Abstract
Background: Transversus abdominis plane (TAP) block and local anaesthetic wound infiltration can provide effective pain relief at the wound site after surgery. However, the relative efficacy of two techniques for postoperative analgesia remains controversial. Methods: We searched PUBMED, EMBASE and CENTRAL databases for randomized controlled trials (RCTs) comparing TAP block with wound infiltration for pain relief after surgery. The primary outcomes were pain scores at rest and on movement at 1, 8 and 24 hours postoperatively and cumulative morphine consumption over 24 hours. The secondary outcomes were time to first rescue analgesic, number of rescue analgesic use and opioids-related side-effects. Results: Nine RCTs with a total of 500 participants were included. TAP block was associated with significant lower rest and dynamic pain scores at 8 hour [MD = -1.08, 95% CI (-1.89-0.26), P = 0.009] and 24 hour [MD = -0.83, 95% CI (-1.60, -0.06), P = 0.03] postoperatively than wound infiltration, but no significant difference was found at 1 hour [MD = -0.94, 95% CI (-1.97, 0.09), P = 0.08] postoperatively. In adults, TAP block significantly reduced 24-hour overall morphine consumption by 3.85 mg [MD = -3.85, 95% CI (-7.47, -0.22), P = 0.04] compared with wound infiltration. Subgroup analysis showed that adults received TAP block appeared to have lower rest pain scores at 24 hour than children (P = 0.008). Conclusion: TAP block provides superior analgesia compared with wound infiltration in the setting of a multimodal analgesic regimen. Subgroup analysis indicated that adults may have benefits additional to the analgesic effect than children.
Keywords: Acute pain, anaesthetic techniques, regional pain, regional blockade, TAP block
Introduction
Much of postoperative pain is derived from the surgical incision and visceral sites [1,2]. Transversus abdominis plane (TAP) block, firstly described by Rafi et al in 2001, can block sensory nerve supply to the anterior abdominal wall by injecting local anaesthetics into the transversus abdominis fascial plane, which is located between the internal oblique and transversus abdominis muscles layers [3]. The TAP block, has shown effective pain relief after abdominal surgery [4,5], hysterectomy surgery [6] and caesarean delivery [7,8] compared with no intervention or placebo in previous meta-analyses.
Local anaesthetic infiltration into the surgical incision can relieve pain at the wound site after surgery, as part of multimodal analgesic approach [9-11]. This simple, safe, low-invasion and low-cost technique, commonly performed by surgeon, is routinely conducted in many centers for postoperative analgesia [2,12,13]. To data, the efficacy of TAP block versus wound infiltration on postoperative analgesia remains controversial. Therefore, the main objective of the current review is to compare the efficacy and safety of TAP block with wound infiltration for pain relief after surgery. The primary outcomes were pain scores at rest and on movement at 1, 8 and 24 hours postoperatively and cumulative morphine consumption over 24 hours. The secondary outcomes were time to first rescue analgesic, number of rescue analgesic use and opioids-related side-effects.
Methods
We followed the PRISMA [14] (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines in the preparation of this review.
Literature search
The PUBMED, EMBASE and Cochrane Central Register of Controlled Trials (CENTRAL) were searched for randomized controlled trials (RCTs) that assessed the efficacy of postoperative pain relief comparing TAP block with local anaesthetic wound infiltration from database inception to 8 August 2014. The free text “TAP”, “transversus abdominis plane”, “transverse abdominis plane”, “infiltration”, “irrigation”, “instillation” were used in combination with the medical subject headings (MeSH), “abdominal muscles”, “abdominal wall”, “nerve block”, “anaesthetics, local”, “anesthesia, local”. No language restriction was used.
Inclusion and exclusion criteria
Inclusion criteria: full-text available RCTs, participants of any age or sex undergoing any type of elective or emergency surgery, comparing TAP block with wound infiltration analgesia, reported at least on pain scores or opioids consumption as postoperative pain outcomes. Exclusion criteria: comparing the combination effect (TAP block + wound infiltration) with TAP or wound infiltration, participants involved other nerve block.
Data collection
Two independent authors assessed the risk of bias of included studies using the Cochrane risk of bias tool. Five parameters (randomization sequence generation, allocation concealment, blinding, incomplete outcome data, selective reporting) of each included studies were assessed as low, unclear or high risk of bias. Any discrepancies were resolved by discussion with the third author.
A data collection sheet was created to extract data from eligible studies by two independent authors. Pain intensity reported on 0 to 100 mm scale with visual analog scale (VAS) or numeric rating scale (NRS) was converted to a 0 to 10 cm scale. Postoperative opioids consumption was converted to the equivalent dose of intravenous morphine as follow: tramadol (1:10) and fentanyl (10:1) [15]. Where data were presented as values other than mean and standard deviations, we tried to contact the author to obtain raw data. If it is not possible, data were converted to mean and standard deviation using previously described methodology and allow more studies to be included in the meta-analysis [16].
