Abstract
Objective
To examine how similar racial/ethnic disparities in clinical quality (Healthcare Effectiveness Data and Information Set [HEDIS]) and patient experience (Consumer Assessment of Healthcare Providers and Systems [CAHPS]) measures are for different measures within Medicare Advantage (MA) plans.
Data Sources/Study Setting
5.7 million/492,495 MA beneficiaries with 2008–2009 HEDIS/CAHPS data.
Study Design
Binomial (HEDIS) and linear (CAHPS) hierarchical mixed models generated contract estimates for HEDIS/CAHPS measures for Hispanics, blacks, Asian‐Pacific Islanders, and whites. We examine the correlation of within‐plan disparities for HEDIS and CAHPS measures across measures.
Principal Findings
Plans with disparities for a given minority group (vs. whites) for a particular measure have a moderate tendency for similar disparities for other measures of the same type (mean r = 0.51/.21 and 53/34 percent positive and statistically significant for CAHPS/HEDIS). This pattern holds to a lesser extent for correlations of CAHPS disparities and HEDIS disparities (mean r = 0.05/0.14/0.23 and 4.4/5.6/4.4 percent) positive and statistically significant for blacks/Hispanics/API.
Conclusions
Similarities in CAHPS and HEDIS disparities across measures might reflect common structural factors, such as language services or provider incentives, affecting several measures simultaneously. Health plan structural changes might reduce disparities across multiple measures.
Keywords: Medicare, disparities, CAHPS, HEDIS, race/ethnicity
Medicare beneficiaries may choose between fee‐for‐service (FFS) Medicare coverage or a Medicare Advantage (MA) managed care plan. MA has been particularly attractive to racial/ethnic minorities. As of 2010, 29 percent of African Americans, 33 percent of Asian Americans, and 36 percent of Hispanic Medicare beneficiaries were enrolled in MA compared to 25 percent of whites (America's Health Insurance Plans Centers for Policy and Research 2012). The popularity of MA among racial/ethnic minorities may be due to the relatively lower out‐of‐pocket costs of managed care (net of any MA premiums) compared to FFS (Atherly and Thorpe 2005). This may be particularly appealing to racial/ethnic minorities, since they tend to be overrepresented among the lower income groups. Despite the popularity of MA among racial/ethnic minorities, prior studies using Healthcare Effectiveness Data and Information Set (HEDIS) (Schneider, Zaslavsky, and Epstein 2002; Trivedi et al. 2005, 2006; Chou et al. 2007) and Consumer Assessment of Healthcare Providers and Systems (CAHPS) data (Lurie et al. 2003; Fongwa et al. 2008; Weech‐Maldonado et al. 2008; Elliott et al. 2011; Haviland et al. 2012) have noted racial/ethnic disparities in care among MA enrollees, as well as in FFS Medicare (Elliott et al. 2011). The observed disparities in care may be a result of racial/ethnic minorities receiving lower quality care than whites within the same plans (within‐plan differences) and/or racial/ethnic minorities being clustered in plans with lower quality care (between‐plan differences) (Weech‐Maldonado et al. 2004; Haviland et al. 2012).
Prior studies have shown that minorities tend to receive care in lower performing Medicare health plans, so at least some of the observed disparities in care can be attributed to between‐plan differences (Trivedi et al. 2005, 2006; Goldstein et al. 2010; Haviland et al. 2012; Lyratzopoulos et al. 2012). However, research suggests that within‐plan differences also account for a substantial proportion of disparities in quality of care (Weech‐Maldonado et al. 2004; Trivedi et al. 2006; Haviland et al. 2012). For example, Trivedi et al. (2006) found that more than 70 percent of disparities between blacks and whites for clinical performance measures in MA were due to within‐plan rather than between‐plan differences. Similarly, Haviland et al. (2012) found that over 85 percent of the overall disparities in Medicare Part D plan experiences (access to and information about prescription medicines) among Hispanics were due to within‐plan differences.
This paper examines the extent to which within‐plan racial/ethnic disparities in clinical performance and patient experiences are similar for different measures and different racial/ethnic groups to better understand the possible causes of these disparities. While prior research has examined the extent to which patient‐level disparities in clinical performance and patient experiences in MA are explained by between‐ and within‐plan differences, relatively little is known about the within‐plan correlations of these patient‐level disparities across measures and racial/ethnic groups.
We consider three different types of within‐plan correlations of CAHPS and HEDIS disparities in this paper: (1) across measures within a given domain (CAHPS or HEDIS), (2) across measures of different domains, and (3) across racial/ethnic groups (Figure 1). First, for a given racial/ethnic group, there may be correlations in the disparities across measures within the CAHPS and HEDIS domains, which may suggest that a common factor is driving the disparities across measures. Second, the racial/ethnic disparities for a given minority group for CAHPS measures may be related to HEDIS disparities for the same group in the same plans. This might indicate similar underlying mechanisms affecting disparities in both patient experience (CAHPS) and clinical processes of care (HEDIS). Finally, large or small disparities for one minority racial/ethnic group may be associated with similar disparities for other minority groups. This may suggest barriers to care or positive organizational attributes that are not specific to a given language or group and that affect several minority groups disproportionately.
Figure 1.
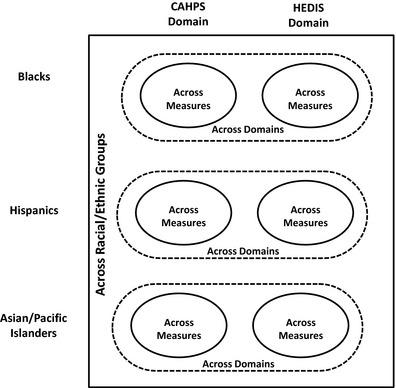
Racial/Ethnic Within‐Group and Across‐Group Correlations in CAHPS and HEDIS Measures
Conceptual Framework
The systems approach views health care organizations as comprised of interrelated and interdependent subsystems, such as patient care, ancillary services, professional staff, financial, informational, physical, and administrative subsystems (Longest, Rakich, and Darr 2000). The organization's capabilities in deploying and coordinating resources across subsystems will influence organizational performance. Similarly, Donabedian's (1988) Structure‐Process‐Outcome model posits that appropriate structures increase the likelihood of good processes and outcomes of care. Structure includes the availability, organization, and quality of professional and organizational resources that can be associated with providing care, such as operating capacities and human resources (Binns 1991). Process refers to actions that are performed on or done to patients, such as communication between staff and patients, or clinical practices (Gustafson and Hundt 1995). Outcomes are the states that result from care processes, such as improvements in health status or patient experience of care (Unruh and Wan 2004; Cella et al. 2007; Hays 2009).
