indicating that abatacept was non‐inferior to adalimumab 6. Among 325 participants of the ADACTA (ADAlimumab and ACTemrA) trial, tocilizumab was superior to adalimumab in the change in DAS28 (–3.3 vs. –1.8, P < 0.001) 8. However, these results reflect only a small number of RA patients who were enrolled in a clinical trial, yielding potential imitations due to small sample size and multiple exclusion criteria that would limit generalizability to real‐world settings.
Several observational studies have been published that directly compared the effectiveness of biologics with one another 4, 17, 18, 19. Of 119 RA patients treated with anti‐TNF drugs, a study conducted in Spain demonstrated no significant differences among users of etanercept, adalimumab and infliximab 20. Similarly, no differences were observed in drug response or remission among 2242 biologic naïve users or switchers of etanercept, adalimumab and infliximab in the consortium of Rheumatology Researchers of North America (CORRONA) registry 4. In contrast, using the nationwide Danish Biologic (DANBIO) registry of RA patients receiving routine care 11 and the Dutch Rheumatoid Arthritis Monitoring (DREAM) registry 21, studies found that compared with infliximab, both adalimumab and etanercept were associated with higher odds of treatment response. Because these RA patient registries have small sample sizes, incomplete data on comorbidities and other medications, their generalizability has been limited 3. The current study used a large administrative claims database and classified these biologics as effective for 26% users of abatacept, 24% of adalimumab, 28% of etanercept and 23% of infliximab users. Without adjustment, the effectiveness of these treatments is broadly comparable. However, after adjustment, we found that abatacept, etanercept and adalimumab users had higher effectiveness than users of infliximab. These findings, being consistent with DANBIO and DREAM studies, provide valuable information to study CER of rheumatoid disease therapies. Furthermore, the cost per effectively treated patient has important cost differences yields infliximab and other biologic groups.
Findings from the present study suggest that medication effectiveness for RA patients was higher among older, non‐disabled patients compared with disabled patients. Although studies have shown that older age was a negative predictor of a clinical response, our study found that disabled patients were less likely to respond, regardless of their age. Our study revealed that patients who were of a non‐White race/ethnicity, a nursing home resident, or a user of antidepressants, narcotics or high dose glucocorticoids were less likely to respond to biologic DMARDs. These results were consistent with previous studies that documented that disability, low functional status and concomitant glucocorticoid use were inversely associated with clinical response 11, 22. The possible explanation for these results could be that patients residing in long term nursing homes were more likely to be disabled and have difficulty functioning in their daily lives. Hence, being a nursing home resident could stand for unmeasured confounders or multimorbidities. The significant inverse association between taking antidepressants or narcotics and effectiveness may be explained because these medications could serve as markers for comorbidities involving chronic pain or mood disorders 22, and RA patients with depression or other chronic pain syndromes may not be perceived to improve as much as patients with RA who do not have these conditions.
This analysis investigated the cost implications of these variations in effective biologic use. The first year drug cost for biologic treatment among rheumatoid arthritis patients was between $12 800 and $13 600. However, after considering the estimates of effectiveness per the claims‐based algorithm for each biologic, cost per patient categorized as effectively treated ranged from $45 910 (etanercept) to $62 666 (infliximab). Nearly 35% of the patients in this cohort had their infliximab dose increased in the 12 month post‐index period. Several previous studies have also reported that dose escalation or more frequent administration is common with infliximab use in clinical practice 23, 24, 25. The high adherence criterion failed other biologic in this analysis by approximately 50% of the patients in the 12 month follow‐up period. The cost differences were amplified in the comparison of cost per effectively treated patient in this analysis, particularly for infliximab with higher cost and lower effectiveness compared with other biologics. Given the relatively comparable effectiveness between biologics, two factors accounted for appreciable variability in differences in costs. These two factors are the potential for some but not all drugs to be dose‐escalated (e.g. infliximab) and infusion‐related administration costs. Elimination of these two factors would likely reduce much of the differences between drugs in the costs per effectively‐treated patients. However, there is a preferential coverage benefit to patients for infused drugs (rather than subcutaneously injected drugs) in the Medicare programme.
