Abstract
Despite several advantages to bringing couples together to learn how to protect themselves and new-born children from the risk of HIV infection, most interventions are designed for individuals or groups, not for dyads. This meta-analysis provides a direct test of whether couple-based interventions are more effective in promoting HIV protective behaviors than interventions delivered to individuals. We conducted systematic searches of five electronic databases and 60 journals. Eligible studies were controlled trials or prospective cohort designs; evaluated a couple-based intervention compared to an individual-level intervention; assessed at least one HIV prevention outcome (e.g., protective sex, drug use, HIV testing, medication adherence, and sexually transmitted infections [STI]); and were published between 1988 and 2014. Fifteen interventions, including 21,882 participants from China, Kenya, Rwanda, Tanzania, Trinidad, Zambia, and the USA, were evaluated. The results of random-effects models showed statistically significant intervention effects for protective sex (OR = 1.60, 95% CI = 1.21, 2.11), HIV testing (OR = 1.79, 95% CI = 1.31, 2.45), and Nevirapine uptake (OR = 1.51, 95% CI = 1.02, 2.24). The evidence demonstrates the usefulness of couple-based interventions in protecting individuals, partners, and new-born children from the risk of HIV transmission and infection.
Keywords: HIV prevention, Couple-based, Systematic review, Meta-analysis, Intervention
INTRODUCTION
Sexual transmission of HIV continues to be the driving force of the epidemic in many parts of the world (UNAIDS, 2013). While a large proportion of HIV transmission takes place between two sexually intimate people, prevention efforts for heterosexuals, men who have sex with men (MSM), and people who use drugs have primarily focused on individuals or groups and typically have not included both members of a dyad (Jiwatram-Negron & El-Bassel, 2014; Meader et al., 2013; Purcell et al., 2014). There are several advantages to bringing couples together to learn how to protect themselves from HIV and other sexually transmitted infections (STIs) (El-Bassel & Wechsberg, 2012; Jiwatram-Negron & El-Bassel, 2014). It gives the couple the opportunity to learn and practice communication and negotiation skills together, facilitate disclosure of HIV serostatus and previous and current sexual risk and drug use behaviors in a safe environment, and foster a joint responsibility for preventing HIV and STI.
Additionally, couple-based voluntary HIV counseling and testing provides a shared knowledge base that, together with confirmation of serostatus, allows a couple to plan and make essential life decisions jointly about HIV treatment and reproductive health care (Jiwatram-Negron & El-Bassel, 2014). Acquiring partner’s support also facilitates adherence to HIV treatment (Langebeek et al., 2014; Sandelowski, Voils, Chang, & Lee, 2009). In the case of intimate couples becoming parents, involving fathers and incorporating their support in couple-based prevention of mother to child transmission may increase HIV testing among pregnant women and the uptake and adherence to Nevirapine among those who are tested positive for HIV (Kiarie, Kreiss, Richardson, & John-Stewart, 2003). Couple-based interventions have the potential for protecting not only individuals and partners, but also new-born children from the risk of HIV transmission and infection.
While a few published systematic reviews have evaluated couple-based interventions (Burton, Darbes, &Operario, 2010; Kennedy, Medley, Sweat, & O’Reilly, 2010; LaCroix, Pellowski, Lennon, & Johnson, 2013), none has directly tested whether couple-based interventions are more effective than interventions delivered to individuals in a relationship (referred to as individual-level interventions in this paper). In this systematic review and meta-analysis, we examine the effects of couple-based interventions that have been evaluated against individual-level interventions through experimental or cohort studies and provide estimates of the magnitude of couple-based intervention effects on HIV protective behaviors.
METHODS
Two content expert librarians conducted systematic, automated, and manual searches to locate relevant HIV intervention evaluation studies with behavioral or biologic outcomes. The automated searches consisted of five databases (and platforms): MEDLINE (OVID), EMBASE (OVID), PsycINFO (OVID), and CINAHL (EBSCOhost) and Sociological Abstracts (ProQuest). Two separate comprehensive searches were conducted: one for locating citations related to HIV/STI risk reduction and the other for locating citations related to HIV treatment and medication adherence. The full search strategy, including terms and key words, used for searching MEDLINE and other databases for each of the two comprehensive searches are available from the corresponding author. The manual search consisted of searching 60 journals to identify potentially relevant citations not yet indexed in electronic databases at the time when the comprehensive searches were conducted.
