Abstract
Background:
Little is known about the population-based burden of ED care for COPD.
Methods:
We analyzed statewide ED surveillance system data to quantify the frequency of COPD-related ED visits, hospital admissions, and comorbidities.
Results:
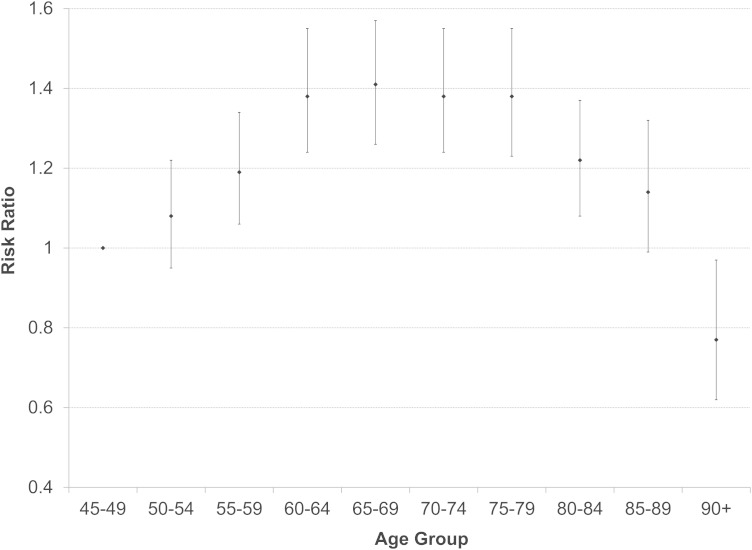
In 2008 to 2009 in North Carolina, 97,511 COPD-related ED visits were made by adults ≥ 45 years of age, at an annual rate of 13.8 ED visits/1,000 person-years. Among patients with COPD (n = 33,799), 7% and 28% had a COPD-related return ED visit within a 30- and 365-day period of their index visit, respectively. Compared with patients on private insurance, Medicare, Medicaid, and noninsured patients were more likely to have a COPD-related return visit within 30 and 365 days and have three or more COPD-related visits within 365 days. There were no differences in return visits by sex. Fifty-one percent of patients with COPD were admitted to the hospital from the index ED visit. Subsequent hospital admission risk in the cohort increased with age, peaking at 65 to 69 years (risk ratio [RR], 1.41; 95% CI, 1.26-1.57); there was no difference by sex. Patients with congestive heart failure (RR, 1.29; 95% CI, 1.22-1.37), substance-related disorders (RR, 1.35; 95% CI, 1.13-1.60), or respiratory failure/supplemental oxygen (RR, 1.25; 95% CI, 1.19-1.31) were more likely to have a subsequent hospital admission compared with patients without these comorbidities.
Conclusions:
The population-based burden of COPD-related care in the ED is significant. Further research is needed to understand variations in COPD-related ED visits and hospital admissions.
COPD is common and costly.1‐3 Nationally, the > 10 million adults with physician-diagnosed COPD had an estimated 1.5 million ED visits and 726,000 hospitalizations in 2000.1 The Centers for Disease Control and Prevention has called for increased analysis and dissemination of COPD-related public health data.4 We addressed this information gap by characterizing patterns in health-care use in COPD using a comprehensive population-based framework.
Materials and Methods
Data Sources
Statewide ED visit data from January 1, 2008, through December 31, 2009, were obtained from the North Carolina Public Health Data Group and the North Carolina Disease Event Tracking and Epidemiologic Collection Tool (NC DETECT) surveillance system. Through legislative mandate, all North Carolina acute care, hospital-affiliated civilian EDs that are open 24/7 in North Carolina are required to provide data on all ED visits to the NC DETECT surveillance system at least daily. Hospitals perform their own medical coding for administrative purposes then securely transmit electronic data streams to a data aggregator using standardized health record data formats. Data are monitored regularly, and data quality issues are communicated back to hospitals for resolution. Some 99.5% of all ED visits in North Carolina were captured from 110 out of 112 (98%) eligible hospitals in 2008 and from 111 out of 114 (97%) hospitals in 2009.5,6 Age- and sex-stratified population denominators for the population ≥ 45 years of age were derived from midyear population estimates for each study year.7 Institutional review board (IRB) approval (University of North Carolina IRB #10-1423) and a data use agreement were obtained from the University of North Carolina IRB and the North Carolina Division of Public Health, respectively.
Study Design and Cohort Definition
We described the frequency and rates of COPD-related ED visits and applied a population-based retrospective cohort design. We identified all patients ≥ 45 years of age who had at least one COPD-related ED visit between January 1, 2008, and December 31, 2008. We defined COPD-related ED visits as those in which the first or second discharge diagnosis positions contained one of the following International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes: 491.xx (chronic bronchitis), 492.xx (emphysema), 493.2x (chronic obstructive asthma), 494.xx (bronchiectasis), or 496.xx (chronic airway obstruction, not elsewhere classified). We chose not to include 490.xx (bronchitis, not specified as acute or chronic) to reduce possible inclusion of patients without diagnosed COPD.8
As a sensitivity analysis, we considered the following: (1) a broader COPD definition that adds two ICD-9-CM codes: 490.xx (bronchitis, not specified as acute or chronic) and 495.xx (extrinsic allergic alveolitis) and removes 493.2 (chronic obstructive asthma);9,10 and (2) a narrower COPD definition with the first discharge diagnosis position only (e-Table 1 (727.2KB, pdf) ). With the broader definition, there were more visits in the younger age groups (45-49 years and 50-54 years), less Medicaid payment, and fewer ED discharges to the hospital. With the narrower definition, we found similar distributions with our COPD definition for age group, sex, ED disposition, and payment method. The most common diagnosis groups in the first position, when COPD was in the second diagnostic position, were “other lower respiratory disease,” pneumonia, and “respiratory failure; insufficiency; arrest” (e-Table 2 (727.2KB, pdf) ). These findings support our definition, with COPD in either the first or second discharge diagnosis position.
The index visit was defined as the first COPD-related ED visit made by the patient to a given facility during calendar year 2008. ED patients (n = 2,264) were excluded from the cohort if they had an index visit disposition of “died” (n = 113), “unknown/missing” (n = 2,117), or “other” (n = 34).
