Abstract
Objective
To examine nurse practitioner (NP) and physician assistant (PA) practice in nursing homes (NHs) during 2000–2010.
Data Sources
Data were derived from the Online Survey Certification and Reporting system and Medicare Part B claims (20 percent sample).
Methods
NP/PA state average employment, visit per bed year (VPBY), and providers per NH were examined. State fixed‐effect models examined the association between state regulations and NP/PA use.
Principal Findings
NHs using any NPs/PAs increased from 20.4 to 35.0 percent during 2000–2010. Average NP/PA VPBY increased from 1.0/0.3 to 3.0/0.6 during 2000–2010. Average number of NPs/PAs per NH increased from 0.2/0.09 to 0.5/0.14 during 2000–2010. The impact of state scope‐of‐practice regulations was mixed.
Conclusions
NP and PA scope‐of‐practice regulations impact their practice in NHs, not always as intended.
Keywords: Medicare claims, Online Survey Certification and Reporting (OSCAR) system, scope‐of‐practice, physician visits in nursing homes, organization of medical staff
Nearly 1.4 million Americans live in nursing homes (NHs) (Kaiser Family Foundation 2014b), which serve postacute and rehabilitative patients and cognitively and physically impaired long‐stay residents suffering from one or more chronic medical conditions (Katz and Karuza 2006). Although there has been a decline in the number of NH residents due to increasing availability of residential care options, residents' complexity and care needs have risen with a growing focus on postacute care and rehabilitation in NHs (Decker 2005; American Health Care Association 2011). Physicians (MDs) are largely unwilling to practice in NHs, likely due to a lack of professional training, low reputation, financial disincentives, and apprehension regarding malpractice lawsuits (Kapp 2009). Moreover, the number of physicians practicing in NHs has declined over time (Bakerjian and Harrington 2012), raising questions about the ability of the nation's physician workforce to meet the complex care needs of the population served (Cooper et al. 2002). Nurse practitioners (NPs), who are registered nurses with graduate degrees and advanced clinical training, and physician assistants (PAs), who are bachelor's‐ or master's‐level members of a physician‐led team, have been shown to provide quality care to NH residents (Intrator, Zinn, and Mor 2004; Intrator et al. 2005). Thus, NPs/PAs may help to reduce the shortage in medical care available in NHs (Mezey et al. 2005; Bakerjian and Harrington 2012).
Among practitioners who provide NH care, NPs and PAs provide more care, on average, than physicians (33 visits annually vs. 21) (Bakerjian and Harrington 2012). Additionally, patients who are seen by both NPs/PAs and physicians receive almost twice as many visits than those who see physicians only, suggesting that NPs and PAs supplement or complement the care that physicians provide (Bakerjian and Harrington 2012). Greater presence of NPs and PAs is also associated with equal or better quality of NH care (Intrator, Zinn, and Mor 2004; Xing, Mukamel, and Temkin‐Greener 2013). Physicians, residents, and their families are highly satisfied with the care that nonphysician practitioners provide (Rosenfeld et al. 2007).
The American Association of Nurse Practitioners (AANP) reports that there were 192,000 NPs in the United States in 2013 (AANP 2014). Although 15.2 percent had long‐term care privileges, only 3 percent described their practice as geriatric. While there were 83,000 PAs (Kaiser Family Foundation 2014a), less than 1 percent reported working in NHs (American Academy of Physician Assistants 2011). Although just 10 percent of NHs used NPs/PAs in 1990, by 2000, the number had increased to 20 percent (Intrator et al. 2005). This low penetration may be due to states' limitation in practice authorization of NP/PAs. It may also be due to comparatively low barriers to entering practice, which inhibit administrator confidence in NPs/PAs ability to practice without supervision.
Changes in states' NP and PA scope‐of‐practice regulations may facilitate greater use of NPs/PAs in NHs, while, at the same time, contributing to substantial variation, both across states and across provider types (i.e., NPs over PAs). Examination of NP and PA regulations demonstrates that greater authority has been granted to NPs and PAs from 2000 to 2010 (Gadbois et al. 2015). This increase in authority is reflected in a variety of dimensions, including reducing the level of physician involvement required for practice, and the ability to prescribe medications independently and at increasingly higher schedules. States have also increased barriers to entering practice; for example, requiring a master's degree in nursing in order for NPs to practice, or a bachelor's or master's degree for PAs to practice (Gadbois et al. 2015). More stringent entry‐to‐practice provisions may facilitate NP/PA employment in NHs by reassuring administration about their ability to practice independently.