We argue that system/organizational factors or structures may facilitate or hinder appropriate care for racial/ethnic minorities (Griffith et al. 2007). One such structural factor is organizational cultural competency because it implies having policies and practices in place that facilitate the delivery of appropriate services to diverse populations, including understanding the needs of the population that they serve, training staff to be culturally competent, and providing interpreters and translation services. Cultural competency policies and practices are intended to facilitate cross‐cultural interactions across a range of sociocultural factors, such as race/ethnicity, nationality, language, health literacy, gender, and socioeconomic status. On the other hand, lack of cultural competency may result in system barriers to care for racial/ethnic minorities, and ultimately lead to disparities in outcomes (Institute of Medicine 2003).
Organizational/system factors, such as presence or lack of cultural competency, are expected to impact multiple process measures simultaneously. In this paper, we use CAHPS and HEDIS as process measures of care. While the CAHPS domain includes measures of patient experiences with care, the HEDIS domain captures measures of clinical performance, particularly preventive care.
For a given racial/ethnic group, we expect to observe correlation in disparities across measures of the same domain (CAHPS or HEDIS). Barriers related to cultural and language differences, low health literacy, or lower socioeconomic status may affect several measures of the same domain (patient experience or clinical quality) simultaneously (Haviland et al. 2012). For example, health educational strategies that take into account low health literacy may result in increased use of HEDIS preventive screenings, such as breast cancer and colorectal cancer screenings. Therefore, we hypothesize that:
Hypothesis 1: For a given racial/ethnic minority group, there is a positive correlation in the disparities (vs. non‐Hispanic whites) across measures of the same domain (CAHPS or HEDIS).
Addressing barriers related to cultural and language differences, low health literacy, or lower socioeconomic status may affect both CAHPS and HEDIS measures simultaneously (Haviland et al. 2012). For example, providing interpreter services to address language barriers for a given racial/ethnic group of a plan may increase use of preventive care services and improve perceptions of care, resulting in both lower HEDIS and CAHPS disparities for the same group in the same plan. However, we expect a weaker correlation of disparities across CAHPS and HEDIS measures compared to correlation of measures within the same domain (CAHPS or HEDIS) since the underlying structures or mechanisms driving CAHPS and HEDIS performance may be different. For example, computerized reminders for preventive services, or translation of educational materials into other languages, are more likely to affect clinical performance (HEDIS) measures than CAHPS measures, while cultural competency training of staff is more likely to affect patient experience (CAHPS) measures. Furthermore, CAHPS measures are case‐mix adjusted, while HEDIS measures are not risk adjusted. This leads us to hypothesize that:
Hypothesis 2: For a given racial/ethnic minority group, there is a positive correlation in the disparities (vs. non‐Hispanic whites) across CAHPS and HEDIS measures. However, these are smaller correlations compared to the correlation of disparities of measures within the CAHPS and HEDIS domains.
Large or small disparities for one minority racial/ethnic group may be associated with similar disparities for other minority groups. This may suggest barriers to care or positive organizational attributes that are not specific to a given language or group and that affect several minority groups disproportionately. For example, cultural competency training of providers and staff may improve patient perceptions of care across racial/ethnic groups. Similarly, health literacy strategies may address disparities across groups. However, we expect the correlations of disparities in CAHPS and HEDIS measures across racial/ethnic groups to be smaller compared to within‐group correlations.
Hypothesis 3: There is a positive correlation in the disparities of CAHPS and HEDIS measures across racial/ethnic minority groups (vs. non‐Hispanic whites). However, these correlations are smaller compared to the disparities of CAHPS and HEDIS measures within the same racial/ethnic minority group.
Methods
Data
Data for this study came from two sources: the MA CAHPS survey and MA HEDIS data, both for 2008 and 2009. The Centers for Medicare & Medicaid Services (CMS) conducts the MA CAHPS survey to collect, analyze, and report data on beneficiaries' experiences with their health care and services. The MA CAHPS survey is a mail survey with telephone follow‐up based on a stratified random sample of MA beneficiaries, with contracts as strata. The 2008 (2009) MA CAHPS survey received responses from 373,334 (378,255) MA enrollees, with a 64.9 percent (64.8 percent) response rate. HEDIS consists of health care process measures and intermediate outcome measures that are based on administrative data, supplemented in some cases by information obtained from individuals' medical records (National Committee for Quality Assurance 2011). Most MA plans are required to report both CAHPS and HEDIS measures to CMS annually. An MA contract, also called a health plan, is a set of offerings (or benefit packages) from a single sponsor in a specific geographic area. We pooled data for 2 years to improve the precision of our contract‐level estimates for racial/ethnic subgroups (Martino et al. 2013).
Sample
The MA CAHPS sample consists of MA enrollees, either with Part D prescription coverage (MA‐PD) or without such coverage (MA‐Only). The analytic sample includes 492,495 MA beneficiaries from any of 441 contracts operating in 2008 or 2009. Responses come from 2008 and 2009, with few respondents included in both years. The HEDIS sample includes data for 5.7 million MA beneficiaries in the period of 2008–2009 that had at least one HEDIS score across 382 reporting contracts operating in 2009. The number of contracts available for CAHPS and HEDIS measure differs because the two sets of measures have slightly different eligibility requirements and some contracts are eligible for some measures but not others (www.medicare.gov).
Variables
The dependent variables consist of CAHPS and HEDIS measures (Tables S1 and S2), which have been found to be reliable for health plan performance reporting by race/ethnicity (Martino et al. 2013) and more generally (Hays et al. 1999; Hargraves, Hays, and Cleary 2003; Martino et al. 2009). The CAHPS measures include three composite measures related to health care contract and care received (getting needed care, getting care quickly, and customer service), and two prescription drug composite measures (getting needed prescription drugs and getting prescription drug information). Following standard approaches (Centers for Medicare & Medicaid Services 2014), responses to each CAHPS item were linearly transformed to a possible range of 0–100 and averaged within composites. The HEDIS measures include four diabetes care measures (HbA1c testing, retinal eye exam, LDL‐cholesterol [LDL‐C] screening, and kidney disease/nephropathy), two cancer screening measures (breast cancer and colorectal cancer), two beneficiary‐reported immunization items (flu and pneumonia), and one summary measure on monitoring patients who take four specific medications (angiotensin converting enzyme/angiotensin receptor blockers, anticonvulsants, digoxin, and diuretics on a persistent basis [at least 180 days]). All HEDIS measures are coded as dichotomous variables (1 = yes; 0 = no), except for the summary measure on specific medications, which is the mean of one to four dichotomous indicators, depending upon how many apply to a given MA beneficiary.