Measures of COPD Care in the ED: Return Visits and Hospital Admissions
We calculated the number and proportion of patients with the following: (1) a subsequent COPD-related ED visit (a “return” visit) to the same facility within 30 days, (2) a return visit within 365 days of the index visit, and (3) three or more COPD-related ED visits within 365 days of their index visit. Most of the patients either had the index visit alone or had two visits (ie, the index visit plus one subsequent visit) in 365 days. Only 11.7% of patients had three or more visits, and just 5.8% had four or more visits. Thus, the number of patients with three or more COPD-related ED visits was already small, and further subdividing this group would not provide meaningful analyses (e-Table 3 (727.2KB, pdf) ). Last, we computed the likelihood of having a hospital admission from the ED at a subsequent ED visit. The likelihoods and related risk ratios (RRs) were computed using log-binomial regression.
Comorbidities
For each cohort member, we created a set of comorbidity indicators based on ICD-9-CM diagnosis codes present in any of the 11 diagnosis positions at the index visit. To group individual ICD-9-CM codes into clinically informative diagnosis groups, we used a modified version of the Clinical Classification Software (CCS),11 which has been validated with ED data.12 To focus on certain disease groups or comorbid conditions of interest, we modified the CCS a priori by combining some related CCS groups and subsetting others. The full list of comorbid condition groups used in the study, and their corresponding CCS group numbers, may be found in e-Table 4 (727.2KB, pdf) . For example, the CCS “respiratory failure/supplemental oxygen/shortness of breath” classification in e-Table 4 (727.2KB, pdf) includes six CCS groups and encompasses ICD-9-CM diagnosis codes for respiratory failure, shortness of breath, supplemental oxygen, and respiratory distress/insufficiency, as well as some other respiratory symptoms and illnesses (see e-Table 4 (727.2KB, pdf) for details). This group is distinct from other CCS groups involving respiratory conditions, such as the CCS groups for pneumonia, upper respiratory infection, asthma, or bronchitis. To quantify the association of tobacco smoking and COPD-related ED visits, we also created a group “Tobacco use” that includes only ICD-9-CM codes 305.1x and V15.82 and is a subset of CCS group 663 (“Screening and history of mental health disease and substance abuse codes”). “Substance-related disorders” includes drug-induced mental disorders and both dependent and nondependent abuse of drugs such as marijuana, cocaine, and opioids.
Statistical Analysis
We calculated the frequency and proportion of COPD-related ED visits by age, sex, payment method, discharge disposition, and comorbidities. Medicare is federal public medical insurance for those ≥ 65 years of age; Medicaid targets low-income individuals, families, and disabled individuals of all ages. Simple annual visit rates by age and sex were computed with state-level Census population denominators. Using the “GENMOD” procedure in SAS version 9.2 (used to run generalized linear models), we estimated crude and adjustedRRs and 95% CIs with log-binomial regression models. Models were checked for convergence and goodness of fit.
Results
Demographic Characteristics of COPD-Related ED Visits
In North Carolina in 2008 to 2009, 97,511 COPD-related ED visits were made by adults aged ≥ 45 years. The incidence rate was 13.78 ED visits/1,000 person-years (Table 1). The highest numbers of visits were found in the 65 to 69 years (14,001 or 14.4%) and 60 to 64 years (13,413 or 13.8%) age groups. Incidence rates were highest among the older age groups 75 to 79, 80 to 84, and 85 to 89 years. Women made more visits than men. Both the number of visits and incidence rates were higher among younger women (45-64 years) compared with younger men (e-Table 5 (727.2KB, pdf) ). At older ages (≥ 75 years), the number of visits was still higher among women, but incidence rates were higher among men (e-Table 5 (727.2KB, pdf) ). Payment method varied by age, with higher rates of noninsured (self-pay) and private insurance among the younger age group (45-64 years). Medicare payment was used by 80.5% of those aged ≥ 65 years (e-Table 6 (727.2KB, pdf) ).
Table 1.
—Characteristics of COPD-Related ED Visits by Patients ≥ 45 Years Old in North Carolina, 2008-2009
| Population Characteristic | COPD Visitsa 2008-2009, No. (%) | Population Denominator, 2008-2009b | Simple Annual Rate (per 1,000 person-y)c | COPD Cohortd 2008-2009, No. (%) |
| Age, y | ||||
| 45-49 | 8,650 (8.9) | 1,383,457 | 6.25 | 2,920 (8.6) |
| 50-54 | 11,153 (11.4) | 1,274,170 | 8.75 | 3,647 (10.8) |
| 55-59 | 11,776 (12.1) | 1,120,570 | 10.51 | 3,985 (11.8) |
| 60-64 | 13,413 (13.8) | 955,150 | 14.04 | 4,510 (13.3) |
| 65-69 | 14,001 (14.4) | 722,638 | 19.37 | 4,684 (13.9) |
| 70-74 | 12,488 (12.8) | 562,630 | 22.20 | 4,403 (13.0) |
| 75-79 | 11,107 (11.4) | 438,742 | 25.32 | 4,000 (11.9) |
| 80-84 | 8,284 (8.5) | 325,473 | 25.45 | 3,090 (9.1) |
| 85-89 | 4,727 (4.9) | 191,348 | 24.70 | 1,766 (5.2) |
| 90+ | 1,912 (2.0) | 103,303 | 18.51 | 794 (2.3) |
| Sex | ||||
| Female | 54,053 (55.4) | 3,815,603 | 14.17 | 18,797 (55.6) |
| Male | 43,447 (44.6) | 3,261,878 | 13.32 | 14,993 (44.4)e |
| Unknown/missing | 11 (0.0) | NA | … | … |
| Payment method | ||||
| Noninsured | ||||
| Self-pay (no insurance) | 8,465 (8.7) | … | … | 2,919 (8.6) |
| Insured | ||||
| Private insurance | 13,810 (14.2) | … | … | 5,283 (15.6) |
| Medicare | 57,396 (58.9) | … | … | 19,879 (58.8) |
| Medicaid | 10,499 (10.8) | … | … | 3,127 (9.3) |
| Other government payments/workers’ compensation | 1,039 (1.1) | … | … | 410 (1.2) |
| Other/unknown/missing | 6,302 (6.5) | … | … | 2,181 (6.5) |
| ED dispositionf | ||||
| Discharged to home or self-care | 43,262 (44.4) | … | … | 15,096 (44.7) |
| Admitted to a hospital department | 45,146 (46.3) | … | … | 17,302 (51.2) |
| Left without treatment or against medical advice | 756 (0.8) | … | … | 246 (0.7) |
| Transferred to another location for additional careg | 2,208 (2.3) | … | … | 824 (2.4) |
| Placed in observation (not admitted) | 863 (0.9) | … | … | 331 (1.0) |
| Died | 270 (0.3) | … | … | NA |
| Other | 211 (0.2) | … | … | NA |
| Unknown/missing | 4,795 (4.9) | … | … | NA |
| Total | 97,511 | 7,077,481 | 13.78 | 33,799 |
ICD-9-CM = International Classification of Diseases, Ninth Revision, Clinical Modification; NA = not applicable.