This study documents trends in NH use of NPs and PAs between 2000 and 2010. The primary objective is to address the prevailing gap in knowledge about NH use of NPs/PAs nationally since 2000 (Intrator et al. 2005; Katz and Karuza 2006) and to describe variation in NPs/PAs use across states during this time period (Bakerjian and Harrington 2012). We also conduct preliminary analyses exploring the relationship between state scope‐of‐practice regulations and NP/PA use in NHs during this time period.
Methods
Data Sources
Information on MD, NP, and PA visits with NH residents was obtained using Medicare Part B billing data available from the Centers for Medicare and Medicaid Services' (CMS) Medicare Carrier File. The annual Carrier File contains claims for provider services and includes Medicare beneficiary identifiers, provider identifiers, dates of service, procedure codes, provider specialty codes, diagnoses, and charges and reimbursement. Part B data have been used previously in other research studies (e.g., Bakerjian and Harrington 2012).
Part B claims do not provide information on the identity of the NH in which services were provided. To obtain information on the number of different NHs that employed NPs or PAs, we used data from the CMS Online Survey Certification and Reporting (OSCAR) system deriving from the CMS certification process, which is conducted on all Medicare/Medicaid certified NHs every 9–15 months. OSCAR data have been widely used in research studies (e.g., Intrator et al. 2005; Temkin‐Greener et al. 2010).
Measurement
All evaluation and management claims from Medicare Part B with place of service code in a NH (31) or skilled nursing facility (32) were used. We used the cross walk between Medicare provider/supplier specialty code and health care provider taxonomy to identify NPs (codes 50), PAs (97), physicians who were likely primary care providers (01: General Practice, 08: Family Medicine; 11: Internal Medicine; 38: Geriatrics), and other physicians (specialty codes 02‐07, 08‐10, 12‐14, 16‐18, 20‐30, 33‐34, 36‐40, 44, 46, 66, 72, 76‐79, 81‐84, 86. 90‐94, 98, 99, C0, C3). We excluded providers who were not physicians (e.g., chiropractors, podiatrists).
Number of claims made by NPs, PAs, primary care MDs (PC‐MDs), or other physicians (O‐MDs) were aggregated per state year as were number of providers (identified by their Unique Provider Identification Number through 2006 and by their National Provider Identifier from 2007 and later). States were identified as the provider state in the Carrier File.
The CMS claim files used for this study represent 20 percent of the NH population from 2000 to 2007 and 20 percent of the U.S. population from 2007 to 2010. Comparison of the numbers in the common year, 2007, identified that the files for 2000–2007 consistently underestimated the number of NP PA, and MD visits in 2007 by a factor of 0.83. Consequently, in our study, we adjusted the number of observed NP, PA, and MD visits in 2000 to 2006 by this factor to ensure comparability across time.
The total number of MD, NP, and separately PA visits in NHs per year in each state was weighted by the 20 percent sample (i.e., multiplied by 5). Because the number of visits depends, in part, on the number of beds available and because the number of beds varies considerably across states, we standardized the number of MD, NP, and PA visits to total number of NH beds in a state yielding the outcome measure, average number of visits per bed year (VPBY). We note that the number of medical staff may not be complete as it is based on those who provided care to the random 20 percent sample of residents. Data constraints precluded observation of Alaska, the District of Columbia, Hawaii, and Virginia.
As part of the annual survey of certification of NHs, nursing homes are required to report the total number of hours in which they employed each staff type: MD and NP/PA (without differentiation), in the 2‐week period leading up to the OSCAR survey (full‐time, part‐time, or on contract). The proportion of NHs employing any NPs/PAs across all 50 states and the District of Columbia was recorded.
Additional information obtained from the OSCAR data included the total number of NH beds annually per state. Finally, data from www.LTCfocUS.org were used to retrieve the average case mix index based on the ratio of the average direct‐care minutes per each Resource Utilization Group to the overall average number of minutes.