Studies were eligible if they were controlled trials or prospective cohort designs, evaluated a couple-based, HIV-prevention intervention with an individual-level comparison group, assessed at least one HIV prevention outcome (e.g., sex or drug use behavior, STI, HIV testing, HIV treatment uptake, and medication adherence), reported data sufficient for calculating effect sizes, and were published between January 1988 and December 2014.
Before abstracting data, we searched for linked citations that are supplementary publications offering additional information on the same study. Pairs of trained coders independently coded each eligible study (with linked citations) using standardized coding forms for study characteristics, participant characteristics, interventions, and outcomes. There was 95% agreement between coders across variables. Coding discrepancies were reconciled by coding pairs. We contacted the primary study investigator to obtain additional information as needed and the response rate was 85%.
Odds Ratios (OR) and corresponding variances were calculated to estimate effect sizes (Lipsey & Wilson, 2001). The magnitude of heterogeneity of the effect sizes was tested using the Q statistic and I2 statistic (Higgins, Thompson, Deeks, & Altman, 2003). The Windsorizing method was applied to adjust any extreme effect size that was three standard errors from the mean of all effect sizes (Lipsey & Wilson, 2001). Weighted effect sizes were combined using a random-effects model (Hedges & Vevea, 1998). Sensitivity tests were conducted by removing one study at a time to determine if any study affected the aggregated point estimate. An OR > 1 indicates a greater odds of protective behavior in the couple-based intervention relative to the individual-level comparison.
RESULTS
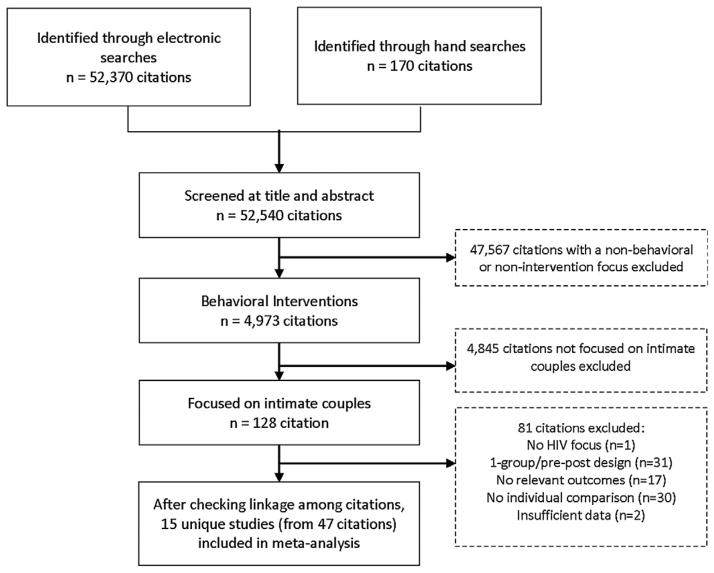
Figure 1 shows the flow of study selection. After screening titles, abstracts and full reports, 15 couple-based interventions, including 21,882 participants, met the inclusion criteria (Figure 1). As seen in Table 1, study locations included China, Kenya, Rwanda, Tanzania, Trinidad, Zambia, and the United States. All studies except two exclusively focused on heterosexual couples. Two studies were specifically designed for HIV-serodiscordant couples. Eight studies were randomized controlled trials.
Figure 1.
Study Selection
Table 1.