ED visits associated with COPD are defined as having an ICD-9-CM codes 491.xx, 492.xx, 493.2, 494.xx, or 496.xx as the first or second diagnosis.
Combined 2008 and 2009 midyear population estimates for the North Carolina population aged ≥ 45 y.
Simple annual rate is an unadjusted rate, calculated from total number of visits in 2008 to 2009 divided by North Carolina population ≥ 45 y old 2008 to 2009.
COPD patient cohort, N = 33,799.
Suppressed due to cell size < 10.
Disposition values presented in the last column refer only to the cohort members’ index visits. The NA that is listed for ED dispositions of “Died,” “Other,” and “Unknown/missing” are exclusions for cohort memberships.
Transfer locations include “another short-term general hospital,” ”skilled nursing facility,” “intermediate care facility,” “another type of institution,” “home, under care of a home IV drug therapy provider,” and “home, under care of certified home care provider/program.”
COPD Patient Cohort and Return ED Visits
The COPD patient cohort (n = 33,799) had a similar distribution of age and sex compared with the visit-based description (Table 1). Within this cohort, 7% and 28%, respectively, had a COPD-related ED return visit within a 30-day and 365-day period; 12% had three or more COPD-related visits within 365 days of their index visit (Table 2). Patients ≥ 80 years of age were less likely to have one or more return visits within 365 days. Patients ≥ 90 years of age were less likely to have a return visit within 30 days. There were no differences among women and men in frequency of return visits. Compared with patients on private insurance, patients with Medicare or Medicaid, the noninsured, or those whose payment method was unknown were more likely to have the following: (1) a COPD-related return visit within 30 or 365 days, and (2) three or more COPD-related visits within 365 days (RRs all statistically significant).
Table 2.
—Risk for COPD-Related ED Visits Within 30 and 365 d, and Hospital Admissions for COPD Patient Cohort (N = 33,799) by Demographic Variables
| Had First Subsequent COPD-Related ED Visit Within | Had ≥ 3 COPD-Related ED Visits (Including Index Visit) Within 365 d | ≥ 1 Subsequent COPD-Related ED Visits Within 365 d That Resulted in Hospital Admissions | |||||||
| 30 d | 365 d | ||||||||
| Patient characteristic | Patient With Index Visit in 2008, No.a | No. (%) | RR (95% CI) | No. (%) | RR (95% CI) | No. (%) | RR (95% CI) | No. (%) | RR (95% CI) |
| Age at index visit, y | |||||||||
| 45-49 | 2,920 | 193 (6.6) | REF | 845 (28.9) | REF | 362 (12.4) | REF | 390 (13.4) | REF |
| 50-54 | 3,647 | 259 (7.1) | 1.07 (0.90-1.29) | 1,056 (29.0) | 1.00 (0.93-1.08) | 462 (12.7) | 1.02 (0.90-1.16) | 525 (14.4) | 1.08 (0.95-1.22) |
| 55-59 | 3,985 | 275 (6.9) | 1.04 (0.87-1.25) | 1,113 (27.9) | 0.97 (0.89-1.04) | 514 (12.9) | 1.04 (0.92-1.18) | 635 (15.9) | 1.19 (1.06-1.34) |
| 60-64 | 4,510 | 348 (7.7) | 1.17 (0.99-1.38) | 1,339 (29.7) | 1.03 (0.95-1.10) | 592 (13.1) | 1.06 (0.94-1.20) | 833 (18.5) | 1.38 (1.24-1.55) |
| 65-69 | 4,684 | 338 (7.2) | 1.09 (0.92-1.29) | 1,383 (29.5) | 1.02 (0.95-1.10) | 616 (13.2) | 1.06 (0.94-1.20) | 879 (18.8) | 1.41 (1.26-1.57) |
| 70-74 | 4,403 | 338 (7.7) | 1.16 (0.98-1.38) | 1,300 (29.5) | 1.02 (0.95-1.10) | 517 (11.7) | 0.95 (0.84-1.07) | 814 (18.5) | 1.38 (1.24-1.55) |
| 75-79 | 4,000 | 285 (7.1) | 1.08 (0.90-1.29) | 1,143 (28.6) | 0.99 (0.92-1.06) | 446 (11.2) | 0.90 (0.79-1.02) | 738 (18.5) | 1.38 (1.23-1.55) |
| 80-84 | 3,090 | 219 (7.1) | 1.07 (0.89-1.29) | 778 (25.2) | 0.87 (0.80-0.95) | 280 (9.1) | 0.73 (0.63-0.85) | 502 (16.3) | 1.22 (1.08-1.37) |
| 85-89 | 1,766 | 99 (5.6) | 0.85 (0.67-1.07) | 393 (22.3) | 0.77 (0.69-0.85) | 128 (7.2) | 0.58 (0.48-0.71) | 270 (15.3) | 1.14 (0.99-1.32) |
| 90+ | 794 | 36 (4.5) | 0.69 (0.48-0.97) | 137 (17.3) | 0.60 (0.51-0.70) | 36 (4.5) | 0.37 (0.26-0.51) | 82 (10.3) | 0.77 (0.62-0.97) |
| Sex | |||||||||
| Female | 18,797 | 1,287 (6.8) | REF | 5,296 (28.2) | REF | 2,165 (11.5) | REF | 3,163 (16.8) | REF |
| Male | 14,993 | 1,102 (7.4) | 1.07 (0.99-1.16) | 4,190 (27.9) | 0.99 (0.96-1.03) | 1,787 (11.9) | 1.03 (0.98-1.10) | 2,504 (16.7) | 0.99 (0.95-1.04) |
| Missing | 9b | 1 (11.1) | … | 1 (11.1) | … | 1 (11.1) | … | 1 (11.1) | … |
| Payment method at index visit | |||||||||
| Noninsured | |||||||||
| Self-pay (no insurance) | 2,919 | 193 (6.6) | 1.24 (1.04-1.48) | 731 (25.0) | 1.09 (1.01-1.18) | 327 (11.2) | 1.27 (1.11-1.45) | 293 (10.0) | 0.72 (0.63-0.82) |
| Insured | |||||||||
| Private insurance | 5,283 | 282 (5.3) | REF | 1,211 (22.9) | REF | 466 (8.8) | REF | 737 (14.0) | REF |
| Medicare | 19,879 | 1,453 (7.3) | 1.37 (1.21-1.55) | 5,688 (28.6) | 1.25 (1.18-1.32) | 2,308 (11.6) | 1.32 (1.20-1.45) | 3,583 (18.0) | 1.29 (1.20-1.39) |
