Abstract
Background:
Critically ill, morbidly obese patients (BMI ≥ 40 kg/m2) are at high risk of respiratory failure requiring invasive mechanical ventilation (IMV). It is not clear if outcomes of critically ill, obese patients are affected by obesity. Due to limited cardiopulmonary reserve, they may have poor outcomes. However, literature to this effect is limited and conflicted.
Methods:
We used the Nationwide Inpatient Sample from 2004 to 2008 to examine the outcomes of morbidly obese people receiving IMV and compared them to nonobese people. We identified hospitalizations requiring IMV and morbid obesity using International Classification of Diseases, 9th Revision, Clinical Modification codes. Primary outcomes studied were inhospital mortality, rates of prolonged mechanical ventilation (≥ 96 h), and tracheostomy. Multivariable logistic regression was used to adjust for potential confounding variables. We also examined outcomes stratified by number of organs failing.
Results:
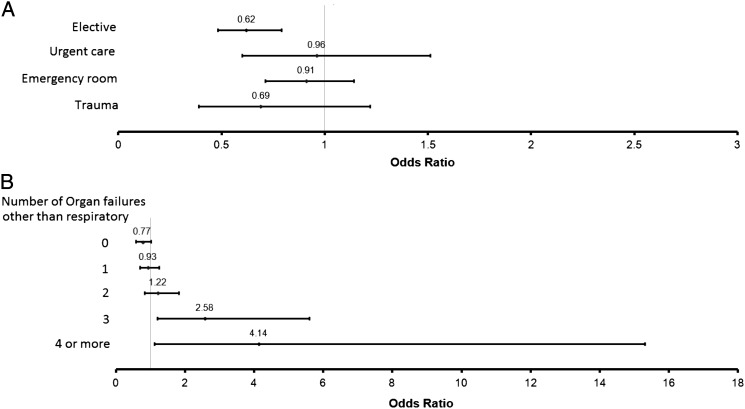
Of all hospitalized, morbidly obese people, 2.9% underwent IMV. Mean age, comorbidity score, and severity of illness were lower in morbidly obese people. The adjusted mortality was not significantly different in morbidly obese people (OR 0.89; 95% CI, 0.74-1.06). When stratified by severity of disease, there was a stepwise increase in risk for mortality among morbidly obese people relative to nonobese people (range: OR, 0.77; 95% CI, 0.58-1.01 for only respiratory failure, to OR, 4.14; 95% CI, 1.11-15.3 for four or more organs failing). Rates of prolonged mechanical ventilation were similar, but rate of tracheostomy (OR 2.19; 95% CI, 1.77-2.69) was significantly higher in patients who were morbidly obese.
Conclusions:
Morbidly obese people undergoing IMV have a similar risk for death as nonobese people if only respiratory failure is present. When more organs fail, morbidly obese people have increased risk for mortality compared with nonobese people.
Obesity is a growing epidemic in the United States, with a current prevalence estimated to be about 32% and 36% in the male and female populations, respectively.1 Approximately 7% of patients requiring admission to the ICU are morbidly obese (BMI > 40 kg/m2).2 Investigations focusing on outcomes of critically ill obese adults have demonstrated conflicting results. Although some studies suggest increased mortality,3,4 others have found a protective effect and lower risk of death.5‐7 Conclusions from most studies are limited by heterogeneous populations and varying definitions. Few specifically address outcomes of obese patients requiring invasive mechanical ventilation (IMV), especially the morbidly obese.8‐10 Secondary to its deleterious effects on pulmonary physiology, obesity11 in the critically ill has been independently associated with prolonged lengths of mechanical ventilation (MV) and ICU stay.3,4,12 A few recent analyses found that although the risk of developing ARDS was higher in obese and severely obese patients who are mechanically ventilated, all other outcomes based on BMI, including mortality, were no different.13,14
Given the inconsistent results of these small studies and the adverse consequences of morbid obesity on pulmonary physiology, which may lead to development of respiratory failure,15,16 it is important to clarify outcomes of such patients undergoing IMV. These investigations will enable health-care planners and policymakers to appropriately allocate resources toward an exponentially expanding population of obese patients.17
We hypothesized that hospitalized, morbidly obese people receiving IMV would have differences in outcomes of mortality, lengths of MV and hospital stay, and discharge dispositions in comparison with a nonobese cohort. We used a large, nationally representative database developed by the Agency of Health Care Research and Quality to ensure sufficient sample size and enhance the generalizability and external validity of our results.