Statistical analysis
Dichotomous data were expressed as risk ratio (RR) with 95% confidence intervals (CI) and continuous variables are expressed as the mean difference (MD) with 95% CI. Difference was considered statistically significant if P<0.05, or 95% CI of RR excluded 1, or 95% CI excluded 0 for the MD. The I2 statistic was used to assess heterogeneity. If heterogeneity was significant (I2>50%), a random effects model was used; otherwise a fixed effects model was used. Analyses were performed using the Review Manager (RevMan) version 5.1 (Copenhagen: The Nordic Cochrane Centre, the Cochrane Collaboration, 2011).
Results
Electronic search resulted in a total of 423studies. After screening title and abstract, we retained 27 studies for further assessment. Finally, nine studies with 500 participants were included in this review. A flowchart of the literature search for included studies is shown in Figure 1.
Figure 1.
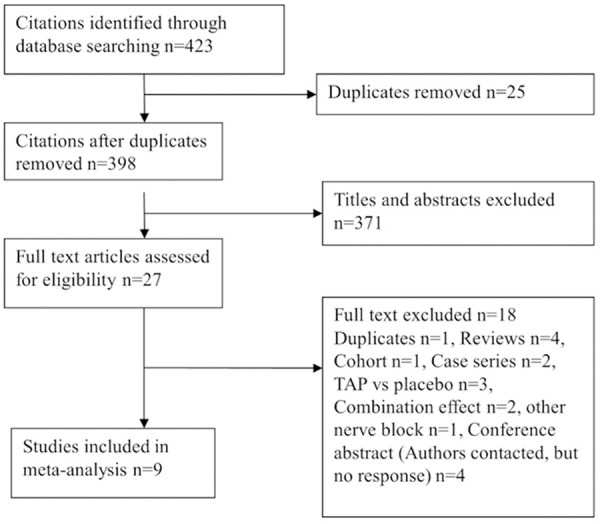
Flowchart of the literature search for included studies.
The sample size of most included studies was small, from 32 to 87 participants. Three studies included a total of 176 child participants, mean or median ages ranged from 0.7 to 11 years [2,12,17]. Studies with adult participants aged from mean or median of 28 to 63 years [18-23]. All nine studies involved elective surgery, including general [2,17,22,23], urinary [12,20], gynecology and obstetrics operations [18,19,21]. Except one study performed caesarean section under spinal anesthesia [18], all studies involved general anesthesia [2,12,17,19-23]. Both TAP block and wound infiltration were performed using single-shot technique in nine studies. The methodological quality of four studies was low risk using the Cochrane risk of bias criteria [2,12,20,23], and remaining five studies was moderate to high risk [17-19,21,22]. Three studies mentioned “randomly”, but did not describe the method to generate a random sequence [17,19,22]. Allocation concealment was not mentioned in two studies [18,21]. In one study, the authors only mentioned that blinding began in the recovery room and recovery room nurse was blinded, thus it was uncertain whether blinding was adequately performed [17]. Aydogmus et al mentioned “double-blinded study” and an investigator who collect data was blinded, but we did not know whether participants were blinded [18]. The characteristics and risk of bias of the included studies are shown in details in Tables 1, 2.
Table 1.
Characteristics of the included studies
| Study | No. of patients | Operation procedure and Anesthetic technology | TAP block group | Wound infiltration group | Postoperative analgesia regimen | Outcomes |
|---|---|---|---|---|---|---|
| Skjelsager 2013 [20] | 48 | Open radical retropubic prostatectomy under GA with propofol and remifentanil | Time: end of the surgery | Time: end of the surgery | Oral paracetamol 1000 mg /6 h, ibuprofen 600 mg/8 h, IV morphine and morphine PCA. | Pain scores at rest and on movement at 1, 2, 4, 6, 8, 20, 24 h, cumulative morphine consumption over 24 h, side-effects (nausea and sedation scores, number of vomiting). |
| T 23 | Localization: ultrasound guide bilateral | Localization: subcutaneous by the operating surgeon | ||||
| W 25 | LA: 20 ml ropivacaine 0.75% on each side | LA: 40 ml ropivacaine 0.75% | ||||
| Atim 2011 [19] | 37 | Total abdominal hysterectomy under GA with sevoflurane | Time: after induction | Time: end of the surgery | Tramadol PCA and IM pethidine as rescue analgesic. | Pain scores at rest and on movement at 1, 2, 4, 6, 24 h, tramadol consumption at 1, 2, 4, 6, 24 h, number of rescue analgesic, rescue analgesic consumption. |
| T 18 | Localization: ultrasound guide bilateral | Localization: skin and subcutaneous tissues of the surgical incision site | ||||
| W 19 | LA: 20 ml bupivacaine 0.25% on each side | LA: 20 ml bupivacaine 0.25% | ||||
| Sahin 2013 [17] | Children 57 | Unilateral inguinal hernia repair under GA with sevoflurane and N2O | Time: after induction | Time: during wound closure | Oral paracetamol 15 mg /kg/4 h and IV morphine 0.05 mg/kg as rescue analgesic | Pain scores at 1, 2, 4, 8, 12, 16, 20, 24 h, time of first analgesic use, number of analgesic uses, cumulative dose of paracetamol, side-effects (postoperative nausea, vomiting, hypotension, bradycardia and arrhythmia). |