State regulations during 2001–2009 were obtained from state websites and compendiums (Gadbois et al. 2015). Separate regulations for NP and PA measures included indicators for the degree of physician involvement, whether prescription of controlled substances was allowed, whether NPs had prescriptive authority separate from MDs, and the educational qualifications required for PAs, a bachelor's or master's degree, and for NPs, a master's degree in nursing or other graduate degree.
Analysis
We use box and whisker plots to describe the distribution of the proportion of NHs using NPs or PAs in each state annually. Similarly, box and whisker plots were used to report the number of NP, PA, PC‐MD, and O‐MD VPBY and the average number of unique NPs, PAs, PC‐MDs, and O‐MDs per bed year in NHs during each study year. The box reports the median on the middle horizontal line; the 25th and 75th percentiles on the lower and upper vertical lines. Outliers are represented by dots.
We used state fixed‐effect models to explore the relationship between state regulations and NP and PA VPBY in NHs, and average number of NP and PA providers per facility, between 2001 and 2009, controlling for the average number of PC‐MDs/O‐MDs VPBY, average number of PC‐MDs/O‐MDs per NH, total beds (in 1,000s), and average case mix index.
Results
Proportion of Nursing Homes Using NPs or PAs
Nationally, the proportion of NHs employing NPs or PAs increased steadily from 20.4 percent in 2000 to 28.6 percent in 2005 and 35.0 percent in 2010 (Figure 1). There was, however, considerable variability across states. In 2010, for example, between 11.5% (West Virginia) and 62.1% (Massachusetts) of NHs per state had NPs/PAs. Most states experienced substantial increases in use of NPs and PAs over the 10 years examined, including 6 with increases greater than 25.0 percent (Connecticut, Kentucky, Massachusetts, Maine, Ohio, Tennessee). A handful of states experienced a decline in NP/PA use (Hawaii, Montana, Wyoming).
Figure 1.
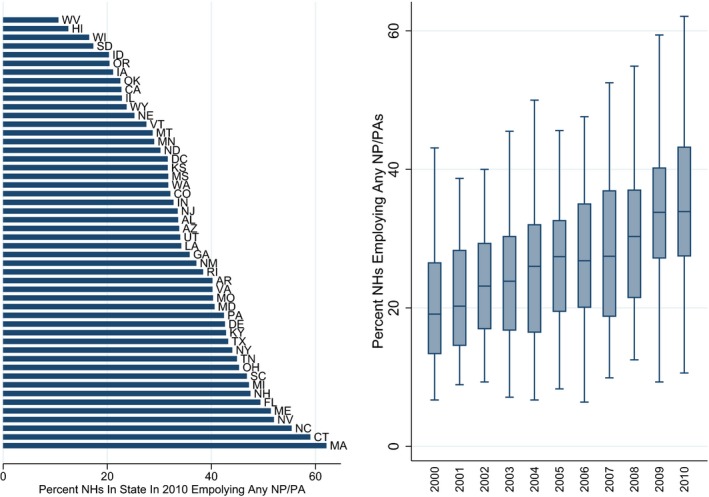
Average Proportion of Nursing Homes (NHs) in States That Employed Any Nurse Practitioners (NPs) or Physician Assistants (PAs) in 2010 Sorted from Least Prevalent to Most Prevalent among NHs in State. Box‐Whisker Plots of Distribution of the Percent of NHs Per Year That Employed Any NP or PA by Year from 2000 to 2010
Average Number of Unique MDs, NPs, and PAs
The average number of unique NPs and PAs providing care in NHs continuously increased over the decade, but the average number of PC‐MDs and O‐MDs decreased (Figure 2a). The number of NPs per NH increased from about 0.2 in 2000 to 0.36 in 2005 and to 0.49 in 2010. The number of PAs increased from 0.1 in 2000 to 0.14 in both 2005 and 2010. The average number of PC‐MDs/O‐MDs providing care in NHs decreased from about 3.5/1.4 per NH in 2000 and 2005 to 2.9/.08 in 2010.
Figure 2.