There are several strengths in the current study including the use of the large Medicare national RA database providing a high degree of generalizability to US adults ≥ 65 years of age and disabled patients. Additional strengths include CER using administrative data with large sample size, high validity and completeness of prescription drug and low cost. Furthermore, this validated algorithm had high sensitivity, specificity and positive predictive values and related to actionable interventions that clinicians use (e.g. increase glucocorticoid dose, add non‐biologic DMARDs) to improve treatment efficacy. However, the results from the current analysis should be interpreted in the context of known and potential limitations. The algorithm has been validated in a Veteran's Administration (VA) population 26 and in a commercially insured population 27, but not specifically in a Medicare RA population. Although the algorithm does not directly include pain, an important determinant of the patient's perception of RA disease activity, use or dose change of glucocorticoids in the algorithms account for the management of pain and flares associated with the inflammation. Additionally, we required patients to have full Medicare coverage through the 12 months baseline and follow‐up. The results of this study may not be generalizable to patients whose follow‐up time was less than 1 year. Finally, we relied on pharmacy fill data to identify our main exposure, but patients do not necessarily take drugs as prescribed.
In conclusion, we evaluated the real world effectiveness of biologic DMARDs in Medicare RA patients using a previously validated claims‐based algorithm. We found that compared with the use of infliximab, use of abatacept, adalimumab and etanercept was associated with higher effectiveness. These associations were stronger when the analyses were limited to disabled patients. We also found that 1 year cost per effectively treated patient was lower for etanercept, adalimumab and abatacept than for infliximab. This study supports further use of the claims‐based algorithm in CER.
Competing Interests
All authors have completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare the submitted work had support from the Agency for Healthcare Research and Quality (AHRQ) and (R01HS018517) and AMGEN.
HY, FX, ED had a research grant from AMGEN for unrelated work in the previous 3 years, KGS had research grants and/or consulting for unrelated work with AMGEN, Abbott, BMS, Celgene, Centocor, CORRONA, Crescendo, Genentech, Janssen, Pfizer, Roche and UCB in the previous 3 years and JRC had research grants and/or consulting for unrelated work with AMGEN, Abbott, BMS, Celgene, Centocor, CORRONA, Crescendo, Genentech, Janssen, Pfizer, Roche and UCB in the previous 3 years.
JGJ is an employee and stockholder of Sanofi and a former employee and stockholder of AMGEN Inc. DJH is an employee and stockholders of AMGEN Inc.
This work was supported by the Agency for Healthcare Research and Quality (AHRQ) (R01HS018517) and AMGEN. Dr Yun was supported by grant 1 K12 HS021694 from the Agency for Healthcare Research and Quality, Rockville, MD, USA. Dr Curtis receives support from the NIH (AR 053351).
Author Contributions
Conception and design: HY, JRC
Analysis and interpretation of the data: HY, FX, Delzell E,ED, KGS, JRC
Drafting of the article: HY, JRC
Critical revision of the article for important intellectual content: HY, FX, ED, LC, SY, KGs, GJJ, DJH, JRC
Final approval of the article: HY, FX, ED, LC, SY, KGS, GJJ, DJH, JRC
Obtaining of funding: JRC
Administrative, technical or logistic support: HY, FX, ED, LC, SY, KGS, GJJ, DJH, JRC
Collection and assembly of data: HY, FX, JRC
Supporting information
Figure S1 Rule‐out sensitivity analysis for unmeasured confounder.
Table S1 Components of the effectiveness algorithm† for adalimumab, etanercept, infliximab and abatacept at one year * among patients who had rheumatologists visits during 10‐14 months of follow up.
Supporting info item
Yun, H. , Xie, F. , Delzell, E. , Chen, L. , Yang, S. , Saag, K. G. , Joseph, G. , Harrison, D. , and Curtis, J. R. (2015) The comparative effectiveness of biologics among older adults and disabled rheumatoid arthritis patients in the Medicare population. Br J Clin Pharmacol, 80: 1447–1457. doi: 10.1111/bcp.12709.
