Summary
The aim of this study was to evaluate the histopathological and apoptotic changes occurring in the rat ipsilateral and contralateral testes, after experimental spermatic cord torsion, and to explore and the role of poly(ADP‐ribose) polymerase (PARP) cleavage in testicular torsion–detorsion injury. A total of 37 Wistar albino rats were subjected to 720° unilateral spermatic cord torsion for 1, 2 and 4 h, followed by 4‐h reperfusion, or else to a sham operation (control group). Histology of the testicle was evaluated using haematoxylin–eosin (H&E) staining and Johnsen's scoring system. Germ cell apoptosis was evaluated via active caspase‐3 immunostaining, and PARP expression levels were evaluated via Western blotting. The mean Johnsen's tubular biopsy scores (JTBS) of the ipsilateral testicles were lower for all torsion groups than for the controls (P < 0.05), but the JTBS of the contralateral testicles were only lower in the 4‐h torsion group (P < 0.05). The mean apoptosis score (AS) of the ipsilateral and contralateral testicles was significantly higher in the torsion groups than in the sham group. AS increased correlatively with torsion time, in both testicles. The effect of testicular torsion on PARP cleavage was time dependent, with the highest effect observed after 4 h of testicular torsion (P < 0.05). Testicular torsion caused time‐dependent histological changes, apoptosis and increases in PARP cleavage. Our results suggest that testicular torsion–detorsion injury caused cell damage and germ cell apoptosis that apparently involved cleavage of PARP. Increased PARP cleavage could, in turn, lead to enhanced apoptosis.
Keywords: apoptosis, poly(ADP‐ribose) polymerase (PARP), testis torsion
Testicular torsion is a serious urological emergency in which misdiagnosis and inappropriate treatment can lead to male infertility (Ramachandra et al. 2015). Events during testicular torsion and detorsion are similar to ischaemia–reperfusion (I/R) injuries observed in other organs. The two most important factors determining testicular damage are the exposure time and the degree torsion of the spermatic cord (Cosentino et al. 1986; Akgur et al. 1994). In vivo data have revealed that a 720° torsion induces ischaemia and that a 1‐h duration of this torsion followed by repair of torsion results in the permanent loss of spermatogenesis which clinicians may encounter in clinic conditions (Turner & Brown 1993).
Reperfusion is one of the most important factors determining further injury in cases of torsion, as the damage from reperfusion is usually more severe than that induced by ischaemia. Several mechanisms are involved in the development of testicular damage following torsion and detorsion (Lysiak et al. 2000). Recently, it was shown that a 1‐h and 720° testicular torsion in the rat model led to germ cell‐specific apoptosis as assessed by in situ TUNEL and by DNA laddering. This increase in apoptosis was noted 3–4 h after torsion repair (Turner et al. 1997; Uyetürk et al. 2013, Mestrovic et al. 2014). An I/R injury in the testis induces germ cell‐specific apoptosis attributable to increases in nitric oxide (NO) and reactive oxygen species (ROS) such as superoxide anions, hydroxyl radicals and hydrogen peroxide, primarily in the spermatogenic cells of the basal compartment of the seminiferous epithelium.
The NO and ROS, which are pro‐inflammatory factors, are generated from reperfusing leucocytes, including neutrophils and haematogenous macrophages, and these infiltrates occur in the interstitial spaces surrounding damaged tubules (Lysiak et al. 2001, 2003). Under physiological conditions, the harmful effects of free radicals are balanced by the endogenous anti‐oxidant system. However, when ROS generation exceeds the capacity of the defence mechanisms, emerging oxidative stress causes (reversible or irreversible) cell injury.
Poly(ADP‐ribose) polymerase [PARP; also known as poly(ADP‐ribose) synthetase (PARS) and poly(ADP‐ribose) transferase (pPADPRT)] is a preserved nuclear enzyme, present throughout the phylogenetic spectrum. The precise physiologic role of PARP is to induce DNA repair and maintain the genomic integrity (de Murcia et al. 1994; Schreiber et al. 1995). PARP activation has also been proposed to represent a cell elimination pathway for the removal of severely damaged cells (Sims & Benjamin 1987). Besides the physiological functions, PARP activation has also been identified as a key pathway in various pathophysiological conditions and disease states.