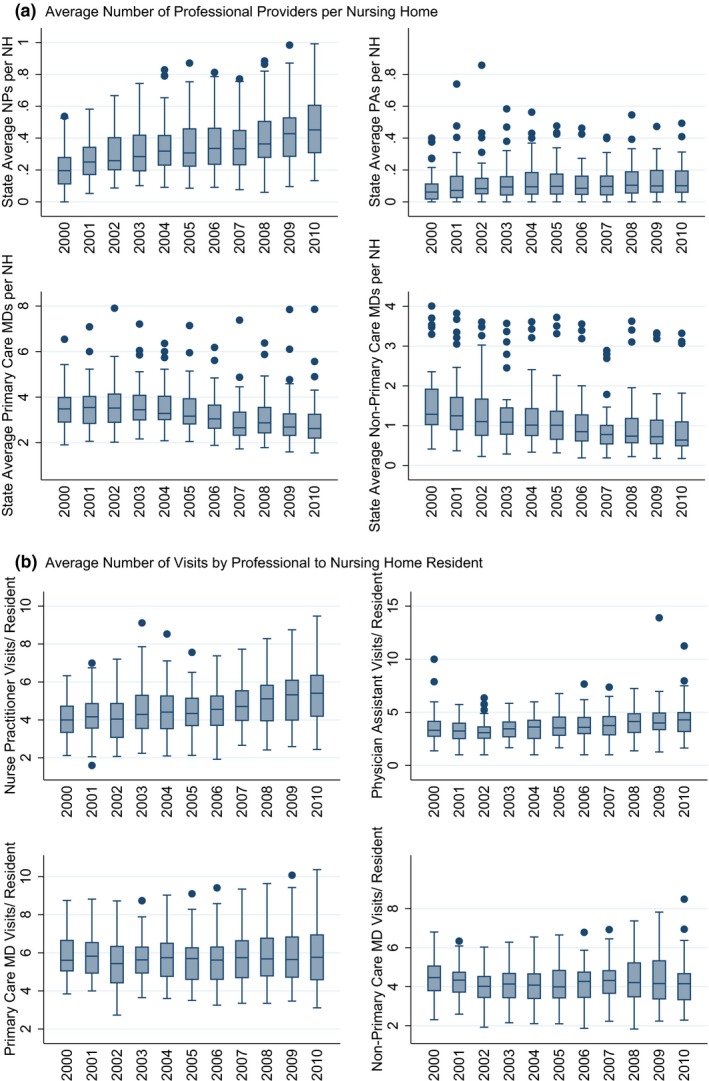
(a) Total Number of Unique NPs, PAs, Primary Care MDs, and Nonprimary Care MDs Who Submitted Evaluation and Management Claims in Nursing Homes (NHs) in a State to the Total Number of NHs in the State. Box‐Whisker Plots Display of Distribution over All States Per Provider Type over the Decade, 2000 to 2010. (b) Average Number of Evaluation and Management Visits in Nursing Homes (NHs) Per Year Per NH Bed in a State Provided by Nurse Practitioners (NPs), Physician Assistants (PAs), Primary Care Physicians (MDs), and Other MDs. Box‐Whisker Plots of Annual Distribution over All 50 US States Annually, from 2000 through 2010
Average Number of MD, NP, and PA Visits
The average number of visits by PC‐MDs remained fairly constant at about 9 VPBY annually; so too the number of O‐MD VPBY at 2.2 (Figure 2b). The average number of NP VPBY tripled from 1 to 2 to 3 in 2000, 2005, and 2010, respectively. The average number of PA VPBY increased more moderately, from 0.3 to 0.4 to 0.6 in 2000, 2005, and 2010, respectively.
There was great cross‐state variability in NP and PA VPBY. In 2000, for example, the number of NP VPBY ranged from 0 (Maine, Vermont) to 3.21 (Nevada); by, 2010, NP VPBY ranged from 0.36 (South Dakota) to 8.95 (Connecticut). All states but New Mexico and Nevada experienced increases in the number of NP VPBY during the time period studied. In 2000, the number of PA VPBY ranged from 0 (Arkansas, California, Louisiana, Massachusetts, Maine, Oregon, Nevada, Utah) to 1.24 (Michigan). By 2010, PA VPBY ranged from 0 (Arizona, Indiana, Oregon, Utah) to 2.59 (Michigan). All states but Wyoming experienced an increase in PA visits from 2000 to 2010. In 2000, the total number of MD visits (PC‐MD and O‐MD) per bed year ranged from 4.22 (Oregon) to 27.95 (Michigan). In 2010, it ranged from 2.46 (Oregon) to 35.18 (New Jersey) VPBY. Most states experienced moderate numbers of MD visits throughout (e.g., California, Colorado, Georgia, Indiana, Kentucky, Missouri, Ohio, Vermont, Wyoming).
