Abstract
Background:
Sleep disturbances are among the most common symptoms of military personnel who return from deployment. The objective of our study was to determine the presence of sleep disorders in US military personnel referred for evaluation of sleep disturbances after deployment and examine associations between sleep disorders and service-related diagnoses of depression, mild traumatic brain injury, pain, and posttraumatic stress disorder (PTSD).
Methods:
This was a cross-sectional study of military personnel with sleep disturbances who returned from combat within 18 months of deployment. Sleep disorders were assessed by clinical evaluation and polysomnogram with validated instruments to diagnose service-related illnesses.
Results:
Of 110 military personnel included in our analysis, 97.3% were men (mean age, 33.6 ± 8.0 years; mean BMI, 30.0 ± 4.3 kg/m2), and 70.9% returned from combat within 12 months. Nearly one-half (47.3%) met diagnostic criteria for two or more service-related diagnoses. Sleep disorders were diagnosed in 88.2% of subjects; 11.8% had a normal sleep evaluation and served as control subjects. Overall, 62.7% met diagnostic criteria for obstructive sleep apnea (OSA) and 63.6% for insomnia. The exclusive diagnoses of insomnia and OSA were present in 25.5% and 24.5% of subjects, respectively; 38.2% had comorbid insomnia and OSA. Military personnel with comorbid insomnia and OSA were significantly more likely to meet criteria for depression (P < .01) and PTSD (P < .01) compared with control subjects and those with OSA only.
Conclusions:
Comorbid insomnia and OSA is a frequent diagnosis in military personnel referred for evaluation of sleep disturbances after deployment. This diagnosis, which is difficult to treat, may explain the refractory nature of many service-related diagnoses.
Sleep disturbances are reported in almost one-third of military personnel who have deployed in support of Overseas Contingency Operations (OCO), resulting in approximately 600,000 military personnel and veterans with clinically relevant sleep conditions.1 US Department of Defense medical data report a marked increase in the incident diagnoses of insomnia and obstructive sleep apnea (OSA) across all services.2,3 From 2001 to 2009, the diagnostic rates for insomnia and OSA increased by 19 and 5.8 times, respectively. Yet to date, the research on sleep disorders in military personnel is limited to subjective assessment tools or retrospective analyses.1,4‐8 Thus, there is limited understanding of the etiology of sleep disorders and the contributing impact of comorbid psychologic and medical factors.
Sleep disturbances in military personnel are attributed to a multifactorial process. Deployment across multiple time zones results in circadian misalignment.9 Chronic sleep deprivation, a component of the military culture,10 is exacerbated by the physical and emotional stressors of deployment; this results in sleep fragmentation and insomnia.4 Mission requirements foster maladaptive sleep practices such as excess caffeine intake and the use of sedative hypnotics.11,12 Upon returning from combat operations, sleep disturbances frequently persist.1,4,13,14 It is currently unknown, though, if deployment exacerbates a previously undiagnosed sleep disorder or results in the onset of a new sleep disorder. The sleep disorder most likely to develop as a result of deployment is insomnia.5,8 However, military personnel in previous studies that included polysomnography (PSG) were diagnosed primarily with OSA.6,7,15 Conceivably, comorbid insomnia and OSA, a condition originally termed “complex insomnia” in 2001,16 may be an underdiagnosed or misdiagnosed clinical entity.17 Moreover, sleep-disordered breathing may be aggravated by the detrimental effects of insomnia and sleep deprivation motivating military personnel to seek care. Failure to fully address all aspects of disordered sleep could result in a less-than-optimal clinical response, potentially compromising the ability of service members to perform military duties or respond fully to treatments.
In addition to sleep disorders, current studies link combat or war-zone experiences to the development of chronic psychologic and physical health problems, including the service-related illnesses of traumatic brain injury (TBI), posttraumatic stress disorder (PTSD), depression, and chronic pain.13,14,18,19 We recently reported that 58.1% of military personnel undergoing a sleep study have one or more medical comorbidities, and that those diagnosed with insomnia are two times more likely to have PTSD and 1.5 times more likely to have pain.15 Collen et al8 reported on 116 soldiers with TBI, noting 97.4% had sleep complaints, with insomnia and OSA as the primary diagnoses. A more comprehensive assessment of sleep disorders and associated diagnoses may demonstrate important implications for the health and well-being of military personnel.
Our study assessed the presence of sleep disorders in military personnel presenting for the evaluation of sleep disturbances after deployment, as well as the service-related diagnoses of depression, mild TBI, pain, and PTSD. The purpose of the study was to determine relationships between service-related diagnoses in military personnel with sleep disorders.
Materials and Methods
Study Design
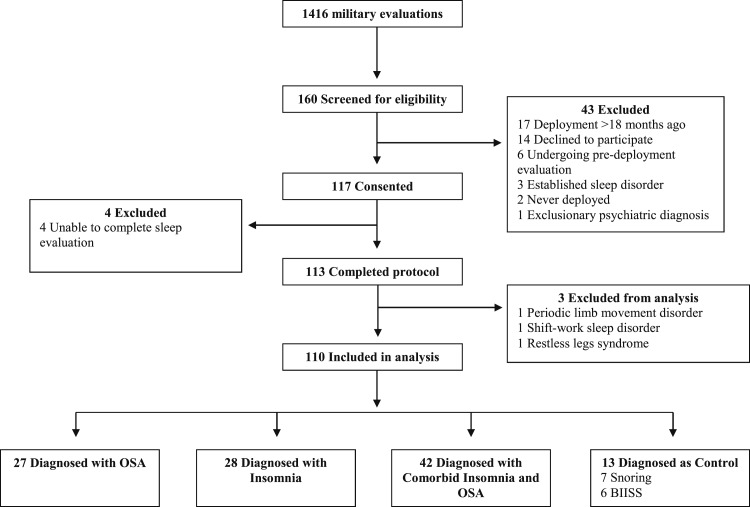
This was a cross-sectional study of US military personnel presenting for an initial evaluation of sleep disturbances. The study was approved by the institutional review board at Madigan Army Medical Center (Protocol #210090), and informed consent was obtained from each participant prior to any measurements. Participants were recruited by advertisements in the Sleep Medicine Clinic and notification by clinic personnel regarding the study. All 1,416 military personnel who underwent a sleep medicine evaluation between March 2011 and May 2012 were potentially eligible to participate. There were 160 who volunteered for participation in the study protocol and underwent eligibility screening (Fig 1). Inclusion criteria included the following: active-duty military personnel presenting for an initial evaluation of sleep disturbances and having returned from deployment within 18 months. Exclusion criteria included the following: no ongoing treatment, or military administrative actions regarding drug or alcohol abuse, or unstable psychiatric diagnoses (ie, schizophrenia or bipolar disorder). One hundred and seventeen patients met eligibility criteria and consented to enrollment. Four subjects were excluded for failure to complete the PSG and sleep medicine evaluation. One hundred thirteen subjects completed baseline assessments, clinical evaluations, and a diagnostic PSG. For these analyses, we excluded three participants who were diagnosed with uncommon sleep disorders in our cohort: periodic limb movement disorder (n = 1), restless legs syndrome (n = 1), and shift-work sleep disorder (n = 1). While these represent significant sleep disorders, their small numbers limit our ability to identify substantive relationships with the variables of interest.