Race/ethnicity is the main independent variable. For CAHPS, it is derived from two self‐reported measures on the CAHPS survey, one item for Hispanic ethnicity and the other item for race. If the respondents indicated Hispanic ethnicity, following the Census approach, we classify them as Hispanic regardless of races endorsed. If not Hispanic and the respondent endorsed exactly one race, or endorsed Asian and/or Native Hawaiian/Pacific Islander (API) and no other race, we classify them as non Hispanic black, API, American Indian/Alaskan Native (AI/AN), or white. If respondents endorsed two or more races (except the exact combination of Asian and Pacific Islander), we classify them as multiracial. If they are missing race and ethnicity, we classify them as unknown. Due to small sample size, we combined two groups constituting less than 2 percent of the population (non‐Hispanic AI/AN, 0.3 percent, and multiracial, 1.5 percent) with the unknown race/ethnicity category (11.4 percent) to create a single racial/ethnic category (other race/ethnicity) for analytic purposes. This resulted in five racial/ethnic subgroups: Hispanics, non‐Hispanic whites, non‐Hispanic blacks, non‐Hispanic API, and other race/ethnicity. We report results for four racial/ethnic groups: Hispanics, non‐Hispanic whites, non‐Hispanic blacks, and API.
HEDIS data do not include self‐reported race/ethnicity. Although CMS administrative data on race/ethnicity are suitable for identifying black beneficiaries, they do not perform well in identifying Hispanics and Asian/Pacific Islanders (Martino et al. 2009). To address this limitation, we adapted a new method for inferring race/ethnicity from surname and residential address data while taking advantage of the racial/ethnic information present in the CMS administrative data (Martino et al. 2013). For each individual, a vector of probabilities (summing to 1) of being in each of six racial/ethnic groups—Hispanic, black, white, API, AI/AN, and multiracial—is derived. A validation of this method using data from approximately 2 million commercially insured beneficiaries (Martino et al. 2009) found 93 percent concordance with self‐reported race/ethnicity. Although the method performs well for identifying white, black, Hispanic, and API groups, it is not yet practical for AI/AN or multiracial groups. Mean HEDIS scores for a given racial/ethnic group are calculated as the weighted means of all HEDIS observations, using the probability of belonging to the group in question as a weight (Martino et al. 2013). As noted earlier, we report estimates of HEDIS performance only for the four largest racial/ethnic groups.
In the analysis of CAHPS data, we adjusted for standard CAHPS case‐mix adjustors (McCaffrey and Elliott 2008). Five case‐mix variables were self‐reported by beneficiaries: age (18–44, 45–54, 55–64, 65–69, 70–74, 75–79, 80–84, 85, and older), highest completed grade or level of school (8th grade or less; some high school, but did not graduate; high school graduate or GED; some college or 2‐year degree; 4‐year college graduate; more than 4‐year college degree), self‐rated general health (excellent, very good, good, fair, or poor), self‐rated mental health (excellent, very good, good, fair, or poor), and proxy help (none, proxy assisted responded, proxy answered for respondent). Following the practice used for public reporting, the HEDIS analysis does not include case‐mix adjustors; however, there are eligibility criteria based on age and other factors for specific measures that are incorporated into the sample selection for each HEDIS measure (Table S2).
Analysis
We use hierarchical models to generate contract‐level estimates for each of the 14 CAHPS and HEDIS measures for each of four racial/ethnic groups (non‐Hispanic blacks, Hispanics, non‐Hispanic API, and non‐Hispanic whites). We use two‐level binomial (HEDIS measures) and linear (CAHPS measures) mixed‐effect models (Raudenbush and Bryk 2002) using individual‐level CAHPS and HEDIS scores as outcomes and with random contract intercepts. In addition, each model contains fixed effects for an individual's race/ethnicity, which consists of indicators for Hispanic, black, API, and other race (reference group is non‐Hispanic white) in the case of CAHPS. In the case of HEDIS, fixed effects are the racial/ethnic probabilities for all groups other than non‐Hispanic whites. The models also include random contract slopes by race/ethnicity (black, Hispanic, API, and other race) (CAHPS only) relative to non‐Hispanic white, which can be thought of as the contract‐specific racial/ethnic disparities. The race/ethnicity fixed effects and the random contract by race/ethnicity effects can be interpreted as if they come from dichotomous indicators (McCaffrey and Elliott 2008). The CAHPS models also include fixed effects for a set of standard case‐mix adjustment variables as previously indicated (Zaslavsky et al. 2001; O'Malley et al. 2005) and are weighted to account for the sample design and nonresponse. Data were weighted to represent the enrolled population of contract‐by‐county combinations, followed by a raking procedure (log‐linear weights by iterative proportional fitting) to match weighted sample and enrolled populations within each contract on gender, age, race/ethnicity, Medicaid, low‐income supplement, and special needs plan status, prescription drug enrollment, and zip‐code level distributions of income, education, and race/ethnicity (Deming and Stephan 1940; Purcell and Kish 1980). Following current practice, we did not use case‐mix adjustment in analyzing HEDIS measures. Fixed effects for year were included in all models.
The resulting contract estimates for each of the 14 CAHPS and HEDIS measures for non‐Hispanic blacks, Hispanics, non‐Hispanic API, and non‐Hispanic whites are “shrunken” in the sense that they are pulled toward the global mean when sample sizes within a contract are small. These shrinkage scores are also known as best linear unbiased predictors (BLUPs) or reliability‐adjusted estimates (Liu, Rong, and Liu 2008). Correlations of BLUPs attempt to estimate what the “true” correlations would be if we had infinite data for each racial/ethnic group in each contract. Correlations calculated on simple estimates rather than BLUPs would be biased toward zero (Spearman 1910).