NP/PA Regulation and Visits Per Bed Year
Fixed‐effect regression results (Table 1) indicate that higher NP VPBY were observed in states that required physician involvement in NP practice (b = .64, p < .001) and in states that allowed NPs to prescribe medications separately from physicians (b = .34, p = .01) (Model 1). NP VPBY were also higher when there were more visits by PC‐MDs (b = .26, p < .001) and more PC‐MDs practicing per NH (b = .27, p = .03) but were lower when there were more visits by O‐MDs (b = −0.44, p < .001).
Table 1.
Results of State Fixed Effects Regression on Average Number of Nurse Practitioner (NP) and Physician Assistant (PA) Visits per Nursing Home Bed Year in Each State and Average Number of Unique NP and PA Providers Per Facility in Each State Per Year. The Relationship of States' Scope of Practice Regulations for NPs and PAs and Volume of Visits and Providers Is Tested
| Coefficient | Standard Error | p‐value | Coefficient | Standard Error | p‐value | ||
|---|---|---|---|---|---|---|---|
| Nurse practitioner visits per bed year (Model 1) | Physician assistant visits per bed year (Model 2) | ||||||
| Physician (MD) required involvement in NP's practice | 0.64 | 0.20 | .00 | ||||
| NPs allowed to prescribe some controlled substances | −0.14 | 0.23 | .55 | PAs allowed to prescribe some controlled substances | −0.13 | 0.05 | .01 |
| NPs allowed to prescribe medications | 0.34 | 0.12 | .01 | ||||
| NP requires master's degree in nursing | −0.12 | 0.13 | .35 | PA requires bachelor's/master's degree | −0.11 | 0.06 | .07 |
| No. of primary care MD visits per bed | 0.26 | 0.04 | .00 | No. of primary care MD visits per bed | 0.02 | 0.01 | .09 |
| No. of other MD visits per bed | −0.44 | 0.09 | .00 | No. of other MD visits per bed | 0.05 | 0.02 | .04 |
| No. of unique primary care MDs/facility | 0.27 | 0.12 | .03 | No. of unique primary care MDs/facility | 0.08 | 0.03 | .03 |
| No. of unique other MDs/facility | −0.18 | 0.21 | .39 | No. of unique other MDs/facility | −0.10 | 0.06 | .11 |
| Year | 0.36 | 0.03 | .00 | Year | 0.04 | 0.01 | .00 |
| Average RUG case mix index | −14.91 | 2.89 | .00 | Average RUG case mix index | 0.43 | 0.51 | .40 |
| Total NH beds | 0.00 | 0.00 | .42 | Total NH beds | 0.00 | 0.00 | .00 |
| Average no. of nurse practitioners per NH (Model 3) | Average no. of physician assistants per NH (Model 4) | ||||||
| MD required involvement in NP's practice | 0.02 | 0.02 | .19 | ||||
| NPs allowed to prescribe some controlled substances | −0.02 | 0.03 | .46 | PAs allowed to prescribe some controlled substances | −0.01 | 0.01 | .29 |
| NPs allowed to prescribe medications | 0.00 | 0.01 | .95 | ||||
| NP requires master's degree in nursing | −0.03 | 0.01 | .02 | PA requires bachelor's/master's degree | 0.00 | 0.02 | .97 |
| No. of primary care MD visits per bed | 0.02 | 0.01 | .03 | No. of primary care MD visits per bed | 0.00 | 0.00 | .24 |
| No. of other MD visits per bed | −0.04 | 0.01 | .00 | No. of other MD visits per bed | 0.01 | 0.01 | .02 |
| No. of unique primary care MDs/facility | 0.10 | 0.01 | .00 | No. of unique primary careMDs/facility | 0.04 | 0.01 | .00 |
| No. of unique nonprimary care MDs/facility | 0.00 | 0.02 | .83 | No. of unique nonprimary care MDs/facility | −0.01 | 0.02 | .53 |
| Year | 0.04 | 0.00 | .00 | Year | 0.00 | 0.00 | .19 |
| Average RUG case mix index | −0.90 | 0.30 | .00 | Average RUG case mix index | 0.33 | 0.13 | .01 |
| Total NH beds | 0.00 | 0.00 | .35 | Total NH beds | 0.00 | 0.00 | .61 |
Lower PA VPBY were observed in states where PAs were allowed to prescribe controlled substances (b = −.13, p = .01) and where they were required to have a college degree or higher (b = −.11, p = .07) (Model 2). PAs had higher volume of visits in states with higher volume of PC‐MD VPBY (b = .02, p = .09) and O‐MD VPBY (b = .05, p = .04), as well as in states where more PC‐MDs practiced in NHs (b = .08, p = .03).