Figure 1.
Inclusion criteria for study participants. BIISS = behaviorally induced insufficient sleep syndrome; OSA = obstructive sleep apnea.
Sleep Medicine Evaluation
All participants underwent a sleep medicine evaluation and diagnostic, attended PSG using standardized techniques. PSG was performed with 16 channels, including electrooculogram, EEG, ECG, electromyogram (submental, bilateral tibial), airflow measurements using both oronasal-thermal sensors and nasal air pressure transducers, tracheal sounds via microphone, rib cage and abdominal movement by inductance plethysmography using thoracoabdominal belts, and continuous pulse oximetry. The patient’s sleep period was approximately 8 h long with recording time starting at approximately 9:30 pm and ending at 5:30 am. This sleep period is conducive for the evaluation of military personnel and their duty requirements. We used the American Academy of Sleep Medicine alternate scoring method for hypopneas requiring a ≥ 50% decrease in the nasal pressure signal excursion from baseline lasting ≥ 10 s with either a ≥ 3% desaturation or an arousal.20 PSGs were scored and interpreted in accordance with American Academy of Sleep Medicine criteria.20 Six of the participants with OSA underwent a split-night PSG in accordance with our laboratory’s standard procedures. The PSG variables we analyzed included sleep onset latency, rapid eye-movement onset latency, total sleep time, wakefulness after sleep onset, sleep efficiency, arousal index, sleep stages (stages N1-3, stage R), apnea-hypopnea index (AHI), and maximal desaturation.
Sleep diagnoses were classified in accordance with the International Classification of Sleep Disorders, Second Edition,21 integrating the clinical assessment, PSG, and questionnaires. For the diagnosis of insomnia, participants were required to have one or more sleep-related complaints consisting of difficulty initiating sleep, maintaining sleep, waking too early, or sleep that is chronically nonrestorative or of poor quality with at least one of the associated symptoms of daytime impairment. The diagnosis of OSA was rendered in cases where the participant’s PSG demonstrated apneas or hypopneas with an AHI > 5/h. For the purposes of this study, the diagnoses of insomnia and OSA were not mutually exclusive; specifically, the diagnosis of comorbid insomnia and OSA was rendered if the participant met criteria for insomnia and if the AHI was > 5/h, unless their insomnia symptoms were solely from a service-related diagnosis or another medical disorder, in accordance with Research Diagnostic Criteria for insomnia related to sleep apnea.22 For analysis purposes, we used the following diagnostic categories: insomnia, comorbid insomnia and OSA, OSA, and control subjects, as these were the most frequent diagnoses rendered. Control subjects were participants diagnosed with behaviorally induced insufficient sleep syndrome or snoring with an otherwise normal PSG. While these military personnel are not without sleep disturbances, our prior research validated these diagnoses as an acceptable control population for military personnel.15 All diagnoses were adjudicated by a physician board-certified in sleep medicine (V. M.).
Demographic characteristics included sex, age, BMI, education, branch of service, rank, deployment history (number and times each military participant left their home base in support of OCO), and time since most recent deployment. Medications that the participants were taking at the time of their PSG were recorded in the following categories: antidepressants, atypical antipsychotics, benzodiazepines, nonbenzodiazepine receptor agonists (NBDRAs), prazosin, and narcotics.
Questionnaires
Clinical data regarding combat experiences, including TBI, psychologic health, pain, and sleep were obtained using validated scales that have demonstrated reliability and validity. The Combat Experiences Scale was used to assess combat intensity, with scores ranging from 0 to 15, with a higher score indicating more, different combat-related exposures on one or more occasions.23 The assessment of TBI was determined using the Warrior Administered Retrospective Casualty Assessment Tool. This tool obtains data on possible TBI-related war injuries as well as postdeployment injuries, assessing alteration of consciousness and presence of postconcussive symptoms at the time of injury.24 The diagnosis of mild TBI was made in accordance with the American Congress of Rehabilitation Medicine mild TBI criteria, which required an injury event followed by a loss of consciousness or alteration of mental state.25
PTSD was assessed by the PTSD Checklist Military Version, with a score of ≥ 50 resulting in a positive diagnostic screen, which is a score that provides the maximum specificity (0.98) and is consistent with the Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders, Third Edition, Revised.26 The Quick Inventory of Depressive Symptoms was used to screen for depression, using a cutoff score of 11 for a positive screen for depression.27 Chronic pain was evaluated using the RAND 36-Item Short-Form Health Survey component for the bodily pain score. We used this score in conjunction with the subject’s medical record to determine a diagnosis of pain, by either score < 70 for military personnel with a pain diagnosis in their electronic medical record,28 or by low bodily pain subscale score (< 30) on the RAND 36-Item Short Form Health Survey.29
Subjective sleep assessments included the following: self-reported habitual sleep duration; measures of sleep quality including difficulties falling asleep, staying asleep, frequent awakenings, and reporting sleep was not sound or refreshing; and the Epworth Sleepiness Scale (ESS), which assesses an individual’s “likelihood of dozing or falling asleep” in eight situations of daily living. Scores > 10 on the ESS are consistent with significant sleepiness.30
Statistical Analysis
Data are presented as the mean ± SD or No. (%). To determine differences among the sleep diagnoses groups, χ2 tests with post hoc standardized residuals test for categorical variables were used; one-way analysis of variance with post hoc analyses was performed using the Bonferroni correction for multiple comparisons. The significance level for group comparisons was set at 0.05 and was corrected for multiple comparisons. The mean and proportional differences among participant groups for the demographic characteristics and the health-related variables are reported in Tables 1 to 3. Data were analyzed using Predictive Analytics SoftWare version 18.0 (IBM).
Table 1.