Description of 15 studies that evaluated the effects of couple-based interventions
| First Author, Publication Year | Location | Participants | Recruited from | Age | Relationship Status | Study Design |
|---|---|---|---|---|---|---|
| Allen et al., 1992 | Kigali, Rwanda | 1442 heterosexual women | Prenatal and pediatric outpatient clinics | Mean=29 years | Mean=8 years | Prospective cohort |
| Becker et al., 2010 | Dar es Salaam, Tanzania | 1,521 heterosexual women | Antenatal clinics | Mean=25 years | Married for at least 2 years | Randomized controlled trial |
| Conkling et al, 2010 | Kigali, Rwanda | 1,940 heterosexual women | Antenatal clinics | Mean=26 years | Mean=5 years | Prospective cohort |
| Conkling et al, 2010 | Lusaka, Zambia | 1,685 heterosexual women | Antenatal clinics | Mean=24 years | Mean=6 years | Prospective cohort |
| El-Bassel et al., 2003 | Bronx, New York City, USA | 217 heterosexual couples | Hospital-based outpatient clinics | Mean=38 years | Together for at least 6 months | Randomized controlled trial |
| El-Bassel et al., 2010 | Atlanta, Georgia; Los Angeles, California; New York, New York; Philadelphia, Pennsylvania, USA | 535 HIV-serodiscordant heterosexual couples | HIV care clinics, other health clinics, AIDS service organizations, community-based organizations, targeted street outreach, word of mouth, and various media outlets | Mean=43 years | Together for at least 6 months | Randomized controlled trial |
| El-Bassel et al., 2011 | New York, USA | 282 HIV-negative, drug-using, heterosexual couples | Street outreach, homeless-shelters, soup kitchens, syringe-exchange programs | Mean=37 years | Together for at least 6 months | Randomized controlled trial |
| Farquhar et al., 2004 | Nairobi, Kenya | 314 HIV-positive heterosexual women | Antenatal clinic | Mean=24 years | Mean=3.7 years | Prospective cohort |
| Jones et al., 2013 | Miami, Florida, USA | 216 heterosexual couples | Community health centers, community agencies and non-governmental organizations and churches | Mean=45 years | Together for at least 6 months | Randomized controlled trial |
| Khoshnood et al., 2006 | Urumqi City, Xinjiang Province, China | 300 heterosexual couples | Antenatal clinics | Mean for women=28 years; 72% men aged 26–30 | Length of time not reported; 100% married | Prospective cohort |
| Msuya et al, 2008 | Moshi, Tanzania | 2654 heterosexual women | Primary healthcare clinics | Mean=25 years | Not reported | Prospective cohort |
| Remien et al., 2005 | New York, New York, USA | 215 HIV-serodiscordant couples (74% heterosexual, 26% same-sex couples) | HIV/AIDS treatment clinics | Mean=42 years | Together for at least 6 months | Randomized controlled trial |
| Semrau et al., 2005 | Lusaka, Zambia | 9409 heterosexual women | Antenatal clinic | Mean=22 years | Length of time not reported; 100% married | Prospective cohort |
| Sullivan et al.., 2014 | Atlanta, Georgia, USA | 11 HIV-serodiscordant men who have sex (MSM) couples | Community-based organizations, retail locations, and web ads | Median=18 to 29 years | Mean=14 months | Randomized controlled trial |
| Voluntary HIV-1 Counseling & Testing Efficacy Study Group, 2000 | Nairobi, Kenya; Dar es Salaam, Tanzania; Port of Spain, Trinidad | 586 heterosexual couples | Communities | Mean for men=29 years; Mean for women = 28 years | Length of time not reported; 64% couple married | Randomized controlled trial |
As reported in Table 2, outcomes examined include protective sex behavior (defined as consistent condom use or no sex without condoms), STIs, HIV testing, Nevirapine uptake among pregnant women, and HIV medication adherence. No studies evaluated drug use behaviors. The results of random-effect models showed statistically significant intervention effects for protective sex (OR = 1.60, 95% CI = 1.21, 2.11, p = 0.0012, nine effect sizes), HIV testing (OR = 1.79, 95% CI = 1.31, 2.45, p = .0000, three effect sizes), and Nevirapine uptake (OR = 1.51, 95% CI = 1.02, 2.24, p =0.0397, six effect sizes). There was insufficient evidence for STI and HIV medication adherence due to a small number of studies (only two studies examining STI and one study on HIV medication adherence). Modest heterogeneity (i.e., I2 around 50%) was observed. One study included in the HIV testing outcome was windsorized (Semrau et al., 2005) and there was no evidence that any other individual effect size exerted influence on the aggregated effect sizes.