The average number of unique NPs practicing in NHs per NH bed was lower in states that required NPs to have a master's degree in nursing or higher (b = −.03, p = .02) and was higher in states in which there were more visits by PC‐MDs (b = .02, p = .03) and where more PC‐MDs practiced in NHs (b = 10, p < .001), but there were fewer visits by NPs if there were more O‐MDs practicing in NHs (b = −.04, p < .001) (Model 3). On the other hand, there were more unique PAs practicing in NHs in states in which there were more O‐MD VPBY (b = .01, p = .02), and more unique O‐MDs practicing per NH bed (b = .04, p < .001) (Model 4).
Discussion
Data deriving from both OSCAR and Medicare Part B demonstrated substantial growth in NP and PA use in NHs from 2000 to 2010. This is reflected in the proportion of NHs using any NPs or PAs increasing from 20.4 to 35.0 percent during the time period studied. Greater use of NPs and PAs in NHs during the first decade of the 21st century demonstrates continuation of trends identified by Intrator et al. (2005), which found the proportion of NPs and PAs in NHs rising from 10 to 20 percent during the 1990s.
There are several factors that may have contributed to the greater use of NPs and PAs in NHs over the decade examined. Research has found that physicians prefer not to practice in NHs (Adams et al. 2002; Cooper et al. 2002; Kapp 2009). Impediments posed by physician preferences combined with the shortage of physicians entering primary care (Cassidy 2013) mean that there are not enough physicians available to care for NH residents (Mezey et al. 2005; Bakerjian and Harrington 2012). Increasing use of NPs and PAs in NHs may reflect the growing practice of supplementing the NH physician workforce with nonphysician practitioners in light of continued physician disengagement from this setting of care. However, we observed that the correlation between the number of primary care physician visits and the number of NP/PA VPBY increased over this time from 0.34/0.06 in 2000 to around 0.46/0.29 from 2000 through 2010, respectively, suggesting that there may be a growing trend of collaborative work among physicians and NPs/PAs in NHs.
Despite considerable growth since 2000, great variability in NP and PA use was evident across states throughout the study period. Both state regulations of PA practices examined‐being allowed to prescribed controlled substances and requiring a bachelor's or higher academic degree to practice‐were related to fewer PA visit volumes. Regression results also indicate higher NP visit volumes in states that allowed NPs to prescribe medications. On the other hand, higher educational requirements of NPs and the ability to prescribe controlled substances were unrelated to differences in visit volume in NHs.
Interestingly, states that required MDs involvement in NP practice saw higher NP visit volumes. This result should be examined in the context of the full medical practice in NHs. In particular, NP visit volume in NHs was higher in states with greater MD visit volume and fewer MDs involved in NH care. Likewise, PAs appeared to provide a greater volume of visits when there were more MDs involved in care, but this was unrelated to the number of MDs practicing in NHs. It is possible that care is more likely to be organized collaboratively in those states with higher MD involvement in NH care. Collaborative medical staff practice in NHs has long been advocated for in the literature (Philpot, Tolson, and Morely 2011).