—Characteristics of Study Participants
| Characteristics | Overall (N = 110) | Insomnia (n = 28) | Comorbid (n = 42) | OSA (n = 27) | Control Subjects (n = 13) | χ2 or F | P Value |
| Demographics | |||||||
| Male sex | 107 (97.3) | 26 (92.9) | 42 (100.0) | 27 (100.0) | 12 (92.3) | 5.20 | .158 |
| Age, y | 33.6 ± 8.0 | 31.4 ± 7.5a | 33.8 ± 7.9 | 38.6 ± 7.2a,b | 27.8 ± 5.7b | 7.67 | < .001 |
| BMI, kg/m2 | 30.0 ± 4.3 | 27.8 ± 3.9a,b | 31.6 ± 3.7a,c | 31.3 ± 4.1b,d | 27.0 ± 4.0c,d | 8.77 | < .001 |
| Education, y | 13.9 ± 2.0 | 13.8 ± 1.9 | 13.7 ± 1.7 | 13.9 ± 2.1 | 14.6 ± 3.5 | 0.43 | .735 |
| Branch of service | 0.99 | .804 | |||||
| Army | 102 (92.7) | 26 (92.9) | 40 (95.2) | 24 (88.9) | 12 (92.3) | ||
| Air Force | 8 (7.3) | 2 (7.1) | 2 (4.8) | 3 (11.1) | 1 (7.7) | ||
| Rank | 12.38 | .054 | |||||
| Junior enlisted (E1-E4) | 69 (62.7) | 19 (67.9) | 29 (69.0) | 13 (48.1) | 8 (61.5) | ||
| Senior enlisted (E5-E9) | 34 (30.9) | 7 (25.0) | 12 (28.6) | 13 (48.1) | 2 (15.4) | ||
| Officers | 7 (6.4) | 2 (7.1) | 1 (2.4) | 1 (3.7) | 3 (23.1) | ||
| Deployments, No. | 7.31 | .605 | |||||
| 1 | 39 (35.5) | 11 (39.3) | 16 (38.1) | 5 (18.5) | 7 (53.8) | ||
| 2 | 28 (25.5) | 7 (25.0) | 11 (26.2) | 8 (29.6) | 2 (15.4) | ||
| 3 | 25 (22.7) | 6 (21.4) | 7 (16.7) | 9 (33.3) | 3 (23.1) | ||
| ≥ 4 | 18 (16.4) | 4 (14.3) | 8 (19.0) | 5 (18.5) | 1 (7.7) | ||
| Time since last deployment, mo | 9.90 | .359 | |||||
| < 3 | 15 (13.6) | 1 (3.6) | 10 (23.8) | 3 (11.1) | 1 (7.7) | ||
| 3-6 | 18 (16.4) | 6 (21.4) | 5 (11.9) | 4 (14.8) | 3 (23.1) | ||
| 6-12 | 45 (40.9) | 14 (50.0) | 16 (38.1) | 9 (33.3) | 6 (46.2) | ||
| 12-18 | 32 (29.1) | 7 (25.0) | 11 (26.2) | 11 (40.7) | 3 (23.1) |
Data are presented as No. (%) or mean ± SD. OSA= obstructive sleep apnea.
Groups with the same letter(s) represent significant differences as tested by one-way analysis of variance with post hoc analysis with Bonferroni correction.
Table 3.
—Medications by Class
| Medication | Overall (N = 110) | Insomnia (n = 28) | Comorbid (n = 42) | OSA (n = 27) | Control Subjects (n= 13) | χ2 | P Value |
| Currently on medications | 41 (37.3) | 12 (42.9) | 21 (50.0)a,b | 6 (22.2)a | 2 (15.4)b | 8.56 | < .05 |
| NBDRA | 6 (5.5) | 2 (7.1) | 3 (7.1) | 1 (3.7) | 0 (0.0) | 1.30 | .730 |
| Antidepressants | 30 (27.3) | 8 (28.6)a | 18 (42.9)b | 2 (7.4)a,b | 2 (15.4) | 11.47 | < .01 |
| Atypical antipsychotics | 2 (1.8) | 1 (3.6) | 1 (2.4) | 0 (0.0) | 0 (0.0) | 1.30 | .730 |
| Benzodiazepines | 4 (3.6) | 3 (10.7) | 0 (0.0) | 1 (3.7) | 0 (0.0) | 6.08 | .108 |
| Narcotics | 18 (16.4) | 6 (21.4) | 9 (21.4) | 3 (11.1) | 0 (0.0) | 4.40 | .221 |
| Prazosin | 6 (5.5) | 2 (7.1) | 4 (9.5) | 0 (0.0) | 0 (0.0) | 3.81 | .283 |
Data are presented as No. (%) unless otherwise indicated. NBDRA = nonbenzodiazepine receptor agonist. See Table 1 legend for expansion of other abbreviation.
Groups with the same letter(s) represent significant differences as tested by χ2 analysis.
Results
This study included 110 active duty military personnel. Most participants were men (97.3%), and 92.7% were active duty in the US Army; 7.3% were active duty in the US Air Force (Table 1). The mean age of participants was 33.6 ± 8.0 years. Most participants recently returned from deployment, with 70.9% in the past year; 64.5% had deployed multiple times. Ninety-seven participants (88.2%) were diagnosed with a sleep disorder and 13 (11.8%) served as control subjects (Table 1). Sixty-nine (62.7%) met PSG criteria for OSA with an AHI > 5 and 70 (63.6%) for insomnia using International Classification of Sleep Disorders, Second Edition, criteria for insomnia. Participants are grouped into the diagnostic categories of insomnia, comorbid insomnia and OSA, OSA, and control subjects.
The category comorbid insomnia and OSA applied to 38.2% of the cohort. Insomnia and OSA were exclusively diagnosed in 25.5% and 24.5% of subjects, respectively. The mean BMIs of participants in the comorbid insomnia and OSA group (31.6 ± 3.7 kg/m2) and OSA group (31.3 ± 4.1 kg/m2) were elevated compared with the control group (27.0 ± 4.0 kg/m2) (P = .001, P < .01, respectively) and insomnia group (27.8 ± 3.9 kg/m2) (P = .001, P < .01, respectively) (Table 1). Reported habitual sleep duration was less in participants with insomnia (5.5 ± 1.3 h) (P < .05) and subjects with comorbid insomnia and OSA (5.1 ± 1.3 h) (P < .001) compared with control subjects (6.8 ± 1.0 h) (Table 2). The mean ESS for all participants was 13, consistent with abnormal daytime sleepiness, which did not differ among the groups (Table 2).
Table 2.