| T 29 | Localization: ultrasound guide | Localization: between the external aponeurosis and the skin by the surgeons | ||||
| W 28 | LA: 0.5 ml/kg levobupivacaine 0.25% | LA: 0.2 ml/kg levobupivacaine 0.25% | ||||
| Ortiz 2012 [23] | 74 | Laparoscopic cholecystectomy under GA with sevoflurane | Time: after induction | Time: preincisional | Oral hydrocodone 10 mg, acetaminophen 1000 mg/6 h and for severe pain IV morphine 4 mg/3 h | Pain scores at 0, 5, 10, 15, 20, 25 h, morphine consumption over 24 h, hydrocodone consumption over 24 h, the number of nausea. |
| T 39 | Localization: ultrasound guided bilateral | Localization: infiltration of the 4 trocar insertion sites | ||||
| W 35 | LA: 15 ml of ropivacaine 0.5% on each side | LA: 20 ml of ropivacaine 0.5% | ||||
| Tolchard 2012 [22] | 43 | Laparoscopic cholecystectomy under GA | Time: no mention | Time: end of surgery | IV fentanyl and oral weak opioids and non-opioid analgesic. | Pain scores at 0, 1, 2, 3, 4 h, fentanyl consumption in PACU, morphine tramadol and codeine consumption in ward, time to discharge. |
| T 21 | Localization: ultrasound guided | Localization: port-site infiltration by surgeon | ||||
| W 22 | LA: 1 mg/kg bupivacaine | LA: 1 mg/kg bupivacaine | ||||
| Sandeman 2011 [2] | Children 87 | Laparoscopic appendicectomy under GA with sevoflurane and N2O | Time: after induction | Time: at the port placement | Morphine PCA and regular oral paracetamol 15 mg/kg. | Pain scores at 0, 4, 8, 12, 16 h, number of PCA use, morphine PCA consumption, time to first morphine use, time to first non-PCA analgesic, side-effects and time in the PACU and hospital. |
| T 42 | Localization: ultrasound guided bilateral | Localization: port sites infiltration by the surgeon | ||||
| W 45 | LA: 0.5 mg/kg ropivacaine 0.2% on each side (2 mg/kg total of ropivacaine) | LA: 0.5 ml/kg of ropivacaine 0.2% (1 mg/kg total ropivacaine) | ||||
| Lorenzo 2014 [12] | Children 32 | Unilateral open pyeloplasty under GA with sevoflurane | Time: before incision | Time: before incision | IV morphine 0.05 mg/kg or ketorolac 0.5 mg/kg in the PACU and oral morphine, acetaminophen and ketorolac in the ward | Pain scores at PACU, number of rescue morphine use, morphine consumption in PACU and ward, side-effects and hospital stay. |
| T 16 | Localization: ultrasound guided | Localization: regional field block by surgeon | ||||
| W 16 | LA: 0.4 ml/kg bupivacaine 0.25% with1:200000 epinephrine | LA: 0.4 ml/kg bupivacaine 0.25% with 1:200000 epinephrine | ||||
| Sivapurapu 2013 [21] | 52 | Lower abdominal gynecological surgery under GA with isoflurane and N2O | Time: after skin closure | Time: after skin closure | IV morphine and morphine PCA. | Pain scores at 2, 4, 6, 24 h, time to first rescue analgesic, 24 h morphine consumption and side-effects (sedation scores at 2, 4, 6, 24 h and PONV incidence). |
| T 26 | Localization: ultrasound guided bilateral | Localization: surgical incision | ||||
| W 26 | LA: 0.3 ml/kg bupivacaine 0.25% on each side | LA: 0.6 ml/kg of 0.25% bupivacaine. | ||||
| Aydogmus 2014 [18] | 70 | Caesarean section under spinal anesthesia with hyperbaric bupivacaine 10 mg plus fentanyl 20 μg | Time: after the surgical procedure was acomplished | Time: completion of the surgical procedure | IM diclofenac sodium 75 mg and IV tramadol 50 mg. | Pain scores at 2, 6, first mobilization, 12, 24 h, time to first analgesic, intraoperative complication, side-effect and patient satisfaction. |
| T 35 | Localization: ultrasound guided bilateral | Localization: subcutaneous wound site infiltration | ||||
| W 35 | LA: 20 ml (50 mg) levobupivacaine 0.25% on each side | LA: 40 ml (100 mg) levobupivacaine 0.25% |
GA = general anesthesia, TAP = transversus abdominis plane, IV = intravenous, IM = intramuscular, LA = local anaesthetic, PCA = patient controlled analgesia, PACU = post-anesthetic care unit, T = TAP block group, W = wound infiltration group.
Table 2.