Limitations
This study is the first to examine trends in NP/PA use in NHs since 2000 and their relationship with state regulations. We do acknowledge several limitations. Although studies have criticized the accuracy of the OSCAR data's information on staffing (Feng et al. 2005), at present this is the most widely used resource for such information. We also note the existence of an additional service code in the Part B claims data for certified nurse specialists and PAs (89), which were excluded in our analyses because it was rarely used and did not distinguish advanced practice nurses from PAs. Furthermore, we only had one common year, 2007, with which to compare Part B data deriving from the NH sample (2000–2007) and national sample (2007–2010). Unfortunately, there are no other sources of data to support the ratio used. Lastly, Part B claims may not be a complete portrayal of all medical staff visits in NHs, in particular, in nursing homes where the MDs/NPs/PAs are employed on‐staff and where a large proportion of the residents are enrolled in Medicare Managed Care. Despite these caveats, the use of both OSCAR reports and Part B data produced findings that are in agreement. We recognize that the impact of many other controls should be evaluated, but we decided to limit the list of potential control variables as a more careful analysis should be conducted at the facility rather than state level. In this analysis, we did not ascertain the particular practice location, so it was not possible to contextualize the observed practice patterns. Future studies should attempt to provide this contextualization. Moreover, specific details about each NH have been shown repeatedly to make a difference in both care practices and quality of care in NHs, and these could not be included due to the state‐level focus of the analyses.
Conclusion
The current data demonstrate the increased use of NPs and PAs in NHs over the first decade of the 21st century, indicating that NPs and PAs may increasingly be used to alleviate the shortage of physicians practicing in NHs. Changes in NH staff organization may underlie these trends; so too might changes in scope‐of‐practice regulation. Findings also suggest the importance of accounting for the broader medical care labor context when conducting evaluations of the impact of regulations on the labor force providing care in the particular setting studied. Future research should examine additional state, facility, and market factors to elucidate the remaining wide variability in NP/PA use across states. With the increasing use of NPs and PAs in NHs, a careful scrutiny of its impact on resident care and outcomes is sorely needed no matter the reason why this trend has taken place.
Supporting information
Appendix SA1: Author Matrix.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: We wish to thank several individuals from the University of Rochester: Shubing Cai, PhD, and Wei Song, MSc, PhD student, for a careful read and helpful comments and Jiejin Li, MS, for her expert preparation of figures. This study was supported by an NIH Program Project entitled “Shaping Long Term Care in America” (NIA 1P01 AG027296, Vince Mor: PI). The research protocol was approved by the Brown University IRB and the University of Rochester RSRB, and the use of CMS data was approved under Data Use Agreements #18900.
Disclosures: None.
Disclaimers: None.
References
- Adams, W. L. , McIlvain H. E., Lacy N. L., Magsi H., Crabtree B. F., Yenny S. K., and Sitorius M. A.. 2002. “Primary Care for Elderly People: Why Do Doctors Find It So Hard?” The Gerontologist 42: 835–842. [DOI] [PubMed] [Google Scholar]
- American Academy of Physician Assistants . 2011. 2010 AAPA Physician Assistant Census. Alexandria, VA: American Academy of Physician Assistants. [Google Scholar]
- American Association of Nurse Practitioners . 2014. “NP Fact Sheet” [accessed on April 23, 2015]. Available at http://www.aanp.org/all-about-nps/np-fact-sheet
- American Health Care Association . 2011. 2011 Annual Quality Report: A Comprehensive Report on the Quality of Care in America's Nursing Homes. Washington, DC: Author; [accessed August 9, 2015]. Available at http://www.ahcancal.org/quality_improvement/Documents/2011QualityReport.pdf [Google Scholar]