PARP has a complex role in cell death induced by DNA damage. Much of the cell death‐related literature focuses on PARP cleavage (as opposed to PARP activation), and PARP cleavage by caspases is a marker of apoptotic cell death. Recent experimental evidence shows that I/R generates free radicals and oxidant species, which, in turn, cause DNA injury and activate a cellular suicidal cascade triggered by PARP activation.
This study aimed to evaluate the testicular biopsy scores, apoptosis and PARP cleavage in rats exposed to testicular torsion–detorsion. We also investigated the association of these values with the presence of histological alterations in the contralateral testicle after unilateral testicular torsion.
Materials and methods
Animals and ethical approval
The study was approved by the Ethical Committee for Animal Research of Suleyman Demirel University and was conducted in accordance with the institutional guidelines and EC Directive 86/609/EEC for animal experiment [European council, 86/609/EEC] (Ethical approval number: 23/02/2010‐5‐09). Thirty‐seven adult male Wistar albino rats weighing between 190 and 220 g were maintained on a 12‐h light/dark cycle and fed ad libitum.
Surgical procedure
Rats were randomly divided into 4 groups as (i) sham operated (n = 7), (ii) 1‐h torsion (n = 10), (iii) 2‐h torsion (n = 10) and (iv) 4‐h torsion (n = 10). All surgical procedures were performed under sterile conditions with ketamine/xylazine anaesthesia (100/10 mg/kg) administered intraperitoneally before operating on each rat. The depth of anaesthesia was observed by finger pinch response and palpebral reflex. The dosage was determined according to Ethical Committee of Suleyman Demirel University and literature (Nazıroğlu et al. 2015). Ketamine was purchased from Pfizer, Istanbul, Turkey, and xylazine was purchased from Egevet, Izmir, Turkey.
In the sham group, the left testis was extracted through the scrotal incision and immediately returned to the scrotal sac. After 4 h, bilateral orchiectomy was performed. In the torsion–detorsion groups (1, 2 and 4 h), the left testis was exposed through a midline incision. Gubernaculum was divided, and the testes freed from its longitudinal and distal pole attachments. Torsion was created by rotating the left testis 720° clockwise and maintained by fixing the testis to the scrotal pouch with a 4.0 silk suture placed through the dartos and tunica albuginea. The incisions were closed, and the testes were left rotated for 1, 2 or 4 h. At the designated time, fixing sutures were cut; testes were counter‐rotated back to the natural positions and reinserted into the scrotum. The wound was closed again via 4.0 silk sutures. Following 4 h of reperfusion, bilateral orchiectomy was performed and the rats were sacrificed by ketamine/xylazine overdose.
Histological analyses
Half of the each testis was fixed in 4% paraformaldehyde (Merck, Darmstadt, Germany) with phosphate‐buffered saline (PBS) (Merck), washed, dehydrated and cleared in xylenes. Tissues embedded in paraffin were cut into 4‐ to 5‐μm sections and then stained with haematoxylin–eosin (H&E) (Merck). The mean testicular biopsy score was graded by Johnsen's scoring system (JTBS). Briefly, randomly selected 10 tubules were evaluated in each slide and a score of 1 to 10 was given to each tubule according to the existence of spermatogonia, spermatocytes, etc. (i.e. 1 for complete absence of cells while 10 for complete set of spermatogenic cells with normal appearance).
While no seminiferous epithelium is evaluated as score 1, complete spermatogenesis with many spermatozoa present is evaluated as score 10 (Dieckmann et al. 2007). Testicular spermatogenesis was evaluated by measuring mean testicular biopsy score.
