Key Clinical Message
Nonvisualization of the gallbladder during the second trimester of pregnancy should prompt concern for biliary atresia. A normal‐sized gallbladder with irregular and crenelated wall associated with a cyst of the extrahepatic tract should raise concern for cystic biliary atresia.
Keywords: Biliary atresia, cyst, fetal ultrasound, gallbladder, prenatal diagnosis
A healthy 21‐year‐old woman was referred at 21 weeks of gestation (WG) for an abdominal right paramedian well‐defined anechoic mass discovered at routine ultrasound examination in an eutrophic female fetus. High‐resolution ultrasound identified an 11‐mm‐diameter cystic mass with a thin wall, in continuity with a small biliary canal and the gallbladder. The gallbladder showed a normal size but its wall was crenelated and irregular. No other abnormalities were observed. The amount of amniotic fluid and the placenta were normal. At 32 WG, the cystic mass and the gallbladder were unchanged in size and morphology (Fig. 1).
Figure 1.
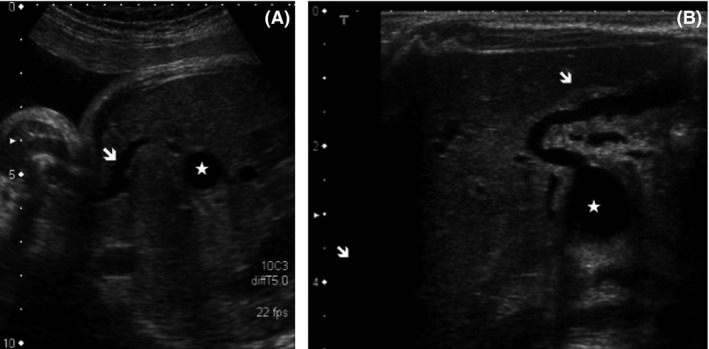
(A): Ultrasound abdominal axial slice at 32 weeks of gestation, using a curved transducer. The cystic mass (white star) displays a thin wall in continuity with a small biliary canal and the gallbladder (white arrow). The wall of the gallbladder is irregular. (B): Abdominal axial slice performed at birth using with a high frequency linear probe. The same findings as those depicted prenatally are present [irregular and crenelated wall of the gallbladder (white arrow), cyst (white star)]. The intrahepatic biliary ducts are not dilated.
The hepatic veins were visualized. The liver parenchyma was homogenous. The intrahepatic ducts were not dilated. Increased echogenicity anterior to bifurcation of the portal vein (the so‐called “triangular cord sign” depicted postnatally 1) was not observed. There were no findings (polysplenia, situs inversus, or absence of retro‐hepatic inferior vena cava with azygos continuation) suggestive of a syndromic biliary atresia. The association of a cystic mass with a normal‐sized gallbladder and an irregular wall led us to suggest the diagnosis a cystic biliary atresia and parental counseling was provided. At birth, the initial clinical examination was normal. At 2 days of age, ultrasound depicted a normal‐sized gallbladder with still a crenelated, irregular, and thick wall, in continuity with a 14 mm‐diameter cyst, localized below the right portal vein (Fig. 1). There was diffuse periportal hyperechogenicity with a triangular cord sign. The biliary intrahepatic ducts were not dilated. Cystic biliary atresia was confirmed during per‐operative cholangiography that showed the communication between the gallbladder and the cyst with absence of opacification of the intrahepatic bile ducts and the common bile duct. The child underwent a Kasai procedure at the age of 21 days.