Materials and Methods
Data Source
We used the Nationwide Inpatient Sample (NIS), the largest, all-payer, inpatient-care database publicly available in the United States. This administrative dataset contains data on 5 to 8 million hospital stays from about 1,000 hospitals sampled to approximate a 20% stratified sample of US community hospitals, but excludes federal hospitals. Each hospitalization is treated as an individual entry in the database and includes International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) codes for the principal diagnosis and up to 14 secondary diagnoses and 15 procedures associated with that stay. Details about the structure of the Healthcare Cost and Utilization Project-NIS database are available online.18 We used data from the years 2004 to 2008 for this study. Because we used a publicly available data set with no patient identifiers, this study was examined and found exempt from formal review by the institutional review board of the Medical College of Wisconsin.
Study Population
We used ICD-9-CM procedure codes 96.70 to 96.72 to identify adult patients aged ≥18 years who were receiving IMV.19 Similarly, we identified people with morbid obesity (BMI ≥ 40 kg/m2) using the ICD-9-CM code 278.01.20,21 Since many people with morbid obesity use noninvasive ventilation (NIV) chronically for sleep apnea syndromes, it is likely that procedure codes indicating this ventilation modality capture a large number of people without acute respiratory failure. We, therefore, restricted our attention only to IMV and excluded people receiving NIV. We also excluded people with ICD-9-CM codes identifying them as being either overweight or obese (BMI 25-39 kg/m2) (ICD-9-CM codes 278.00 and 278.02).
Definition of Variables
We used NIS variables to identify patient characteristics of age, sex, race, and insurance status. Information about race is omitted from 20% to 25% of records in any given year. Those with missing race information were grouped together into an “unknown” category.
We used the Charlson-Deyo comorbidity index to account for burden of comorbid disease.22 We examined rates of tracheostomy using ICD-9-CM codes 31.1, 31.2, 31.21, and 31.29, and defined prolonged MV as duration of MV > 96 h (ICD-9-CM code 96.72). We also identified plausible acute medical conditions associated with IMV using standard ICD-9-CM codes and used these conditions for adjustment in our multivariable model. The diseases studied were severe sepsis, COPD exacerbation, asthma exacerbation, congestive heart failure exacerbation, acute stroke, acute myocardial infarction, and cardiac arrest. We defined severe sepsis using ICD-9-CM codes per the scheme validated by Martin et al23 and used standard ICD-9-CM codes for the other conditions studied (specific codes provided in e-Table 1 (398.3KB, pdf) ). People who received IMV but who did not have any of the aforementioned conditions listed as diagnoses were classified as “other.”
We used the number of organs failing as a surrogate for severity of acute disease. We identified each organ failure using standard ICD-9-CM codes.23 Since the entire study population received IMV, people with respiratory failure and no other organs failing were classified as having “0” organ failure, those with one organ failing in addition to respiratory failure as “1” organ failure, and so on. We examined the NIS variable for admission source categorized as elective, urgent care, ED, trauma, and other.
Outcomes
Our primary outcome of interest was inhospital mortality, which is recorded as such in the NIS database. Secondary outcomes included rates of tracheostomy and prolonged MV, length of stay (LOS), and discharge disposition.
Statistical Analysis
We performed all statistical analyses using Stata/IC 11.0 (StataCorp LP). We used the strata and weights with appropriate survey commands to generate national estimates. We used the Pearson χ2 test and Student t test to compare categorical and continuous variables as appropriate for their distribution. Since LOS was not normally distributed, we used Wilcoxon rank-sum test for comparison and report results as medians and interquartile ranges (IQR). Statistical significance for all tests was defined as a P < .05
We constructed several multivariable models to elucidate the independent association of morbid obesity with inhospital mortality in people receiving IMV. We used single predictor, logistic regression analysis to identify putative risk factors associated with mortality in our primary model. We included all variables that were significantly associated with mortality in the bivariable analysis at P < .10 in our final multivariable model. We checked these variables for multicollinearity using tolerance and a variance inflation factor. For the variables used in the final model, both the tolerance and the variation inflation factor were very close to unity, indicating minimal collinearity. We examined all two-way interaction terms between variables and included those found significant in the model. For our primary model, we then performed sensitivity analysis by excluding race as a variable. We also used similar techniques to construct a multivariable model to determine the independent association of obesity with receipt of IMV.