Detection of apoptosis
Slides for immunohistochemistry, were rehydrated and quenched in 3% H2O2 (Thermo Scientific, Fremont, CA, USA). Heat‐activated antigen retrieval was performed in Tris‐ethylenediaminetetraacetic acid (EDTA) buffer (Merck) at pH 6.0. Non‐specific binding was eliminated via Ultra V Block (Thermo Scientific). One of the sections in each slide was stained with rabbit active caspase‐3 antibody (Abcam, Cambridge, MA. USA. Cat. # ab44976), while second section was stained with goat anti‐polyvalent solution (Thermo) instead of primary antibody as control for non‐specific reactions. Tissues were incubated with primary antibodies at +4°C overnight within a humidified chamber. Goat anti‐polyvalent solution (Thermo Scientific, Waltham, MA, USA) was used as secondary antibody. 3,3′‐Diaminobenzidine (DAB) staining was performed with UltraVision Plus Large Volume Detection Kit (Thermo Scientific), and slides were counterstained with haematoxylin. Tubules examined under Olympus BX51 light microscope (Olympus Optical Co., Ltd., Tokyo, Japan) were evaluated according to semiquantitative method (McCarty et al. 1986), which is adapted to testes slides (Gunduz et al. 2009). The number of counted spermatogenic cells was increased to 100 for each animal for the study. Caspase‐3‐positive cells per 100 spermatogenic cells were determined.
Western blot analysis
One‐dimensional sodium dodecyl sulphate (SDS) electrophoresis was performed with a 4–12% gradient Tris–glycine. Separated proteins were then electrophoretically transferred, for 2 h at 0.8 mA/cm2,, in a semidry blotter onto nitrocellulose membrane for subsequent probing. Blot membranes were incubated overnight with 5% (w/v) non‐fat dry milk in Tris‐buffered saline with 0.1% Tween‐20 (TBST) to block residual protein binding sites. Blocked membranes were then incubated first for 2 h with the anti‐poly(ADP‐ribose) polymerase (PARP) antibody (46D11; from rabbit, Cell Signaling Technology, Beverly, MA, USA) and the anti‐β‐actin antibody (8H10D10; from mouse, Cell Signaling Technology) diluted 1:1000 in TBST. The primary antibody was removed and blots were washed three times for 10 min each with TBST. To detect the primary antibodies, blots were incubated with the appropriate horseradish peroxidase‐conjugated anti‐IgG antibody diluted 1:5000 in 2.5% (w/v) non‐fat dry milk in TBST, washed three times in TBST and exposed to enhanced chemiluminescence reagents for 5 min. Blots were then exposed to photographic films, and the optical density was estimated using scanning densitometry (Espino et al. 2010).
Statistical analysis
Statistical analyses were performed by GraphPad Instant Tm program on Windows(TM) (GraphPad Instant 3, GraphPad Software, Inc, CA, USA). Data were expressed as means ± standard deviation (SD) of the numbers of determinations. To compare the different treatments, statistical significance was calculated by Mann–Whitney U‐test and one‐way analysis of variance followed by the Tukey's multiple comparison tests. P < 0.05 was considered to indicate a statistically significant difference.
Results
Mean JTBS and apoptosis score (AS) values for all groups after 4 h of detorsion are shown in Table 1. The mean testicular biopsy scores in the ipsilateral testes of all torsion–detorsion groups were significantly lower than those of the sham group (P < 0.05). The JTBS of contralateral testes were also significantly lower in the 4‐h torsion group than in the sham group (P < 0.05), whereas no significant differences were observed between the contralateral testes of other torsion groups (1 and 2 h) and the sham group (P > 0.05). Active caspase‐3 staining of the testis sections revealed very few (0.79 ± 0.17) positive cells in the sham‐operated animals (Figure. 2). However, sections taken 4 h after the repair of torsion in all torsion–detorsion groups showed significantly increased numbers of apoptotic cells (P < 0.05) (Table 1; Figure. 2). The contralateral testicles also exhibited significantly higher AS values in all torsion groups than in the sham group (P < 0.05). Among the torsion groups, AS increased with torsion time in both the ipsilateral and contralateral testicles. A statistically significant difference was observed between the AS of ipsilateral and contralateral testicles in all torsion groups.
Table 1.