| Medicaid | 3,127 | 271 (8.7) | 1.62 (1.38-1.91) | 1,076 (34.4) | 1.50 (1.40-1.61) | 502 (16.1) | 1.82 (1.62-2.05) | 589 (18.8) | 1.35 (1.22-1.49) |
| Other government payments/workers compensation | 410 | 25 (6.1) | 1.14 (0.77-1.70) | 88 (21.5) | 0.94 (0.77-1.13) | 32 (7.8) | 0.88 (0.63-1.25) | 51 (12.4) | 0.89 (0.68-1.16) |
| Other/unknown/missing | 2,181 | 166 (7.6) | 1.43 (1.18-1.72) | 693 (31.8) | 1.39 (1.28-1.50) | 318 (14.6) | 1.65 (1.45-1.89) | 415 (19) | 1.36 (1.22-1.52) |
| ED disposition at index visit | |||||||||
| Discharged to home or self-care | 15,096 | 1,306 (8.7) | REF | 4,474 (29.6) | REF | 1,895 (12.6) | REF | 2,079 (13.8) | REF |
| Admitted to a hospital department | 17,302 | 1,003 (5.8) | 0.67 (0.62-0.73) | 4,666 (27.0) | 0.91 (0.88-0.94) | 1,920 (11.1) | 0.88 (0.83-0.94) | 3,411 (19.7) | 1.43 (1.36-1.50) |
| Left without treatment or against medical advice | 246 | 17 (6.9) | 0.80 (0.51-1.27) | 63 (25.6) | 0.86 (0.70-1.07) | 26 (10.6) | 0.84 (0.58-1.21) | 23 (9.4) | 0.68 (0.46-1.00) |
| Transferred to another location for additional carec | 824 | 47 (5.7) | 0.66 (0.50-0.87) | 187 (22.7) | 0.77 (0.67-0.87) | 75 (9.1) | 0.73 (0.58-0.90) | 99 (12) | 0.87 (0.72-1.05) |
| Placed in observation (not admitted) | 331 | 17 (5.1) | 0.59 (0.37-0.95) | 97 (29.3) | 0.99 (0.84-1.17) | 37 (11.2) | 0.89 (0.66-1.21) | 56 (16.9) | 1.23 (0.96-1.56) |
| Total | 33,799 | 2,390 (7.1) | … | 9,487 (28.1) | … | 3,953 (11.7) | … | 5,668 (16.8) | … |
Proportion of patients who had subsequent COPD-related ED visits to the same facility within 30 and 365 d or were admitted to a hospital department directly from the ED among those who had a COPD-related ED visit in 2008, by patient characteristics. Statistically significant associations are bolded. REF = reference; RR = risk ratio.
Excluding 2,264 patients whose ED discharge disposition at the index visit was “died” (n = 131), “unknown/missing” (2,117), or “other” (n = 34).
Cell size suppressed, since < 10.
Transfer locations include: “another short-term general hospital,” “skilled nursing facility,” “intermediate care facility,” “another type of institution,” “home, under care of a home IV drug therapy provider,” and “home, under care of certified home care provider/program.”
Index Hospital Admissions
Fifty-one percent of the COPD patient cohort was admitted to the hospital from the ED at their index visit. Compared with patients discharged to home at their index visit, patients admitted to the hospital were statistically significantly less likely to have a subsequent ED visit in a 30- or 365-day period or to have three or more ED visits within 365 days (Table 2). However, patients admitted to the hospital directly from the ED at their index visit were at increased risk (RR, 1.43; 95% CI, 1.36-1.5) to have a subsequent hospital admission within 365 days of their index visit, compared with those who were discharged to home at their index visit (Table 2).
Subsequent Hospital Admissions
Within the patient cohort, 16.8% had one or more subsequent COPD-related ED visits that resulted in hospital admission within 365 days of the index visit. The RR of having a subsequent hospital admission increased with age from 45 to 60 years, plateaued from 60 to 79 years with a statistically significant increase risk (RR range from 1.38-1.41) compared with those 45 to 49 years, then decreased for those aged ≥ 80 years and older (Fig 1). No differences in subsequent hospital admissions were found by sex. Patients enrolled in Medicare and Medicaid were 29% and 35% more likely, respectively, to have one or more subsequent hospital admissions compared with those with private insurance. Patients with no insurance were 28% less likely than the privately insured to have a subsequent hospital admissions.
Figure 1.
Cohort risk of COPD hospital admission, by age.
Comorbidity Analysis and Return Visits
The five most common comorbidities among the cohort were hypertension (42%), respiratory failure/supplemental oxygen/shortness of breath (37%), heart disease (30%), tobacco use (29%), diabetes (29%), and congestive heart failure (21%) (Table 2). Patients with COPD with a respiratory failure/supplemental oxygen/shortness of breath comorbidity were at statistically significant increased risk of a subsequent COPD-related ED return visit within 30 days and 365 days as well as three or more COPD-related visits within 365 days, compared with those without this comorbidity. Those with diabetes and congestive heart failure comorbidities were also at increased risk of one or more subsequent COPD-related ED visits within 365 days. Those with pneumonia comorbidity were less likely to have a return visit in 30 days or three or more return visits within 365 days.