The risk of bias of the included studies
| Study | Radom squence geeration | Allocation cocealment | Blinding of participants and personnel | Blinding of outcome assessment | Incomplete outcome data | Selective reporting |
|---|---|---|---|---|---|---|
| Skjelsager 2013 [20] | Low | Low | Low | Low | Low | Low |
| Atim 2011 [19] | Unclear | Low | Low | Low | Low | Unclear |
| Sahin 2013 [17] | Unclear | Low | High | High | Low | Low |
| Ortiz 2012 [23] | Low | Low | Low | Low | Low | Low |
| Tolchard 2012 [22] | Unclear | Low | Low | Low | Low | Low |
| Sandeman 2011 [2] | Low | Low | Low | Low | Low | Low |
| Lorenzo 2014 [12] | Low | Low | Low | Low | Low | Low |
| Sivapurapu2013[21] | Low | Unclear | Low | Low | Low | Low |
| Aydogmus 2014 [18] | Low | Unclear | Unclear | Low | Low | Low |
Pain scores at rest at 1, 8 and 24 hour postoperatively
Rest pain scores were reported at 1 hour postoperatively in five studies [17,19,20,22,23], at 2 hour in two studies [18,21], at 4 hour in one study [22], at 6 hours in two studies [18,19], at 8 hour in four studies [2,17,20,23], at 16 hour in one study [2] and at 24 hours in six studies [17-21,23]. Rest pain scores at 2 hours were combined into that at 1hour; pain scores at 4 and 6 hour were combined into that at 8 hours and pain scores at 16 hour were combined into that at 24 hours. TAP block showed significant lower rest pain scores at 8 hour [MD = -1.08, 95% CI (-1.89-0.26), P = 0.009] and 24-hour [MD = -0.83, 95% CI (-1.60, -0.06), P = 0.03] than wound infiltration, but no significant difference was found at 1 hour [MD = -0.94, 95% CI (-1.97, 0.09), P = 0.08]. However, there was significant heterogeneity in all analyses (for 1 hour: I2 = 89%; for 8 hour: I2 = 84%; for 24 hour: I2 = 93%) (Figure 2). Subgroup analysis of different participants didn’t reveal any difference between children and adults in rest pain scores at 1 (P = 0.07) and 8 hour (P = 0.73). However, adults received TAP block appeared to have lower rest pain scores at 24 hour than children (P = 0.008) (Supplementary Figure 1). Comparing different types of surgery showed no significant difference between laparoscopic and non-laparoscopic surgery in rest pain scores at all end-points (for 1 hour: P = 0.48; for 8 hour: P = 0.16; for 24 hour: P = 0.17) (Supplementary Figure 2). TAP block performed at the end of surgery had marginally significant lower pain scores than that performed before incision at 24 hour postoperatively (P = 0.05), but no significant difference was found at 1 (P = 0.17) and 8 hour (P = 0.63) (Supplementary Figure 3).
Figure 2.

Pain scores at rest at 1, 8 and 24 hour postoperatively.
Pain scores on movement at 1, 8 and 24 hour postoperatively
Dynamic pain scores were assessed at 1 hour postoperatively in two studies [19,20], at 6 hour in one study [19], at 8 hour in one study [20] and at 24 hour in two studies [19,20]. TAP block showed significant lower dynamic pain scores at 8 hour [MD = -0.66, 95% CI (-1.30, -0.03), P = 0.04] and 24 hour [MD = -0.93, 95% CI (-1.48, -0.39), P = 0.0007], but no significant difference was seen at 1 hour [MD = -1.01, 95% CI (-2.06, 0.04), P = 0.06] compared with wound infiltration (Figure 3). There was no significant heterogeneity in both analyses (for 1, 8 and 24 hour: I2 = 0%).
Figure 3.
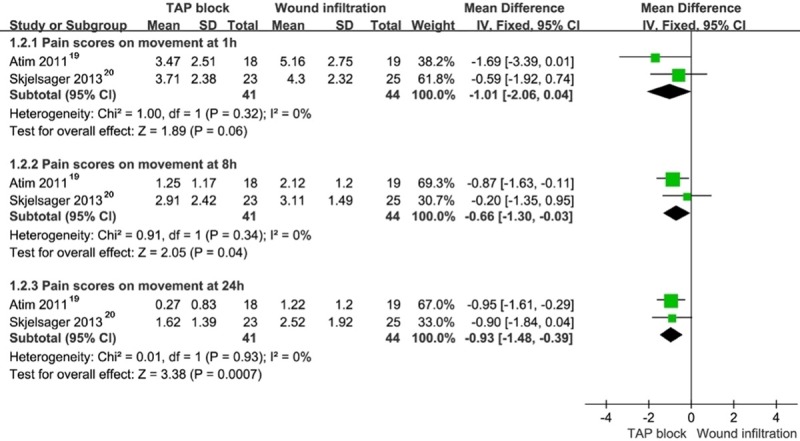
Pain scores on movement at 1, 8 and 24 hour postoperatively.
