Abstract
Objective
The concurrent use of multiple health care systems may duplicate or fragment care. We assessed the characteristics of veterans who were dually enrolled in both the Veterans Affairs (VA) health care system and a Medicare Advantage (MA) plan, and compared intermediate quality outcomes among those exclusively receiving care in the VA with those receiving care in both systems.
Data Sources/Study Setting
VA and MA quality and administrative data from 2008 to 2009.
Study Design
We used propensity score methods to test the association between dual use and five intermediate outcome quality measures. Outcomes included control of cholesterol, blood pressure, and glycosylated hemoglobin among persons with coronary heart disease (CHD), hypertension, and diabetes.
Data Collection/Extraction Methods
VA and MA data were merged to identify VA‐only users (n = 1,637) and dual‐system users (n = 5,006).
Principal Findings
We found no significant differences in intermediate outcomes between VA‐only and dual‐user populations. Differences ranged from a 3.2 percentage point (95 percent CI: −1.8 to 8.2) greater rate of controlled cholesterol among VA‐only users with CHD to a 2.2 percentage point (95 percent CI: −2.4 to 6.6) greater rate of controlled blood pressure among dual users with diabetes.
Conclusions
For the five measures studied, we did not find evidence that veterans with dual use of VA and MA care experienced improved or worsened outcomes as compared with veterans who exclusively used VA care.
Keywords: Dual‐system use, Veterans Affairs, Medicare Advantage, outcomes, quality of care
Many veterans enrolled in the Department of Veterans Affairs (VA) health care system have alternative sources of insurance coverage and rely on non‐VA providers for some portion of their health care needs (DeVito, Morgan, and Virnig 1997; Fisher et al. 1998; Borowsky and Cowper 1999; Shen et al. 2003; Maciejewski et al. 2009; Liu et al. 2011). The use of services in a second system may provide an avenue for veterans to seek additional complementary care as needed. For instance, prior work has shown that veterans receiving care in non‐VA settings may prefer to use VA pharmacy benefits, which requires at least one VA outpatient encounter per year (Morgan et al. 2009). However, the concurrent use of VA and non‐VA care may also duplicate, fragment, or otherwise negatively impact care by hindering providers’ ability to monitor and coordinate services for dual‐using veterans (Hester, Cook, and Robbins 2005; Pizer and Gardner 2011).
Relatively little is known about the health consequences of dual use of VA and non‐VA care, and prior studies have been limited to veterans enrolled in the Medicare fee‐for‐service program (Wolinsky et al. 2006). For example, Helmer et al. (2008) reported poorer glycosylated hemoglobin control among dual users with diabetes relative to VA‐only users. Similarly, Jia et al. (2007) found that multiple‐system users in Florida were significantly more likely than VA‐only users to be rehospitalized within a year following a stroke.
The VA health care system is a federally funded managed care system administered by the Veterans Health Administration (VHA). VHA networks receive annual funding to provide veteran care based on network‐specific workloads using the Veterans Equitable Resource Allocation model. Medicare‐eligible veterans may choose to remain in the traditional fee‐for‐service Medicare program or enroll in a Medicare Advantage (MA) plan—a managed care plan administered by private health insurance companies that contract with the Centers for Medicare and Medicaid Services. Most MA plans cover additional benefits beyond those covered by traditional Medicare. Similarly, MA enrollees who are eligible to receive care in the VA can do so with no premium and relatively low copayments. Such factors make dual enrollment an attractive and affordable option for eligible veterans to acquire health insurance coverage of both VA and non‐VA health care services.
While prior studies have focused on the population of veterans receiving care in the VA and via traditional Medicare, very little work has characterized the increasing amount of dual participation in the VA and MA (Hynes et al. 2007; Keyhani et al. 2007; Carey et al. 2008; Humensky et al. 2012). Trivedi et al. (2012) found that the number of dual MA and VA enrollees nearly doubled in 5 years, growing from 485,651 in 2004 to 924,792 in 2009. In 2012, more than 10 percent of the approximately 8 million VA beneficiaries were enrolled in an MA plan, and more than 8 percent of the approximately 13 million MA enrollees were enrolled in the VA. Because both the VA and MA are federally funded managed care systems, expenditures are duplicated for individuals who are dually enrolled. There is little evidence to suggest that such increased federal spending is associated with better health outcomes for those enrolled in both systems.
Concerns about quality consequences of fragmented care are similar for veterans dually enrolled in the VA and fee‐for‐service Medicare or the VA and MA, and relate to the potential for inadequate communication between providers across systems. However, the differences in payment mechanisms for traditional Medicare and MA have the potential to differentially impact the proportion of care dual enrollees receive in the VA. In fee‐for‐service Medicare, payment is rendered only for the covered services that beneficiaries use. Conversely, MA plans receive capitated, prospective payments to cover all subsequent care required by their enrollees, providing a strong financial incentive for plans to reduce enrollees’ use of health services and potentially shift the costs of care to another government payer. Unlike the traditional Medicare program, MA plans can restrict the networks of available providers and alter their insurance benefits for Medicare‐covered services (Cooper and Trivedi 2012). Therefore, the reliance on VA care and the potential health consequences for dually enrolled veterans in MA plans may differ from what has been reported in the fee‐for‐service population.
Using national VA and MA administrative data from 2008 and 2009, we characterized the population of VA users with diabetes, hypertension, and coronary heart disease (CHD) who were dually enrolled in both managed care systems. We compared the quality of care among those who exclusively received care in the VA with care quality among those who received care in both the VA and MA. Because of prior research suggesting dual use is associated with care fragmentation, we hypothesized that dual VA and MA use would be associated with poorer quality as measured by intermediate health outcomes than VA‐only use.
Methods
Conceptual Framework
In this study, we employ the conceptual model of dual‐system use described by Petersen et al. (2010). This model posits that the choice of using a particular health system is influenced by patients’ sociodemographic and clinical characteristics, their geographic and financial access, and their patient perceptions of the health system (Figure S1). Sociodemographic characteristics include such factors as age, sex, race/ethnicity, and socioeconomic position. Geographic and financial access includes factors such as the distance to the nearest provider and insurance coverage, including copayments and other out‐of‐pocket costs for medical care. Health status includes medical complexity and comorbid conditions, which can act directly to influence the choice of health care system or indirectly by shaping patients’ perceptions of available health systems. Other factors that may influence patients’ perceptions of available health systems include health systems’ reputations, prior experience, provider recommendations, and the availability of specific health care–related programs, ancillary services, or amenities.