Mean values of JTBS and apoptosis in the ipsilateral and contralateral testicles
| JTBS ± SD | Apoptosis ± SD | ||||
|---|---|---|---|---|---|
| N | Ipsilateral | Contralateral | Ipsilateral | Contralateral | |
| Sham | 7 | 9.74 ± 0.15 | – | 0.79 ± 0.17 | – |
| One hour | 10 | 9.18 ± 0.42a | 9.62 ± 0.15 | 3.18 ± 1.31a, b | 1.50 ± 0.11a |
| Two hours | 10 | 8.66 ± 0.85a | 9.46 ± 0.16 | 5.13 ± 0.51a, b | 2.11 ± 0.22a |
| Four hours | 10 | 7.82 ± 0.96a | 9.36 ± 0.17a | 6.50 ± 0.86a, b | 2.59 ± 0.17a |
JTBS, Johnsen's tubular biopsy scores; SD, Standard deviation.
Value significantly different from that of the control group (P < 0.05).
Value significantly different from that of contralateral testis in the same group (P < 0.05).
PARP cleavage was analysed using a specific monoclonal anti‐PARP antibody, which detects the total full‐length form (116 kDa) and also the large fragment (89 kDa) produced by caspase cleavage. Cleaved PARP was not observed or was virtually negligible in both testes of the control group rats (sham group) and the contralateral testes of the torsion group rats. Nevertheless, PARP cleavage was detected in lysates from the testicular tissues of rats subjected to testicular torsion (Figure. 1a). The effect of testicular torsion on PARP cleavage was time dependent, with the highest effect being achieved after 4 h of testicular torsion (Figure. 1b, P < 0.05).
Figure 1.
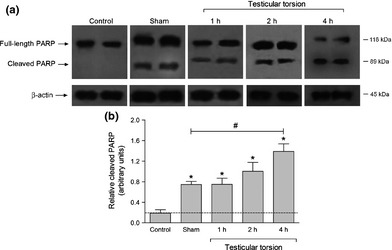
Testicular torsion induces poly(ADP‐ribose) polymerase (PARP) cleaving in rat testes. (a) To determine PARP cleaving, testes were lysed and then subjected to gradient Tris–glycine isolation and subsequent Western blotting with a specific anti‐PARP (46D11) antibody and reprobed with anti‐β‐actin (8H10D10) antibody for protein loading control. Cleaved PARP was not observed in testes of control rats. In rats subjected to testicular torsion (1–4 h), PARP cleaving was detected in lysates from testicular tissue. Sham rats were used as positive control. (b) Histograms represent the relative amount of cleaved PARP expressed as arbitrary units. Values are presented as mean ± SD of the number of animals. *P < 0.05 regarding control animals. # P < 0.05 regarding sham animals. Control group also means contralateral testes. PARP: poly(ADP‐ribose) polymerase. SD: Standard deviation.
Discussion
Testicular torsion is a medical emergency that usually requires surgical intervention to allow reperfusion of the affected testis. Current management for the preservation of spermatogenesis and fertility is detorsion following early diagnosis. The recovery rate is inversely proportional to the duration of torsion. Although reperfusion is essential for the survival of ischaemic tissue, the main pathophysiology of testicular torsion is ischaemia–reperfusion injury of the testes caused by the release of the twisted spermatic cord. Despite the return of blood flow after testis detorsion, spermatogenesis loss is still observed (Anderson & Williamson 1986). Improved knowledge of the pathophysiologic cascade initiated after testis detorsion will increase the effectiveness of treatment approaches. In the present study, we have investigated the histopathological changes, apoptosis and PARP activation in a torsion–detorsion rat model.
The experimental model used in this study to induce I/R by testicular torsion was described by Ryan et al. (Ryan et al. 1988). The target rats were subjected to 720° unilateral spermatic cord torsion for 1, 2 and 4 h followed by 4‐h reperfusion or sham operation. The time of ischaemia was set at 1–4 h. According to Akgür et al. (1993), when ischaemia duration exceeds 6 h, the reperfusion injury does not occur (Akgür et al. 1993). Periods of ischaemia longer than 4–6 h result in permanent tissue injury. The increase in apoptosis was noted 4 h after torsion repair in rats (Turner & Brown 1993).