Cumulative morphine consumption over 24 hour
Five studies investigated 24-hour overall morphine consumption in adult participants [19-23]. TAP block reported significant reduction in 24-hour overall morphine consumption compared with wound infiltration [MD = -3.85, 95% CI (-7.47, -0.22), P = 0.04]. However, there was significant heterogeneity (I2 = 80%) (Figure 4). In one study with 57 children, TAP block consumed less oral paracetamol (mg/kg) over 24 hour than wound infiltration [MD = -33.30, 95% CI (-35.88, -30.72)] 17. In another children study reporting morphine consumption (μg/kg) at 0-8 hour and 8-16 hour as median and range found no significant difference between two groups [2]. In Lorenzo et al, more morphine (mg/kg) consumption was found in TAP block in PACU [MD = 0.04, 95% CI (0.01, 0.07)], but no significant difference was found with respect to overall morphine consumption (PACU + ward) [MD = 0.01, 95% CI (-0.04, 0.06)] in 32 children [12] The subgroup analysis of different types of surgery (laparoscopic vs non- laparoscopic surgery, P = 0.77) and different time of TAP block performed (before incision vs end of surgery, P = 0.86) didn’t reveal any significant difference in cumulative morphine consumption over 24 hour (Supplementary Figures 4, 5).
Figure 4.
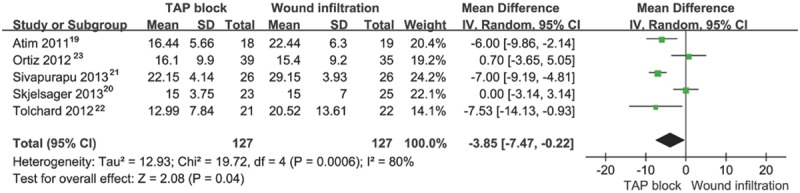
Cumulative morphine consumption over 24 hour (mg).
Time to first rescue analgesic and number of rescue analgesic use
Time to first rescue analgesic (hour) assessed in four studies reported no significant difference between TAP block and wound infiltration [MD = 2.55, 95% CI (-0.36, 5.46), P = 0.09] (Figure 5) [2,17,18,21]. There was also no significant difference in number of rescue analgesic use between two groups [RR = 0.95, 95% CI (0.56, 1.60), P = 0.85] (Figure 6) [12,17-19]. However there was significant heterogeneity (for former: I2 = 84%; for later: I2 = 83%).
Figure 5.
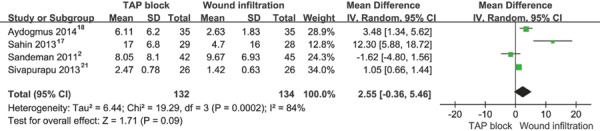
Time to first rescue analgesic (hour).
Figure 6.
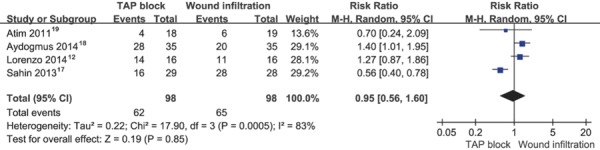
Number of rescue analgesic use.
Side-effects
Six studies reported incidence of postoperative nausea and vomiting (PONV), but only three studies present enough data for quantity analysis [12,17,18,20,21,23]. Pool results showed no significant difference in PONV incidence between two groups [RR = 1.08, 95% CI (0.69, 1.71), P = 0.73, I2 = 0%] (Figure 7) [17,20,23]. In qualitative analysis, two of remaining three studies reported similar PONV incidence between two groups [12,18], whereas one study showed significant lower PONV incidence in TAP block [21]. One study reporting sedation scores as median and interquartile distance showed no significant difference between TAP block and wound infiltration [20]. In another study, TAP block had significant lower sedation scores at 2 and 4 hour postoperatively than wound infiltration [21]. Two studies investigated excessive sedation incidence reported no difference between two groups [2,12].
Figure 7.
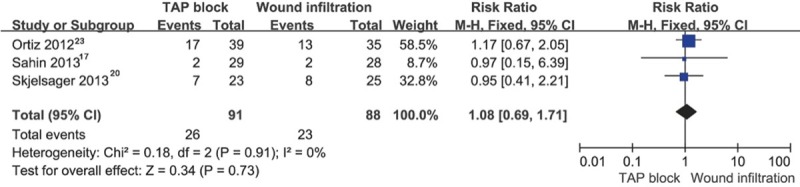
Postoperative nausea and vomiting (PONV) incidence.
Discussion
In this review, we included nine studies with a total of 500 participants comparing the postoperative analgesia efficacy and safety of TAP block with wound infiltration.
TAP block had lower VAS pain scores at rest and on movement at 8 and 24 hour postoperatively, but no significant difference was found at 1 hour compared with wound infiltration. Our findings indicated that local anaesthetic wound infiltration may provide brief pain relief for less than 8 hour after surgery. Similarly, several previous studies have shown that wound infiltration only decrease immediate postoperative pain scores (in PACU or within several hours postoperatively) compared with placebo or no intervention in breast surgery [24,25], hip arthroplasty [26], inguinal herniorrhaphy [27] and caesarean section [28]. In contrast, using catheter technique, both wound infiltration and TAP block can permit the delivery of continuous analgesia for a longer postoperative duration than single-shot block. In a meta-analysis included nine studies with 505 participants, continuous local anaesthetic wound catheter infiltration even was equivalent to epidural analgesia in terms of pain scores at rest and on movement at 24 and 48 hour after abdominal surgery [29] Therefore, future RCTs are needed to assess the analgesia efficacy of local anaesthetic wound catheter infiltration after surgery.