Sources of Data and Study Population
Our study population was derived from the 2008 and 2009 VA External Peer Review Program (EPRP) clinical performance assessment data, available from the VA Office of Quality and Performance. The EPRP data include a nationally representative random sample of veterans who are eligible for inclusion by having had at least one “anchoring” outpatient visit 13–24 months prior to the date of the performance assessment. To identify concurrent use of VA and MA services, we merged VA EPRP data with 2008 and 2009 Medicare Healthcare Effectiveness Data and Information Set (HEDIS) data, which include individual‐level information on MA outpatient, inpatient, and emergency service utilization. VA and Medicare HEDIS data were conservatively linked using a validated combination of the individual's social security number, date of birth, and sex (Fleming et al. 1992). Figure 1 depicts the construction of the study population.
Figure 1.
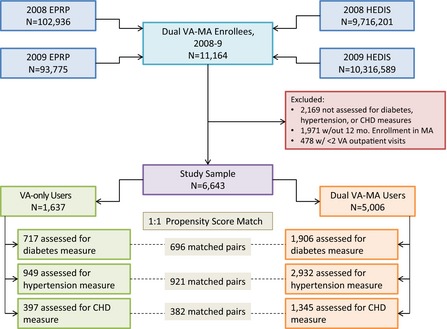
Flowchart of Study Sample Construction
Information about demographics, VA service utilization, and VA priority enrollment status was drawn from the 2008 and 2009 VA enrollment and utilization records. VA beneficiaries are assigned to one of the eight priority enrollment groups based primarily on service‐connected disability and income. High‐priority groups (groups 1–6) have lower VA copays than low‐priority groups (groups 7–8). Information about comorbid condition diagnoses was also obtained from VA records using a 2‐year look‐back period for all individuals in the study sample. Socioeconomic characteristics of each individual's zip code were derived from 2009 Census data, and the straight‐line distance from the center of each zip code to the nearest VA facility was obtained from the VA Planning Systems Support Group.
Of the 11,164 dually enrolled individuals in the sample, we excluded 2,169 (19.4 percent of total) individuals who were not assessed for the EPRP measures related to diabetes, hypertension, or CHD. We further excluded 1,971 (17.7 percent of total) individuals without 12 months of continuous enrollment in a single MA plan during the measurement year, because their opportunities for MA and VA utilization were not equivalent. We also excluded 478 individuals (4.3 percent of total) who had fewer than two VA outpatient encounters in the measurement year, as assessment of their health status in VA records may be incomplete. Our final study sample consisted of 6,643 elderly or disabled individuals with diabetes, hypertension, or CHD who were simultaneously enrolled in the VA and a HEDIS‐reporting MA plan during 2008 or 2009.
Variables
The independent variable of interest was whether a dually enrolled individual used outpatient services exclusively in the VA, or whether outpatient services were received in both the VA and MA in calendar year 2008 or 2009. We generated a measure of VA outpatient reliance, defined as the proportion of all outpatient visits (MA and VA) that occurred in the VA (Liu et al. 2011). Outpatient visits in the VA and MA were quantified using the same specifications, allowing for multiple encounters with different providers on the same day. Individuals with a reliance value of 1.0 were classified as VA‐only users, and individuals with reliance values less than 1.0 were considered dual VA and MA users. In a sensitivity analysis, we categorized the independent variable in the following three categories: predominant VA use (as defined by >0.8 VA reliance), predominant MA use (<0.2 VA reliance), and dual use (VA reliance 0.2 to 0.8).
The dependent variables of interest were five EPRP measures of outpatient quality in calendar year 2008 or 2009, assessing the intermediate outcomes of blood pressure control <140/90 mm Hg among persons with hypertension; low‐density lipoprotein (LDL) cholesterol control <100 mg/dl among persons with CHD; and LDL cholesterol control <100 mg/dl, blood pressure control <130/80 mmHg, and glycosylated hemoglobin control <9.0 percent among persons with diabetes. To achieve these intermediate outcome measures, a beneficiary must have had the outcome measured by the VA within the 12 preceding months and must have met the targeted goal on his or her most recent measurement (if multiple measurements are recorded during the 12‐month interval). If the most recent measurement did not meet the targeted goal, or if the outcome was not measured during the year, the beneficiary failed the measure.
Covariates included age, sex, race, U.S. Census region, Medicaid enrollment, special needs plan (SNP) enrollment (i.e., MA plans focusing on beneficiaries who are institutionalized, dually eligible, and/or have severe or disabling chronic conditions), VA enrollment priority status (high and low), 30 Elixhauser comorbid conditions, the proportion of persons older than 65 years with at least some college education in the individual's zip code, the median household income of persons older than 65 years in the individual's zip code, and the distance from the center of the individual's zip code to the nearest VA facility.
Analysis
We compared the demographic characteristics and use of services among dually enrolled individuals exclusively receiving care in the VA and those receiving care in both the VA and MA, using chi‐square and t‐tests to determine whether characteristics varied between the two groups. We also compared the quality of care in these two groups of dual enrollees, focusing on the five intermediate outcome measures described above, using both a propensity score and a standard multivariate approach. A propensity score for the use of VA‐only care was generated using the following covariates: age, sex, race, VA priority status, Medicaid and SNP enrollment, region, area‐level socioeconomic status, distance from enrollee zip code to nearest VA facility, and the presence of each of the 30 Elixhauser comorbid conditions (Elixhauser et al. 1998). VA‐only patients were matched to dual VA–MA users on propensity score on a one‐to‐one basis without replacement using the “Greedy 5 → 1 Digit Match” algorithm (Parsons 2001). In this approach, the highest digit “best” matches are made first, followed by lesser digit “next‐best” matches, until no more matches can be made. Once a match is made, it is not reconsidered, and if more than one match is available, a selection is made at random. We then calculated the mean, unadjusted difference between propensity score‐matched groups to compare the quality outcomes in VA‐only users and dual users. In addition, we used generalized linear regression models with generalized estimating equations to determine the association between dual use and intermediate outcomes after accounting for individual covariates and clustering of individuals in VA facilities. Regression models assumed an independent correlation structure and used an identity link to express differences on the risk difference scale and included an indicator for VA‐only or dual VA–MA use, adjusting for age, sex, race, VA priority status, Medicaid and SNP enrollment, region, area‐level socioeconomic status, distance from enrollee zip code to nearest VA facility, and the presence of each of the 30 Elixhauser comorbid conditions. Both propensity score and regression analyses were completed for veterans with diabetes, hypertension, and CHD.