ROS can arise in reperfusing tissues from parenchymal cells or from leucocytes that first adhere to the reperfusing venule wall before diapedesing into the tissue itself. Significant leucocyte adhesion in testicular subtunical venules is observed 4 h after the initiation of reperfusion. The margination of leucocytes and diapedesis in subtunical venules occurs 4 h after torsion repair, providing a potential source of increased ROS activity in the testis. It is also from 4 h after torsion repair that there is a significant increase in lipid peroxidation, a known effect of ROS exposure.
Germ cell apoptosis is stimulated contemporaneously by the margination and diapedesis of leucocytes as is an increase in intratesticular oxidative damage. Turner et al. (1997) showed that 1‐h torsion with reperfusion increased apoptosis as early as 4 h after torsion repair. They observed a significant increase in the maximum and mean numbers of apoptotic nuclei per tubule as well as the percentages of tubules with apoptotic nuclei at this time. In the light of these findings, we subjected the rats in the present study to 720° unilateral spermatic cord torsion for 1, 2 and 4 h followed by 4‐h reperfusion. A 1‐h, 720° torsion was sufficient to induce apoptosis in the ipsilateral and contralateral testicles, while 2‐ and 4‐h torsion further increased the induction of apoptosis (in both testicles). The highest increase was achieved after 4‐h torsion (Table 1). The trend towards an increase in germ cell apoptosis 4 h after torsion repair supports the previous data from Turner & Brown (1993), Turner et al. (1997) and Lysiak et al. (2000) who detected significant increases in germ cell apoptosis 4 h after torsion repair. Here, AS had increased in all torsion–detorsion groups (1, 2, 4 h) 4 h after torsion repair in both the ipsilateral and contralateral testicles (P < 0.05) (Table 1; Figure. 2). Among the torsion groups, AS increased with torsion time in both the ipsilateral and contralateral testicles. AS was higher in the ipsilateral testicle than in the contralateral testicle for all torsion groups (P < 0.05) (Table 1). Our results show that AS is a useful and sensitive marker to evaluate pathologies in both testicles in the testicular I/R rat model.
Figure 2.
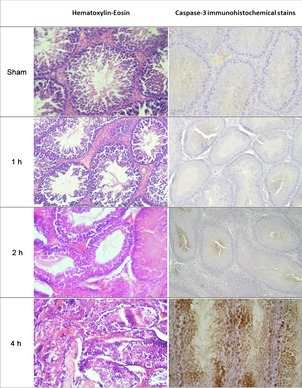
Representative photographs of haematoxylin–eosin (H&E) (left column) and active caspase‐3 immunohistochemical (IHC) (right column) staining of four groups. H&E slides showed minor to serious damage at the seminiferous tubules, haemorragia at the interstitial area and loss of spermatogenic cells all increasing with time. Active caspase‐3 immunohistochemical staining clearly demonstrates apoptotic cells, stained as dark brown, increased to high numbers in some animals, especially at the 4‐h torsion group. (Magnification 240 X).
Rat germ cell apoptosis following torsion and torsion repair is likely initiated through two separate apoptotic pathways (Lysiak et al. 2000; Richburg et al. 2000). One pathway involves Bax, which causes cytochrome c release from mitochondria. This activates caspase‐9 and the subsequent caspase cascade, leading to DNA degradation. The second pathway involves FasL binding to Fas and its cell surface receptor and the initiation of the apoptosis cascade via caspase‐8.
The effects of unilateral torsion on the contralateral testis are controversial; ipsilateral torsion has been reported to cause no damage to the contralateral testicle in rats (Turner 1987; Bozlu et al. 2003). However, some studies have demonstrated that ipsilateral torsion resulted in contralateral testicular damage in rabbits (Tanyel et al. 1989), rats (Sade et al. 1988) and humans (Hadziselimovic et al. 1998). In this study, we demonstrated that ipsilateral testicular torsion led to histological changes in the contralateral testis, but only after 4 h of torsion, and not before, which is consistent with previous findings. Pro‐inflammatory factors, secreted from reperfusing leucocytes, can infiltrate into the interstitial spaces surrounding damaged tubules (Lysiak et al. 2001, 2003), and these factors may be responsible for the observed damage to the contralateral testis.