Opioid requirement, a surrogate marker of pain, was lower by 3.85 mg in TAP block compared with wound infiltration over 24 hour in adults. However, the inconsistency in reporting cumulative opioid consumption precluded quantitative analysis in three studies with 176 children. In qualitative analysis, two of three child studies shown no significant difference in cumulative morphine consumption between two groups, but TAP block required significant less oral paracetamol than wound infiltration in study of Sahin et al. However, the methodological quality of Sahin et al was high risk, as the blinding was not likely to be adequately performed.
The PONV incidence and sedation scores were not significant difference between TAP block and wound infiltration in most included studies. Furthermore, no serious complications were reported following two groups in all nine studies. TAP block is a less invasive method, but it is not without risk. With or without ultrasound guidance, reports of liver, bowl, nerve injuries and intraperitoneal and intravascular injection following TAP block have recently emerged [30-32]. Given the paucity of case reports about serious complications and popularity of TAP block, the incidence of catastrophic complications seem extremely small.
There was significant heterogeneity among studies, likely due to different participants, different types of surgery, different TAP block and wound infiltration technique, difference in dose and volume of local anaesthetic administrated and different postoperative analgesia. An attempt was made to pool the studies according to participants, types of surgery and the time TAP block performed. The subgroup analysis demonstrated that adults received TAP block showed more benefits from rest pain scores than children at 24 hour postoperatively, but no significant benefits were found at 1 and 8 hour postoperatively. We also found that TAP block performed at the end of surgery seems to provide marginally more effective pain relief than that performed before incision at 24 hour postoperatively, and no significant difference was found at 1 and 8 hour postoperatively. However, limited studies were conducted to subgroup analysis and there still was significant heterogeneity in most subgroup analysis. Therefore, the results from subgroup analysis may be biased and need to be interpreted with caution.
Epidural analgesia is still considered as “golden standard” for postoperative analgesia, mostly because of its strong analgesic effects. However, the relative efficacy of TAP block and epidural analgesia remains controversial. TAP block was inferior to epidural analgesia with respect to postoperative analgesia in two studies [33,34]. On the contrary, comparable analgesia efficacy was found between TAP block and epidural analgesia in other two studies [35,36]. Future studies with large sample size are necessary to compare TAP block with epidural analgesia for postoperative analgesia to reach a definite conclusion.
Conclusion
In conclusion, TAP block appeared to be superior to local anaesthetic wound infiltration with respect to postoperative analgesia in the setting of a multimodal analgesic regimen. Adults may have benefits additional to the analgesic effect than children. It deserves to further assess the postoperative analgesia efficacy of TAP block versus epidural analgesia in the future study.
Disclosure of conflict of interest
None.
Supporting Information
References
- 1.Carney J, McDonnell JG, Ochana A, Bhinder R, Laffey JG. The transversus abdominis plane block provides effective postoperative analgesia in patients undergoing total abdominal hysterectomy. Anesth Analg. 2008;107:2056–60. doi: 10.1213/ane.0b013e3181871313. [DOI] [PubMed] [Google Scholar]
- 2.Sandeman DJ, Bennett M, Dilley AV, Perczuk A, Lim S, Kelly KJ. Ultrasound-guided transversus abdominis plane blocks for laparoscopic appendicectomy in children: A prospective randomized trial. Br J Anaesth. 2011;106:882–6. doi: 10.1093/bja/aer069. [DOI] [PubMed] [Google Scholar]
- 3.Rafi AN. Abdominal field block: A new approach via the lumbar triangle. Anaesthesia. 2001;56:1024–6. doi: 10.1046/j.1365-2044.2001.02279-40.x. [DOI] [PubMed] [Google Scholar]
- 4.Johns N, O’Neill S, Ventham NT, Barron F, Brady RR, Daniel T. Clinical effectiveness of transversus abdominis plane (TAP) block in abdominal surgery: A systematic review and meta-analysis. Colorectal Dis. 2012;14:e635–42. doi: 10.1111/j.1463-1318.2012.03104.x. [DOI] [PubMed] [Google Scholar]