We studied outcomes in two a priori defined subgroups stratified by source of admission and stratified by number of organs failing. We used logistic regression to determine the independent association of morbid obesity with mortality in these subgroups. We similarly used multivariable logistic regression analysis for our secondary end points.
Results
An estimated 4,070,419 morbidly obese people were hospitalized during the years 2004 to 2008 in the United States. Of these, 119,759 (2.9%) required IMV (Table 1, Fig 1), which was a significantly larger percentage than that of nonobese people requiring IMV (2.6%). On adjusted analysis, hospitalized, morbidly obese people had 1.37 times (95% CI, 1.20-1.57) higher odds of receiving IMV than nonobese people (e-Table 2 (398.3KB, pdf) ).
Table 1.
—Demographic Characteristics of Nonobese and Morbidly Obese Patients Undergoing IMV: 2004 to 2008
| Patient Characteristicsa | Nonobese | Morbidly Obese |
| Total admissions, No. | 152,638,750 | 4,070,419 |
| Undergoing MV, No. (%) | 4,039,583 (2.6) | 119,759 (2.9) |
| Age, mean ± SD | 63.0 ± 17.8 | 56.5 ± 13.3 |
| Age group | ||
| 18-34 y | 8.6 | 6.3 |
| 35-49 y | 13.7 | 22.7 |
| 50-64 y | 25.6 | 42.5 |
| ≥ 65 y | 52.1 | 28.5 |
| Sex | ||
| Female | 46.1 | 58.8 |
| Race | ||
| White | 52.8 | 53.8 |
| Black | 11.4 | 15.4 |
| Hispanic | 7.0 | 6.8 |
| Asian | 2.0 | 0.7 |
| Others | 2.8 | 2.7 |
| Unknown | 23.9 | 20.6 |
| Insurance | ||
| Medicare | 56.5 | 46.5 |
| Medicaid | 12 | 18.3 |
| Private | 21.6 | 27.4 |
| Self | 6.1 | 4.6 |
| Others | 3.8 | 3.1 |
| Hospital type/size | ||
| Teaching | 51.8 | 44.8 |
| Small | 9.2 | 10.5 |
| Medium | 23.6 | 23.9 |
| Large | 67.2 | 65.7 |
| Admission type | ||
| Elective | 9.5 | 14.6 |
| Urgent care | 13.5 | 13.6 |
| ED | 64.5 | 59 |
| Trauma | 1.3 | 0.4 |
| Others | 11.1 | 12.4 |
Data are given as % unless otherwise indicated. IMV = invasive mechanical ventilation; MV = mechanical ventilation.
P < .05 for all characteristics except Hispanic race and the race category “Others,” medium hospital size, and urgent care admission.
Figure 1.
Trends in admission and invasive mechanical ventilation in morbidly obese people.
Demographics
People with morbid obesity who were receiving IMV were significantly younger as compared with the nonobese cohort receiving IMV (mean age 56.5 years vs 63.0 years; P < .001). Significantly larger proportions of morbidly obese People were female and of black race. Among the morbidly obese, elective admissions were more frequent. Table 1 describes the demographic characteristics of both cohorts receiving IMV.
Clinical Characteristics
The burden of comorbid disease as defined by the Charlson-Deyo score was higher in nonobese people. Specifically, a larger proportion of nonobese people had scores ≥ 7. Conversely, more patients with morbid obesity had scores between 1 and 3 (Table 2). Severity of acute illness as indicated by number of organs failing was similarly higher in nonobese people. A larger proportion of people with three or more organs failing were nonobese as compared with the morbidly obese (Table 2).
Table 2.