Because PARP is assumed to be an important enzyme in DNA repair, its cleavage would be expected to lead to enhanced apoptosis. Depending on the severity of DNA damage, genotoxic stimuli can trigger three different pathways (Virag & Szabo 2002). In the case of mild DNA damage, PARP facilitates DNA repair and thus promotes cell survival. Moderate DNA damage induces apoptotic cell death by the activation of caspases which inactivates PARP by cleaving it into two fragments (p89 and p24). This pathway allows cells with irreparable DNA damage to be safely eliminated. Severe DNA damage may cause excessive PARP activation and depletion of NAD+ and ATP stores; this depletion blocks apoptosis and results in necrosis (Szabo et al. 2004).
In the present study, PARP cleavage was analysed using a specific monoclonal anti‐PARP antibody. As shown in Figure 1, PARP cleavage was detected in lysates from the testicular tissue of rats subjected to testicular torsion. The effect of testicular torsion on PARP cleavage was time dependent with the highest effect achieved after 4 h of testicular torsion. In our study, we maintained torsion time at a medium range (1–4 h) followed by moderate detorsion period (4 h), and we found that apoptosis increased in both testicles and PARP cleavage increased in the ipsilateral testicles. Although no increase was noted in PARP cleavage in the contralateral testicles, apoptosis in the contralateral testes did increase. Induction of apoptosis in the contralateral testicles may be attributed to factors other than activation of PARP. Nevertheless, the activation of PARP may play a role in the testicular injury of ipsilateral testicles due to torsion–detorsion.
Administration of PARP inhibitors has shown possible benefits in a torsion–detorsion model of testis (Johnsen 1970; Schreiber et al. 1995; Virag & Szabo 2002). Bozlu et al. (2004) showed that PARP may have a role in the testicular damage caused by I/R. Administration of PARP inhibitors before reperfusion in a torsion–detorsion model of testis indicates a potential for decreasing the long‐term histological damage that occurs after testicular torsion. Kar et al. showed that nicotinamide as a PARP inhibitor may successfully decrease the tissue damage due to ischaemia–reperfusion injury in the early and late periods in both the ipsilateral and contralateral testicles (Kar et al. 2010).
In support of these findings, our study showed that testicular torsion–detorsion caused cell damage, increased PARP cleavage and promoted apoptosis in a time‐dependent manner. Our results suggest that testicular torsion–detorsion injury caused germ cell apoptosis by the induction of PARP cleavage. The increase in PARP cleavage could, in turn, lead to enhanced apoptosis. Therefore, our model can be used to simulate I/R damage in rat testes in a period as short as 4 h.
Conflict of interest
None of the authors have any conflicts to disclose. All authors approved the final manuscript.
Acknowledgements
PAK and AK formulated the present hypothesis and were also responsible for writing the report. JE, ACU and BC were responsible for WB analysis. HD was responsible for immunohistochemistry. HT and IO were responsible for the induction of animal model. ABR made critical revision to the manuscript. The current study was partially supported by The Scientific Research Unit of Suleyman Demirel University (SDU‐BAP‐2174‐TU‐10).