Subsequent Hospital Admissions:
There were substantial differences in subsequent hospital admission risk among those with and without comorbidities. Nine of the 15 comorbidities were significantly associated with increased risk of subsequent hospital admissions within 365 days (RRs ranging from 1.11 to 1.35) (Table 3). Compared with those without these comorbidities, patients with congestive heart failure or substance-related disorders had the highest RRs for subsequent hospital admissions, followed by respiratory failure/supplemental oxygen/shortness of breath and cardiac dysrhythmias/cardiac arrest/ventricular fibrillation CCS comorbidities. In contrast, patients with comorbidities of upper respiratory infection or COPD “other” (bronchitis unspecified acute/chronic, ICD-9-CM 490.x) were statistically significantly less likely to have one or more hospital admissions within 365 days of the index visit. Patients with COPD with recorded tobacco use at the index visit were not at statistically significant higher risk of having one or more subsequent hospital admissions.
Table 3.
—Risks for COPD-Related ED Visits Within 30 or 365 d, and Hospital Admissions for COPD Patient Cohort (N = 33,799), by Comorbidities Present at Index Visit Compared With Those Without the Comorbidity
| Subsequent COPD-Related Visit Within 30 d | Subsequent COPD-Related Visit Within 365 d | ≥ 3 COPD-Related Visits Within 365 d (Including Index Visit) | ≥ 1 Subsequent COPD-Related ED Visits That Resulted in Hospital Admissions Within 365 d | ||||||
| Comorbid Condition | No. (%) With Comorbidity at Index Visit | No. (%) | Adjusted RR (95% CI) | No. (%) | Adjusted RR (95% CI) | No. (%) | Adjusted RR (95% CI) | No. (%) | Adjusted RR (95% CI) |
| Hypertension | 14,334 (42.4) | 965 (6.7) | 0.92 (0.85-1.00) | 3,969 (27.7) | 0.98 (0.95-1.02) | 1,658 (11.6) | 1.00 (0.94-1.06) | 2,495 (17.4) | 1.05 (1.00-1.10) |
| “Respiratory failure/supplemental oxygen/shortness of breath” | 12,615 (37.3) | 949 (7.5) | 1.10 (1.02-1.19) | 3,875 (30.7) | 1.16 (1.12-1.20) | 1,690 (13.4) | 1.26 (1.19-1.33) | 2,432 (19.3) | 1.25 (1.19-1.31) |
| Screening and history of mental health and substance abuse codes | 10,014 (29.6) | 739 (7.4) | 1.05 (0.96-1.15) | 2,889 (28.9) | 1.01 (0.97-1.05) | 1,245 (12.4) | 1.02 (0.96-1.09) | 1,686 (16.8) | 1.02 (0.97-1.08) |
| Tobacco use | 9,937 (29.4) | 733 (7.4) | 1.05 (0.96-1.14) | 2,868 (28.9) | 1.01 (0.97-1.05) | 1,239 (12.5) | 1.02 (0.96-1.09) | 1,677 (16.9) | 1.03 (0.97-1.08) |
| Heart disease | 9,892 (29.3) | 633 (6.4) | 0.86 (0.79-0.94) | 2,795 (28.3) | 1.02 (0.98-1.06) | 1,141 (11.5) | 1.00 (0.93-1.06) | 1,824 (18.4) | 1.13 (1.07-1.19) |
| Diabetes | 7,076 (20.9) | 498 (7.0) | 0.98 (0.89-1.08) | 2,122 (30.0) | 1.08 (1.03-1.12) | 887 (12.5) | 1.08 (1.00-1.15) | 1,350 (19.1) | 1.16 (1.09-1.22) |
| Congestive heart failure | 5,050 (14.9) | 357 (7.1) | 1.01 (0.91-1.13) | 1,509 (29.9) | 1.11 (1.06-1.16) | 627 (12.4) | 1.15 (1.06-1.24) | 1,056 (20.9) | 1.29 (1.22-1.37) |
| Cardiac dysrhythmias, cardiac arrest and ventricular fibrillation | 4,322 (12.8) | 285 (6.6) | 0.93 (0.82-1.05) | 1,204 (27.9) | 1.02 (0.97-1.08) | 465 (10.8) | 0.98 (0.89-1.07) | 855 (19.8) | 1.20 (1.12-1.28) |
| Pneumonia | 4,250 (12.6) | 235 (5.5) | 0.76 (0.66-0.86) | 1,151 (27.1) | 0.97 (0.92-1.02) | 441 (10.4) | 0.89 (0.81-0.98) | 788 (18.5) | 1.11 (1.03-1.19) |
| Osteoarthritis | 1,312 (3.9) | 81 (6.2) | 0.88 (0.71-1.10) | 353 (26.9) | 0.98 (0.89-1.07) | 142 (10.8) | 0.97 (0.83-1.14) | 227 (17.3) | 1.02 (0.91-1.16)) |
| Bronchitis | 1,065 (3.2) | 58 (5.5) | 0.77 (0.60-0.99) | 281 (26.4) | 0.93 (0.84-1.03) | 106 (10.0 | 0.83 (0.69-1.00) | 169 (15.9) | 0.95 (0.83-1.10) |
| Upper respiratory infection | 973 (2.9) | 62 (6.4) | 0.90 (0.71-1.15) | 245 (25.2) | 0.89 (0.79-0.99) | 106 (10.9) | 0.91 (0.76-1.09) | 127 (13.1) | 0.79 (0.67-0.93) |
| Substance-related disorders | 512 (1.5) | 37 (7.2) | 1.00 (0.73-1.38) | 167 (32.6) | 1.14 (1.01-1.30) | 64 (12.5) | 1.00 (0.79-1.26) | 108 (21.1) | 1.35 (1.13-1.60) |
| Asthma | 427 (1.3) | 32 (7.5) | 1.07 (0.76-1.50) | 130 (30.4) | 1.07 (0.92-1.23) | 66 (15.5) | 1.28 (1.02-1.60) | 66 (15.5) | 0.96 (0.77-1.20) |
| COPD other | 385 (1.1) | 34 (8.8) | 1.25 (0.91-1.73) | 102 (26.5) | 0.93 (0.79-1.10) | 48 (12.5) | 1.04 (0.80-1.36) | 49 (12.7) | 0.76 (0.59-0.99) |
| Influenza | 219 (0.6) | 18 (8.2) | 1.19 (0.76-1.85) | 60 (27.4) | 1.00 (0.80-1.24) | 27 (12.3) | 1.09 (0.76-1.55) | 45 (20.6) | 1.25 (0.96-1.62) |
Comorbidity groups are based on a modified version of the Clinical Classification Software; see e-Table 4 (727.2KB, pdf) for details. Age- and sex-adjusted risk ratios compare the risk of the specified outcome (subsequent visit or hospital admission) within the risk period (30 or 365 d) among cohort members for whom a diagnosis code for the comorbid condition was present in any of the 11 diagnosis positions at the index visit to the risk among cohort members for whom a diagnosis code for the comorbid condition was not present at the index visits.