—Clinical Characteristics of Nonobese and Morbidly Obese Patients Undergoing IMV: 2004 to 2008
| Patient Characteristicsa | Nonobese | Morbidly Obese |
| Charlson-Deyo comorbidity score | ||
| 0 | 27.5 | 16.9 |
| 1-3 | 58 | 71.9 |
| 4-6 | 9.8 | 9.3 |
| ≥ 7 | 4.7 | 1.8 |
| Charlson comorbidity index, mean | 1.83 | 1.80 |
| Organ failures other than respiratory, No. | ||
| 0 | 43.6 | 52 |
| 1 | 30.9 | 30 |
| 2 | 16 | 12.7 |
| 3 | 6.8 | 4.1 |
| 4 | 2.2 | 1.0 |
| 5 or 6 | 0.5 | 0.2 |
| ≥3 organ failures | 9.5 | 5.3 |
| Organ failure, mean | 0.72 | 0.95 |
| Type of organ failure | ||
| Cardiovascular | 24.6 | 16.4 |
| Renal | 25.9 | 23.8 |
| Hepatic | 4.1 | 1.9 |
| Metabolic | 14.6 | 14 |
| Neurologic | 14.5 | 11.1 |
| Hematologic | 10.9 | 5.5 |
| Reason for IMV | ||
| Severe sepsis | 30.5 | 19.5 |
| Pneumonia | 43 | 36.9 |
| COPD exacerbation | 9.4 | 14.9 |
| Asthma exacerbation | 5.3 | 14.2 |
| CHF exacerbation | 1.6 | 2.2 |
| Acute coronary syndrome | 11.1 | 7.5 |
| Cardiac arrest | 10.4 | 8.1 |
| Stroke | 7.7 | 3.6 |
Data given as % unless otherwise indicated. CHF = congestive heart failure. See Table 1 legend for expansion of other abbreviations.
P < .05 for all characteristics.
Outcomes
Mortality:
The unadjusted, all-cause, inhospital mortality in morbidly obese people receiving IMV was significantly lower in comparison with the nonobese cohort (19.5% vs 33%; P < .001) (Table 3). After multivariable adjustment for potential confounders, odds of mortality among the morbidly obese were no different than that for nonobese people (OR 0.89; 95% CI, 0.74-1.06) (Table 4). Our results did not change significantly even when we examined people placed on IMV within the first 48 h of admission to the hospital (data not shown). Similarly, our results were the same when we performed sensitivity analysis by excluding race from our regression model (e-Table 3 (398.3KB, pdf) ).
Table 3.
—Outcomes of IMV in Nonobese and Morbidly Obese Patients: 2004 to 2008
| Outcome | Nonobese | Morbidly Obese |
| All-cause, inhospital mortalitya | 33 | 19.5 |
| IMV > 96 h | 39.9 | 39.4 |
| Tracheostomy | 9.7 | 11.3 |
| Disposition of survivors | ||
| Home | 32.2 | 35.3 |
| Home care | 13.7 | 18.9 |
| Any facility | 44.3 | 36.3 |
| To short-term hospitals | 8.3 | 8.4 |
| Left AMA/unknown | 1.4 | 1.0 |
| LOS, median (IQR), d | ||
| LOS in survivors | 11 (6-20) | 10 (6-17) |
| Time to death | 6 (2-14) | 5 (2-12) |
Data given as % unless otherwise indicated. AMA = against medical advice; IQR = interquartile range; LOS = length of stay. See Table 1 for expansion of other abbreviation.
P < .05 for all except IMV > 96 h and disposition to any facility.
Table 4.