A sensitivity analysis was conducted to evaluate the potential effect of alternative, nondichotomous characterizations of dual VA and MA use. We fitted a generalized linear regression model with generalized estimating equations using a three‐level independent variable of VA reliance (predominant VA use, predominant MA use, and dual use) and the covariates described above.
Additionally, we conducted a supplemental analysis to determine whether increasing numbers of VA visits were associated with better patient outcomes. In an assessment that also included dually enrolled individuals with fewer than two VA outpatient visits (n = 7,121), we grouped dual VA and MA enrollees according to their number of VA outpatient visits (≤2, 3–5, 6–9, ≥10). We then compared the quality outcomes of interest across strata of VA outpatient utilization.
The study was approved by the Providence VA Medical Center Institutional Review Board; the requirement for informed consent was waived. All analyses were performed with SAS Statistical Software (version 9.2). Results are reported with two‐tailed p‐values (α = .05) or 95 percent confidence intervals.
Results
Of the 6,643 individuals in the sample who were dually enrolled in the VA and MA, 1,637 (24.6 percent) exclusively received outpatient care in the VA, having an average of 27.2 annual VA outpatient visits. The remaining 5,006 (75.4 percent) received outpatient services in both the VA and MA, and on average had 15.1 annual VA outpatient visits and 8.8 annual MA outpatient visits (Table S1). VA‐only users were more likely to be younger (69.2 years vs. 71.3) and non‐white (20.7 percent vs. 10.6 percent) than dual VA–MA users (Table 1). They were also more likely to have high VA priority enrollment status (76.9 percent vs. 59.9 percent) and to be enrolled in Medicaid (2.4 percent vs. 1.4 percent) or a special needs plan (8.4 percent vs. 5.6 percent). On average, VA‐only users had more comorbid conditions than dual VA–MA users (4.7 conditions vs. 3.8) and lived one mile closer to a VA medical center (11.1 miles vs. 12.1). VA‐only users were also more likely to reside in zip codes with lower household incomes and fewer college‐educated residents age 65 and older.
Table 1.
Characteristics of Individuals with Diabetes, Hypertension, and/or CHD Dually Enrolled in the VA Health Care System and Medicare Advantage Plans in 2008–2009 (n = 6,643)
| VA‐Only Use | Dual VA–MA Use | p‐value for Difference | |
|---|---|---|---|
| n | 1,637 | 5,006 | |
| Age | |||
| Mean (SD) | 69.2 (8.0) | 71.3 (7.7) | <0.001 |
| Sex | |||
| Male (%) | 98.2 | 98.5 | 0.371 |
| Female (%) | 1.8 | 1.5 | |
| Race | |||
| White (%) | 79.3 | 89.4 | <0.001 |
| Black (%) | 17.3 | 7.9 | |
| Other (%) | 3.4 | 2.7 | |
| Region | |||
| Northeast (%) | 16.4 | 25.7 | <0.001 |
| Midwest (%) | 27.5 | 23.8 | |
| South (%) | 30.4 | 28.6 | |
| West (%) | 25.7 | 21.9 | |
| Medicaid and special needs plan enrollment | |||
| Enrolled in Medicaid (%) | 2.4 | 1.4 | 0.004 |
| Enrolled in SNP (%) | 8.4 | 5.6 | <0.001 |
| VA enrollment priority status | |||
| High priority—Groups 1–6 (%) | 76.9 | 59.9 | <0.001 |
| Low priority—Groups 7–8 (%) | 23.1 | 40.1 | |
| Number of comorbid conditions | |||
| Mean (SD) | 4.7 (2.5) | 3.8 (2.1) | <0.001 |
| Comorbid conditions | |||
| AIDS (%) | 0.1 | 0.3 | 0.087 |
| Alcohol abuse (%) | 8.8 | 4.4 | <0.001 |
| Blood loss anemia (%) | 0.7 | 0.5 | 0.228 |
| Chronic pulmonary disease (%) | 31.4 | 24.1 | <0.001 |
| Coagulopathy (%) | 5.3 | 3.5 | 0.001 |
| Congestive heart failure (%) | 18.0 | 13.0 | <0.001 |
| Deficiency anemia (%) | 22.0 | 15.1 | <0.001 |
| Depression (%) | 24.8 | 20.0 | <0.001 |
| Diabetes—complicated (%) | 27.7 | 20.4 | <0.001 |
| Diabetes—uncomplicated (%) | 57.7 | 54.8 | 0.040 |
| Drug abuse (%) | 4.4 | 2.4 | <0.001 |
| Fluid and electrolyte disorder (%) | 16.7 | 8.3 | <0.001 |
| Hypertension—complicated (%) | 94.1 | 89.9 | <0.001 |
| Hypothyroidism (%) | 10.1 | 9.2 | 0.288 |
| Liver disease (%) | 2.6 | 1.6 | 0.011 |
| Lymphoma (%) | 0.9 | 0.9 | 0.921 |
| Metastatic cancer (%) | 0.7 | 0.5 | 0.414 |
| Myocardial infarction (%) | 21.3 | 19.9 | 0.247 |
| Neurological disorder (%) | 6.9 | 5.5 | 0.043 |
| Obesity (%) | 36.0 | 29.5 | <0.001 |
| Paralysis (%) | 3.2 | 1.3 | <0.001 |
| Peripheral vascular disorder (%) | 19.6 | 15.2 | <0.001 |
| Psychoses (%) | 17.0 | 12.1 | <0.001 |
| Pulmonary circulation disorder (%) | 2.8 | 1.1 | <0.001 |
| Renal failure (%) | 5.1 | 4.2 | 0.131 |
| Rheumatoid arthritis (%) | 3.4 | 2.8 | 0.249 |
| Tumor—without metastasis (%) | 15.2 | 15.6 | 0.671 |
| Ulcer (%) | 0.4 | 0.1 | 0.010 |
| Valvular disease (%) | 7.1 | 6.4 | 0.283 |
| Weight loss (%) | 4.4 | 2.6 | <0.001 |
| Distance from zip code to VA | |||
| Mean (SD) | 11.1 (10.8) | 12.1 (10.8) | <0.001 |
| Proportion of persons >65 with some college education in zip code | |||
| Mean (SD) | 29.8 (13.0) | 30.6 (13.7) | 0.042 |
| Median household income for persons 65–74 in zip code | |||
| Mean (SD) | $29,618 ($9,362) | $31,417 ($9,389) | <0.001 |
| Median household income for persons >75 in zip code | |||
| Mean (SD) | $21,636 ($7,251) | $22,562 ($7,393) | <0.001 |
Bold text signifies p‐value for difference <.05.
