Abstract
In a time of scientific and technological developments and budgetary constraints, the National Cancer Institute (NCI)’s Provocative Questions (PQ) Project offers a novel funding mechanism for cancer epidemiologists. We reviewed the purposes underlying the PQ Project, present information on the contributions of epidemiologic research to the current PQ portfolio, and outline opportunities that the cancer epidemiology community might capitalize on to advance a research agenda that spans a translational continuum from scientific discoveries to population health impact.
In 2010, Harold Varmus began his stewardship as the director of the National Cancer Institute (NCI) with a key initiative called the Provocative Questions (PQ) Project. The primary purpose of the PQ Project is to invigorate and “engage a diverse range of scientists in a challenging intellectual exercise to define and then solve the major unsolved or neglected problems in oncology” (1). The initiative builds on a rich history of scientific discoveries and comes at a time of great scientific and technological advances in fields like genomics and related disciplines. The NCI’s PQ Project differs from larger global initiatives that tend to set overarching goals (e.g., the United Nations’ Millennium Development Goals) or post challenges (e.g., Gates Foundation’s Grand Challenges in Global Health) (1). Instead, this NCI initiative identifies and funds the search for answers to specific scientific questions, reflecting the belief that addressing specific and intractable problems can inspire the most outstanding work in science.
Towards this effort to identify important but unanswered scientific questions, the NCI launched the Provocative Questions Project website (2) and gathered questions from the cancer research community. Concurrently, in a series of workshops across the country, an assembled group of scientific leaders deliberated on potential questions and selected 24 PQ questions to provide the basis of the PQ’s Funding Opportunity Announcements (FOAs) (3) in October 2011. As noted on the website, these questions do not represent the scope of NCI’s priorities in cancer research, but serve to probe and challenge cancer researchers to deliberate about problems in key areas of cancer research that are significant but have been neglected.
Contemporaneous with the introduction of the PQ Project, an independent undercurrent of thought-provoking publications appeared. These publications simultaneously call for a reexamination of priorities and strategic approaches across different health-related disciplines as the conduct of scientific research (and thinking) must adapt quickly to an evolving technological, demographic, and budgetary landscape. For example, in their essay on 21st century public health, Lang and Rayner lamented the need to revamp the practice of public health and alter the public’s misconception of the field by reminding the audience of the inter-relationship between health and societal progress (4). Furthermore, they advocated for the embracement of ecological public health as essential to progress instead of its abandonment or neglect in times of economic hardships (4). Coincidentally, epidemiology, a discipline at the heart of public health, is undergoing a similar rethinking. The field, opined Michael Lauer, Director of the Division of Cardiovascular Sciences of the National Heart, Lung, and Blood Institute, is in need of a “creative transformation” to include refocused scientific questions, incorporation of technologies, centralized governance, cross-discipline collaboration, and clinical trials embedded in registries (5). In tandem, the Epidemiology and Genomics Research Program (EGRP) at NCI led a strategic planning “longitudinal” meeting, Trends in 21st Century Epidemiology: From Scientific Discoveries to Population Health Impact in December 2012 to invigorate 21st century epidemiologists (6, 7). From the NCI’s Workshop, several recommendations emerged for the epidemiology community to consider. These recommendations, published elsewhere in this special edition (see Khoury et al 2013), include (i) extending the reach of epidemiology beyond discovery and etiologic research to include interdisciplinary/ multilevel evaluation, implementation, and outcomes research; (ii) transforming the practice of epidemiology by moving towards more access and sharing of protocols, data, metadata, and specimens to foster collaboration, to ensure reproducibility and replication, and accelerate translation; (iii) expanding cohort studies to collect exposure, clinical and other information across the life course and examining multiple health-related endpoints; (iv) developing and validating reliable methods and technologies to quantify exposures and outcomes on a massive scale, and to assess concomitantly the role of multiple factors in complex diseases; (v) integrating “big data” science into the practice of epidemiology; (vi) expanding knowledge integration to drive research, policy and practice; (vii) transforming training of 21st century epidemiologists to address interdisciplinary and translational research; and (viii) optimizing the use of resources and infrastructure for epidemiologic studies. Echoing across these intellectual discourses is a concerted exhortation for adaptation of changes (e.g. disruptive technologies) and optimizing resources to evolve constructively and ensure relevance and continued contribution to society.
The current fiscal constraints for funding scientific research, however, dampens enthusiasm for the translation of these ideas into actions as budgetary constraints act as a major disincentive for expanding or extending research. Nevertheless, a resource-scarce environment necessitates greater resourcefulness and innovation. Although receiving less attention, the PQ Project’s second purpose is to experiment with an innovative funding mechanism that permits investigators to “propose intriguing questions in cancer research that need attention but would usually find it difficult to get” (1). In the initial FOAs, $17 million were dedicated to fund awarded PQ proposals. The NCI received approximately 750 applications in response to the PQ’s Request For Applications (RFAs). In reaction to this overwhelming response from the scientific community, the Fiscal Year (FY) 2012 budget dedicated to funding PQ projects increased to $22 million.