Table 2.
Effect of couple-based interventions on protective sex, STIs, HIV testing, Nevirapine uptake, and medication adherence
| Outcomes Author (year), Study Location |
OR | low 95% | upper 95% | Z | p value | Q statistic, p value | I2 |
|---|---|---|---|---|---|---|---|
| Protective Sex | |||||||
| Allen (1992), Rwanda | 2.31 | 1.77 | 3.00 | 6.23 | 0.0000 | ||
| Becker (2010), Tanzania | 6.00 | 0.77 | 46.58 | 1.71 | 0.0866 | ||
| El-Bassel (2003), USA | 1.37 | 0.61 | 3.07 | 0.77 | 0.4398 | ||
| El-Bassel (2010), USA | 1.75 | 1.21 | 2.52 | 3.00 | 0.0027 | ||
| El-Bassel (2011), USA | 0.76 | 0.44 | 1.30 | −1.01 | 0.3131 | ||
| Farquhar (2004), Kenya | 6.50 | 0.77 | 54.93 | 1.72 | 0.0856 | ||
| Jones (2013), USA | 1.14 | 0.63 | 2.04 | 0.43 | 0.6692 | ||
| Sullivan (2014), USA | 1.00 | 0.14 | 7.10 | 0.00 | 1.0000 | ||
| VCT HIV-1 Eff Stdy Grp (2000), Kenya, Tanzania, Trinidad | 1.75 | 1.40 | 2.20 | 4.86 | 0.0000 | ||
| Random Effect Model | 1.60 | 1.21 | 2.11 | 3.28 | 0.0012 | 19.01, p=.015 | 57.93 |
| Reduction of Sexually transmitted infections (STIs) | |||||||
| El-Bassel (2010), USA | 1.02 | 0.64 | 1.62 | 0.09 | 0.9316 | ||
| El-Bassel (2011), USA | 3.47 | 1.01 | 11.89 | 1.98 | 0.0475 | ||
| Random Effect Model | 1.64 | 0.51 | 5.27 | 0.83 | 0.4075 | 3.33, p=.068 | 65.14 |
| HIV Testing | |||||||
| Becker (2010), Tanzania | 1.59 | 1.09 | 2.32 | 2.43 | 0.0153 | ||
| Khoshnood (2006), China | 1.42 | 0.90 | 2.24 | 1.50 | 0.1328 | ||
| Semrau (2005)a, Zambia | 2.37 | 1.68 | 3.33 | 4.93 | 0.0000 | ||
| Random Effect Model | 1.79 | 1.31 | 2.45 | 3.64 | 0.0000 | 3.90, p=.142 | 48.76 |
| Nevirapine uptake among HIV-positive pregnant women | |||||||
| Becker (2010), Tanzania | 3.87 | 1.00 | 14.98 | 1.96 | 0.0500 | ||
| Conkling (2010), Rwanda | 0.94 | 0.55 | 1.61 | −0.23 | 0.8178 | ||
| Conkling (2010), Zambia | 1.62 | 0.55 | 4.76 | 0.87 | 0.3842 | ||
| Farquhar (2004), Kenya | 2.36 | 1.02 | 5.43 | 2.02 | 0.0439 | ||
| Msuya (2008), Tanzania | 3.44 | 0.99 | 11.97 | 1.94 | 0.0521 | ||
| Semrua (2005), Zambia | 1.17 | 0.91 | 1.51 | 1.22 | 0.2218 | ||
| Random Effect Model | 1.51 | 1.02 | 2.24 | 2.06 | 0.0397 | 8.92, p=.112 | 43.98 |
| HIV medication adherence | |||||||
| Remien (2005), USA | 1.23 | 0.73 | 2.08 | 0.776 | 0.438 | ||
Windsorized to the value of three standard errors from the means of all the effect sizes for HIV testing. The original effect size was OR=6.16, 95% CI=4.38, 8.68.