Discussion
Little population-based research has been conducted to estimate the burden of COPD-related ED visits. NC DETECT, a surveillance system that captures 99.5% of ED visits in North Carolina, provided an excellent opportunity to characterize COPD-related ED visits among a large population. We found that the COPD-related ED visit rate of 13.8 per 1,000 person-years among adults 45 years and older for 2008 to 2009 was higher than a national average of 8.72 per 1,000 person-years for 1992 to 2000 for adults ≥ 25 years of age.13 Our estimate was very similar to the 13.16 (per 1,000 person-years) annual rate for ages 55 to 64 years13 but lower than the study by Rosychuk et al,14 which included those ≥ 55 years of age (25.6/1,000). Differences between our rates and previous estimates are likely influenced by the study’s age distribution, COPD definition, and temporal increases in disease.
ED Visits
Our findings related to multiple ED visits were mixed compared with previous reports in US and Canadian EDs. We found patients on Medicare or Medicaid or noninsured patients were consistently more likely to have subsequent 30-day, 365-day, and multiple COPD ED visits within 365 days. Although Tsai et al15 similarly found Medicaid was associated with increased COPD ED visits, “other public (all Canadian and Medicare)” insurance was not. Similar to Watson et al,16 we found no sex differences for ED visits.
Hospital Admissions
Fifty-one percent of the cohort of patients with COPD was admitted to the hospital from the ED at the index visit. This percentage is twice as large as the overall hospitalization percentage for all ED visits made by patients aged ≥ 45 years in the NC DETECT data (25.8%). Regarding subsequent hospital admissions, older age was associated with increased likelihood of hospital admission,17 although in our study, the increased risk plateaued at ages 65 to 79 years. Again, similar to Watson et al,16 we did not find sex differences in subsequent hospital admission. In our study, public insurance (Medicaid, Medicare) was associated with increased likelihood of subsequent hospital admission; whereas Tsai et al17 found neither Medicaid nor “other public” insurance was associated with hospital admissions, which may suggest that these factors affect initial and subsequent hospital admissions differently.
Similar to Watson et al,16 we found no sex differences for hospitalizations. In contrast, Tsai et al17 found women at higher risk (RR, 2.3) of hospital admission, whereas Gonzalez et al18 found men at a higher risk of a COPD rehospitalization (hazard ratio, 1.12; 95% CI, 1.09-1.15). The variations in the published literature may be driven by differences in the severity and management of COPD in the various cohorts as well as secular trends in tobacco smoking among men and women.
Comorbidities
The prevalence of various comorbidities can vary by characteristics of the cohort and coding practices in the ED. In the literature, some cohorts have a very high prevalence of hypertension (63.4%),19 whereas others, including ours (42%), are within the 40% to 60% range.20‐22 Our congestive heart failure estimate of 21% was substantially higher than the 5% to 7% in Soriano et al23 and Curkendall et al22 but closer to the 15% found by Tsai et al.15 Some of these differences are likely due to the proportion of one sex vs another among the cohorts; other differences may be due to variations in ED coding practices.
“Respiratory failure/supplemental oxygen/shortness of breath” and congestive heart failure were two of the comorbidities with the largest association with increased hospital admissions; a “COPD other” comorbidity was associated with decreased hospital admissions. Our pneumonia comorbidity hospital admission RR (1.11) was comparable, although smaller in magnitude, with Tsai et al17 and Soriano et al.23 Tsai et al17 found that patients with pneumonia as a concomitant diagnosis were 4.87 (95% CI, 2.01-11.82) times as likely to be admitted to the hospital. Similarly, Soriano et al23 found patients with newly diagnosed COPD at higher risk for pneumonia comorbidity within the first year of diagnosis (RR, 16.0). Patients with a CCS congestive heart failure or “cardiac dysrhythmia/arrest/ventricular fibrillation” comorbidity grouping were 1.29 (95% CI, 1.22-1.37) and 1.20 (95% CI, 1.12-1.28) times as likely to be subsequently admitted to the hospital, respectively. These estimates are slightly lower than those from Dalal et al24 for patients with cardiovascular disease comorbidities—they were 1.62 (95% CI, 1.40-1.88) times as likely to be admitted to the hospital. Patients with “mixed” COPD/asthma diagnoses have been shown to be less likely to have hospital admissions (OR, 0.45; 95% CI, 0.25-0.80)15; similarly, we found cohort members with a “COPD-other” comorbidity (490.x, bronchitis, not specified as acute or chronic), at less risk of subsequent hospital admission.
Interestingly, “substance-related disorders” comorbidity, although present in only a small percentage (1.5%, 512 of 33,799) of the cohort, had the largest association with increased subsequent hospital admission among the comorbidities we examined. In examining the ICD-9-CM codes within the substance-related disorders cluster more closely, cocaine use (305.60) was the most frequent (23.5%), followed by “other, mixed or unspecified drug abuse” (305.90). We are unaware of published research that has directly shown such an association. We speculate the reasons for this increased hospital admission risk are multifaceted—substance abuse affects physical health and impedes access to care.25,26 We suggest further investigation of the relationship between substance-related disorders and COPD-related ED visits.