- 5.Siddiqui MR, Sajid MS, Uncles DR, Cheek L, Baig MK. A meta-analysis on the clinical effectiveness of transversus abdominis plane block. J Clin Anesth. 2011;23:7–14. doi: 10.1016/j.jclinane.2010.05.008. [DOI] [PubMed] [Google Scholar]
- 6.Champaneria R, Shah L, Geoghegan J, Gupta JK, Daniels JP. Analgesic effectiveness of transversus abdominis plane blocks after hysterectomy: A meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2013;166:1–9. doi: 10.1016/j.ejogrb.2012.09.012. [DOI] [PubMed] [Google Scholar]
- 7.Abdallah FW, Halpern SH, Margarido CB. Transversus abdominis plane block for postoperative analgesia after Caesarean delivery performed under spinal anaesthesia? A systematic review and meta-analysis. Br J Anaesth. 2012;109:679–87. doi: 10.1093/bja/aes279. [DOI] [PubMed] [Google Scholar]
- 8.Mishriky BM, George RB, Habib AS. Transversus abdominis plane block for analgesia after Cesarean delivery: A systematic review and meta-analysis. Can J Anaesth. 2012;59:766–78. doi: 10.1007/s12630-012-9729-1. [DOI] [PubMed] [Google Scholar]
- 9.Feroci F, Kroning KC, Scatizzi M. Effectiveness for pain after laparoscopic cholecystectomy of 0.5% bupivacaine-soaked Tabotamp placed in the gallbladder bed: a prospective, randomized, clinical trial. Surg Endosc. 2009;23:2214–20. doi: 10.1007/s00464-008-0301-6. [DOI] [PubMed] [Google Scholar]
- 10.Bamigboye AA, Hofmeyr GJ. Local anaesthetic wound infiltration and abdominal nerves block during caesarean section for postoperative pain relief. Cochrane Database Syst Rev. 2009:CD006954. doi: 10.1002/14651858.CD006954.pub2. [DOI] [PubMed] [Google Scholar]
- 11.Rosaeg OP, Bell M, Cicutti NJ, Dennehy KC, Lui AC, Krepski B. Pre-incision infiltration with lidocaine reduces pain and opioid consumption after reduction mammoplasty. Reg Anesth Pain Med. 1998;23:575–9. doi: 10.1016/s1098-7339(98)90084-0. [DOI] [PubMed] [Google Scholar]
- 12.Lorenzo AJ, Lynch J, Matava C, El-Beheiry H, Hayes J. Ultrasound Guided Transversus Abdominis Plane vs. Surgeon Administered Intraoperative Regional Field Infiltration with Bupivacaine for Early Postoperative Pain Control in Children Undergoing Open Pyeloplasty. J Urol. 2014;192:207–13. doi: 10.1016/j.juro.2014.01.026. [DOI] [PubMed] [Google Scholar]
- 13.Dingemann J, Kuebler JF, Wolters M, von Kampen M, Osthaus WA, Ure BM, Reismann M. Perioperative analgesia strategies in fast-track pediatric surgery of the kidney and renal pelvis: lessons learned. World J Urol. 2010;28:215–9. doi: 10.1007/s00345-009-0442-9. [DOI] [PubMed] [Google Scholar]
- 14.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8:336–41. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 15.Pereira J, Lawlor P, Vigano A, Dorgan M, Bruera E. Equianalgesic dose ratios for opioids. a critical review and proposals for long-term dosing. J Pain Symptom Manage. 2001;22:672–87. doi: 10.1016/s0885-3924(01)00294-9. [DOI] [PubMed] [Google Scholar]
- 16.Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13. doi: 10.1186/1471-2288-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sahin L, Sahin M, Gul R, Saricicek V, Isikay N. Ultrasound-guided transversus abdominis plane block in children: a randomised comparison with wound infiltration. Eur J Anaesthesiol. 2013;30:409–14. doi: 10.1097/EJA.0b013e32835d2fcb. [DOI] [PubMed] [Google Scholar]
- 18.Aydogmus MT, Sinikoglu SN, Naki MM, Ocak NB, Sanli N, Alagol A. Comparison of analgesic efficiency between wound site infiltration and ultrasound-guided transversus abdominis plane block after cesarean delivery under spinal anaesthesia. Hippokratia. 2014;18:28–31. [PMC free article] [PubMed] [Google Scholar]
- 19.Atim A, Bilgin F, Kilickaya O, Purtuloglu T, Alanbay I, Orhan ME, Kurt E. The efficacy of ultrasound-guided transversus abdominis plane block in patients undergoing hysterectomy. Anaesth Intensive Care. 2011;39:630–4. doi: 10.1177/0310057X1103900415. [DOI] [PubMed] [Google Scholar]
- 20.Skjelsager A, Ruhnau B, Kistorp TK, Kridina I, Hvarness H, Mathiesen O, Dahl JB. Transversus abdominis plane block or subcutaneous wound infiltration after open radical prostatectomy: A randomized study. Acta Anaesthesiol Scand. 2013;57:502–8. doi: 10.1111/aas.12080. [DOI] [PubMed] [Google Scholar]