—Multivariate Analysis: Predictors of Mortality Among All Patients (Morbidly Obese and Nonobese)Undergoing IMV
| Predictor of Mortality | OR | 95% CI |
| Morbid obesity | 0.89 | 0.74-1.06 |
| Age group, y | ||
| 18-34 | Reference | … |
| 35-49 | 1.23 | 1.20-1.27 |
| 50-64 | 1.61 | 1.56-1.64 |
| ≥65 | 2.76 | 2.69-2.83 |
| Sex | ||
| Male | Reference | … |
| Female | 1.00 | 0.99-1.01 |
| Race | ||
| White | Reference | … |
| Black | 0.95 | 0.94-0.97 |
| Hispanic | 0.97 | 0.97-1.01 |
| Asian | 1.06 | 0.96-1.03 |
| Others | 0.98 | 0.96-1.02 |
| Unknown | 0.97 | 0.95-0.98 |
| Insurance | ||
| Medicare | Reference | … |
| Medicaid | 0.95 | 0.92-0.96 |
| Private | 0.94 | 0.92-0.95 |
| Self | 1.21 | 1.17-1.24 |
| Others | 0.93 | 0.90-0.95 |
| Hospital teaching status | ||
| Nonteaching | Reference | … |
| Teaching | 1.07 | 1.06-1.08 |
| Hospital size | ||
| Small | Reference | … |
| Medium | 0.99 | 0.97-1.00 |
| Large | 1.01 | 0.99-1.03 |
| Admission type | ||
| Elective admission | Reference | … |
| From urgent care | 1.40 | 1.37-1.43 |
| From ED | 1.40 | 1.37-1.42 |
| Trauma | 2.07 | 1.97-2.18 |
| Others | 1.40 | 1.37-1.43 |
| Charlson-Deyo comorbidity index | ||
| 0 | Reference | … |
| 1-3 | 1.35 | 1.32-1.37 |
| 4-6 | 1.81 | 1.78-1.85 |
| ≥ 7 | 3.41 | 3.32-3.49 |
| Organ failures, No. | ||
| 0 | Reference | … |
| 1 | 1.77 | 1.76-1.92 |
| 2 | 2.80 | 2.76-2.84 |
| 3 | 4.16 | 4.07-4.24 |
| 4 | 6.11 | 5.91-6.33 |
| 5 or 6 | 9.03 | 8.40-9.71 |
| Year | ||
| 2004 | Reference | … |
| 2005 | 0.93 | 0.91-0.94 |
| 2006 | 0.86 | 0.85-0.87 |
| 2007 | 0.74 | 0.73-0.76 |
| 2008 | 0.71 | 0.70-0.72 |
See Table 1 legend for expansion of abbreviation.
Among morbidly obese people, analysis of the predefined subgroups revealed that the risk for mortality relative to nonobese people was no different in admissions originating from the ED, urgent care, or trauma unit. However, this risk was lower for morbidly obese people who were admitted electively (Fig 2A). There was a stepwise increment in the risk for mortality relative to nonobese people with increasing number of organ failures in morbidly obese people (range: OR, 0.77; 95% CI, 0.58-1.01 for no organs failing, to OR, 4.14; 95% CI, 1.11-15.3 for four or more organs failing) (Fig 2B).
Figure 2.
Forest plot showing odds of mortality between morbidly obese patients undergoing mechanical ventilation when compared with nonobese people (reference). A, According to admission type. B, According to severity of illness (number of organ failures).
Prolonged MV and Tracheostomy:
The proportion of morbidly obese patients requiring prolonged MV was similar to nonobese patients (adjusted OR, 0.98; 95% CI, 0.78-1.23) (e-Table 4 (398.3KB, pdf) ). Conversely, the proportion receiving tracheostomy was significantly higher among the morbidly obese (9.7% vs 11.3%, P < .001; adjusted OR, 2.19; 95% CI ,1.77-2.69) (e-Table 5 (398.3KB, pdf) ).
LOS and Discharge Dispositions in Survivors:
The median LOS was shorter by approximately 1 day in morbidly obese survivors as compared with the nonobese survivors (P < .001). Among the morbidly obese cohort receiving IMV, discharges to skilled nursing facilities were lower, but discharges to home or home with home health care were higher as compared with the nonobese cohort (Table 3, e-Tables 6-8 (398.3KB, pdf) ).
Discussion
We show that hospital admissions for people who are morbidly obese increased numerically and proportionately over the time period of our study. The fraction of such people receiving IMV also increased. Though the risk of IMV relative to nonobese people was much higher in people with morbid obesity (OR, 1.37), the mortality after adjustment for potential confounding factors was remarkably similar. This is even more remarkable given the fact that morbidly obese people received tracheostomy more often, suggesting that a larger proportion, compared with nonobese people, was unable to be weaned from IMV.
Results from other studies examining outcomes of people with excess weight and critical illness have been pooled in three meta-analyses.5‐7 All three analyses included all obese patients and may not be comparable to our study because we restricted our attention to a distinct, morbidly obese cohort of patients receiving IMV. We judged that this approach would ensure comparison of a high-risk cohort of patients requiring ICU admission and would likely eliminate bias introduced by inclusion of overweight and obese people, thereby allowing us to detect differences in outcomes more robustly.