VA EPRP intermediate outcome quality measures were comparable for VA‐only users and dual VA–MA users (Figure 2). Outcomes were marginally better for VA‐only users on the measures relating to hypertension control (n = 3,881) and CHD control (n = 1,742). Conversely, dual VA–MA users experienced slightly better outcomes on measures relating to diabetes control (n = 2,623) (p > .05 for all differences).
Figure 2.
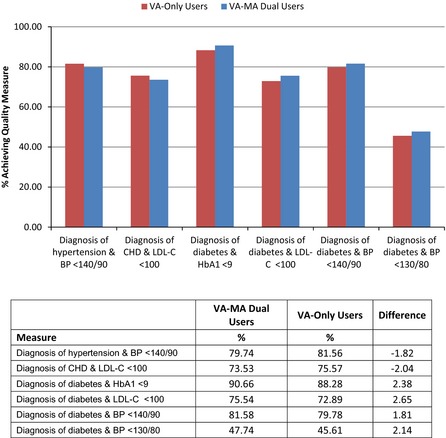
VA External Peer Review Process (EPRP) Quality Performance among VA‐Only Users and Dual VA–MA Users (Hypertension n = 3,881; CHD n = 1,742; Diabetes n = 2,623)
In propensity score analyses, we matched VA‐only users to dual VA and MA users (696 matched pairs with diabetes, 921 matched pairs with hypertension, 382 matched pairs with CHD). Only 3 percent of VA‐only users could not be matched to dual users. Propensity score matching improved the covariate balance between VA‐only users and VA–MA dual users (mean propensity score in matched groups: 0.30) (Table 2; Table S2). In the matched cohorts, VA‐only users and dual users were similar with respect to mean age, gender, and race distribution, VA priority enrollment status, comorbidity, and geographic measures of educational attainment and income. VA EPRP quality measures for matched VA‐only users and dual VA–MA users were also similar (p > .05 for all differences). Between‐group differences ranged from a 3.2 percentage point difference (95 percent CI: −1.8 to 8.2) favoring VA‐only users in the proportion of CHD patients with controlled cholesterol to a 2.2 percentage point difference (95 percent CI: −2.4 to 6.6) favoring dual users in the proportion of diabetes patients with controlled blood pressure. In regression analyses adjusting for enrollee characteristics, health status, and number of VA outpatient visits, the quality differences between VA‐only and dual VA–MA users remained small (p > .05 for all differences). Figure 3 presents the unadjusted, regression‐adjusted, and propensity score–matched differences between the two groups.
Table 2.
Characteristics of Propensity Score‐Matched Individuals with Diabetes, Hypertension, and CHD Dually Enrolled in the VA Health Care System and Medicare Advantage Plans in 2008–2009
| Diabetes | Hypertension | CHD | ||||
|---|---|---|---|---|---|---|
| VA‐Only Use | Dual VA–MA Use | VA‐Only Use | Dual VA–MA Use | VA‐Only Use | Dual VA–MA Use | |
| n | 696 | 696 | 921 | 921 | 382 | 382 |
| Agea | ||||||
| Mean (SD) | 66.4 (6.5) | 66.1 (7.3) | 71.0 (8.5) | 70.6 (9.3) | 67.7 (5.8) | 66.9 (6.3) |
| Sex | ||||||
| Male (%) | 98.3 | 98.3 | 98.1 | 98.1 | 99.0 | 99.0 |
| Female (%) | 1.7 | 1.7 | 1.9 | 1.9 | 1.0 | 1.0 |
| Racea | ||||||
| White (%) | 77.9 | 80.6 | 78.3 | 80.1 | 85.1 | 86.4 |
| Black (%) | 18.4 | 15.1 | 18.6 | 14.8 | 10.7 | 10.0 |
| Other (%) | 3.7 | 4.3 | 3.1 | 5.1 | 4.2 | 3.6 |
| Regiona | ||||||
| Northeast (%) | 17.0 | 15.2 | 15.2 | 15.4 | 16.2 | 14.7 |
| Midwest (%) | 25.1 | 23.6 | 29.1 | 20.4 | 26.4 | 22.5 |
| South (%) | 31.9 | 38.2 | 30.3 | 36.1 | 29.9 | 38.7 |
| West (%) | 26.0 | 23.0 | 25.4 | 28.1 | 27.5 | 24.1 |
| Medicaid and special needs plan enrollment | ||||||
| Enrolled in Medicaid (%) | 1.9 | 1.3 | 2.4 | 2.0 | 1.8 | 1.3 |
| Enrolled in SNP (%) | 9.0 | 9.0 | 7.4 | 7.1 | 7.6 | 7.6 |
| VA enrollment priority statusb | ||||||
| High priority—Groups 1–6 (%) | 19.9 | 25.0 | 76.2 | 75.4 | 75.9 | 73.3 |
| Low priority—Groups 7–8 (%) | 80.2 | 75.0 | 23.8 | 24.6 | 24.1 | 26.7 |
| Number of comorbid conditionsc | ||||||
| Mean (SD) | 5.1 (2.4) | 5.1 (2.3) | 4.3 (2.4) | 4.3 (2.4) | 5.1 (2.7) | 4.8 (2.3) |
| Comorbid conditions | ||||||
| AIDS (%) | 0.1 | 0.0 | 0.0 | 0.1 | 0.0 | 0.3 |
| Alchohol abuse (%) | 7.2 | 7.0 | 9.7 | 8.0 | 8.6 | 6.5 |
| Blood loss anemia (%) | 0.3 | 0.7 | 0.5 | 0.4 | 1.3 | 0.5 |
| Chronic pulmonary disease (%)c | 27.9 | 30.2 | 30.9 | 29.8 | 38.3 | 31.2 |
| Coagulopathy (%) | 4.6 | 5.3 | 6.1 | 5.0 | 6.3 | 7.1 |
| Congestive heart failure (%) | 17.0 | 17.1 | 16.1 | 16.0 | 25.9 | 24.4 |
| Deficiency anemia (%) | 21.6 | 21.7 | 22.6 | 22.5 | 19.4 | 18.3 |
| Depression (%)c | 26.4 | 27.3 | 24.5 | 23.9 | 28.8 | 22.0 |
| Diabetes—complicated (%) | 48.0 | 47.6 | 21.3 | 21.5 | 21.7 | 23.3 |
| Diabetes—uncomplicated (%) | 98.0 | 96.3 | 44.5 | 44.1 | 45.3 | 48.7 |
| Drug abuse (%) | 4.0 | 4.6 | 4.8 | 3.2 | 3.1 | 1.8 |
| Fluid and electrolyte disorder (%) | 15.8 | 16.2 | 16.6 | 15.1 | 15.7 | 14.9 |
| Hypertension—complicated (%) | 93.1 | 93.5 | 97.5 | 97.6 | 90.1 | 92.4 |
| Hypothyroidism (%) | 9.3 | 9.3 | 10.3 | 10.6 | 9.2 | 9.7 |