Biliary atresia (BA) is an inflammatory condition of the immature extra and intrahepatic biliary tract with progressive obliteration of the bile ducts. BA is the leading cause of extrahepatic obstructive neonatal jaundice. In the absence of early surgical treatment, the outcome is poor (hepatic insufficiency and cirrhosis). Cystic biliary atresia (CBA) is an uncommon form of BA with an occurrence rate of approximately 10% of cases. It is a well‐described postnatal entity 2 associating biliary atresia and a portal cyst. Nonvisualization of the gallbladder during the second trimester ultrasound should prompt concern for BA 3, 4, 5. Other gallbladder abnormalities can be diagnosed prenatally such as agenesis, left‐sided, septated or bilobed gallbladder 6. The diagnosis of BA is more challenging when the gallbladder is visible. A gallbladder with an irregular wall associated with a cyst of the extrahepatic biliary tract should raise suspicion for CBA 1. In BA, a microcyst is sometimes present at the level of the hepatic hilum but its diameter is much smaller than in CBA (<5 mm).
Cystic BA should be differentiated from a choledochal cyst, which is associated with a normal gallbladder, and is usually larger in size and may increase in size during pregnancy 7. The dilatation of the intrahepatic biliary ducts is suggestive of a choledochal cyst and then the diagnosis of CBA can be ruled out 1, 8.
The prenatal diagnosis of CBA allows better parental counseling and neonatal management. A specialized consultation at 2 weeks of life evaluates the presence or not of cholestatic jaundice (acholic stools), biological liver test, and liver ultrasound. In case of acholic stools with suspicion of BA, surgical management (Kasai portoenterostomy) aiming at restoring bile flow to the bowel, should be performed ideally before 40 days following birth, after umbilical cord healing, in order to improve BA prognosis.
We report the first case of crenelated and irregular gallbladder wall associating with a cyst of the extrahepatic biliary tract and allowing us to assess prenatally the diagnosis of cystic biliary atresia.
Conflict of Interest
None declared.
Clinical Case Reports 2015; 3(12): 1050–1051
References
- 1. Humphrey, T. M. , and Stringer M. D.. 2007. Biliary atresia: US diagnosis. Radiology 244:845–851. [DOI] [PubMed] [Google Scholar]
- 2. Burc, L. , Vuillard E., Guibourdenche J., Conti M., Garel C., Porquet D., et al. 2001. Prenatal diagnosis and follow up of biliary atresia. BJOG 108:1108–1110. [DOI] [PubMed] [Google Scholar]
- 3. Ben‐Ami, M. , Perlitz Y., Shalev S., Shajrawi I., and Muller F.. 2002. Prenatal diagnosis of extrahepatic biliary duct atresia. Prenat. Diagn. 22:583–585. [DOI] [PubMed] [Google Scholar]
- 4. Caponcelli, E. , Knisely A. S., and Davenport M.. 2008. Cystic biliary atresia: an etiologic and prognostic subgroup. J. Pediatr. Surg. 43:1619–1624. [DOI] [PubMed] [Google Scholar]
- 5. Shen, O. , Rabinowitz R., Yagel S., and Gal M.. 2011. Absent gallbladder on fetal ultrasound: prenatal findings and postnatal outcome. Ultrasound Obstet. Gynecol. 37:673–677. [DOI] [PubMed] [Google Scholar]
- 6. Bronshtein, M. , Weiner Z., Abramovici H., Filmar S., Erlik Y., and Blumenfeld Z.. 1993. Prenatal diagnosis of gall bladder anomalies–report of 17 cases. Prenat. Diagn. 13:851–861. [DOI] [PubMed] [Google Scholar]
- 7. Casaccia, G. , Bilancioni E., Nahom A., Trucchi A., Aite L., Marcellini M., et al. 2002. Cystic anomalies of biliary tree in the fetus: is it possible to make a more specific prenatal diagnosis? J. Pediatr. Surg. 37:1191–1194. [DOI] [PubMed] [Google Scholar]
- 8. Zhou, L.‐Y. , Guan B.‐Y., Li L., Xu Z.‐F., Dai C.‐P., Wang W., et al. 2012. Objective differential characteristics of cystic biliary atresia and choledochal cysts in neonates and young infants: sonographic findings. J Ultrasound Med. 31:833–841. [DOI] [PubMed] [Google Scholar]