—Validated Questionnaires and Service-Related Diagnoses
| Variable | Overall (N = 110) | Insomnia (n = 28) | Comorbid (n = 42) | OSA (n = 27) | Control Subjects (n = 13) | χ2 or F | P Value |
| Questionnaires | |||||||
| PCL-M | 40.3 ± 16.2 | 42.2 ± 16.6a | 48.6 ± 15.4b,c | 29.4 ± 10.7a,b | 31.9 ± 11.2c | 11.63 | < .001 |
| QIDS | 10.3 ± 5.0 | 10.9 ± 5.1a | 13.0 ± 4.1b,c | 6.5 ± 3.1a,b | 8.0 ± 5.0c | 14.41 | < .001 |
| SF-36 Bodily Pain | 58.6 ± 25.2 | 53.0 ± 25.1 | 50.9 ± 23.8a,b | 69.4 ± 24.0a | 73.3 ± 20.5b | 5.46 | < .01 |
| CES | 6.5 ± 4.3 | 7.5 ± 4.5 | 7.1 ± 4.2 | 4.9 ± 3.9 | 5.5 ± 4.4 | 2.34 | .077 |
| ESS | 13.0 ± 5.2 | 12.3 ± 4.5 | 12.8 ± 5.7 | 14.5 ± 4.9 | 12.2 ± 5.0 | 1.05 | .375 |
| SR-Habitual Sleep Duration | 5.6 ± 1.3 | 5.5 ± 1.3a | 5.1 ± 1.3b | 6.0 ± 1.1 | 6.8 ± 1.0a,b | 6.73 | < .001 |
| Diagnosis | |||||||
| > 2 | 52 (47.3) | 14 (50.0)a | 28 (66.7)b,c | 6 (22.2)a,b | 4 (30.8)c | 14.64 | < .01 |
| None | 33 (30.0) | 7 (25.0) | 6 (14.3)a,b | 13 (48.1)a | 7 (53.8)b | 13.03 | < .01 |
| PTSD | 39 (35.5) | 10 (35.7)a | 25 (59.5)b,c | 2 (7.4)a,b | 2 (15.4)c | 22.20 | < .001 |
| Depression | 49 (44.5) | 12 (42.9)a,b | 30 (71.4)a,c,d | 3 (11.1)b,c | 4 (30.8)d | 25.54 | < .001 |
| Pain | 43 (39.1) | 14 (50.0) | 17 (40.5) | 10 (37.0) | 2 (15.4) | 4.55 | .208 |
| Mild TBI | 48 (43.6) | 14 (50.0) | 23 (54.8) | 7 (25.9) | 4 (30.8) | 6.89 | .075 |
Data are presented as No. (%) or mean ± SD. CES = Combat Experiences Scale; ESS = Epworth Sleepiness Scale; PCL-M = PTSD Checklist Military Version; PTSD = posttraumatic stress disorder; QIDS = Quick Inventory of Depressive Symptoms; SF-36 = RAND 36-Item Short-Form Health Survey; SR-Habitual Sleep Duration = Self-Reported Habitual Sleep Duration; TBI = traumatic brain injury. See Table 1 legend for expansion of other abbreviation.
Groups with the same letter(s) represent significant differences as tested by one-way analysis of variance with post hoc analysis with Bonferroni correction or χ2 analysis.
Seventy percent of our cohort exhibited service-related diagnoses with a mean of 1.6 (± 1.4) diagnoses, which included depression, mild TBI, pain, and PTSD (Table 2). The comorbid insomnia and OSA group reported the highest scores on the Quick Inventory of Depressive Symptoms and PTSD Checklist Military Version, with 71.4% meeting criteria for depression and 59.5% for PTSD, rates that were far higher than the control group (P = .001) and the OSA group (P < .001). Not surprisingly, subjects in the comorbid insomnia and OSA group were also more likely than those in the OSA group to be taking one of the medication classes assessed (P < .05) as well as antidepressants (P < .01) (Table 3).
Post hoc analysis among the four diagnostic groups revealed a significant increase in rapid eye-movement latency in the insomnia vs the OSA group (+65.6; P = .01) (Table 4). Comparing the severity of sleep-disordered breathing in military personnel with OSA vs the comorbid insomnia and OSA group, those with OSA had a higher AHI (+14.0; P = .001), with a similar desaturation percentage (Table 4). Otherwise, there were no significant differences in the PSG variables between the OSA and comorbid insomnia and OSA groups.
Table 4.
—Polysomnographic Variables by Sleep Diagnoses
| Variable | Overall (N = 110) | Insomnia (n = 28) | Comorbid (n = 42) | OSA (n = 27) | Control Subjects (n = 13) | F | P Value |
| SOL, min | 10.3 ± 15.3 | 12.9 ± 22.6 | 12.6 ± 15.2 | 5.3 ± 4.9 | 7.5 ± 6.0 | 1.72 | .168 |
| REM latency, min | 114.6 ± 78.3 | 145.1 ± 93.2a | 114.7 ± 77.2 | 79.6 ± 54.4a | 121.0 ± 66.3 | 3.47 | < .05 |
| TST, min | 422.9 ± 57.1 | 422.7 ± 50.7 | 421.9 ± 59.7 | 420.1 ± 64.1 | 432.4 ± 51.8 | 0.14 | .935 |
| Sleep efficiency, % | 91.3 ± 6.7 | 90.6 ± 9.0 | 90.3 ± 7.0 | 92.4 ± 3.5 | 93.7 ± 4.0 | 1.25 | .296 |
| Stage N1, % | 11.3 ± 7.0 | 9.4 ± 4.7 | 11.8 ± 5.5 | 13.8 ± 11.0 | 8.7 ± 3.3 | 2.51 | .063 |
| Stage N2, % | 43.5 ± 9.1 | 44.1 ± 8.8 | 43.3 ± 9.6 | 43.4 ± 10.3 | 43.1 ± 5.8 | 0.06 | .981 |
| Stage N3, % | 19.7 ± 9.2 | 20.7 ± 9.1 | 18.8 ± 8.6 | 18.9 ± 10.7 | 21.7 ± 8.3 | 0.53 | .660 |
| Stage R, % | 18.6 ± 8.3 | 16.7 ± 6.4 | 17.7 ± 6.2 | 21.4 ± 12.4 | 20.1 ± 5.9 | 1.88 | .137 |
| WASO, min | 38.0 ± 29.0 | 41.3 ± 40.1 | 41.9 ± 28.0 | 33.6 ± 19.6 | 27.7 ± 16.6 | 1.14 | .338 |
| Arousal index | 21.8 ± 16.7 | 15.5 ± 10.3a | 22.3 ± 13.5 | 31.2 ± 25.0a,b | 14.8 ± 5.1b | 5.42 | < .01 |
| Apnea-hypopnea index | 13.4 ± 17.3 | 2.0 ± 1.4a,b | 14.7 ± 11.1a,c,d | 28.7 ± 24.5b,c,e | 1.9 ± 1.5d,e | 20.06 | < .001 |
| Desaturation, % | 86.0 ± 6.2 | 90.4 ± 3.8a,b | 84.0 ± 5.2a,c | 83.3 ± 7.3b,d | 88.8 ± 4.7c,d | 11.27 | < .001 |
| Self-reported sleep duration, h | 5.3 ± 1.7 | 5.5 ± 2.0 | 5.0 ± 1.3 | 5.4 ± 1.7 | 5.8 ± 2.0 | 0.88 | .457 |
Data are presented as mean ± SD. Desaturation = minimum recorded oximetry value during sleep; REM = rapid eye movement; SOL = sleep onset latency; TST = total sleep time; WASO = wakefulness after sleep onset. See Table 1 legend for expansion of other abbreviation.