Hypothetically, morbidly obese patients may have worse outcomes due to limited cardiopulmonary reserve, reduced thoracoabdominal compliance leading to difficulties with IMV, and increased prevalence of comorbid conditions.24 Morbidly obese individuals might also receive some diagnostic tests such as CT scans less often than nonobese people, due to mechanical constraints.25 Further, there may be increased complications related to common procedures such as central-line placement due to factors intrinsic to morbid obesity. Therefore, our findings of similar risks for mortality in morbidly obese people and people who are not obese are counterintuitive. One plausible explanation is that morbidly obese people are somehow healthier and have lower severity of illness than their nonobese counterparts in ways we could not measure. Our premise is supported by our findings of significantly younger age, lower comorbidity scores, fewer organ failures, and a larger number of elective admissions among the morbidly obese cohort. Further, our observation that risk for mortality in morbidly obese people is significantly higher once severity of acute illness (as measured by number of organs failing) is sufficiently increased also lends credence to our hypothesis (OR, 4.14 for morbidly obese with four or more organs failing). Finally, a larger proportion of morbidly obese people, in comparison with nonobese people, returned home with or without home health care. Conversely, a lower proportion was discharged to skilled nursing facilities. This implies better functional recovery after critical illness and receipt of IMV, which may suggest lesser acuity of illness to begin with.
Disparities in care provided may have biased our results toward favorable survival in the morbidly obese cohort. Physicians may have a lower threshold to admit morbidly obese people, while opting for outpatient therapy with close clinical follow-up in the nonobese population. Secondary to their body habitus, obese patients have greater physical care requirements.26 They may, thus, inadvertently be triaged to higher standards of care. Moreover, in anticipation of difficulties with airway management, physicians may be more vigilant about physiologic deterioration and have lower thresholds for intubation in morbidly obese patients.24 Indeed, a recent investigation by O’Brien et al27 concluded that processes of care affect inferences about outcomes in critically ill obese adults and should be considered when making such inferences.
Our study is best compared with that by Anzueto et al,13 who studied a cohort of 4,698 patients on MV and found that 4.3% were morbidly obese. Morbidly obese people were more likely to develop ARDS and acute kidney injury, but outcomes were no different based on BMI. The mortality of nonobese patients in their study was 32%. We arrived at remarkably similar conclusions in a more contemporary time frame, except that only 2.8% of our ventilated cohort was morbidly obese and we did not examine risks of ARDS and acute kidney injury. Differences in the proportion of morbidly obese people receiving MV arise from the fact that while Anzueto et al13 examined patients receiving both IMV and NIV, we restricted our attention to IMV only.
Despite the use of a well-characterized national database, our study has important limitations. First, from our analysis of an administrative database we were unable to identify several processes of care that affect outcomes in IMV. Such processes include, but are not limited to, spontaneous breathing trials, interruption of sedative medications, use of low tidal-volume ventilation, and use of prophylaxis against thromboembolism and stress ulcers. Disparities in adherence to these accepted practices may have accounted for some of our observations and biased our results toward improved outcomes in the obese cohort. For example, one observational study found that obese patients were more likely to receive prophylaxis for thromboembolism.28 Second, our classifications of patients were made on the basis of ICD-9-CM codes and not actual height and weight data. We, therefore, cannot rule out inconsistencies and inaccuracies in coding practices that could have led to potential misclassifications. Further, even if coded accurately, we cannot discount inaccuracies in measuring BMI. For example, fluid balance in the ICU is one factor known to confound measurements.27 Third, we did not have any information on abdominal or truncal obesity, which may have a greater impact on outcomes than BMI itself, as demonstrated by a recent, large, population-based study.29 Fourth, inclusion of underweight and cachectic patients in our nonobese category may have biased our results toward finding no difference in outcomes. Indeed several studies have now demonstrated poor outcomes for underweight patients.30 Fifth, though we tried to reduce selection bias by including people with a clear indication for ICU admission (IMV) and rigorously adjusted for confounders, we cannot exclude residual confounding by unmeasured factors. Specifically, we did not have information about physiologic data such as vital signs, laboratory values, or radiographic studies, and were unable to control for these variables. Finally, since NIS does not have variables for processes of care such as reintubation rates, receipt of IMV for chronic respiratory failure, and length of MV, we were unable to use these as relevant outcome measures.
Conclusions
Despite these limitations, our study demonstrates that adjusted outcomes of morbidly obese people receiving IMV are at least similar to their nonobese counterparts. In a large cohort of patients, this is partly explained by selection bias, wherein hospitalized obese patients receiving IMV are probably healthier at baseline and have lesser severity of acute illness than nonobese patients. Our findings also have future research implications. Studies focusing on outcomes of critically ill morbidly obese patients should refine criteria for inclusion and direct attention toward confounding factors to determine whether true associations exist between obesity and outcomes.