DISCUSSION
Our systematic review and meta-analysis provides direct evidence that couple-based interventions are more effective in promoting protective sex, HIV testing and Nevirapine uptake when directly compared to interventions delivered to individuals. The evidence demonstrates the usefulness of couple-based interventions in protecting individuals, partners, and newborn children from the risk of HIV transmission and infection.
Our findings are particularly important in the era of treatment as prevention. Couples HIV counseling and testing allows both members of a couple to learn their HIV status and make informed choices surrounding antiretroviral prophylaxis during pregnancy (for heterosexual couples) and antiretroviral therapy (ART). ART reduces HIV-1 infection within discordant couples (Baggaley, White, Hollingsworth, & Boily, 2013; Cohen et al., 2011); however, the non-zero transmission risk from partners receiving ART points to the need of appropriate counseling and risk-reduction strategies for discordant couples (Baggaley et al., 2013). Couple-based interventions can provide a supportive environment that enables a couple to disclose more safely to each other about personal and potentially difficult information (e.g., outside partners, STIs), to make a joint decision and responsibility for safer sex practice, and to capitalize partner’s support for prevention and care. Given the promise of couple-based interventions (Jiwatram-Negron & El-Bassel, 2014; Purcell et al., 2014), it is exciting that several treatment-as-prevention and preexposure prophylaxis (PrEP) trials have incorporated the couple-based component as part of biomedical interventions (Cohen et al., 2011; Baeten et al., 2012).
Several limitations warrant comment. The evidence presented is primarily driven by behavior changes among heterosexual couples. Only one study (Sullivan et al., 2014) that compared the couple-based intervention with an intervention delivered to individuals was specifically designed for MSM couples. Additionally, none of the included studies targeted drug users or evaluated drug use behaviors and only one study evaluated medication adherence outcomes. The findings should be reassessed when additional data become available. The U.S.-based studies primarily focused on sexual risk reduction, while most of the international studies focused on couple HIV testing or prevention of mother-to-child transmission. Replicating and adapting effective couple-based interventions in the countries where the interventions were not previously tested will be an important quest.
Based on the current couple-based research literature, several important operational questions merit future examinations: (1) Which intervention modalities work best and under what circumstances? and (2) What are the best strategies to combine couple-based interventions with other behavioral, structural and biomedical interventions in a scalable and cost-effective way? Although additional operational research is needed, couple-based interventions can be utilized to enhance prevention effects and reduce HIV transmission and infection in the era of treatment as prevention.
Acknowledgments
We thank other members of the HIV/AIDS Prevention Research Synthesis (PRS) Project members for their contribution to the coding and maintenance of the PRS database that was used for this systematic review (listed alphabetically): Adebukola Adegbite, Terrika Barham, Julia B. DeLuca, Darrel Higa, Linda Kay (former), Theresa A. Sipe, and Christina White.
Footnotes
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the U.S. Centers for Disease Control and Prevention.
Human Participant Protection. No human subjects were involved in this study.
Contributors. N Crepaz originated the study and was responsible for writing the brief. MV Tungol-Ashmon, HW Vosburgh, BN Baack, and MM Mullins did data coding, conducted analyses, and provided technical and material support, article review and editing.
Conflicts of interest. All the authors declare no conflict of interest. This work was supported by the Division of HIV/AIDS Prevention at the U.S. Centers for Disease Control and Prevention and was not funded by any other organization.