Using Pearson correlations from the shrunken contract‐level estimates, we calculated (a) within racial/ethnic groups, the correlation of within‐plan disparities across measures in the same domain (CAHPS and HEDIS; Hypothesis 1), (b) the correlation between CAHPS and HEDIS contract‐level disparities within racial/ethnic group (Hypothesis 2), and (c) the correlation of contract‐level disparities within individual CAHPS/HEDIS measures across racial/ethnic groups (Hypothesis 3). We describe the proportion of correlations that are significant using a two‐sided significance criterion (p < .05). In addition, we report mean correlation coefficients as summaries of magnitude. We do not include in our calculations correlations that are based on fewer than 100 individuals per contract or fewer than 10 contracts.
Results
Table 1 shows significant differences in Medicare MA contract enrollment and case‐mix attributes by race/ethnicity. Whites and Hispanics are most likely to be in contracts of which their group constitutes a high proportion, with the average white beneficiary in a contract that is 73 percent white, and the average Hispanic beneficiary in a contract that is 42 percent Hispanic. Corresponding percentages are only 17 percent and 18 percent for blacks and API, respectively. Age, education, and health differ dramatically by race/ethnicity. Beneficiaries under age 65, all of whom are eligible for Medicare via disability, are most common among blacks and least common among API beneficiaries, whereas beneficiaries 80 and older are most common among white and API groups and least common among blacks and Hispanics. Educational attainment is lowest among Hispanic beneficiaries, whereas 4‐year college education is most common among API beneficiaries. Self‐rated overall health is higher for whites and API than other groups.
Table 1.
Contract‐Level Race Proportions and Case‐Mix Adjustors (Percentages) by Race/Ethnicity for Medicare Advantage CAHPS Respondents (2008–2009)
| Total ‡ | White | Hispanic | Black | API | |
|---|---|---|---|---|---|
| N | 492,495 | 321,646 | 53,190 | 40,599 | 12,461 |
| Proportion of 2009 surveys | 54 | 55 | 55 | 56 | 53** |
| Contract‐level race proportions‡ | |||||
| Average contract‐level proportion white | 67 | 73 | 38*** | 57*** | 52*** |
| Average contract‐level proportion Hispanic | 10 | 6 | 42*** | 9*** | 10*** |
| Average contract‐level proportion black | 7 | 6 | 7*** | 17*** | 6** |
| Average contract‐level proportion Asian/Pacific Islander | 2 | 2 | 2*** | 2*** | 18*** |
| Case‐mix adjustors (%) | |||||
| Age | |||||
| 18–44 | 1 | 1 | 2*** | 2*** | <1** |
| 45–54 | 2 | 2 | 4*** | 5*** | 1*** |
| 55–64 | 6 | 5 | 9*** | 10*** | 3*** |
| 65–69 | 23 | 23 | 24** | 23 | 23 |
| 70–74 | 24 | 24 | 25*** | 25*** | 27*** |
| 75–79 | 20 | 21 | 18*** | 18*** | 22* |
| 80–84 | 14 | 15 | 11*** | 11*** | 14 |
| 85 or older | 10 | 10 | 7*** | 7*** | 10 |
| Education | |||||
| Less than 8th grade | 10 | 6 | 34*** | 15*** | 13*** |
| Some high school | 13 | 12 | 17*** | 24*** | 9*** |
| High school diploma/GED | 35 | 38 | 25*** | 31*** | 25*** |
| Some college or 2‐year degree | 24 | 25 | 15*** | 21*** | 20*** |
| Four year college graduate | 8 | 9 | 5*** | 4*** | 17*** |
| More than 4‐year college degree | 9 | 10 | 4*** | 6*** | 16*** |
| Self‐rated general health | |||||
| Excellent | 9 | 9 | 10** | 6*** | 8*** |
| Very good | 27 | 30 | 17*** | 19*** | 28*** |
| Good | 37 | 37 | 32*** | 38** | 41*** |
| Fair | 22 | 19 | 34*** | 30*** | 20 |
| Poor | 5 | 5 | 7*** | 7*** | 4*** |
| Self‐rated mental health | |||||
| Excellent | 31 | 33 | 27*** | 26*** | 27*** |
| Very good | 33 | 35 | 24*** | 28*** | 35 |
| Good | 25 | 24 | 29*** | 31*** | 28*** |
| Fair | 9 | 7 | 17*** | 13*** | 9*** |
| Poor | 2 | 1 | 3*** | 2*** | 2 |
| Proxy help | |||||
| None | 90 | 92 | 75*** | 87*** | 76*** |
| Proxy assisted respondent (exclude answered) | 7 | 5 | 21*** | 10*** | 16*** |
| Proxy answered for respondent | 3 | 3 | 4*** | 3 | 8*** |
Tests compared each race and ethnic group to non‐Hispanic white via three sets of linear regression models predicting each measure category (e.g., eight models for age) from the race/ethnicity indicator.
‡The total includes AI/AN, multiracial, and unknown races.* p <.05, ** p <.01, *** p <.001.
Table 2 summarizes the correlations of within‐plan disparities for each racial/ethnic group (vs. non‐Hispanic whites) across measures within the CAHPS or HEDIS domains (see Tables S3a and S4c for the full set of correlations). There is support for Hypothesis 1; results show consistent tendency for moderately positive associations across CAHPS measures (53 percent positive and significant, mean r = 0.51) and across HEDIS measures (34 percent positive and significant, mean r = 0.21) in contract‐level differences between the scores for a given minority group and whites in that contract. For CAHPS measures, these correlations were higher among API (mean r = 0.85, 100 percent positive and significant out of 3) than among blacks (mean r = 0.28, 33 percent positive and significant out of 2) or Hispanics (mean r = 0.41, 50 percent positive and significant out of 5). For all minority racial/ethnic groups, within‐plan CAHPS correlations were highest among the prescription drug composites, getting needed care, and plan customer service. Among API, getting care quickly was highly correlated with several CAHPS measures (getting needed care, getting prescription drugs, and customer service). For HEDIS measures, these correlations were similar across all racial/ethnic groups: API (mean r = 0.23, 19 percent positive and significant out of 26), blacks (mean r = 0.20, 39 percent positive and significant out of 36), and Hispanics (mean r = 0.20, 39 percent positive and significant out of 14). For all minority racial/ethnic groups, within‐plan HEDIS correlations were highest between the two diabetes care screenings (LDL‐C and HbAlc).