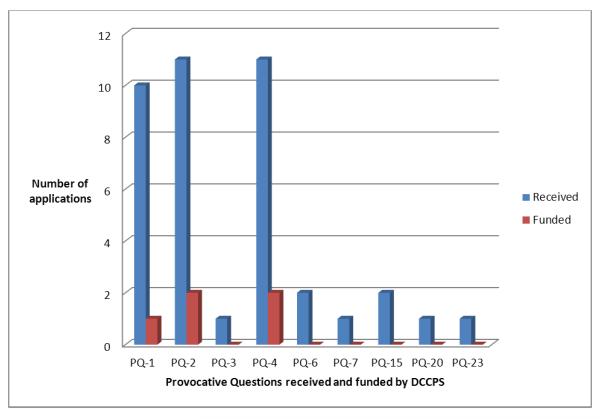
While the PQ Project does not focus on particular scientific disciplines, Dr. Varmus and the NCI leadership recognized the contributions of epidemiology in cancer. In a 2011 town hall meeting (8), Dr. Varmus stated, “I expect to see a pretty dramatic revolution in epidemiology... defining cancers by genetic subsets. I expect to see molecular tools brought more forcefully into the realm of cancer diagnosis... talking about ways to discriminate among early lesions and pre-cancerous lesions that may have malignant potential.” (9). Examination of the PQ applications received in response to the initial RFAs revealed that there was an underrepresentation of applications submitted that were epidemiologic in nature. For the purpose of this commentary, we broadly defined epidemiologic research as research conducted on human populations to understand determinants of cancer occurrence and outcomes. Of the total 748 applications, only 40 (5%) of the applications were from population scientists and referred to the NCI’s Division of Cancer Control and Population Sciences (DCCPS), Figure 1. These statistics are grossly lower than the typical number of applications received by NCI and referred to DCCPS annually. For example in FY 2012, NCI received 10,448 competing applications for funding, and approximately 14% (N= 1,509) were related to population sciences and referred to DCCPS. This suggests that cancer epidemiologists might not have fully capitalized on this new funding mechanism and opportunity.
Figure 1.
Applications received from the initial announcement of the PQ Project that were referred to and funded by the NCI, Division on Cancer Control and Population Sciences (DCPPS)
NOTE: The PQs from the initial announcement can be found at: http://provocativequestions.nci.nih.gov/rfa-archive
The success rate for funding of epidemiology-related PQ proposals was slightly higher comparatively to the proportion of applications. The NCI awarded 57 applicants whose research individually sought to answer one of the 24 provocative questions. Population sciences research represented 9% (N=5) of the 57 awarded applications (Figure 1). The majority of the PQ applications referred to DCCPS were responding to three PQ questions: (1) How does obesity contribute to cancer risk? (PQ-1); (2) What environmental factors change the risk of various cancers when people move from one geographic region to another? (PQ-2); and (3) Why don’t more people alter behaviors known to increase the risk of cancers? (PQ-4). Successful PQ epidemiology-related proposals reflected this distribution (Figure 1).
Some of the remaining 21 PQs posed could have leveraged epidemiologic methods; unfortunately, these received very few applications from population scientists. Several reasons may explain the lackluster number of PQ applications from the cancer epidemiology community. Population-based research is costly and it is conceivable that the original funding allocated for the PQ Project may have deterred some epidemiologists from applying. However, as mentioned earlier, the NCI leadership devoted more funding to the initial round to fund additional meritorious PQ proposals.
Another reason for the lower number of epidemiologic applications may be that the 24 provocative questions originally identified may have been viewed as skewed heavily towards basic science and thus leaving a narrow opportunity for applications that uses epidemiologic concepts and methods to answer the questions. The reach and application of epidemiology should not be narrowed by this misperception. Epidemiology is circular by nature—findings can inform bench science which informs epidemiology and further downstream can influence translation of findings into policy and guidelines. As a central infrastructure, epidemiologic concepts and methods can be leveraged to address some of the basic science questions such as those in the PQs. Extending the boundaries of epidemiology as recommended by the NCI Workshop (see Khoury et al 2013) requires creativity, provocativeness, resourcefulness, and collaboration across disciplines. Proposals to integrate basic or clinical studies within the framework of traditional epidemiologic studies, for example, could be submitted. Alternatively, epidemiologists can modify or adapt the current PQs to develop proposals with a more population approach or gauge the programmatic interests based on the questions to generate new research ideas. These proposals can be submitted under the omnibus investigator-initiated FOAs (10). Lastly, the PQ Project is a dynamic initiative in which provocative questions are continually being developed.