Groups with the same letter(s) represent significant differences as tested by one-way analysis of variance with post hoc analysis with Bonferroni correction.
Discussion
To our knowledge, this is the first study to diagnose sleep disorders with a clinical evaluation and PSG, as well as associated psychologic and medical comorbidities, using validated clinical instruments in a sample of military personnel recently returned from deployment. In military personnel with sleep disturbances after deployment that warranted a sleep medicine evaluation, 88.2% were diagnosed with a clinically significant sleep disorder. Considering insomnia and OSA as separate disorders, 62.7% subjects met PSG criteria for OSA and 63.6% clinical criteria for insomnia. However, if comorbid insomnia and OSA is classified as a distinct disorder, it was the most common diagnosis in 38.2% of subjects. The reported incidence of sleep disturbances in military personnel and veterans who served in OCO ranges from 30% to 93.5%1,4,13,14; yet, most research efforts have focused on the diagnoses of mild TBI and PTSD. Sleep disorders are increasingly recognized by medical providers; nonetheless, it is common to ascribe sleep disturbances solely to insomnia or an associated diagnosis,8,31 and delay or forgo a definitive sleep evaluation and PSG. This delay further aggravates the difficulties in treating service-related diagnoses of depression, mild TBI, and PTSD.32,33
Our finding that comorbid insomnia and OSA (“complex insomnia”) was a frequent diagnosis in military personnel with combat exposures is consistent with previously reported civilian studies of patients who had traumatic experiences.16,34,35 As our study, to our knowledge, is the first substantial assessment of the complex insomnia diagnosis in military personnel, it raises concerns about whether comorbid insomnia and OSA is underreported in military personnel as has been noted in civilian studies.17,36 In the literature, there are two distinct groups of patients with comorbid insomnia and OSA: patients without an associated behavioral-medicine diagnosis37,38 and those who have anxiety, depression, or PTSD with comorbid insomnia and OSA.16,34,35,39,40 Most of the patients with comorbid insomnia and OSA (66.7%) met criteria for a service-related diagnosis, which is consistent with the “complex sleep disorders or complex insomnia” model postulated by Krakow et al31 that integrates their sleep and behavioral-medicine diagnoses and treatment. A recent study showed compliance with CPAP in soldiers with OSA and PTSD, many of whom had comorbid insomnia and OSA, was suboptimal, suggesting that treating this syndrome is difficult.33 Another study reported that achieving CPAP compliance in these patients requires much more effort, which is consistent with our clinical experience.41 There are no definitive treatment recommendations for comorbid insomnia and OSA, although combined therapy addressing insomnia with cognitive behavioral therapy and either surgical treatment or CPAP for OSA has shown promise.38,42‐44
In this study, we report that medical and psychologic comorbidities are frequent in military personnel referred for sleep disturbances, with 70% having at least one of the following: depression, mild TBI, pain, or PTSD, and almost one-half (47.3%) reporting two or more diagnoses. These rates are similar to studies that used either an interview or questionnaire to determine rates of diagnoses, and lower than studies that relied on retrospective reviews of medical records.13,45‐48 Patients with comorbid insomnia and OSA had the highest rates of depression, mild TBI, PTSD, and two or more diagnoses. When compared with both the control and OSA groups, these were significant differences except for mild TBI, which trended toward significance. This finding is consistent with previous reports in which patients with comorbid insomnia and OSA had elevated rates of psychiatric diagnoses and illustrates the multifaceted nature of complex insomnia in military personnel.49
Medication use, especially antidepressants and narcotics, was frequent in our cohort and highest in military personnel diagnosed with comorbid insomnia and OSA. Notably, while 63.7% of the participants received an insomnia diagnosis, only 5.5% were receiving an NBDRA. Possible explanations for this include that participants with insomnia were not previously diagnosed with this sleep disorder, that is, were referred solely for sleep disturbances, or that prior treatment with an NBDRA was not effective, thus, resulting in a sleep referral. Similarly, while 35.5% of participants met diagnostic criteria for PTSD, only 5.5% were receiving prazosin, a medication used in the treatment of nightmares. Previous studies have shown that OSA is more prevalent in both veteran and nonveteran populations with PTSD and mental health disorders.41,50‐52 This is consistent with our finding of a high prevalence of sleep-disordered breathing (62.7%) in our cohort. Seal et al53 recently reported veterans with PTSD were 2.6 times more likely to receive opioids and 5.5 times more likely to receive sedative hypnotics than those without PTSD. In this study, prescription opioids were associated with adverse outcomes (eg, ED or inpatient admissions). While there are no studies, to our knowledge, that specifically addressed this, a sleep medicine evaluation early in the diagnoses of PTSD and pain could conceivably help mitigate medication-related complications. Treating insomnia and OSA with nonpharmacologic therapies such as cognitive behavioral therapy and CPAP may well decrease the need for, and the complications of, sedatives and opioids; the latter have been known to exacerbate OSA or even provoke central sleep apnea.