References
- Akgur F.M., Kilinc K., Tanyel F.C., Buyukpamukcu N. & Hicsonmez A. (1994) Ipsilateral and contralateral testicular biochemical acute changes after unilateral testicular torsion and detorsion. Urology 44, 413–418. [DOI] [PubMed] [Google Scholar]
- Akgür F.M., Kılınç K. & Aktuğ T. (1993) Reperfusion injury after detorsion of unilateral testicular torsion. Urol. Res. 21, 395–399. [DOI] [PubMed] [Google Scholar]
- Anderson J.B. & Williamson R.C. (1986) The fate of the human testes following unilateral torsion of the spermatic cord. Br. J. Urol. 58, 698–704. [DOI] [PubMed] [Google Scholar]
- Bozlu M., Eskandari G., Cayan S., Canpolat B., Akbay E. & Atik U. (2003) The effect of poly (adenosine diphosphate‐ribose) polymerase inhibitors on biochemical changes in testicular ischemia‐reperfusion injury. J. Urol. 169, 1870–1873. [DOI] [PubMed] [Google Scholar]
- Bozlu M., Coskun B., Cayan S. et al (2004) Inhibition of poly(adenosine diphosphate‐ribose) polymerase decreases long‐term histologic damage in testicular ischemia‐reperfusion injury. Urology 63, 791–795. [DOI] [PubMed] [Google Scholar]
- Cosentino M.J., Nishida M., Rabinowitz R. & Cockett A.T. (1986) Histopathology of prepubertal rat testes subjected to various durations of spermatic cord torsion. J. Androl. 7, 23–31. [DOI] [PubMed] [Google Scholar]
- Dieckmann K.P., Linke J., Pichlmeier U., Kulejewski M. & Loy V. (2007) German Testicular Cancer Study Group: spermatogenesis in the contralateral testis of patients with testicular germ cell cancer: histological evaluation of testicular biopsies and a comparison with healthy males. BJU Int. 99, 1079–1085. [DOI] [PubMed] [Google Scholar]
- Espino J., Bejarano I., Redondo P.C. et al (2010) Melatonin reduces apoptosis induced by calcium signaling in human leukocytes: evidence for the involvement of mitochondria and Bax activation. J. Membr. Biol. 233, 105–118. [DOI] [PubMed] [Google Scholar]
- Gunduz B., Karakas A., Terzi H., Oner J., Serin E. & Kukner A. (2009) The effect of pinealectomy and leptin hormone on the proliferation and apoptosis activation in Syrian hamster testis in different photoperiods. Int. J. Androl. 32, 343–352. [DOI] [PubMed] [Google Scholar]
- Hadziselimovic F., Geneto R. & Emmons L.R. (1998) Increased apoptosis in the contralateral testes of patients with testicular torsion as a factor for infertility. J. Urol. 160, 1158–1160. [DOI] [PubMed] [Google Scholar]
- Johnsen S.G. (1970) Testicular biopsy score count–a method for registration of spermatogenesis in human testes: normal values and results in 335 hypogonadal males. Hormones 1, 2–25. [DOI] [PubMed] [Google Scholar]
- Kar A., Ozden E., Yakupoglu Y.K., Kefeli M., Sarikaya S., Yilmaz A.F.. (2010). Experimental unilateral spermatic cord torsion: the effect of polypolymerase enzyme inhibitor on histopathological and biochemical changes in the early and late periods in the ipsilateral and contralateral testicles. Urology 76, 507.e1‐507.e5. [DOI] [PubMed] [Google Scholar]
- Lysiak J.J., Turner S.D. & Turner T.T. (2000) Molecular pathway of germ cell apoptosis following ischemia/reperfusion of the rat testis. Biol. Reprod. 63, 1465–1472. [DOI] [PubMed] [Google Scholar]
- Lysiak J.J., Turner S.D., Nguyen Q.A., Singbartl K., Ley K. & Turner T.T. (2001) Essential role of neutrophils in germ cell‐specific apoptosis following ischemia/reperfusion injury of the mouse testis. Biol. Reprod. 65, 718–725. [DOI] [PubMed] [Google Scholar]
- Lysiak J.J., Nguyen Q.A., Kirby J.L. & Turner T.T. (2003) Ischemia‐reperfusion of the murine testis stimulates the expression of proinflammatory cytokines and activation of c‐jun N‐terminal kinase in a pathway to E‐selectin expression. Biol. Reprod. 69, 202–210. [DOI] [PubMed] [Google Scholar]