| Liver disease (%) | 3.3 | 3.4 | 2.4 | 2.9 | 3.1 | 1.3 |
| Lymphoma (%) | 0.9 | 0.6 | 0.8 | 0.8 | 1.0 | 0.5 |
| Metastatic cancer (%) | 0.6 | 0.7 | 1.0 | 0.8 | 0.8 | 1.0 |
| Myocardial infarction (%)b , c | 9.8 | 6.6 | 7.6 | 6.5 | 67.8 | 59.7 |
| Neurological disorder (%) | 6.5 | 5.5 | 6.8 | 7.4 | 7.8 | 5.5 |
| Obesity (%) | 47.6 | 48.7 | 31.3 | 32.4 | 34.8 | 33.0 |
| Paralysis (%) | 3.2 | 2.4 | 2.8 | 2.6 | 4.7 | 3.1 |
| Peripheral vascular disorder (%) | 18.2 | 17.5 | 18.9 | 18.0 | 23.8 | 23.8 |
| Psychoses (%) | 20.1 | 19.8 | 16.3 | 16.5 | 16.0 | 14.7 |
| Pulmonary circulation disorder (%) | 1.4 | 1.7 | 2.6 | 2.1 | 3.9 | 3.1 |
| Renal failure (%) | 5.2 | 5.7 | 5.5 | 6.4 | 4.2 | 3.9 |
| Rheumatoid arthritis (%) | 2.7 | 2.7 | 3.4 | 3.0 | 2.1 | 2.1 |
| Tumor—without metastasis (%) | 12.6 | 14.5 | 17.2 | 17.7 | 13.1 | 14.7 |
| Ulcer (%) | 0.1 | 0.2 | 0.1 | 0.0 | 0.3 | 0.3 |
| Valvular disease (%) | 5.0 | 4.7 | 7.0 | 8.5 | 10.2 | 6.5 |
| Weight loss (%) | 2.6 | 3.0 | 5.4 | 4.5 | 3.1 | 3.4 |
| Distance from zip code to VAa | ||||||
| Mean (SD) | 11.5 (11.3) | 12.9 (12.1) | 10.5 (10.0) | 12.0 (10.7) | 12.1 (11.3) | 13.1 (11.5) |
| Proportion of persons >65 with some college education in zip code | ||||||
| Mean (SD) | 29.3 (12.9) | 29.4 (12.8) | 30.4 (13.4) | 30.0 (13.3) | 30.0 (12.3) | 30.3 (13.2) |
| Median household income for persons 65–74 in zip code | ||||||
| Mean (SD) | $29,332 ($9,221) | $29,466 ($8,740) | $29,859 ($9,464) | $29,535 ($8,725) | $29,689 ($8,658) | $29,818 ($8,660) |
| Median household income for persons >75 in zip code | ||||||
| Mean (SD) | $21,559 ($7,505) | $21,570 ($7,623) | $21,812 ($7,277) | $21,664 ($6,836) | $21,580 ($6,283) | $22,008 ($7,416) |
| Propensity score | ||||||
| Mean (SD) | 0.3 (0.1) | 0.3 (0.1) | 0.3 (0.1) | 0.3 (0.1) | 0.3 (0.1) | 0.3 (0.1) |
Individuals with more than one of the chronic conditions of interest were included in all relevant matched cohorts.
p‐value for difference in hypertension cohort <.05.
p‐value for difference in CHD cohort <.05.
p‐value for difference in diabetes cohort <.05.
Figure 3.

Unadjusted and Adjusted Differences (with 95 Percent Confidence Intervals) in VA EPRP Quality Performance for VA–MA Dual Users Relative to VA‐Only Users in Regression Analyses (Hypertension n = 3,881; CHD n = 1,742; Diabetes n = 2,623) and Propensity Score Analyses (Hypertension n = 1,842; CHD n = 764; Diabetes n = 1,392)
In the sensitivity analysis evaluating a three‐level characterization of dual use, we found that 2,976 individuals (44.8 percent) predominantly used VA services, having VA reliance greater than 0.8. An additional 3,039 individuals (45.7 percent) were classified as dual VA–MA users, having VA reliance between 0.2 and 0.8. The remaining 628 dual enrollees (9.5 percent) primarily used MA services (VA reliance <0.2) (Table S3). Again, VA EPRP intermediate outcome quality measures were comparable for all three groups (Figure S2). We did not observe a significant association between the dual‐use category and the five intermediate outcomes of interest.
In an additional analysis to assess the potential confounding effect of the number of VA outpatient visits on quality outcomes measured by the VA, we observed no association between more frequent VA outpatient service use and better outcomes, and we found no evidence of a threshold number of VA outpatient visits beyond which outcomes are improved (Figure S3). In addition, repeating the regression analysis including the 478 individuals with fewer than two VA outpatient visits did not substantially alter the magnitude or direction of effect estimates (p > .05 for all differences).
Discussion
In this study of the association of dual VA and MA health system use with the quality of care among veterans with diabetes, hypertension, and CHD, we found no significant differences in intermediate health outcomes between dual enrollees who use services in both the VA and MA and those who exclusively use VA services. Results were similar when classifying enrollees as predominant VA users, dual VA and MA users, and predominant MA users. We also noted a high intensity of VA service utilization, even among dual VA and MA users. Despite extensive VA service utilization overall, dually enrolled individuals with fewer VA outpatient visits had comparable outcomes to those with many VA outpatient encounters, suggesting the absence of a threshold number of VA visits for achieving better intermediate outcomes in diabetes, hypertension, and heart disease.