Supplementary Material
Online Supplement
Acknowledgments
Author contributions: Dr Nanchal had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Dr Kumar: contributed to study design, statistical analysis, and writing the manuscript, and served as principal author.
Dr Majumdar: contributed to critical review and revision of manuscript.
Dr Jacobs: contributed to critical review and revision of manuscript.
Ms Danesh: contributed to critical review and revision of manuscript.
Dr Dagar: contributed to critical review and revision of manuscript.
Dr Deshmukh: contributed to critical review and revision of manuscript.
Dr Taneja: contributed to critical review and revision of manuscript.
Dr Nanchal: contributed to study design, statistical analysis, and writing the manuscript.
Financial/nonfinancial disclosures: The authors have reported to CHEST that no potential conflicts of interest exist with any companies/organizations whose products or services may be discussed in this article.
Additional information: The e-Tables can be found in the “Supplemental Materials” area of the online article.
Abbreviations
- ICD-9-CM
International Classification of Diseases, 9th Revision, Clinical Modification
- IMV
invasive mechanical ventilation
- LOS
length of stay
- MV
mechanical ventilation
- NIS
Nationwide Inpatient Sample
- NIV
noninvasive ventilation
Footnotes
Funding/Support: The authors have reported to CHEST that no funding was received for this study.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians. See online for more details.
References
- 1.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999-2008. JAMA. 2010;303(3):235-241. [DOI] [PubMed] [Google Scholar]
- 2.Ray DE, Matchett SC, Baker K, Wasser T, Young MJ. The effect of body mass index on patient outcomes in a medical ICU. Chest. 2005;127(6):2125-2131. [DOI] [PubMed] [Google Scholar]
- 3.Bercault N, Boulain T, Kuteifan K, Wolf M, Runge I, Fleury JC. Obesity-related excess mortality rate in an adult intensive care unit: a risk-adjusted matched cohort study. Crit Care Med. 2004;32(4):998-1003. [DOI] [PubMed] [Google Scholar]
- 4.Yaegashi M, Jean R, Zuriqat M, Noack S, Homel P. Outcome of morbid obesity in the intensive care unit. J Intensive Care Med. 2005;20(3):147-154. [DOI] [PubMed] [Google Scholar]
- 5.Akinnusi ME, Pineda LA, El Solh AA. Effect of obesity on intensive care morbidity and mortality: a meta-analysis. Crit Care Med. 2008;36(1):151-158. [DOI] [PubMed] [Google Scholar]
- 6.Hogue CW, Jr, Stearns JD, Colantuoni E, et al. The impact of obesity on outcomes after critical illness: a meta-analysis. Intensive Care Med. 2009;35(7):1152-1170. [DOI] [PubMed] [Google Scholar]
- 7.Oliveros H, Villamor E. Obesity and mortality in critically ill adults: a systematic review and meta-analysis. Obesity (Silver Spring). 2008;16(3):515-521. [DOI] [PubMed] [Google Scholar]
- 8.Duarte AG, Justino E, Bigler T, Grady J. Outcomes of morbidly obese patients requiring mechanical ventilation for acute respiratory failure. Crit Care Med. 2007;35(3):732-737. [DOI] [PubMed] [Google Scholar]
- 9.Martino JL, Stapleton RD, Wang M, et al. Extreme obesity and outcomes in critically ill patients. Chest. 2011;140(5):1198-1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Frat JP, Gissot V, Ragot S, et al. ; Association des Réanimateurs du Centre-Ouest (ARCO) study group. Impact of obesity in mechanically ventilated patients: a prospective study. Intensive Care Med. 2008;34(11):1991-1998. [DOI] [PubMed] [Google Scholar]
- 11.Salome CM, King GG, Berend N. Physiology of obesity and effects on lung function. J Appl Physiol. 2010;108(1):206-211. [DOI] [PubMed] [Google Scholar]
- 12.Morris AE, Stapleton RD, Rubenfeld GD, Hudson LD, Caldwell E, Steinberg KP. The association between body mass index and clinical outcomes in acute lung injury. Chest. 2007;131(2):342-348. [DOI] [PubMed] [Google Scholar]