Over the past year, NCI updated the original set of 24 PQs. The revised 24 PQs are categorized into four groups (Group A to Group D) based on PQ theme (Table 1). For example, Group A consists of six questions related to cancer prevention and risk while Group D’s questions relate to cancer therapy and outcomes. Cancer epidemiologists should think more broadly across the translational research continuum when reviewing the revised set of PQs as well as their research objectives. Collaborations between basic, clinical and population scientists, for example, can extend the boundaries of traditional epidemiology to help unravel the answers to some of the PQs. Illustratively, the answer or answers to PQD3 “What underlying causal events - e.g., genetic, epigenetic, biologic, behavioral, or environmental - allow certain individuals to survive beyond the expected limits of otherwise highly lethal cancers?” may benefit from such a trans/multi-disciplinary collaboration. New approaches like integrative epidemiology, as advocated by Spitz et al (11), can be applied to explore the mechanistic underpinnings of epidemiologic observations in cancer risk and outcomes.
Table 1.
List of current 24 Provocative Questions (PQ) by group and thematic focus
| PQ Group | Focus | Questions |
|---|---|---|
| Group A (RFA-CA-12- 015 and RFA- CA-12-016)* |
Cancer Prevention and Risk |
|
| Group B (RFA-CA-12- 017 and RFA- CA-12-018)* |
Mechanisms of Tumor Development or Recurrence |
|
| Group C (RFA-CA-12- 019 and RFA- CA-12-020)* |
Tumor Detection, Diagnosis and Prognosis |
|
| Group D (RFA-CA-12- 021 and RFA- CA-12-022)* |
Cancer Therapy and Outcomes |
|
NOTE: This grouping does not reflect any priority of PQs for review or funding purposes. Supporting information relating to the 24 PQs can be found at:http://provocativequestions.nci.nih.gov/rfa.
Letter of Intent in response to PQ’s RFAs due on May 20, 2013.
For the current PQ process, NCI has issued eight FOAs, utilizing the RO1 (N=4) and R21 (N=4) funding mechanisms (12). The scientific scope of the application must correspond to one and only one PQ in the group (Table 1). The next deadline for response to RFAs relating to the PQ Project is in May 2013. We encourage epidemiologists to collaborate with their basic science and clinical colleagues to take full advantage of this funding mechanism. Development of provocative questions for 2014 is underway, which may include new population science questions. Investigators should stay alert for subsequent PQ announcements.
Cancer epidemiology is at the cusp of a paradigm shift and several “drivers” have been influencing the field in the near decades (7). The drivers include: (i) collaboration and team science; (ii) methods and technologies; (iii) multi-level analyses and interventions; and (iv) knowledge integration from basic, clinical and population sciences (7). The PQ Project is one vehicle to enable the incorporation of these drivers into cancer epidemiologic research and part of a collective and fluid movement towards a transformation in health research. The provocativeness lies not only in the scientific questions, but also in the resourcefulness of the investigators to seize funding opportunities and to think in creative and transformative ways to get to answers that can have an impact on reducing the burden of cancer in populations.
REFERENCES
- 1.Varmus H, Harlow E. Science funding: Provocative questions in cancer research. Nature. 2012;481(7382):436–7. doi: 10.1038/481436a. [DOI] [PubMed] [Google Scholar]
- 2.The NCI’s Provocative Questions Project. http://provocativequestions.nci.nih.gov/
- 3.PQ’s Funding Opportunity Announcements. http://provocativequestions.nci.nih.gov/rfa-archive.
- 4.Lang T, Rayner G. Ecological public health: the 21st century’s big idea? An essay by Tim Lang and Geof Rayner. BMJ. 2012;345:e5466. doi: 10.1136/bmj.e5466. [DOI] [PubMed] [Google Scholar]
- 5.Lauer MS. Time for a creative transformation of epidemiology in the United States. Jama. 2012;308(17):1804–5. doi: 10.1001/jama.2012.14838. [DOI] [PubMed] [Google Scholar]
- 6.Khoury MJ, Freedman AN, Gillanders EM, Harvey CE, Kaefer C, Reid BC, et al. Frontiers in cancer epidemiology: a challenge to the research community from the Epidemiology and Genomics Research Program at the National Cancer Institute. Cancer Epidemiol Biomarkers Prev. 2012;21(7):999–1001. doi: 10.1158/1055-9965.EPI-12-0525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lam TK, Spitz M, Schully SD, Khoury MJ. “Drivers” of Translational Cancer Epidemiology in the 21st Century: Needs and Opportunities. Cancer Epidemiol Biomarkers Prev. 2013 doi: 10.1158/1055-9965.EPI-12-1262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harold Varmus’ Town Hall Meeting. 2011 http://videocast.nih.gov/launch.asp?16391.
- 9.Varmus H. National Cancer Institute Hown Hall Meeting. 2011.
- 10.Investigator-initiated Funding Opportunity Announcement. http://grants.nih.gov/grants/guide/parent_announcements.htm.
- 11.Spitz MR, Caporaso NE, Sellers TA. Integrative cancer epidemiology--the next generation. Cancer Discov. 2012;2(12):1087–90. doi: 10.1158/2159-8290.CD-12-0424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.2012 RFA Links and Provocative Questions. 2013 http://provocativequestions.nci.nih.gov/rfa.