Table 2.
The Correlation of Within‐Plan Disparities (vs. Whites) of Measures within CAHPS and HEDIS Domains by Racial/Ethnic Group
| Meana (Min, Max) | No. of Reliable Correlations | Significant and Positive Correlationsb n (%) | |
|---|---|---|---|
| CAHPS (5 measures) | |||
| Black | 0.278 (0.132, 0.493) | 6 (of 10) | 2 (33) |
| Hispanic | 0.413 (0.125, 0.811) | 10 (of 10) | 5 (50) |
| Asian/Pacific Islander | 0.847 (0.793, 0.877) | 3 (of 10) | 3 (100) |
| Overall | 0.513 (0.125, 0.877) | 19 (of 30) | 10 (53) |
| HEDIS (9 measures) | |||
| Black | 0.201 (−0.072, 0.667) | 36 (of 36) | 14 (39) |
| Hispanic | 0.200 (−0.256, 0.747) | 36 (of 36) | 14 (39) |
| Asian/Pacific Islander | 0.231 (−0.464, 0.705) | 26 (of 36) | 5 (19) |
| Overall | 0.211 (−0.464, 0.747) | 98 (of 108) | 33 (34) |
Statistics for each row are for all non‐diagonal correlation coefficients of within‐plan disparities from a matrix of five CAHPS or nine HEDIS measures, across measures and within racial/ethnic group.
Minimum of 10 contracts with 100 members for the given racial/ethnic group.
p < .05; no significant negative correlation.
Table 3 summarizes the correlations of contract‐level disparities between CAHPS and HEDIS measures within racial/ethnic groups (see Tables S5a–c for the full set of correlations) where there are at least 10 contracts with 100 observations for both measures for the racial/ethnic group in question. The correlations tend to be positive for all racial/ethnic groups (Hispanics: 98 percent [44 of 45], blacks: 80 percent [36 of 45], and API: 24 percent [24 of 45]). This suggests a generally positive relationship between patient experience disparities and clinical process disparities, although few were individually statistically significant (2 for blacks, 7 for Hispanics, and 2 for API). Mean correlation was highest for API (r = 0.23) and lowest for blacks (r = 0.05). This provides support for Hypothesis 2. There were generally positive correlations between CAHPS and HEDIS disparities across all racial/ethnic groups; however, the magnitude of the correlation between CAHPS and HEDIS disparities was smaller compared to the correlation of disparities across measures of the same domain (CAHPS and HEDIS).
Table 3.
The Correlation of Within‐Plan Disparities (vs. White) of CAHPS with HEDIS Measures by Racial/Ethnic Group
| Mean (Min, Max) | No. of Correlationsa | Significant and Positive Correlationsb n (%) | |
|---|---|---|---|
| Black | 0.048 (−0.293, 0.383) | 36 (of 45) | 2 (6) |
| Hispanic | 0.140 (−0.246, 0.693) | 44 (of 45) | 7 (16) |
| Asian/Pacific Islander | 0.230 (−0.259, 0.783) | 11 (of 45) | 2 (18) |
| Overall | 0.139 (−0.293, 0.783) | 91 (of 135) | 11 (12) |
Statistics for each row are for all correlation coefficients of within‐plan disparities from a 5 × 9 matrix of five CAHPS measures with nine HEDIS measures, within racial/ethnic group (that is, maximum of 45 correlations summarized per row).
Minimum of 10 contracts with 100 members for each pair of measures.
p < .05; no significant negative correlation.
Table 4 summarizes the correlations of contract‐level disparities across racial/ethnic groups within individual CAHPS and HEDIS measures (see Tables S6 and S7 for the full set of correlations). There are generally small positive associations across minority racial/ethnic groups in disparities (vs. whites) for the individual CAHPS (80 percent positive, mean r = 0.15, none of 5 statistically significant) and HEDIS (91 percent positive, mean r = 0.24, 8 of 22 positive and statistically significant) measures. This provides limited support for Hypothesis 3. Correlations of CAHPS/HEDIS measures across racial/ethnic groups were generally positive, and strongest between blacks and Hispanics. However, these correlations were generally smaller compared to the correlation in disparities within individual CAHPS/HEDIS measures and few were statistically significant. None of the CAHPS correlation coefficients across racial/ethnic groups were statistically different. Among HEDIS measures, there were positive and significant correlations of disparities across all racial/ethnic groups for monitoring patients on persistent medications, and positive and significant correlations of disparities for blacks and Hispanics for breast cancer screening, HbA1c testing, LDL‐C screening, and colorectal screening.
Table 4.
The Correlation of Within‐Plan Disparities (vs. Whites) across Racial/Ethnic Groups by Measures
| Racial/Ethnic Groups Compared | |||||||
|---|---|---|---|---|---|---|---|
| Black, Hispanic | Black, Asian/Pacific Islander | Hispanic, Asian/Pacific Islander | |||||
| Correlation | No. of Contracts | Correlation | No. of Contracts | Correlation | No. of Contracts | Average Correlation | |
| CAHPS | |||||||
| Getting needed care | 0.157 | 15 | — | <10 | — | <10 | 0.157 |
| Getting care quickly | 0.252 | 30 | — | <10 | −0.324 | 10 | −0.036 |
| Getting prescription drugs | 0.294 | 30 | — | <10 | 0.370 | 10 | 0.332 |
| Overall | 0.234 | — | 0.023 | 0.151 | |||
| HEDIS | |||||||
| Flu immunization | 0.010 | 39 | — | <10 | 0.524 | 10 | 0.267 |
| Pneumonia immunization | 0.152 | 32 | — | <10 | — | <10 | 0.152 |
| Breast cancer screening | 0.348 | 70 | 0.296 | 36 | 0.061 | 31 | 0.235 |
| Diabetes care: blood sugar/HbA1c testing | 0.599 | 42 | 0.490 | 12 | 0.097 | 12 | 0.395 |
| Diabetes care: retinal eye exam | 0.101 | 42 | −0.189 | 13 | 0.729 | 12 | 0.213 |
| Diabetes care: LDL‐C screening | 0.425 | 42 | 0.325 | 12 | 0.001 | 12 | 0.251 |
| Diabetes care: kidney disease/nephropathy | 0.314 | 33 | — | <10 | — | <10 | 0.314 |
| Colorectal cancer screening | 0.378 | 38 | 0.270 | 23 | −0.431 | 20 | 0.072 |
| Monitoring patients on persistent medications (summary) | 0.220 | 148 | 0.274 | 98 | 0.219 | 94 | 0.237 |
| Overall | 0.283 | 0.244 | 0.171 | 0.237 | |||
Bold indicates p < .05.