There are several limitations in our study. First, detailed clinical data (eg, spirometry, blood gas measurements, GOLD [Global Initiative for Chronic Obstructive Lung Disease outcomes]2) were not available. Using ICD-9-CM codes alone without clinical data, some patients with COPD could be misclassified. However, these detailed codes (491, 492, 496) have been shown to have good sensitivity (85%) and modest specificity (78.4%).8,27 Second, we chose to define a COPD-related visit when a COPD diagnostic code appeared in the first or second position. This decision was made using both previously reported approaches8‐10,27 and our sensitivity analysis using both a narrower and broader definition. Third, our study was conducted in North Carolina and may not be entirely representative of the pattern of COPD-related ED care for the nation. Adult smoking in NC is slightly higher than in the rest of the United States (19.8% vs 17.4%).28 However, the proportion who are ≥ 65 years of age is nearly equal to that of the country as a whole (13.2% vs 13.3%).29 Last, we are using secondary data, which are subject to general limitations, including potential coding errors, missing information, and changes in coding practices. For example, the use of the ICD-9-CM code for tobacco use has increased in recent years in NC DETECT ED visit data. Unlike a primary data collection effort, we are not able to definitively confirm whether the absence of a diagnosis code for a specific comorbidity means that the patient truly did not have that condition. However, several factors lend support to the validity and completeness of our comorbidity assessments: (1) provision of diagnosis codes is required for a hospital to be in compliance with the NC DETECT system; (2) diagnosis codes are used for billing purposes, so providers have a reimbursement incentive to provide full diagnoses; and (3) up to 11 diagnosis codes for each ED visit are collected and updated codes are accepted by NC DETECT.
Despite these limitations, a major strength of this research was the population-based nature of these surveillance system data; we characterized the burden of COPD-related ED care for a population of 9 million. The size of our study cohort was larger than many clinic-based studies20,23 and allowed sufficient statistical power to assess demographic variations in return ED visits, hospital admissions, and comorbidities. Existing national estimates have primarily been based on the Multicenter Airway Research Collaboration (MARC), with 29 EDs in 15 US states and three Canadian provinces, self-report interviews, and 2-week follow-up.15,30 In contrast, our estimates are based on administrative data from 110 to 111 EDs in rural and urban regions from one US state over a 2-year period. Both study designs are informative, and any differences in the results may reflect advantages or disadvantages of each approach.
We quantified estimates of COPD-related ED visits, return visits, hospital admissions, and comorbidities in the population. A high burden of COPD-related ED care was found for both repeat ED visits and hospital admissions. Next steps include both (1) further investigating the substance-related disorder comorbidity finding, and (2) conducting a validation of the case definition with chart reviews in a random sample of EDs within the NC DETECT system. Our research helps fill the information gap on the population-based burden of COPD-related ED care.
Supplementary Material
Online Supplement
Acknowledgments
Author contributions: Dr Yeatts takes responsibility for the integrity of the data and the accuracy of the data analysis.
Dr Yeatts: contributed to the study supervision, study concept and design, analysis and interpretation of the data, and statistical analysis; drafted the manuscript; and contributed critical revisions of the manuscript for important intellectual content.
Mr Lippmann: contributed to the concept and design, analysis and interpretation of the data, statistical analysis, and critical revisions of the manuscript for important intellectual content.
Dr Waller: contributed to the study concept and design, acquisition of the data, analysis and interpretation of the data, and critical revisions of the manuscript for important intellectual content.
Dr Hassmiller Lich: contributed to the study concept and design, analysis and interpretation of the data, and critical revisions of the manuscript for important intellectual content.
Dr Travers: contributed to the study concept and design, analysis and interpretation of the data, and critical revisions of the manuscript for important intellectual content.
Dr Weinberger: contributed to the study concept and design, analysis and interpretation of the data, and critical revisions of the manuscript for important intellectual content.
Dr Donohue: contributed to the study concept and design, analysis and interpretation of the data, and critical revisions of the manuscript for important intellectual content.
Financial/nonfinancial disclosures: The authors have reported to CHEST that no potential conflicts of interest exist with any companies/organizations whose products or services may be discussed in this article.
Role of sponsors: The content of this paper is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources, the National Institutes of Health, the Centers for Disease Control and Prevention, the North Carolina Public Health Data Group, or the NC DETECT. The NC DETECT Data Oversight Committee does not take responsibility for the scientific validity or accuracy of methodology, results, statistical analyses, or conclusions presented.
Other contributions: We thank David Richardson, PhD, for his support; he funded Mr Lippmann’s graduate research assistant position through a Gillings Innovation Laboratory grant. Data were obtained from the NC Department of Health and Human Services/Division of Public Health NC DETECT system under a data use agreement.
Additional information: The e-Tables can be found in the “Supplemental Materials” area of the online article.
Abbreviations
- CCS
Clinical Classification Software
- ICD-9-CM
International Classification of Diseases, Ninth Revision, Clinical Modification
- IRB
institutional review board
- NC DETECT
North Carolina Disease Event Tracking and Epidemiologic Collection Tool
- RR
risk ratio
Footnotes
Funding/Support: The statistical analysis for this research was partially supported by a University of North Carolina, Gillings School of Global Public Health Gillings Innovation Grant. Drs Lich and Weinberger’s time was partially supported by the National Center for Research Resources [Award KL2RR025746 to Dr Lich], a VA Senior Research Career Scientist Award from the Health Services Research and Development Service [RCS 91-408] (Dr Weinberger). North Carolina Disease Event Tracking and Epidemiologic Collection Tool data were provided by the North Carolina Public Health Data Group.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians. See online for more details.
References
- 1.Mannino DM, Homa DM, Akinbami LJ, Ford ES, Redd SC. Chronic obstructive pulmonary disease surveillance—United States, 1971-2000. MMWR Surveill Summ. 2002;51(6):1-16. [PubMed] [Google Scholar]
- 2.Vestbo J, Hurd SS, Agustí AG, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD Executive Summary. Am J Respir Crit Care Med. 2013;187(4):347-365. [DOI] [PubMed] [Google Scholar]
- 3.Rodríguez-Roisin R, Soriano JB. Chronic obstructive pulmonary disease with lung cancer and/or cardiovascular disease. Proc Am Thorac Soc. 2008;5(8):842-847. [DOI] [PubMed] [Google Scholar]
- 4.CDC. Public health strategic framework for COPD prevention. Centers for Disease Control website. 2011. http://www.cdc.gov/copd/pdfs/Framework_for_COPD_Prevention.pdf. Accessed July 19, 2012.
- 5.UNC Department of Emergency Medicine Carolina Center for Health Informatics Report, NC DETECT Emergency Department Data: 2008. Carolina Center for Health Informatics, Department of Emergency Medicine, University of North Carolina at Chapel Hill; 2010. NC Disease Event Tracking and Epidemiologic Collection Tool website. http://www.ncdetect.org/NCD%202008%20AnnualRep%20Final%20Color%202010July.pdf. Accessed July 29, 2012.