The pathogenesis of sleep disorders, specifically the onset of symptoms, in participants in our study is unknown as there was no difference in number of deployments or time from deployment among the diagnostic groups. The most likely etiology in those that received a diagnosis of insomnia is that it developed, in part, due to stressors during their deployment, as their Combat Experiences Scale scores were the highest.4,5 It is also more than likely that some proportion of participants in our study who were diagnosed with OSA suffered from this condition prior to deployment. Hoge et al13 suggests disturbed sleep in combat, which is the result of prolonged operations or lack of quality sleep due to insomnia, is a potential precursor not only to PTSD but to postconcussive symptoms following a TBI. There is evidence that disturbed sleep prior to a traumatic event poses an increased risk of PTSD.54 The importance of this temporal relationship is further illustrated by a study of military personnel that reported high levels of sleep disturbances following deployment, which were subsequently linked to a greater risk for PTSD.55 As our study shows high rates of insomnia and sleep-disordered breathing in otherwise young, healthy military personnel, it is possible that prolonged sleep deprivation along with fragmentation and hyperarousal due to the physical and psychologic stressors of combat contributed to the pathogenesis of not only insomnia but OSA as well. A potential mechanism is the combined effects of sleep deprivation, which are known to exacerbate sleep-disordered breathing,56,57 and increased arousals resulting in the development of OSA. Arousals are typically viewed as protective for patients with OSA. In some patients with OSA, arousals can cause ventilatory instability by triggering ventilatory overshoot, resulting in an increased tendency for upper airway collapse.58,59
There are several limitations to our study that should be addressed. Participation in our study was low, with only 11.3% of potentially eligible military personnel referred for screening. It is possible that through this selection bias, only those with more significant sleep disturbances volunteered for our study. This could elevate the percentage of those diagnosed with sleep disorders and service-related illnesses. Our control group was not truly normal, as control subjects had sleep complaints and nearly one-half had a service-related diagnosis. This may have minimized the differences between the diagnostic and control groups regarding service-related diagnoses. The cross-sectional nature of our study did not allow us to definitively establish the onset or etiology of the sleep disorders rendered. Military personnel are assessed for medical disorders prior to deployment and receive appropriate evaluations to ensure predeployment conditions are addressed. Thus, it is more than likely that their deployment experiences contributed in some part to the development or worsening of their sleep disorder. Six participants in our study underwent a split-night PSG. This likely affected their AHI but would not have otherwise affected their sleep diagnosis. As we only evaluated military personnel, the results of our study likely do not apply to all patients with sleep disturbances, but are potentially applicable to civilians who experience significant trauma, especially those who subsequently develop PTSD or TBI. Although there are limits to our methods, this is the first study, to our knowledge, to comprehensively assess sleep disorders and service-related diagnoses in military personnel and can serve as a reference for larger studies that are required given the scope of this problem.
The nearly universal feature of all service-related diagnoses is the complaint of “sleep disturbances,” and our findings show it is not merely sleep disturbances but specific “sleep disorders” in the majority of cases. Although our study included only military personnel, sleep disturbances are present in virtually all patients with TBI and PTSD. Thus, our findings of a high prevalence of sleep-disordered breathing and comorbid insomnia and OSA are likely applicable to physicians who treat civilian patients with similar traumatic experiences. Of considerable clinical import, seeking care for disturbed sleep does not typically carry the stigma of mental health disorders in military personnel.60 Therefore, we believe sleep evaluations are an underused portal to address the complex disorders of military personnel and veterans. With the extremely high reported rates of sleep disturbances, the mounting evidence that these are specific sleep disorders, and that improved sleep results in enhanced outcomes, the requirement for sleep research in military personnel is substantial.
Acknowledgments
Author contributions: Dr Mysliwiec had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Dr Mysliwiec: contributed to the data collection, project design, and the majority of the manuscript writing.
Dr Gill: contributed to the project design, statistical and data analysis, and writing of the manuscript.
Dr Lee: contributed to the statistical and data analysis and editing of the manuscript.
Ms Baxter: contributed to the data collection, statistical and data analysis, and editing of the manuscript.
Ms Pierce: contributed to the data collection, project design, and writing of the manuscript.
Dr Barr: contributed to the project design and editing of the manuscript.
Dr Krakow: contributed to the editing of the manuscript.
Dr Roth: contributed to the editing of the manuscript.
Financial/nonfinancial disclosures: The authors have reported to CHEST the following conflicts of interest: Dr Krakow conducts continuing medical education/continuing education units educational programs for medical and mental health providers to learn about sleep disorders. Sometimes these programs involve the attendee paying a fee directly to the Sleep and Human Health Institute. Other times, Dr Krakow conducts the workshops at other locations, which may be paid for by vendors such as Respironics Inc and ResMed Corp, or other institutions such as the US Army Medical Department Center and School, Veterans Affairs Medical Centers, and regional sleep center conferences. He is also president of a nonprofit sleep research center, the Sleep & Human Health Institute, that occasionally provides consultation services or receives grants for pilot studies, the most recent of which were from the Con Alma Health Foundation; Respironics, Inc; GlaxoSmithKline plc; Covidien, Inc; the Simon Charitable Foundation; and the Oxnard Foundation. Drs Mysliwiec, Gill, Lee, Barr, Roth, and Mss Baxter and Pierce have reported that no potential conflicts of interest exist with any companies/organizations whose products or services may be discussed in this article.
Role of sponsors: The sponsors had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the manuscript. The opinions and assertions in this manuscript are those of the authors and do not necessarily represent those of the Department of the Army, Department of Defense, US Government, the National Institutes of Health, or the Center for Neuroscience and Regenerative Medicine.
Other contributions: This study was performed at the Madigan Army Medical Center.The authors thank the following for their contributions: Angela Mysliwiec, MD, Madigan Army Medical Center, for editing assistance and review of the manuscript, and Raywin Huang, PhD, Madigan Army Medical Center, for statistical consultation. Neither of these individuals received compensation for their contributions.
Abbreviations
- AHI
apnea-hypopnea index
- ESS
Epworth Sleepiness Scale
- NBDRA
nonbenzodiazepine receptor agonist
- OCO
Overseas Contingency Operations
- OSA
obstructive sleep apnea
- PSG
polysomnography
- PTSD
posttraumatic stress disorder
- TBI
traumatic brain injury
Footnotes
Funding/Support: This study was supported, in part, by the Center for Neuroscience and Regenerative Medicine [Grant 60855]. Funding support was provided by the intramural department of the National Institutes of Health, National Institute of Nursing Research (to Drs Gill and Lee).
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians. See online for more details.