Statistics for each row are for all non‐diagonal correlation coefficients from a 3 × 3 matrix of CAHPS or HEDIS within‐plan disparities across minority groups and within measure (i.e., maximum 3 correlation coefficients summarized per row).
Minimum of 10 contracts with 100 members for each pair of measures.
Correlation coefficients for customer service and getting prescription drug information could not be computed given there were no contracts with the required two sets of BLUPS.
Conclusions
The purpose of this research was to examine the extent to which racial/ethnic disparities in clinical performance and patient experiences within MA contracts are similar for different measures and different racial/ethnic groups. We find a common relationship in disparities across individual CAHPS/HEDIS measures. For all racial/ethnic groups, positive and significant correlations of disparities are observed for the access measures (getting needed care and prescription drug composites) and HEDIS diabetes care measures (LDL‐C and HbAlc). For example, contracts with low disparities for blacks (relative to whites) in LDL‐C testing have a tendency to have low black/white disparities for HbAlc testing among diabetics, and vice versa. Further research is needed to explore potential common drivers that may affect several measures simultaneously. Such drivers might include plan structural elements such as computerized reminders for preventive services, provider incentives, language services, or sensitivity to the needs and barriers of minorities.
To a lesser extent, this pattern also holds when comparing CAHPS disparities and HEDIS disparities for each racial/ethnic group. Thus, contracts have somewhat similar racial/ethnic disparities in patient experience (CAHPS) and clinical performance (HEDIS) for a given racial/ethnic group. The largest correlations between disparities in CAHPS and HEDIS measures are observed among API and Hispanics; contracts with low disparities for these groups in CAHPS also have low disparities in HEDIS. Further research is needed to examine the common drivers of disparities in CAHPS and HEDIS measures. Common drivers might include both patient‐level and plan‐level factors. For example, there may be unobserved patient socioeconomic differences that may account for the correlation in CAHPS and HEDIS disparities. On the other hand, plan‐level factors such as increased access to language services may reduce disparities in both CAHPS and HEDIS measures, especially among those API and Hispanic beneficiaries whose preferred language is not English (Morales et al. 2006; Karliner et al. 2007).
We also find consistent small positive correlations of disparities within individual CAHPS and HEDIS measures across racial/ethnic groups, although few were statistically significant. To a slight extent, contracts with low disparities for one minority group tend to have low disparities for other groups, especially for monitoring patients on persistent medications. Correlations in HEDIS cancer screenings and diabetes care disparities are observed between blacks and Hispanics. It might be the case that HEDIS disparities are driven more by socioeconomic factors (e.g., lack of transportation and cost barriers) or health literacy factors, rather than linguistic factors, given the lower mean income and socioeconomic status of black and Hispanic adults relative to white and Hispanic adults (America's Health Insurance Plans Centers for Policy and Research 2012). Further research is needed to examine how health plan efforts to reduce transportation and health literacy barriers may reduce disparities simultaneously across different racial/ethnic groups.
In general, our findings suggest that to some extent there are high‐disparity and low‐disparity plans. In low‐disparity plans, the experiences of racial/ethnic minorities tend to be more favorable than in high‐disparity plans, relative to the experiences of white beneficiaries in each plan. The consistency of disparities is greatest within a single CAHPS/HEDIS domain but generalizes to some extent across domains. However, data limitations preclude the identification of particular plan‐level mechanisms that may be driving the high and low disparities, such as provision of language services or computerized reminders for preventive services.
Further research is needed into potential interventions to improve care in high‐disparity plans. This may include case studies or mixed method (quantitative/qualitative) studies to examine the structural factors that may explain low‐versus high‐disparity plans. Cultural barriers, lack of trust, and perceived discrimination may affect the interaction of minorities with the health care system. Recent research has shown that perceived discrimination is associated with racial/ethnic differences in health plan CAHPS measures across racial/ethnic groups (Weech‐Maldonado et al. 2012). From a policy perspective, this may lend support to system‐wide interventions that target common drivers to improve scores on multiple measures at the same time across racial/ethnic groups. This may include plan‐level diversity/cultural competency initiatives that involve recruitment/retention of diverse staff/providers, cultural competency training, data collection on language preference, and strategic goals and quality improvement activities targeted at reducing racial/ethnic disparities in care (Weech‐Maldonado et al. 2011). Recent research suggests that patients receiving care in hospitals with higher cultural competency, as evidenced by higher adherence to the cultural and linguistic appropriate services standards, experience better overall patient experiences, and this particularly benefits minorities in their interactions with nurses and hospital staff (Weech‐Maldonado et al. 2012).
Reducing CAHPS and HEDIS disparities by improving the care for black, Hispanic, and API Medicare beneficiaries can also improve the financial position of MA plans, as the Patient Protection and Affordable Care Act of 2010 established bonus payments for Medicare managed care plans beginning in 2012 that include CAHPS and HEDIS measures.
Implications for Policy, Delivery, or Practice
Within both clinical quality and patient experience domains, results suggest that some common elements may influence disparities across measures and to a lesser extent across minority groups, permitting efficient and broadly effective interventions to reduce disparities. Future research should identify the key elements of low‐disparity plans' success. Newly mandated reporting of CAHPS and HEDIS measures by race/ethnicity may facilitate assessment of progress in meeting these goals (Martino et al. 2013).
Supporting information
Appendix SA1. Author Matrix.
Table S1. Detail on Seven CAHPS Measures.
Table S2. Detail on Seven HEDIS Measures.
Table S3. (a) Correlations of CAHPS Measure Disparities, Black Beneficiaries; (b) Correlations of CAHPS Measure Disparities, Hispanic Beneficiaries; (c) Correlations of CAHPS Measure Disparities, Asian/Pacific Islander Beneficiaries.
Table S4. (a) Correlations of HEDIS Measure Disparities, Black Beneficiaries; (b) Correlations of HEDIS Measure Disparities, Hispanic Beneficiaries; (c) Correlations of HEDIS Measure Disparities, Asian/Pacific Islander Beneficiaries.