References
- 1. Helmick CG, Felson DT, Lawrence RC, Gabriel S, Hirsch R, Kwoh CK, Liang MH, Kremers HM, Mayes MD, Merkel PA, Pillemer SR, Reveille JD. Stone JH and National Arthritis Data Workgroup. Estimates of the prevalence of arthritis and other rheumatic conditions in the united states. Part i. Arthritis Rheum 2008; 58: 15–25. [DOI] [PubMed] [Google Scholar]
- 2. Siegel J. Comparative effectiveness of treatments for rheumatoid arthritis. Ann Intern Med 2008; 148: 162–3. [DOI] [PubMed] [Google Scholar]
- 3. Kim SY, Solomon DH. Use of administrative claims data for comparative effectiveness research of rheumatoid arthritis treatments. Arthritis Res Ther 2011; 13: 129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Greenberg JD, Reed G, Decktor D, Harrold L, Furst D, Gibofsky A, Dehoratius R, Kishimoto M, Kremer JM. A comparative effectiveness study of adalimumab, etanercept and infliximab in biologically naive and switched rheumatoid arthritis patients: Results from the US CORRONA registry. Ann Rheum Dis 2012; 71: 1134–42. [DOI] [PubMed] [Google Scholar]
- 5. Institute of Medicine . Initial national priorities for comparative effectiveness research. Washington, DC: Institute of Medicine, 2009. [Google Scholar]
- 6. Weinblatt ME, Schiff M, Valente R, van der Heijde D, Citera G, Zhao C, Maldonado M, Fleischmann R. Head‐to‐head comparison of subcutaneous abatacept versus adalimumab for rheumatoid arthritis. Arthritis Rheum 2012; 73: 86–94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kavanaugh A, Emery P, van Vollenhoven RF, Dikranian AH, Alten R, Klearman M, Musselman D, Agarwal S, Green J, Gabay C. Tocilizumab monotherapy compared with adalimumab monotherapy in patients with rheumatoid arthritis: Results of a 24‐week study. Arthritis Rheum 2012; 64: S333–4. [Google Scholar]
- 8. Gabay C, Emery P, van Vollenhoven R, Dikranian A, Alten R, Pavelka K, Klearman M, Musselman D, Agarwal S, Green J, Kavanaugh A, on behalf of the ADACTA study investigators . Tocilizumab monotherapy versus adalimumab monotherapy for treatment of rheumatoid arthritis (ADACTA): A randomised, double‐blind, controlled phase 4 trial. Lancet 2013; 381: 1541–50. [DOI] [PubMed] [Google Scholar]
- 9. Weaver AL, Lautzenheiser RL, Schiff MH, Gibofsky A, Perruquet JL, Luetkemeyer J, Paulus HE, Xia HA, Leff JA. Real‐world effectiveness of select biologic and DMARD monotherapy and combination therapy in the treatment of rheumatoid arthritis: Results from the Radius Observational Registry. Curr Med Res Opin 2006; 22: 185–98. [DOI] [PubMed] [Google Scholar]
- 10. Geborek P, Crnkic M, Petersson IF, Saxne T. Etanercept, infliximab, and leflunomide in established rheumatoid arthritis: Clinical experience using a structured follow up programme in southern Sweden. Ann Rheum Dis 2002; 61: 793–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hetland ML, Christensen IJ, Tarp U, Dreyer L, Hansen A, Hansen IT, Kollerup G, Linde L, Lindegaard HM, Poulsen UE, Schlemmer A, Jensen DV, Jensen S, Hostenkamp G, Ostergaard M, All Departments of Rheumatology in Denmark . Direct comparison of treatment responses, remission rates, and drug adherence in patients with rheumatoid arthritis treated with adalimumab, etanercept, or infliximab: Results from eight years of surveillance of clinical practice in the nationwide Danish DANBIO registry. Arthritis Rheum 2010; 62: 22–32. [DOI] [PubMed] [Google Scholar]
- 12. Greenwald LM. Medicare part D data: Major changes on the horizon. Med Care 2007; 45: S9–12. [DOI] [PubMed] [Google Scholar]
- 13. Yun H, Kilgore ML, Curtis JR, Delzell E, Gary LC, Saag KG, Morrisey MA, Becker DJ, Matthews R, Smith W, Locher JL. Identifying types of nursing facility stays using medicare claims data: An algorithm and validation. Health Serv Outcomes Res Method 2010; 10: 100–10. [Google Scholar]
- 14. Roland M, Torgerson DJ. What are pragmatic trials? BMJ 1998; 316: 285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Schneeweiss S. Sensitivity analysis and external adjustment for unmeasured confounders in epidemiologic database studies of therapeutics. Pharmacoepidemiol Drug Saf 2006; 15: 291–303. [DOI] [PubMed] [Google Scholar]