References
- 1.Seelig AD, Jacobson IG, Smith B, et al. ; Millennium Cohort Study Team. Sleep patterns before, during, and after deployment to Iraq and Afghanistan. Sleep. 2010;33(12):1615-1622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Armed Forces Health Surveillance Center. Insomnia, active component, US Armed Forces, January 2000-December 2009. Medical Surveillance Monthly Report. 2010;17(5):12-15. [Google Scholar]
- 3.Armed Forces Health Surveillance Center. Obstructive sleep apnea, active component, US Armed Forces, January 2000-December 2009. Medical Surveillance Monthly Report. 2010;17(5):8-11. [Google Scholar]
- 4.Peterson AL, Goodie JL, Satterfield WA, Brim WL. Sleep disturbance during military deployment. Mil Med. 2008;173(3):230-235. [DOI] [PubMed] [Google Scholar]
- 5.Luxton DD, Greenburg D, Ryan J, Niven A, Wheeler G, Mysliwiec V. Prevalence and impact of short sleep duration in redeployed OIF soldiers. Sleep. 2011;34(9):1189-1195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Capaldi VF, II, Guerrero ML, Killgore WD. Sleep disruptions among returning combat veterans from Iraq and Afghanistan. Mil Med. 2011;176(8):879-888. [DOI] [PubMed] [Google Scholar]
- 7.Lettieri CJ, Eliasson AH, Andrada T, Khramtsov A, Raphaelson M, Kristo DA. Obstructive sleep apnea syndrome: are we missing an at-risk population? J Clin Sleep Med. 2005;1(4):381-385. [PubMed] [Google Scholar]
- 8.Collen J, Orr N, Lettieri CJ, Carter K, Holley AB. Sleep disturbances among soldiers with combat-related traumatic brain injury. Chest. 2012;142(3):622-630. [DOI] [PubMed] [Google Scholar]
- 9.Ferrer CF, Jr, Bisson RU, French J. Circadian rhythm desynchronosis in military deployments: a review of current strategies. Aviat Space Environ Med. 1995;66(6):571-578. [PubMed] [Google Scholar]
- 10.Miller NL, Shattuck LG, Matsangas P. Longitudinal study of sleep patterns of United States Military Academy cadets. Sleep. 2010;33(12):1623-1631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention. Great American Smokeout. MMWR. 2012;61(44):889-908.23134971 [Google Scholar]
- 12.Joint Mental Health Advisory Team 7 (J-MHAT 7). Operation Enduring Freedom 2010. Office of the Surgeon General United States Army Medical Command, Office of the Command Surgeon HQ, USCENTCOM and Office of the Command Surgeon US Forces Afghanistan USFOR-A. Joint Mental Health Advisory Team 7 (J-MHAT 7) Operation Enduring Freedom 2010 Afghanistan. Army Medicine website. http://www.armymedicine.army.mil/reports/mhat/mhat_vii/J_MHAT_7.pdf. Accessed November 5, 2012.
- 13.Hoge CW, McGurk D, Thomas JL, Cox AL, Engel CC, Castro CA. Mild traumatic brain injury in US soldiers returning from Iraq. N Engl J Med. 2008;358(5):453-463. [DOI] [PubMed] [Google Scholar]
- 14.Lew HL, Pogoda TK, Hsu PT, et al. Impact of the “polytrauma clinical triad” on sleep disturbance in a department of veterans affairs outpatient rehabilitation setting. Am J Phys Med Rehabil. 2010;89(6):437-445. [DOI] [PubMed] [Google Scholar]
- 15.Mysliwiec V, McGraw L, Pierce R, Smith P, Trapp B, Roth BJ. Sleep disorders and associated medical comorbidities in active duty military personnel. Sleep. 2013;36(2):167-174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Krakow B, Melendrez D, Pedersen B, et al. Complex insomnia: insomnia and sleep-disordered breathing in a consecutive series of crime victims with nightmares and PTSD. Biol Psychiatry. 2001;49(11):948-953. [DOI] [PubMed] [Google Scholar]
- 17.Al-Jawder SE, Bahammam AS. Comorbid insomnia in sleep-related breathing disorders: an under-recognized association. Sleep Breath. 2012;16(2):295-304. [DOI] [PubMed] [Google Scholar]
- 18.Seal KH, Bertenthal D, Miner CR, Sen S, Marmar C. Bringing the war back home: mental health disorders among 103,788 US veterans returning from Iraq and Afghanistan seen at Department of Veterans Affairs facilities. Arch Intern Med. 2007;167(5):476-482. [DOI] [PubMed] [Google Scholar]
- 19.Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med. 2004;351(1):13-22. [DOI] [PubMed] [Google Scholar]
- 20.Iber C, Ancoli-Israel S, Chesson AL, Jr, Quan SF. The AASM Manual for the Scoring of Sleep and Associated Events. Westchester, IL: American Academy of Sleep Medicine; 2007. [Google Scholar]
- 21.American Academy of Sleep Medicine. International Classification of Sleep Disorders: Diagnostic and Coding Manual.Second edition Westchester, IL: American Academy of Sleep Medicine; 2005. [Google Scholar]
- 22.Edinger JD, Bonnet MH, Bootzin RR, et al. ; American Academy of Sleep Medicine Work Group. Derivation of research diagnostic criteria for insomnia: report of an American Academy of Sleep Medicine Work Group. Sleep. 2004;27(8):1567-1596. [DOI] [PubMed] [Google Scholar]
- 23.Vogt DS, Proctor SP, King DW, King LA, Vasterling JJ. Validation of scales from the Deployment Risk and Resilience Inventory in a sample of Operation Iraqi Freedom veterans. Assessment. 2008;15(4):391-403. [DOI] [PubMed] [Google Scholar]
- 24.Terrio H, Brenner LA, Ivins BJ, et al. Traumatic brain injury screening: preliminary findings in a US Army Brigade Combat Team. J Head Trauma Rehabil. 2009;24(1):14-23. [DOI] [PubMed] [Google Scholar]
- 25.American Congress of Rehabilitation Medicine. Definition of mild traumatic brain injury. American Congress of Rehabilitation Medicine website. http://www.acrm.org/pdf/TBIDef_English_Oct2010.pdf. Accessed September 20, 2012.