Table S5. (a) Correlations of CAHPS and HEDIS Measures Disparities, Black Beneficiaries; (b) Correlations of CAHPS and HEDIS Measures Disparities, Hispanic Beneficiaries; (c) Correlations of CAHPS and HEDIS Measures Disparities, Asian/Pacific Islander Beneficiaries.
Table S6. CAHPS Disparity Correlations across Racial/Ethnic Groups.
Table S7. HEDIS Disparity Correlations across Racial/Ethnic Groups.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: This article was funded by the Centers for Medicare & Medicaid Services (CMS) under contract number HHSM‐500‐2005‐000281. No author has a conflict of interest relating to this manuscript. However, please note that one of the authors, Dr. Sarah Gaillot, is an employee of CMS, the Federal Agency that sponsors the collection of CAHPS and HEDIS data discussed within the manuscript. We would like to thank Fergal McCarthy, M.Phil., for his assistance with manuscript preparation.
Disclosures: None.
Disclaimers: None.
References
- America's Health Insurance Plans Centers for Policy and Research . 2012. “Low‐Income & Minority Beneficiaries in Medicare Advantage Plans, 2010” [accessed on February 16, 2015]. Available at http://www.ahip.org/MALowIncomeMinorityReport2012/
- Atherly, A. , and Thorpe K. E.. 2005. Value of Medicare Advantage to Low‐Income and Minority Medicare Beneficiaries. Atlanta, GA: Emory University. [Google Scholar]
- Binns, G. S. 1991. “The Relationship among Quality, Cost, and Market Share in Hospitals.” Topics in Health Care Financing 18 (2): 21–32. [PubMed] [Google Scholar]
- Cella, D. , Yount S., Rothrock N., Gershon R., Cook K., Reeve B., Ader D., Fries J. F., Bruce B., Rose M., and P. C. Group . 2007. “The Patient‐Reported Outcomes Measurement Information System (PROMIS): Progress of an NIH Roadmap Cooperative Group during Its First Two Years.” Medical Care 45 (5 Suppl 1): S3–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Medicare & Medicaid Services . 2014. “Medicare.gov Medicare Plan Finder” [accessed on October 2, 2014]. Available at https://www.medicare.gov/find-a-plan/questions/home.aspx
- Chou, A. F. , Brown A. F., Jensen R. E., Shih S., Pawlson G., and Scholle S. H.. 2007. “Gender and Racial Disparities in the Management of Diabetes Mellitus among Medicare Patients.” Womens Health Issues 17 (3): 150–61. [DOI] [PubMed] [Google Scholar]
- Deming, W. E. , and Stephan F. F.. 1940. “On a Least‐Squares Adjustment of a Sampled Frequency Table When the Expected Marginal Totals Are Known.” Annals of Mathematical Statistics 11 (4): 3–18. [Google Scholar]
- Donabedian, A. 1988. “The Quality of Care. How Can It Be Assessed?” Journal of the American Medical Association 260 (12): 1743–8. [DOI] [PubMed] [Google Scholar]
- Elliott, M. N. , Haviland A. M., Orr N., Hambarsoomian K., and Cleary P. D.. 2011. “How Do the Experiences of Medicare Beneficiary Subgroups Differ between Managed Care and Original Medicare?” Health Services Research 46 (4): 1039–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fongwa, M. N. , Cunningham W., Weech‐Maldonado R., Gutierrez P. R., and Hays R. D.. 2008. “Reports and Ratings of Care: Black and White Medicare Enrollees.” Journal of Health Care for the Poor and Underserved 19 (4): 1136–47. [DOI] [PubMed] [Google Scholar]
- Goldstein, E. , Elliott M. N., Lehrman W. G., Hambarsoomian K., and Giordano L. A.. 2010. “Racial/Ethnic Differences in Patients' Perceptions of Inpatient Care Using the HCAHPS Survey.” Medical Care Research and Review 67 (1): 74–92. [DOI] [PubMed] [Google Scholar]
- Griffith, D. M. , Childs E. L., Eng E., and Jeffries V.. 2007. “Racism in Organizations: The Case of a County Public Health Department.” Journal of Community Psychology 35 (3): 287–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustafson, D. H. , and Hundt A. S.. 1995. “Findings of Innovation Research Applied to Quality Management Principles for Health Care.” Health Care Management Review 20 (2): 16–33. [PubMed] [Google Scholar]
- Hargraves, J. L. , Hays R. D., and Cleary P. D.. 2003. “Psychometric Properties of the Consumer Assessment of Health Plans Study (CAHPS) 2.0 Adult Core Survey.” Health Services Research 38 (6 Pt 1): 1509–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haviland, A. M. , Elliott M. N., Weech‐Maldonado R., Hambarsoomian K., Orr N., and Hays R. D.. 2012. “Racial/Ethnic Disparities in Medicare Part D Experiences.” Medical Care 50 (Suppl): S40–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hays, R. D. 2009. “Patient Satisfaction” In Encyclopedia of Medical Decision Making, edited by Kattan M. W., pp. 867–9. Thousand Oaks, CA: Sage Publications. [Google Scholar]
- Hays, R. D. , Shaul J. A., Williams V. S., Lubalin J. S., Harris‐Kojetin L. D., Sweeny S. F., and Cleary P. D.. 1999. “Psychometric Properties of the CAHPS 1.0 Survey Measures. Consumer Assessment of Health Plans Study.” Medical Care 37 (3 Suppl): MS22–31. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine . 2003. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: Institute of Medicine. [Google Scholar]
- Karliner, L. S. , Jacobs E. A., Chen A. H., and Mutha S.. 2007. “Do Professional Interpreters Improve Clinical Care for Patients with Limited English Proficiency? A Systematic Review of the Literature.” Health Services Research 42 (2): 727–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, X.‐Q. , Rong J.‐Y., and Liu X.‐Y.. 2008. “Best Linear Unbiased Prediction for Linear Combinations in General Mixed Linear Models.” Journal of Multivariate Analysis 99 (8): 1503–17. [Google Scholar]
- Longest, B. B. , Rakich S. J., and Darr K.. 2000. Managing Health Services Organizations and Systems. Baltimore, MD: Health Professions Press. [Google Scholar]