- 13.Anzueto A, Frutos-Vivar F, Esteban A, et al. ; Ventila group. Influence of body mass index on outcome of the mechanically ventilated patients. Thorax. 2011;66(1):66-73. [DOI] [PubMed] [Google Scholar]
- 14.Gong MN, Bajwa EK, Thompson BT, Christiani DC. Body mass index is associated with the development of acute respiratory distress syndrome. Thorax. 2010;65(1):44-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pelosi P, Croci M, Ravagnan I, et al. The effects of body mass on lung volumes, respiratory mechanics, and gas exchange during general anesthesia. Anesth Analg. 1998;87(3):654-660. [DOI] [PubMed] [Google Scholar]
- 16.Kress JP, Pohlman AS, Alverdy J, Hall JB. The impact of morbid obesity on oxygen cost of breathing (VO(2RESP)) at rest. Am J Respir Crit Care Med. 1999;160(3):883-886. [DOI] [PubMed] [Google Scholar]
- 17.Wang Y, Beydoun MA, Liang L, Caballero B, Kumanyika SK. Will all Americans become overweight or obese? Estimating the progression and cost of the US obesity epidemic. Obesity (Silver Spring). 2008;16(10):2323-2330. [DOI] [PubMed] [Google Scholar]
- 18.Healthcare Cost and Utilization Project. Introduction to the HCUP Nationwide Inpatient Sample (NIS) 2008. Healthcare Cost and Utilization Project website. http://www.hcup-us.ahrq.gov/db/nation/nis/NIS_Introduction_2008.jsp. Accessed October 26, 2011.
- 19.Quan H, Parsons GA, Ghali WA. Validity of procedure codes in International Classification of Diseases, 9th revision, clinical modification administrative data. Med Care. 2004;42(8):801-809. [DOI] [PubMed] [Google Scholar]
- 20.Hutter MM, Randall S, Khuri SF, et al. Laparoscopic versus open gastric bypass for morbid obesity: a multicenter, prospective, risk-adjusted analysis from the National Surgical Quality Improvement Program. Ann Surg. 2006;243(5):657-662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Memtsoudis SG, Bombardieri AM, Ma Y, Walz JM, Chiu YL, Mazumdar M. Mortality of patients with respiratory insufficiency and adult respiratory distress syndrome after surgery: the obesity paradox. J Intensive Care Med. 2012;27(5):306-311. [DOI] [PubMed] [Google Scholar]
- 22.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613-619. [DOI] [PubMed] [Google Scholar]
- 23.Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348(16):1546-1554. [DOI] [PubMed] [Google Scholar]
- 24.Lewandowski K, Lewandowski M. Intensive care in the obese. Best Pract Res Clin Anaesthesiol. 2011;25(1):95-108. [DOI] [PubMed] [Google Scholar]
- 25.Baskerville JR, Moore RK. Morbidly obese patients receive delayed ED care: body mass index greater than 40 kg/m2 have longer disposition times. Am J Emerg Med. 2012;30(5):737-740. [DOI] [PubMed] [Google Scholar]
- 26.Choi JC, Bakaeen FG, Cornwell LD, et al. Morbid obesity is associated with increased resource utilization in coronary artery bypass grafting. Ann Thorac Surg. 2012;94(1):23-28. [DOI] [PubMed] [Google Scholar]
- 27.O’Brien JM, Jr, Philips GS, Ali NA, Aberegg SK, Marsh CB, Lemeshow S. The association between body mass index, processes of care, and outcomes from mechanical ventilation: a prospective cohort study. Crit Care Med. 2012;40(5):1456-1463. [DOI] [PubMed] [Google Scholar]
- 28.O’Brien JM, Jr, Phillips GS, Ali NA, Lucarelli M, Marsh CB, Lemeshow S. Body mass index is independently associated with hospital mortality in mechanically ventilated adults with acute lung injury. Crit Care Med. 2006;34(3):738-744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Paolini JB, Mancini J, Genestal M, et al. Predictive value of abdominal obesity vs. body mass index for determining risk of intensive care unit mortality. Crit Care Med. 2010;38(5):1308-1314. [DOI] [PubMed] [Google Scholar]
- 30.Adams KF, Schatzkin A, Harris TB, et al. Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. N Engl J Med. 2006;355(8):763-778. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Online Supplement