- Bakerjian, D. , and Harrington C.. 2012. “Factors Associated with the Use of Advanced Practice Nurses/Physician Assistants in a Fee‐for‐Service Nursing Home Practice: A Comparison with Primary Care Physicians.” Research in Gerontological Nursing 5 (3): 163–173. doi:10.3928/19404921‐20120605‐01. [DOI] [PubMed] [Google Scholar]
- Cassidy, A. 2013. “Health Policy Brief: Nurse Practitioners and Primary Care (Updated).” Health Affairs, May 15, 2013. [Google Scholar]
- Cooper, R. A. , Getzen T. E., McKee H. J., and Laud P.. 2002. “Economic and Demographic Trends Signal an Impending Physician Shortage.” Health Affairs 21: 140–154. [DOI] [PubMed] [Google Scholar]
- Decker, F. H. 2005. Nursing Homes, 1977–99: What Has Changed, What Has Not?. Hyattsville, MD: National Center for Health Statistics; [accessed August 10, 2015]. Available at http://www.cdc.gov/nchs/data/nnhsd/nursinghomes1977_99.Pdf [Google Scholar]
- Feng, Z. , Katz P. R., Intrator O., Karuza J., and Mor V.. 2005. “Physician and Nurse Staffing in Nursing Homes: The Role and Limitations of the Online Survey Certification and Reporting (OSCAR) System.” Journal of the American Medical Directors Association 6 (1): 27–33. [DOI] [PubMed] [Google Scholar]
- Gadbois, E. A. , Miller E. A., Tyler D., and Intrator O.. 2015. “Trends in State Regulation of Nurse Practitioners and Physician Assistants, 2001‐2010.” Medical Care Research and Review 72 (2): 200–219. doi:10.1177/1077558714563763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Intrator, O. , Zinn J., and Mor V.. 2004. “Nursing Home Characteristics and Potentially Preventable Hospitalizations of Long‐Stay Residents.” Journal of the American Geriatrics Society 52 (10): 1730–1736. [DOI] [PubMed] [Google Scholar]
- Intrator, O. , Feng Z., Mor V., Gifford D., Bourbonniere M., and Zinn J.. 2005. “The Employment of Nurse Practitioners and Physician Assistants in U.S. Nursing Homes.” The Gerontologist 45 (4): 486–495. [DOI] [PubMed] [Google Scholar]
- Kaiser Family Foundation . 2014a. “Physician Assistants by Primary State of Employment” [accessed on April 23, 2015]. Available at http://kff.org/other/state-indicator/total-physician-assistants/
- Kaiser Family Foundation . 2014b. “State Health Facts. Total Number of Residents in Certified Nursing Facilities” [accessed on April 23, 2015]. Available at http://kff.org/other/state-indicator/number-of-nursing-facility-residents/
- Kapp, M. B. 2009. “The Liability Environment for Physicians Providing Nursing Home Care: Does It Make a Difference for Residents?” Elder Law Journal 16 (2): 249–293. [Google Scholar]
- Katz, P. R. , and Karuza J.. 2006. “The Nursing Home Physician Workforce.” Journal of the American Medical Directors Association 5 (3): 394–398. [DOI] [PubMed] [Google Scholar]
- Mezey, M. , Burger S. G., Bloom H. G., Bonner A., Bourbonniere M., Bowers B., and Ter Maat M.. 2005. “Experts Recommend Strategies for Strengthening the Use of Advanced Practice Nurses in Nursing Homes.” Journal of the American Geriatrics Society 53: 1790–1797. [DOI] [PubMed] [Google Scholar]
- Philpot, C. , Tolson D., and Morely J. E.. 2011. “Advanced Practice Nurses and Attending Physicians: A Collaboration to Improve Quality of Care in the Nursing Home.” Journal of the American Medical Directors Association 12 (3): 161–165. [DOI] [PubMed] [Google Scholar]
- Rosenfeld, P. , Kobayashi M., Barber P., and Mezey M.. 2007. “Utilization of Nurse Practitioners in Long‐Term Care: Findings and Implications of a National Survey.” Journal of the American Medical Directors Association 5 (1): 9–15. [PubMed] [Google Scholar]
- Temkin‐Greener, H. , Zheng N., Cai S., Zhao H., and Mukamel D.. 2010. “Nursing Home Environment and Organizational Performance: Association with Deficiency Citations.” Medical Care 48 (4): 357–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xing, J. , Mukamel D. B., and Temkin‐Greener H.. 2013. “Hospitalizations of Nursing Home Residents in the Last Year of Life: Nursing Home Characteristics and Variation in Potentially Avoidable Hospitalizations.” Journal of the American Geriatrics Society 61 (11): 1900–1908. doi:10.1111/jgs.12517. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.