Reference List
- Allen S, Tice J, Van de Perre P, Serufilira A, Hudes E, Nsengumuremyi F, Hulley S. Effect of serotesting with counselling on condom use and seroconversion among HIV discordant couples in Africa. British Medical Journal. 1992;304:1605–1609. doi: 10.1136/bmj.304.6842.1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baeten JM, Donnell D, Ndase P, Mugo NR, Campbell JD, Wangisi J, Celum C. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. New England Journal of Medicine. 2012;367:399–410. doi: 10.1056/NEJMoa1108524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baggaley RF, White RG, Hollingsworth TD, Boily MC. Heterosexual HIV-1 infectiousness and antiretroviral use: Systematic review of prospective studies of discordant couples. Epidemiology. 2013;24:110–121. doi: 10.1097/EDE.0b013e318276cad7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker S, Mlay R, Schwandt HM, Lyamuya E. Comparing couples’ and individual voluntary counseling and testing for HIV at antenatal clinics in Tanzania: A randomized trial. AIDS and Behavior. 2010;14:558–566. doi: 10.1007/s10461-009-9607-1. [DOI] [PubMed] [Google Scholar]
- Burton J, Darbes LA, Operario D. Couples-focused behavioral interventions for prevention of HIV: Systematic review of the state of evidence. AIDS and Behavior. 2010;14:1–10. doi: 10.1007/s10461-008-9471-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, Fleming TR. Prevention of HIV-1 infection with early antiretroviral therapy. New England Journal of Medicine. 2011;365:493–505. doi: 10.1056/NEJMoa1105243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conkling M, Shutes EL, Karita E, Chomba E, Tichacek A, Sinkala M, Allen SA. Couples’ voluntary counselling and testing and nevirapine use in antenatal clinics in two African capitals: A prospective cohort study. Journal of the International AIDS Society. 2010;13:10. doi: 10.1186/1758-2652-13-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Bassel N, Wechsberg WM. Couple-based HIV behavioral interventions: Placing HIV risk reduction responsibility and agency on the female and male dyad. Couple and Family Psychology: Research and Practice. 2012;1:94–105. [Google Scholar]
- El-Bassel N, Witte SS, Gilbert L, Wu E, Chang M, Hill J, Steinglass P. The efficacy of a relationship-based HIV/STD prevention program for heterosexual couples. American Journal of Public Health. 2003;93:963–969. doi: 10.2105/ajph.93.6.963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Bassel N, Jemmott JB, Landis JR, Pequegnat W, Wingood GM, Wyatt GE, Bellamy SL. National institute of mental health multisite eban HIV/STD prevention intervention for african american HIV serodiscordant couples: A cluster randomized trial. Archives of Internal Medicine. 2010;170:1594–1601. doi: 10.1001/archinternmed.2010.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Bassel N, Gilbert L, Wu E, Witte SS, Chang M, Hill J, Remien RH. Couple-based HIV prevention for low-income drug users from New York City: A randomized controlled trial to reduce dual risks. Journal of Acquired Immune Deficiency Syndromes. 2011;58:198–206. doi: 10.1097/QAI.0b013e318229eab1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farquhar C, Kiarie JN, Richardson BA, Kabura MN, John FN, Nduati RW, John-Stewart GC. Antenatal couple counseling increases uptake of interventions to prevent HIV-1 transmission. Journal of Acquired Immune Deficiency Syndromes. 2004;37:1620–1626. doi: 10.1097/00126334-200412150-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedges LV, Vevea JL. Fixed- and random-effects models in meta-analysis. Psychological Methods. 1998;3:486–504. [Google Scholar]