- 6.UNC Department of Emergency Medicine Carolina Center for Health Informatics Report, Overview and Analysis of NC DETECT Emergency Department Data: 2009. Carolina Center for Health Informatics, Department of Emergency Medicine, University of North Carolina at Chapel Hill; 2011. NC Disease Event Tracking and Epidemiologic Collection Tool website. http://www.ncdetect.org/Final_2009NCDETECT_ANNUALREPORT_Color.pdf. Accessed July 29, 2012.
- 7.North Carolina State Demographics Branch of the Office of State Budget and Management. http://www.osbm.state.nc.us/ncosbm/facts_and_figures/socioeconomic_data/population_estimates/county_projections.shtm. Accessed July 29, 2012.
- 8.Gershon AS, Warner L, Cascagnette P, Victor JC, To T. Lifetime risk of developing chronic obstructive pulmonary disease: a longitudinal population study. Lancet. 2011;378(9795):991-996. [DOI] [PubMed] [Google Scholar]
- 9.Morbidity and mortality 2012 chartbook on cardivascular, blood, and lung diseases. 2012. National Heart, Lung and Blood Institute. http://www.nhlbi.nih.gov/resources/docs/2012_ChartBook.pdf. Accessed July 29, 2012.
- 10.American Lung Association COPD trend report 2010. 2010. American Lung Association website. http://www.lung.org/finding-cures/our-research/trend-reports/copd-trend-report.pdf. Accessed July 29, 2012.
- 11.Clinical classification software (CCS) for ICD-9-CM. Healthcare Cost of Utilization Project website. http://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp. Accessed July 29, 2012.
- 12.Travers DA, Haas SW, Waller AE, Tintinalli JE. Diagnosis clusters for emergency medicine. Acad Emerg Med. 2003;10(12):1337-1344. [DOI] [PubMed] [Google Scholar]
- 13.Mannino DM, Homa DM, Akinbami LJ, Ford ES, Redd SC. Chronic obstructive pulmonary disease surveillance—United States, 1971-2000. Respir Care. 2002;47(10):1184-1199. [PubMed] [Google Scholar]
- 14.Rosychuk RJ, Voaklander DC, Senthilselvan A, Klassen TP, Marrie TJ, Rowe BH. Presentations to emergency departments for chronic obstructive pulmonary disease in Alberta: a population-based study. CJEM. 2010;12(6):500-508. [DOI] [PubMed] [Google Scholar]
- 15.Tsai CL, Griswold SK, Clark S, Camargo CA., Jr Factors associated with frequency of emergency department visits for chronic obstructive pulmonary disease exacerbation. J Gen Intern Med. 2007;22(6):799-804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Watson L, Vestbo J, Postma DS, et al. Gender differences in the management and experience of chronic obstructive pulmonary disease. Respir Med. 2004;98(12):1207-1213. [DOI] [PubMed] [Google Scholar]
- 17.Tsai CL, Clark S, Cydulka RK, Rowe BH, Camargo CA., Jr Factors associated with hospital admission among emergency department patients with chronic obstructive pulmonary disease exacerbation. Acad Emerg Med. 2007;14(1):6-14. [DOI] [PubMed] [Google Scholar]
- 18.Gonzalez AV, Suissa S, Ernst P. Gender differences in survival following hospitalisation for COPD. Thorax. 2011;66(1):38-42. [DOI] [PubMed] [Google Scholar]
- 19.Almagro P, Cabrera FJ, Diez J, et al. ; Working Group on COPD, Spanish Society of Internal Medicine. Comorbidities and short-term prognosis in patients hospitalized for acute exacerbation of COPD: the EPOC en Servicios de Medicina Interna (ESMI) study. Chest. 2012;142(5):1126-1133. [DOI] [PubMed] [Google Scholar]
- 20.Patel AR, Hurst JR. Extrapulmonary comorbidities in chronic obstructive pulmonary disease: state of the art. Expert Rev Respir Med. 2011;5(5):647-662. [DOI] [PubMed] [Google Scholar]
- 21.Barr RG, Celli BR, Mannino DM, et al. Comorbidities, patient knowledge, and disease management in a national sample of patients with COPD. Am J Med. 2009;122(4):348-355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Curkendall SM, DeLuise C, Jones JK, et al. Cardiovascular disease in patients with chronic obstructive pulmonary disease, Saskatchewan Canada cardiovascular disease in COPD patients. Ann Epidemiol. 2006;16(1):63-70. [DOI] [PubMed] [Google Scholar]
- 23.Soriano JB, Visick GT, Muellerova H, Payvandi N, Hansell AL. Patterns of comorbidities in newly diagnosed COPD and asthma in primary care. Chest. 2005;128(4):2099-2107. [DOI] [PubMed] [Google Scholar]
- 24.Dalal AA, Shah M, Lunacsek O, Hanania NA. Clinical and economic burden of depression/anxiety in chronic obstructive pulmonary disease patients within a managed care population. COPD. 2011;8(4):293-299. [DOI] [PubMed] [Google Scholar]
- 25.Snyder LD, Eisner MD. Obstructive lung disease among the urban homeless. Chest. 2004;125(5):1719-1725. [DOI] [PubMed] [Google Scholar]
- 26.Mandelberg JH, Kuhn RE, Kohn MA. Epidemiologic analysis of an urban, public emergency department’s frequent users. Acad Emerg Med. 2000;7(6):637-646. [DOI] [PubMed] [Google Scholar]
- 27.Gershon AS, Wang C, Guan J, Vasilevska-Ristovska J, Cicutto L, To T. Identifying individuals with physcian diagnosed COPD in health administrative databases. COPD. 2009;6(5):388-394. [DOI] [PubMed] [Google Scholar]
- 28.Behavioral Risk Factor Surveillance Survey. Centers for Disease Control and Prevention website. http://apps.nccd.cdc.gov/statesystem/HighlightReport/HighlightReport.aspx?FromHomePage=Y&StateName=North%20Carolina&StateId=NC. Accessed January 14, 2013. [Google Scholar]
- 29.United States Census Bureau. State & county quickfacts. US Census Bureau website. http://quickfacts.census.gov/qfd/states/37000.html. Accessed January 14, 2013. [Google Scholar]
- 30.Rowe BH, Cydulka RK, Tsai CL, Clark S, Sinclair D, Camargo CA., Jr Comparison of Canadian versus United States emergency department visits for chronic obstructive pulmonary disease exacerbation. Can Respir J. 2008;15(6):295-301. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Online Supplement