Among dual enrollees, the group of veterans exclusively using the VA was younger, much more likely to be black, and had lower socioeconomic status and more comorbidity. Prior studies of dual use of VA and Medicare fee‐for‐service care have also found younger and black enrollees to be more likely to be exclusive VA users (Humensky et al. 2012). Unlike previous studies which found dual VA and Medicare users to have poorer health status, our analysis found exclusive VA users to have more comorbid conditions (Hynes et al. 2007; Humensky et al. 2012). Additionally, we noted only minor differences in the mean distance to the nearest VA facility for exclusive VA users and dual users (11.1 miles vs. 12.1 miles). Several studies have reported larger differences in proximity to a VA facility between exclusive VA‐only users and dual VA and Medicare users, with VA‐only users generally residing nearer to VA facilities (Burgess and DeFiore 1994; Hynes et al. 2007; Carey et al. 2008). Similarly, Petersen et al. (2010) found that dual VA and Medicare fee‐for‐service enrollees with a greater differential distance to a VA facility relative to the nearest Medicare hospital had lesser VA outpatient reliance.
Prior studies have found that VA reliance has a unique bimodal distribution with peaks at 0 (indicating exclusive non‐VA use) and 1 (indicating exclusive VA reliance), and lower proportions of veterans between 0 and 1 who simultaneously use VA and non‐VA services. VA reliance also differs between types of services and by clinical condition (Petersen et al. 2010; Liu et al. 2013). This prior work informed our decision to compare VA‐only users with dual VA–MA users for specific clinical outcomes and, in a sensitivity analysis, to examine outcomes among three strata of reliance. Our study adds to the existing literature about multiple system utilization by presenting alternative methods for categorizing dual use based on VA reliance. We noted only minor differences between exclusive VA users (VA reliance of 1.0) and dual users who relied primarily on VA services (VA reliance >0.8). Future studies comparing the relationship between dual use and the quality of care must carefully consider the unique nature of VA reliance. The observed relationship between dual use and quality of care may depend on how an analysis handles VA reliance as a predictor of outcomes.
Several previous studies of single VA medical centers have characterized the extent of dual VA and Medicare HMO service use (DeVito, Morgan, and Virnig 1997; Passman et al. 1997; Hester, Cook, and Robbins 2005). In our sample, approximately one quarter of dual enrollees received no outpatient care through their MA plan. This finding is consistent with those of Hester, Cook, and Robbins (2005) in a survey of Medicare HMO enrollees receiving primary care at the Denver VA. On average, we found that dual VA and MA users with at least two VA visits had more than half of their total annual outpatient encounters at the VA. An internal VA study using data from 1996 also found that dually enrolled patients received substantial amounts of care in the VA (Fisher et al. 1998). Relative to previous studies of dual use, the veterans in this study made particularly intensive use of outpatient services, both in the VA and overall. As our sample was restricted to veterans with chronic conditions—many of whom became eligible for VA coverage via a service‐connected disability—this degree of outpatient utilization relative to the general population is not unexpected.
There is limited evidence about the clinical consequences of dual enrollment in the VA and MA. Our study is the first to compare quality outcomes for dually enrolled individuals exclusively using the VA with outcomes among those using both VA and MA services. Helmer et al. (2008) similarly examined control of glycosylated hemoglobin (as measured by the VA in 2000) in a large sample of dual VA and Medicare fee‐for‐service enrollees, finding that dual users had worse diabetes control than VA‐only users. Of note, the magnitude of reported difference was fairly small. The results of our analysis also show only a small difference between groups. Moreover, quality did not significantly differ between predominant VA users and predominant MA users.
Although we found no evidence of the quality care being negatively impacted by dual use of VA and MA services, we observed no apparent benefit from dual‐system use with respect to intermediate health outcomes, despite a duplication of federal expenditure for dually enrolled individuals. A prior study of dual VA and MA utilization estimated that the total cost of Medicare‐covered services spent in the VA to deliver care to MA enrollees from 2004 to 2009 was approximately $13.0 billion (Trivedi et al. 2012). Because the VA is prohibited by the Social Security Act from collecting reimbursements from the Medicare program, MA plans benefit when dual enrollees receive a greater share of their care in the VA. Approximately 25 percent of the dual VA and MA enrollees identified in this study had a VA outpatient reliance of 1.0, indicating exclusive use of VA outpatient services during the year. An additional 20 percent of the sample had a VA reliance greater than 0.8. The MA plans in which these individuals are enrolled stand to profit greatly under these circumstances, providing few or no services despite having been prospectively paid for the beneficiaries’ annual care.
Our study had a number of limitations. Foremost, we were limited to using plan‐reported HEDIS data for information about MA utilization and quality. MA claims and encounter data are not available to researchers, precluding our understanding of conditions treated and care delivered to dual enrollees by MA providers. For this reason, policy makers’ understanding of dual use of VA and MA services has remained limited since Fisher et al. (1998) reported on the subject. An additional limitation relates to the use of HEDIS encounter data for information about dual enrollees’ MA utilization. Landon et al. (2012) noted that these utilization measures are minimally audited, and that they may be more likely to be incomplete as they are not tied to plan payment. Incomplete capture of MA utilization in the HEDIS data may partly explain the lower total number of outpatient encounters observed in dual users.
Because so few individuals in the VA EPRP sample were also sampled for MA HEDIS quality measures, we were unable to conduct analyses of intermediate outcomes as measured by MA plans using this population. The absence of quality indicators from MA may bias our estimates for the dual‐using population in a downward direction (Byrne et al. 2006). We adjusted for the distance to the nearest VA provider, but we were unable to adjust for the differential distance between the nearest VA and nearest in‐network MA provider because this information was not available. We were further limited to comorbidity information available in VA data and therefore are missing comorbidities captured exclusively in MA data. We restricted our analytic sample to individuals having at least two VA outpatient encounters to ensure some assessment of comorbid conditions. As dual VA and MA users had an average of 15.1 VA outpatient visits, the information on comorbidity available in the VA data should be complete for the majority of this group. We also lacked information about Medicaid utilization for the small number of veterans who were triply enrolled. However, results were not materially changed in a sensitivity analysis excluding these individuals.
Our assessment used all outpatient visits, as we were not able to isolate primary care visits that would be most directly related to achieving the outcome measures in this study. Future studies examining dual users’ reliance on the VA and MA for primary care would be of value. Additionally, as outpatient utilization and outpatient chronic condition quality indicators were the focus of our study, it was not possible to examine the role of acute events in determining dual‐system use. Our analysis used observational data, and therefore unmeasured confounding may have biased our effect estimates. Although propensity score and standard multivariate regression analyses provide adequate control for measured confounders, they cannot account for unobserved characteristics. Finally, our study was not designed to determine why veterans choose to enroll in a Medicare Advantage plan, how they make decisions about which system to use for various clinical conditions, or the regional and system factors underlying variations in dual enrollment. Although we employed the conceptual framing by Petersen et al. (2010), alternative models may enhance our understanding of how veterans make decisions about their use of VA and non‐VA care. Given the limited information about these topics, such questions should be assessed in future research.