- 21.Sivapurapu V, Vasudevan A, Gupta S, Badhe AS. Comparison of analgesic efficacy of transversus abdominis plane block with direct infiltration of local anesthetic into surgical incision in lower abdominal gynecological surgeries. J Anaesthesiol Clin Pharmacol. 2013;29:71–5. doi: 10.4103/0970-9185.105807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tolchard S, Davies R, Martindale S. Efficacy of the subcostal transversus abdominis plane block in laparoscopic cholecystectomy: Comparison with conventional port-site infiltration. J Anaesthesiol Clin Pharmacol. 2012;28:339–43. doi: 10.4103/0970-9185.98331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ortiz J, Suliburk JW, Wu K, Bailard NS, Mason C, Minard CG, Palvadi RR. Bilateral transversus abdominis plane block does not decrease postoperative pain after laparoscopic cholecystectomy when compared with local anesthetic infiltration of trocar insertion sites. Reg Anesth Pain Med. 2012;37:188–92. doi: 10.1097/AAP.0b013e318244851b. [DOI] [PubMed] [Google Scholar]
- 24.Albi-Feldzer A, Mouret-Fourme EE, Hamouda S, Motamed C, Dubois PY, Jouanneau L, Jayr C. A double-blind randomized trial of wound and intercostal space infiltration with ropivacaine during breast cancer surgery: effects on chronic postoperative pain. Anesthesiology. 2013;118:318–26. doi: 10.1097/ALN.0b013e31827d88d8. [DOI] [PubMed] [Google Scholar]
- 25.Vallejo MC, Phelps AL, Sah N, Romeo RC, Falk JS, Johnson RR, Keenan DM, Bonaventura MA, Edington HD. Preemptive analgesia with bupivacaine for segmental mastectomy. Reg Anesth Pain Med. 2006;31:227–32. doi: 10.1016/j.rapm.2006.02.007. [DOI] [PubMed] [Google Scholar]
- 26.Busch CA, Whitehouse MR, Shore BJ, MacDonald SJ, McCalden RW, Bourne RB. The efficacy of periarticular multimodal drug infiltration in total hip arthroplasty. Clin Orthop Relat Res. 2010;468:2152–9. doi: 10.1007/s11999-009-1198-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bays RA, Barry L, Vasilenko P. The use of bupivacaine in elective inguinal herniorrhaphy as a fast and safe technique for relief of postoperative pain. Surg Gynecol Obstet. 1991;173:433–7. [PubMed] [Google Scholar]
- 28.Trotter TN, Hayes-Gregson P, Robinson S, Cole L, Coley S, Fell D. Wound infiltration of local anaesthetic after lower segment caesarean section. Anaesthesia. 1991;46:404–7. doi: 10.1111/j.1365-2044.1991.tb09558.x. [DOI] [PubMed] [Google Scholar]
- 29.Ventham NT, Hughes M, O’Neill S, Johns N, Brady RR, Wigmore SJ. Systematic review and meta-analysis of continuous local anaesthetic wound infiltration versus epidural analgesia for postoperative pain following abdominal surgery. Br J Surg. 2013;100:1280–9. doi: 10.1002/bjs.9204. [DOI] [PubMed] [Google Scholar]
- 30.Frigon C, Mai R, Valois-Gomez T, Desparmet J. Bowel hematoma following an iliohypogastric-ilioinguinal nerve block. Paediatr Anaesth. 2006;16:993–6. doi: 10.1111/j.1460-9592.2006.01909.x. [DOI] [PubMed] [Google Scholar]
- 31.Jankovic Z, Ahmad N, Ravishankar N, Archer F. Transversus abdominis plane block: how safe is it? Anesth Analg. 2008;107:1758–9. doi: 10.1213/ane.0b013e3181853619. [DOI] [PubMed] [Google Scholar]
- 32.Lancaster P, Chadwick M. Liver trauma secondary to ultrasound-guided transversus abdominis plane block. Br J Anaesth. 2010;104:509–10. doi: 10.1093/bja/aeq046. [DOI] [PubMed] [Google Scholar]
- 33.Wu Y, Liu F, Tang H, Wang Q, Chen L, Wu H, Zhang X, Miao J, Zhu M, Hu C, Goldsworthy M, You J, Xu X. The analgesic efficacy of subcostal transversus abdominis plane block compared with thoracic epidural analgesia and intravenous opioid analgesia after radical gastrectomy. Anesth Analg. 2013;117:507–13. doi: 10.1213/ANE.0b013e318297fcee. [DOI] [PubMed] [Google Scholar]
- 34.Wahba SS, Kamal SM. Analgesic efficacy and outcome of transversus-abdominis plane block versus low thoracic-epidural analgesia after laparotomy in ischemic heart disease patients. J Anesth. 2013;28:517–23. doi: 10.1007/s00540-013-1774-6. [DOI] [PubMed] [Google Scholar]
- 35.Rao Kadam V, Van Wijk RM, Moran JI, Miller D. Epidural versus continuous transversus abdominis plane catheter technique for postoperative analgesia after abdominal surgery. Anaesth Intensive Care. 2013;41:476–81. doi: 10.1177/0310057X1304100407. [DOI] [PubMed] [Google Scholar]
- 36.Niraj G, Kelkar A, Hart E, Horst C, Malik D, Yeow C, Malik D, Yeow C, Singh B, Chaudhri S. Comparison of analgesic efficacy of four-quadrant transversus abdominis plane (TAP) block and continuous posterior TAP analgesia with epidural analgesia in patients undergoing laparoscopic colorectal surgery: an open-label, randomised, non-inferiority trial. Anaesthesia. 2014;69:348–55. doi: 10.1111/anae.12546. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