- 16. Luce BR, Kramer JM, Goodman SN, Connor JT, Tunis S, Whicher D, Schwartz JS. Rethinking randomized clinical trials for comparative effectiveness research: The need for transformational change. Ann Intern Med 2009; 151: 206–9. [DOI] [PubMed] [Google Scholar]
- 17. Greenberg JD, Reed G, Decktor D, Harrold L, Furst D, Gibofsky A, Dehoratius R, Kishimoto M, Kremer JM, CORRONA Investigators . A comparative effectiveness study of adalimumab, etanercept and infliximab in biologically naive and switched rheumatoid arthritis patients: Results from the US CORRONA registry. Ann Rheum Dis 2012; 71: 1134–42. [DOI] [PubMed] [Google Scholar]
- 18. Soliman MM, Hyrich KL, Lunt M, Watson KD, Symmons DP, Ashcroft DM, British Society for Rheumatology Biologics Register . Rituximab or a second anti‐tumor necrosis factor therapy for rheumatoid arthritis patients who have failed their first anti‐tumor necrosis factor therapy? Comparative analysis from the British Society for Rheumatology Biologics Register. Arthritis Care Res (Hoboken) 2012; 64: 1108–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Soliman MM, Hyrich KL, Lunt M, Watson KD, Symmons DP, Ashcroft DM, British Society for Rheumatology Biologics Register . Effectiveness of rituximab in patients with rheumatoid arthritis: Observational study from the British Society for Rheumatology Biologics Register. J Rheumatol 2012; 39: 240–6. [DOI] [PubMed] [Google Scholar]
- 20. Arenere Mendoza M, Manero Ruiz FJ, Carrera Lasfuentes P, Navarro Aznarez H, Pecondon Espanol A, Rabanaque Hernandez MJ. [Tumour necrosis factor alpha antagonists in established rheumatoid arthritis: Effectiveness comparative study]. Med Clin 2010; 134: 665–70. [DOI] [PubMed] [Google Scholar]
- 21. Kievit W, Adang EM, Fransen J, Kuper HH, van de Laar MA, Jansen TL, De Gendt CM, De Rooij DJ, Brus HL, Van Oijen PC, Van Riel PC. The effectiveness and medication costs of three anti‐tumour necrosis factor alpha agents in the treatment of rheumatoid arthritis from prospective clinical practice data. Ann Rheum Dis 2008; 67: 1229–34. [DOI] [PubMed] [Google Scholar]
- 22. Hyrich KL, Watson KD, Silman AJ, Symmons DP. Predictors of response to anti‐TNF‐{alpha} therapy among patients with rheumatoid arthritis: Results from the British Society for Rheumatology Biologics Register. Rheumatology (Oxford) 2006; 45: 1559‐65. [DOI] [PubMed] [Google Scholar]
- 23. Wu E, Chen L, Birnbaum H, Yang E, Cifaldi M. Retrospective claims data analysis of dosage adjustment patterns of tnf antagonists among patients with rheumatoid arthritis. Curr Med Res Opin 2008; 24: 2229–40. [DOI] [PubMed] [Google Scholar]
- 24. Moots RJ, Haraoui B, Matucci‐Cerinic M, van Riel PL, Kekow J, Schaeverbeke T, Davis A, Tedeschi MA, Freundlich B, Chang DJ, Singh A. Differences in biologic dose‐escalation, non‐biologic and steroid intensification among three anti‐tnf agents: Evidence from clinical practice. Clin Exp Rheumatol 2011; 29: 26–34. [PubMed] [Google Scholar]
- 25. Etemad L, Yu EB, Wanke LA. Dose adjustment over time of etanercept and infliximab in patients with rheumatoid arthritis. Manag Care Interface 2005; 18: 21–7. [PubMed] [Google Scholar]
- 26. Curtis JR, Baddley JW, Yang S, Patkar N, Chen L, Delzell E, Mikuls TR, Saag KG, Singh J, Safford M, Cannon GW. Derivation and preliminary validation of an administrative claims‐based algorithm for the effectiveness of medications for rheumatoid arthritis. Arthritis Res Ther 2011; 13: R155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Curtis JR, Chastek B, Becker L, Harrison DJ, Collier D, Yun H, Joseph GJ. Further evaluation of a claims‐based algorithm to determine the effectiveness of biologics for rheumatoid arthritis using commercial claims data. Arthritis Res Ther 2013; 15: 404. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1 Rule‐out sensitivity analysis for unmeasured confounder.
Table S1 Components of the effectiveness algorithm† for adalimumab, etanercept, infliximab and abatacept at one year * among patients who had rheumatologists visits during 10‐14 months of follow up.
Supporting info item