Dual enrollment in the VA and private managed care plans is expected to intensify following the full implementation of the Affordable Care Act (Kizer 2012). Many VA enrollees who previously lacked other insurance coverage will be eligible to purchase insurance coverage in state‐based insurance exchanges or acquire Medicaid coverage in states that opt to expand Medicaid eligibility. Developing an evidence base for dual use among veterans with private insurance and Medicaid will be critical in predicting the use of services among dually enrolled veterans, understanding how dual use impacts the quality of care for chronically ill populations, and in appropriately allocating federal funds. In addition, Medicare beneficiaries’ enrollment in private MA plans has continued to grow since 2009 and now represents 30 percent of the Medicare population (15.7 million in 2014) (Gold et al. 2014). Therefore, the $3.2 billion that the VA spent to care for MA enrollees in 2009 (Trivedi et al. 2012) is likely to be substantially higher in 2015. Future studies should therefore further examine the determinants and consequences of dual enrollment. If dual enrollment facilitates access to needed care or enhances health outcomes, policy makers should coordinate services and payment across these two federally funded managed care systems.
For the five intermediate outcome measures assessed in this sample, dual VA and MA use was not associated with poorer patient outcomes. Moreover, the VA continues to be the primary source of outpatient care for the majority of dual VA and MA enrollees with diabetes, hypertension, and CHD, even among those who receive care in both systems. The high intensity of VA outpatient service use among VA–MA dual users may explain why intermediate health outcomes are comparable to those achieved by veterans exclusively receiving care from the VA, despite the potential for fragmentation of care with dual use. Although dual use does not appear to erode quality of care, we found no evidence that dual use—and the attendant duplication of federal expenditure—promotes higher quality care.
Supporting information
Appendix SA1: Author Matrix.
Table S1: Utilization of Individuals with Diabetes, Hypertension, and/or CHD Dually Enrolled in the VA Health Care System and Medicare Advantage Plans in 2008–9 (n = 6,643).
Table S2: Utilization of Propensity Score‐Matched Individuals with Diabetes, Hypertension, and CHD Dually Enrolled in the VA Health Care System and Medicare Advantage Plans in 2008–9.
Table S3: Characteristics of Individuals with Diabetes, Hypertension, and/or CHD Dually Enrolled in the VA Health Care System and Medicare Advantage Plans in 2008–9 (n = 6,643), Grouped According to Degree of VA Reliance.
Figure S1: Conceptual Model of Factors Influencing Choice of Health care System, Adapted from Petersen et al. (2010).
Figure S2: VA External Peer Review Process (EPRP) Quality Performance among Predominant VA Users (n = 2,976), Dual VA–MA Users (n = 3,039), and Predominant MA Users (n = 628).
Figure S3: Quality Outcomes across Categories of Annual VA Outpatient Visits in Full Dual VA and MA Enrolled Sample (n = 7,121).
Acknowledgments
Joint Acknowledgment/Disclosure Statement: This study was funded by the VA Health Services Research & Development (HSR&D) Service. The funding agency had no role in the design and conduct of the study; the collection, management, analysis, and interpretation of the data; the preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication. A copy of the approved manuscript will be shared with the funding agency prior to publication. Drs. Cooper, Yoon, Charlton, Wilson, Kizer, Trivedi, and Ms. Jiang have no disclosures. Dr. Mor reports grants from Brown University during the conduct of the study; personal fees from PointRight, Inc., HCRManorCare, Inc., and NaviHealth, Inc.; and board membership for Hospice Home Care of Rhode Island outside the submitted work.
Disclosures: None.
Disclaimers: None.
References
- Borowsky, S. J. , and Cowper D. C.. 1999. “Dual Use of VA and Non‐VA Primary Care.” Journal of General Internal Medicine 14 (5): 274–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgess, J. F. , and DeFiore D. A.. 1994. “The Effect of Distance to VA Facilities on the Choice and Level of Utilization of VA Outpatient Services.” Social Science and Medicine 39 (1): 95–104. [DOI] [PubMed] [Google Scholar]
- Byrne, M. M. , Kuebeler M., Pietz K., and Petersen L. A.. 2006. “Effect of Using Information from Only One System for Dually Eligible Health Care Users.” Medical Care 44 (8): 768–73. [DOI] [PubMed] [Google Scholar]
- Carey, K. , Montez‐Rath M. E., Rosen A. K., Christiansen C. L., Loveland S., and Ettner S. L.. 2008. “Use of VA and Medicare Services by Dually Eligible Veterans with Psychiatric Problems.” Health Services Research 43 (4): 1164–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper, A. L. , and Trivedi A. N.. 2012. “Fitness Memberships and Favorable Selection in Medicare Advantage Plans.” New England Journal of Medicine 366 (2): 150–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeVito, C. A. , Morgan R. O., and Virnig B. A.. 1997. “Use of Veterans Affairs Medical Care by Enrollees in Medicare HMOs.” New England Journal of Medicine 337 (14): 1013–4. [DOI] [PubMed] [Google Scholar]
- Elixhauser, A. , Steiner C., Harris D. R., and Coffey R. M.. 1998. “Comorbidity Measures for Use with Administrative Data.” Medical Care 36 (1): 8–27. [DOI] [PubMed] [Google Scholar]
- Fisher, E. S. , Wright S. M., Weeks W., Passman L. J., and Hults D.. 1998. Use of VA Services by Medicare HMO Enrollees. Washington, DC: Veterans Administration Office of Policy, Planning and Performance. [Google Scholar]
- Fleming, C. , Fisher E. S., Chang C. H., Bubolz T. A., and Malenka D. J.. 1992. “Studying Outcomes and Hospital Utilization in the Elderly: The Advantages of a Merged Data Base for Medicare and Veterans Affairs Hospitals.” Medical Care 30: 377–91. [DOI] [PubMed] [Google Scholar]