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. British Medical Journal. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiwatram-Negron T, El-Bassel N. Systematic review of couple-based HIV intervention and prevention studies: Advantages, gaps, and future directions. AIDS and Behavior. 2014;18:1864–1887. doi: 10.1007/s10461-014-0827-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones DL, Kashy D, Villar-Loubet OM, Cook R, Weiss SM. The impact of substance use, sexual trauma, and intimate partner violence on sexual risk intervention outcomes in couples: A randomized trial. Annals of Behavioral Medicine. 2013;45:318–328. doi: 10.1007/s12160-012-9455-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy CE, Medley AM, Sweat MD, O’Reilly KR. Behavioural interventions for HIV positive prevention in developing countries: A systematic review and meta-analysis. Bulletin of the World Health Organization. 2010;88:615–623. doi: 10.2471/BLT.09.068213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khoshnood K, Wilson KS, Filardo G, Liu Z, Keung NH, Wu Z. Assessing the efficacy of a voluntary HIV counseling and testing intervention for pregnant women and male partners in Urumqi City, China. AIDS and Behavior. 2006;10:671–681. doi: 10.1007/s10461-006-9092-8. [DOI] [PubMed] [Google Scholar]
- Kiarie JN, Kreiss JK, Richardson BA, John-Stewart GC. Compliance with antiretroviral regimens to prevent perinatal HIV-1 transmission in Kenya. AIDS. 2003;17:65–71. doi: 10.1097/01.aids.0000042938.55529.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaCroix JM, Pellowski JA, Lennon CA, Johnson BT. Behavioural interventions to reduce sexual risk for HIV in heterosexual couples: A meta-analysis. Sexually Transmitted Infections. 2013;89:620–627. doi: 10.1136/sextrans-2013-051135. [DOI] [PubMed] [Google Scholar]
- Langebeek N, Gisolf EH, Reiss P, Vervoort SC, Hafsteinsdottir TB, Richter C, Nieuwkerk PT. Predictors and correlates of adherence to combination antiretroviral therapy (ART) for chronic HIV infection: a meta-analysis. BMC Medicine. 2014;12:142. doi: 10.1186/s12916-014-0142-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipsey MW, Wilson DB. Practical meta-analysis. Thousand Oaks, CA: Sage Publications; 2001. [Google Scholar]
- Meader N, Semaan S, Halton M, Bhatti H, Chan M, Llewellyn A, Des Jarlais DC. An international systematic review and meta-analysis of multisession psychosocial interventions compared with educational or minimal interventions on the HIV sex risk behaviors of people who use drugs. AIDS and Behavior. 2013;17:1963–1978. doi: 10.1007/s10461-012-0403-y. [DOI] [PubMed] [Google Scholar]
- Msuya SE, Mbizvo EM, Hussain A, Uriyo J, Sam NE, Stray-Pedersen B. Low male partner participation in antenatal HIV counselling and testing in northern Tanzania: Implications for preventive programs. AIDS Care. 2008;20:700–709. doi: 10.1080/09540120701687059. [DOI] [PubMed] [Google Scholar]
- Purcell DW, Mizuno Y, Smith DK, Grabbe K, Courtenay-Quick C, Tomlinson H, Mermin J. Incorporating couples-based approaches into HIV prevention for gay and bisexual men: Opportunities and challenges. Archives of Sexual Behavior. 2014;43:35–46. doi: 10.1007/s10508-013-0205-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Remien RH, Stirratt MJ, Dolezal C, Dognin JS, Wagner GJ, Carballo-Dieguez A, Jung TM. Couple-focused support to improve HIV medication adherence: A randomized controlled trial. AIDS. 2005;19:807–814. doi: 10.1097/01.aids.0000168975.44219.45. [DOI] [PubMed] [Google Scholar]
- Sandelowski M, Voils CI, Chang Y, Lee EJ. A systematic review comparing antiretroviral adherence descriptive and intervention studies conducted in the USA. AIDS Care. 2009;21:953–966. doi: 10.1080/09540120802626212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Semrau K, Kuhn L, Vwalika C, Kasonde P, Sinkala M, Kankasa C, Thea DM. Women in couples antenatal HIV counseling and testing are not more likely to report adverse social events. AIDS. 2005;19:603–609. doi: 10.1097/01.aids.0000163937.07026.a0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan PS, White D, Rosenberg ES, Barnes J, Jones J, Dasgupta S, Stephenson R. Safety and acceptability of couples HIV testing and counseling for US men who have sex with men: A randomized prevention study. Journal of the International Association of Providers in AIDS Care. 2014;13:135–144. doi: 10.1177/2325957413500534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNAIDS. Global Report UNAIDS report on the global AIDS epidemic 2013. 2013 Retrieved January 20, 2015, from http://UNAIDS.org.
- Voluntary HIV-1 Counseling and Testing Efficacy Study Group. Efficacy of voluntary HIV-1 counselling and testing in individuals and couples in Kenya, Tanzania, and Trinidad: A randomised trial. Lancet. 2000;356:103–112. [PubMed] [Google Scholar]