- Lurie, N. , Zhan C., Sangl J., Bierman A. S., and Sekscenski E. S.. 2003. “Variation in Racial and Ethnic Differences in Consumer Assessments of Health Care.” American Journal of Managed Care 9 (7): 502–9. [PubMed] [Google Scholar]
- Lyratzopoulos, G. , Elliott M., Barbiere J. M., Henderson A., Staetsky L., Paddison C., Campbell J., and Roland M.. 2012. “Understanding Ethnic and Other Socio‐Demographic Differences in Patient Experience of Primary Care: Evidence from the English General Practice Patient Survey.” BMJ Quality & Safety 21 (1): 21–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martino, S. C. , Elliott M. N., Cleary P. D., Kanouse D. E., Brown J. A., Spritzer K. L., Heller A., and Hays R. D.. 2009. “Psychometric Properties of an Instrument to Assess Medicare Beneficiaries' Prescription Drug Plan Experiences.” Health Care Financing Review 30 (3): 41–53. [PMC free article] [PubMed] [Google Scholar]
- Martino, S. C. , Weinick R. M., Kanouse D. E., Brown J. A., Haviland A. M., Goldstein E., Adams J. L., Hambarsoomian K., Klein D. J., and Elliott M. N.. 2013. “Reporting CAHPS and HEDIS Data by Race/Ethnicity for Medicare Beneficiaries.” Health Services Research 48 (2 Pt 1): 417–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCaffrey, D. F. , and Elliott M. N.. 2008. “Power of Tests for a Dichotomous Independent Variable Measured with Error.” Health Services Research 43 (3): 1085–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morales, L. S. , Elliott M., Weech‐Maldonado R., and Hays R. D.. 2006. “The Impact of Interpreters on Parents' Experiences with Ambulatory Care for Their Children.” Medical Care Research and Review 63 (1): 110–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Committee for Quality Assurance . 2011. “What Is HEDIS?” [accessed on April 23, 2011]. Available at http://www.ncqa.org/HEDISQualityMeasurement/WhatisHEDIS.aspx
- O'Malley, A. J. , Zaslavsky A. M., Elliott M. N., Zaborski L., and Cleary P. D.. 2005. “Case‐Mix Adjustment of the CAHPS Hospital Survey.” Health Services Research 40 (6 Pt 2): 2162–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Purcell, N. J. , and Kish L.. 1980. “Postcensal Estimates for Local Areas (or Domains).” International Statistical Review 48 (1): 3–18. [Google Scholar]
- Raudenbush, S. W. , and Bryk A. S.. 2002. Hierarchical Linear Models: Applications and Data Analysis Methods, 2d Edition Newbury Park, CA: Sage. [Google Scholar]
- Schneider, E. C. , Zaslavsky A. M., and Epstein A. M.. 2002. “Racial Disparities in the Quality of Care for Enrollees in Medicare Managed Care.” Journal of the American Medical Association 287 (10): 1288–94. [DOI] [PubMed] [Google Scholar]
- Spearman, C. 1910. “Correlation Calculated from Faulty Data.” British Journal of Psychology 3 (3): 271–95. [Google Scholar]
- Trivedi, A. N. , Zaslavsky A. M., Schneider E. C., and Ayanian J. Z.. 2005. “Trends in the Quality of Care and Racial Disparities in Medicare Managed Care.” New England Journal of Medicine 353 (7): 692–700. [DOI] [PubMed] [Google Scholar]
- Trivedi, A. N. , Zaslavsky A. M., Schneider E. C., and Ayanian J. Z.. 2006. “Relationship between Quality of Care and Racial Disparities in Medicare Health Plans.” Journal of the American Medical Association 296 (16): 1998–2004. [DOI] [PubMed] [Google Scholar]
- Unruh, L. , and Wan T. T.. 2004. “A Systems Framework for Evaluating Nursing Care Quality in Nursing Homes.” Journal of Medical Systems 28 (2): 197–214. [DOI] [PubMed] [Google Scholar]
- Weech‐Maldonado, R. , Elliott M. N., Morales L. S., Spritzer K., Marshall G. N., and Hays R. D.. 2004. “Health Plan Effects on Patient Assessments of Medicaid Managed Care among Racial/Ethnic Minorities.” Journal of General Internal Medicine 19 (2): 136–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weech‐Maldonado, R. , Fongwa M. N., Gutierrez P., and Hays R. D.. 2008. “Language and Regional Differences in Evaluations of Medicare Managed Care by Hispanics.” Health Services Research 43 (2): 552–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weech‐Maldonado, R. , Al‐Amin M., Nishimi R. Y., and Salam F.. 2011. “Enhancing the Cultural Competency of Health‐Care Organizations.” Advanced Healthcare Management 10: 43–67. [DOI] [PubMed] [Google Scholar]
- Weech‐Maldonado, R. , Elliott M., Pradhan R., Schiller C., Hall A., and Hays R. D.. 2012. “Can Hospital Cultural Competency Reduce Disparities in Patient Experiences with Care?” Medical Care 50 (Suppl): S48–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaslavsky, A. M. , Zaborski L. B., Ding L., Shaul J. A., Cioffi M. J., and Cleary P. D.. 2001. “Adjusting Performance Measures to Ensure Equitable Plan Comparisons.” Health Care Financing Review 22 (3): 109. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1. Author Matrix.
Table S1. Detail on Seven CAHPS Measures.
Table S2. Detail on Seven HEDIS Measures.
Table S3. (a) Correlations of CAHPS Measure Disparities, Black Beneficiaries; (b) Correlations of CAHPS Measure Disparities, Hispanic Beneficiaries; (c) Correlations of CAHPS Measure Disparities, Asian/Pacific Islander Beneficiaries.
Table S4. (a) Correlations of HEDIS Measure Disparities, Black Beneficiaries; (b) Correlations of HEDIS Measure Disparities, Hispanic Beneficiaries; (c) Correlations of HEDIS Measure Disparities, Asian/Pacific Islander Beneficiaries.
Table S5. (a) Correlations of CAHPS and HEDIS Measures Disparities, Black Beneficiaries; (b) Correlations of CAHPS and HEDIS Measures Disparities, Hispanic Beneficiaries; (c) Correlations of CAHPS and HEDIS Measures Disparities, Asian/Pacific Islander Beneficiaries.
Table S6. CAHPS Disparity Correlations across Racial/Ethnic Groups.
Table S7. HEDIS Disparity Correlations across Racial/Ethnic Groups.