- 26.Wilkins KC, Lang AJ, Norman SB. Synthesis of the psychometric properties of the PTSD checklist (PCL) military, civilian, and specific versions. Depress Anxiety. 2011;28(7):596-606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Trivedi MH, Rush AJ, Ibrahim HM, et al. The Inventory of Depressive Symptomatology, Clinician Rating (IDS-C) and Self-Report (IDS-SR), and the Quick Inventory of Depressive Symptomatology, Clinician Rating (QIDS-C) and Self-Report (QIDS-SR) in public sector patients with mood disorders: a psychometric evaluation. Psychol Med. 2004;34(1):73-82. [DOI] [PubMed] [Google Scholar]
- 28.McHorney CA, Ware JE, Jr, Lu JF, Sherbourne CD. The MOS 36-item Short-Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med Care. 1994;32(1):40-66. [DOI] [PubMed] [Google Scholar]
- 29.Sinnott C, Rogers MA, Lehmann D, Weinstock RS. Bodily pain, poor physical functioning, and poor glycemic control in adults with diabetes. Diabetes Care. 2005;28(6):1534. [DOI] [PubMed] [Google Scholar]
- 30.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14(6):540-545. [DOI] [PubMed] [Google Scholar]
- 31.Krakow B, Melendrez D, Warner TD, Dorin R, Harper R, Hollifield M. To breathe, perchance to sleep: sleep-disordered breathing and chronic insomnia among trauma survivors. Sleep Breath. 2002;6(4):189-202. [DOI] [PubMed] [Google Scholar]
- 32.Peppard PE, Reichmuth KJ. Sound sleep, a crucial component of military medicine’s armamentarium? Sleep. 2013;36(1):7-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Collen JF, Lettieri CJ, Hoffman M. The impact of posttraumatic stress disorder on CPAP adherence in patients with obstructive sleep apnea. J Clin Sleep Med. 2012;8(6):667-672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Krakow B, Melendrez D, Johnston L, et al. Sleep-disordered breathing, psychiatric distress, and quality of life impairment in sexual assault survivors. J Nerv Ment Dis. 2002;190(7):442-452. [DOI] [PubMed] [Google Scholar]
- 35.Krakow BJ, Melendrez DC, Johnston LG, et al. Sleep dynamic therapy for Cerro Grande Fire evacuees with posttraumatic stress symptoms: a preliminary report. J Clin Psychiatry. 2002;63(8):673-684. [DOI] [PubMed] [Google Scholar]
- 36.Luyster FS, Buysse DJ, Strollo PJ., Jr Comorbid insomnia and obstructive sleep apnea: challenges for clinical practice and research. J Clin Sleep Med. 2010;6(2):196-204. [PMC free article] [PubMed] [Google Scholar]
- 37.Chung KF. Insomnia subtypes and their relationships to daytime sleepiness in patients with obstructive sleep apnea. Respiration. 2005;72(5):460-465. [DOI] [PubMed] [Google Scholar]
- 38.Guilleminault C, Davis K, Huynh NT. Prospective randomized study of patients with insomnia and mild sleep disordered breathing. Sleep. 2008;31(11):1527-1533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Smith S, Sullivan K, Hopkins W, Douglas J. Frequency of insomnia report in patients with obstructive sleep apnoea hypopnea syndrome (OSAHS). Sleep Med. 2004;5(5):449-456. [DOI] [PubMed] [Google Scholar]
- 40.Yang CM, Liao YS, Lin CM, Chou SL, Wang EN. Psychological and behavioral factors in patients with comorbid obstructive sleep apnea and insomnia. J Psychosom Res. 2011;70(4):355-361. [DOI] [PubMed] [Google Scholar]
- 41.Krakow B, Melendrez D, Ferreira E, et al. Prevalence of insomnia symptoms in patients with sleep-disordered breathing. Chest. 2001;120(6):1923-1929. [DOI] [PubMed] [Google Scholar]
- 42.Wickwire EM, Collop NA. Insomnia and sleep-related breathing disorders. Chest. 2010;137(6):1449-1463. [DOI] [PubMed] [Google Scholar]
- 43.Schutte-Rodin S, Broch L, Buysse D, Dorsey C, Sateia M. Clinical guideline for the evaluation and management of chronic insomnia in adults. J Clin Sleep Med. 2008;4(5):487-504. [PMC free article] [PubMed] [Google Scholar]
- 44.Krakow B, Lowry C, Germain A, et al. A retrospective study on improvements in nightmares and post-traumatic stress disorder following treatment for co-morbid sleep-disordered breathing. J Psychosom Res. 2000;49(5):291-298. [DOI] [PubMed] [Google Scholar]
- 45.Vanderploeg RD, Belanger HG, Horner RD, et al. Health outcomes associated with military deployment: mild traumatic brain injury, blast, trauma, and combat associations in the Florida National Guard. Arch Phys Med Rehabil. 2012;93(11):1887-1895. [DOI] [PubMed] [Google Scholar]
- 46.Frayne SM, Chiu VY, Iqbal S, et al. Medical care needs of returning veterans with PTSD: their other burden. J Gen Intern Med. 2011;26(1):33-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hoge CW, Auchterlonie JL, Milliken CS. Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. JAMA. 2006;295(9):1023-1032. [DOI] [PubMed] [Google Scholar]
- 48.Brenner LA, Ivins BJ, Schwab K, et al. Traumatic brain injury, posttraumatic stress disorder, and postconcussive symptom reporting among troops returning from Iraq. J Head Trauma Rehabil. 2010;25(5):307-312. [DOI] [PubMed] [Google Scholar]
- 49.Krell SB, Kapur VK. Insomnia complaints in patients evaluated for obstructive sleep apnea. Sleep Breath. 2005;9(3):104-110. [DOI] [PubMed] [Google Scholar]
- 50.Sharafkhaneh A, Giray N, Richardson P, Young T, Hirshkowitz M. Association of psychiatric disorders and sleep apnea in a large cohort. Sleep. 2005;28(11):1405-1411. [DOI] [PubMed] [Google Scholar]
- 51.Krakow B, Haynes PL, Warner TD, et al. Nightmares, insomnia, and sleep-disordered breathing in fire evacuees seeking treatment for posttraumatic sleep disturbance. J Trauma Stress. 2004;17(3):257-268. [DOI] [PubMed] [Google Scholar]
- 52.Spoormaker VI, Montgomery P. Disturbed sleep in post-traumatic stress disorder: secondary symptom or core feature? Sleep Med Rev. 2008;12(3):169-184. [DOI] [PubMed] [Google Scholar]
- 53.Seal KH, Shi Y, Cohen G, et al. Association of mental health disorders with prescription opioids and high-risk opioid use in US veterans of Iraq and Afghanistan. JAMA. 2012;307(9):940-947. [DOI] [PubMed] [Google Scholar]
- 54.Bryant RA, Creamer M, O’Donnell M, Silove D, McFarlane AC. Sleep disturbance immediately prior to trauma predicts subsequent psychiatric disorder. Sleep. 2010;33(1):69-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.McLay RN, Klam WP, Volkert SL. Insomnia is the most commonly reported symptom and predicts other symptoms of post-traumatic stress disorder in U.S. service members returning from military deployments. Mil Med. 2010;175(10):759-762. [DOI] [PubMed] [Google Scholar]
- 56.Persson HE, Svanborg E. Sleep deprivation worsens obstructive sleep apnea. Comparison between diurnal and nocturnal polysomnography. Chest. 1996;109(3):645-650. [DOI] [PubMed] [Google Scholar]
- 57.Stoohs RA, Dement WC. Snoring and sleep-related breathing abnormality during partial sleep deprivation. N Engl J Med. 1993;328(17):1279. [DOI] [PubMed] [Google Scholar]
- 58.Ryan CM, Bradley TD. Pathogenesis of obstructive sleep apnea. J Appl Physiol. 2005;99(6):2440-2450. [DOI] [PubMed] [Google Scholar]
- 59.Younes M. Role of arousals in the pathogenesis of obstructive sleep apnea. Am J Respir Crit Care Med. 2004;169(5):623-633. [DOI] [PubMed] [Google Scholar]
- 60.Greene-Shortridge TM, Britt TW, Castro CA. The stigma of mental health problems in the military. Mil Med. 2007;172(2):157-161. [DOI] [PubMed] [Google Scholar]