- Gold, M. , Jacobson G., Damico A., and Neuman T.. 2014. Medicare Advantage 2014 Spotlight: Enrollment Market Update. Menlo Park, CA: The Henry J. Kaiser Family Foundation. [Google Scholar]
- Helmer, D. , Sambamoorthi U., Shen Y., Tseng C. L., Rajan M., Tiwari A., Maney M., and Pogach L.. 2008. “Opting Out of an Integrated Healthcare System: Dual‐System Use Is Associated with Poorer Glycemic Control in Veterans with Diabetes.” Primary Care Diabetes 2 (2): 73–80. [DOI] [PubMed] [Google Scholar]
- Hester, E. J. , Cook D. J., and Robbins L. J.. 2005. “The VA and Medicare HMOs—Complementary or Redundant?” New England Journal of Medicine 353 (12): 1302–3. [DOI] [PubMed] [Google Scholar]
- Humensky, J. , Caretta H., De Groot K., Brown M. M., Tarlov E., and Hynes D. M.. 2012. “Service Utilization of Veterans Dually Eligible for VA and Medicare Fee‐for‐Service: 1999‐2004.” Medicare and Medicaid Research Review 2 (3): E1–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hynes, D. M. , Koelling K., Stroupe K., Arnold N., Mallin K., Sohn M. W., Weaver F. M., Manheim L., and Kok L.. 2007. “Veterans’ Access to and Use of Medicare and Veterans Affairs Health Care.” Medical Care 45 (3): 214–23. [DOI] [PubMed] [Google Scholar]
- Jia, H. , Zheng Y., Reker D. M., Cowper D. C., Wu S. S., Vogel W. B., Young G. C., and Duncan P. W.. 2007. “Multiple System Utilization and Mortality for Veterans with Stroke.” Stroke 38 (2): 355–60. [DOI] [PubMed] [Google Scholar]
- Keyhani, S. , Ross J. S., Hebert P., Dellenbaugh C., Penrod J. D., and Siu A. L.. 2007. “Use of Preventive Care by Elderly Male Veterans Receiving Care through the Veterans Health Administration, Medicare Fee‐for‐Service, and Medicare HMO Plans.” American Journal of Public Health 97: 2179–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kizer, K. W. 2012. “Veterans and the Affordable Care Act.” Journal of the American Medical Association 307 (8): 789–90. [DOI] [PubMed] [Google Scholar]
- Landon, B. E. , Zaslavsky A. M., Saunders R. C., Pawlson L. G., Newhouse J. P., and Ayanian J. Z.. 2012. “Analysis of Medicare Advantage HMOs Compared with Traditional Medicare Shows Lower Use of Many Services during 2003‐09.” Health Affairs 31: 2609–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, C. , Manning W. G., Burgess J. F., Hebert P. L., Bryson C. L., Fortney J., Perkins M., Sharp N., and Maciejewski M. L.. 2011. “Reliance on Veterans Affairs Outpatient Care by Medicare‐Eligible Veterans.” Medical Care 49: 911–7. [DOI] [PubMed] [Google Scholar]
- Liu, C. , Burgess J. F., Manning W. G., and Maciejewski M. L.. 2013. “Beta‐Binomial Regression and Bimodal Utilization.” Health Services Research 48 (5): 1769–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maciejewski, M. L. , Birken S., Perkins M., Burgess J. F., Sharp N., and Liu C.. 2009. “Medicare Managed Care Enrollment by Disability‐Eligible and Age‐Eligible Veterans.” Medical Care 47: 1180–5. [DOI] [PubMed] [Google Scholar]
- Morgan, R. O. , Petersen L. A., Hasche J. C., Davila J. A., Byrne M. M., Osemene N. I., Wei I. I., and Johnson M. L.. 2009. “VHA Pharmacy Use in Veterans with Medicare Drug Coverage.” American Journal of Managed Care 15 (3): e1–8. [PubMed] [Google Scholar]
- Parsons, L. S. 2001. Reducing Bias in a Propensity Score Matched‐Pair Sample Using Greedy Matching Techniques. Paper presented at the Proceedings of the 26th Annual SAS Users Group International Conference. [Google Scholar]
- Passman, L. J. , Garcia R. E., Campbell L., and Winter E.. 1997. “Elderly Veterans Receiving Care at a Veterans Affairs Medical Center While Enrolled in Medicare‐Financed HMOs.” Journal of General Internal Medicine 12 (4): 247–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersen, L. A. , Byrne M. M., Daw C. N., Hasche J., Reis B., and Pietz K.. 2010. “Relationship between Clinical Conditions and Use of Veterans Affairs Health Care among Medicare‐Enrolled Veterans.” Health Services Research 45 (3): 762–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pizer, S. D. , and Gardner J. A.. 2011. “Is Fragmented Financing Bad for Your Health?” Inquiry 48 (2): 109–22. [DOI] [PubMed] [Google Scholar]
- Shen, Y. , Hendricks A., Zhang S., and Kazis L. E.. 2003. “VHA Enrollees’ Health Care Coverage and Use of Care.” Medical Care Research and Review 60 (2): 253–67. [DOI] [PubMed] [Google Scholar]
- Trivedi, A. N. , Grebla R. C., Jiang L., Yoon J., Mor V., and Kizer K. W.. 2012. “Duplicate Federal Payments for Dual Enrollees in Medicare Advantage Plans and the Veterans Affairs Health Care System.” Journal of the American Medical Association 308 (1): 67–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolinsky, F. D. , Miller T. R., An H., Brezinski P. R., Vaughn T. E., and Rosenthal G. E.. 2006. “Dual Use of Medicare and the Veterans Health Administration: Are There Adverse Health Outcomes?” BMC Health Services Research 6: 131. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.
Table S1: Utilization of Individuals with Diabetes, Hypertension, and/or CHD Dually Enrolled in the VA Health Care System and Medicare Advantage Plans in 2008–9 (n = 6,643).
Table S2: Utilization of Propensity Score‐Matched Individuals with Diabetes, Hypertension, and CHD Dually Enrolled in the VA Health Care System and Medicare Advantage Plans in 2008–9.
Table S3: Characteristics of Individuals with Diabetes, Hypertension, and/or CHD Dually Enrolled in the VA Health Care System and Medicare Advantage Plans in 2008–9 (n = 6,643), Grouped According to Degree of VA Reliance.
Figure S1: Conceptual Model of Factors Influencing Choice of Health care System, Adapted from Petersen et al. (2010).
Figure S2: VA External Peer Review Process (EPRP) Quality Performance among Predominant VA Users (n = 2,976), Dual VA–MA Users (n = 3,039), and Predominant MA Users (n = 628).
Figure S3: Quality Outcomes across Categories of Annual VA Outpatient Visits in Full Dual VA and MA Enrolled Sample (n = 7,121).