- McCarty K.S. Jr, Szabo E., Flowers J.L. et al (1986) Use of a monoclonal anti‐estrogen receptor antibody in the immunohistochemical evaluation of human tumors. Cancer Res. 46, 4244–4248. [PubMed] [Google Scholar]
- Mestrovic J., Drmic‐Hofman I., Pogorelic Z. et al (2014) Beneficial effect of nefedipine on testicular torsion‐detorsion injury in rats. Urology 84, 1194–1198. [DOI] [PubMed] [Google Scholar]
- de Murcia G., Schreiber V., Molinete M. et al (1994) Structure and function of poly(ADP‐ribose) polymerase. Mol. Cell. Biochem. 138, 15–24. [DOI] [PubMed] [Google Scholar]
- Nazıroğlu M., Çelik Ö., Uğuz A.C. & Bütün A. (2015) Protective effects of riboflavin and selenium on brain microsomal Ca(2 + )‐ATPase and oxidative damage caused by Glyceryl Trinitrate in a rat headache model. Biol. Trace Elem. Res. 164, 72–79. [DOI] [PubMed] [Google Scholar]
- Ramachandra P., Palazzi K.L., Holmes N.M. & Marietti S. (2015) Factor influencing rate of testicular salvage in acute testicular torsion at a tertiary pediatric center. West J. Emerg. Med. 16, 190–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richburg J.H., Nanez A., Williams L.R., Embree M.E. & Boekelheide K. (2000) Sensitivity of testicular germ cells to toxicant‐induced apoptosis ingld mice that express a nonfunctional form of Fas ligand. Endocrinology 141, 787–793. [DOI] [PubMed] [Google Scholar]
- Ryan P.C., Gorey T.F. & Fitzpatrick J.M. (1988) Experimental testicular torsion:fixation without parenchymal trauma. Eur. Urol. 14, 141–144. [DOI] [PubMed] [Google Scholar]
- Sade M., Amato S., Buyuksu C., Mertan S., Canda M.S. & Kaplanoglu N. (1988) The effect of testicular torsion on the contralateral testis and the value of various types of treatment. Br. J. Urol. 62, 69–71. [DOI] [PubMed] [Google Scholar]
- Schreiber V., Hunting D., Trucco C. et al (1995) A dominant‐negative mutant of human poly(ADP‐ribose) polymerase affects cell recovery, apoptosis, and sister chromatid exchange following DNA damage. Proc. Natl Acad. Sci. USA 92, 4753–4757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sims J.L. & Benjamin R.C. (1987) Alteration of poly(adenosine diphosphoribose) metabolism by ethanol: mechanism of action. Arch. Biochem. Biophys. 253, 357–366. [DOI] [PubMed] [Google Scholar]
- Szabo G., Liaudet L., Hagl S. & Szabo C. (2004) Poly(ADP‐ribose) polymerase activation in the reperfused myocardium. Cardiovasc. Res. 61, 471–480. [DOI] [PubMed] [Google Scholar]
- Tanyel F.C., Buyukpamukcu N. & Hicsonmez A. (1989) Contralateral testicular blood flow during unilateral testicular torsion. Br. J. Urol. 63, 522–524. [DOI] [PubMed] [Google Scholar]
- Turner T.T. (1987) On unilateral testicular and epididymal torsion: no effect on the contralateral testis. J. Urol. 138, 1285–1290. [DOI] [PubMed] [Google Scholar]
- Turner T.T. & Brown K.J. (1993) Spermatic cord torsion: loss of spermatogenesis despite return of blood flow. Biol. Reprod. 49, 401–407. [DOI] [PubMed] [Google Scholar]
- Turner T.T., Tung K.S., Tomomasa H. & Wilson L.W. (1997) Acute testicular ischemia results in germ cell‐specific apoptosis in the rat. Biol. Reprod. 57, 1267–1274. [DOI] [PubMed] [Google Scholar]
- Uyetürk U., Terzi E.H., Gucuk A., Kemahli E., Öztürk H. & Tosun M. (2013) Prevention of torsion‐induced testicular injury by Rhodiola rosea. Urology. 82 (1), 254–259. [DOI] [PubMed] [Google Scholar]
- Virag L. & Szabo C. (2002) The therapeutic potential of poly(ADP‐ribose) polymerase inhibitors. Pharmacol. Rev. 54, 375–429. [DOI] [PubMed] [Google Scholar]


