Abstract
Objective: To compare correlation between right ventricular ejection fraction (RVEF) derived from MRI and equilibrium radionuclide angiocardiography (ERNA) depicted from the left anterior oblique (LAO) view and anterior (ANT) view [designated as ERNA (LAO) and ERNA (ANT), respectively]. Methods: Twenty-one patients with cardiac disorders received ERNA and cardiac MRI examination within 2 weeks were enrolled in this study. The region of interest (ROI) in right ventricle was depicted from the LAO and anterior (ANT) views to calculate the ERNA (LAO) and ERNA (ANT). Cardiac MRI was performed as served as reference standard to compare correlation between RVEF derived from MRI and ERNA (LAO)/ERNA (ANT), respectively. The repeatability was evaluated according to the intraclass correlation coefficient (ICC). Results: RVEF obtained through MRI was closely correlated with that obtained through ERNA (LAO) view (r=0.883) and ERNA (ANT) view (r=0.891), respectively. Bland-Altam analysis indicated the RVEF derived from the ERNA (LAO) view was obviously underestimated in patients with right ventricular enlargement. Meanwhile, the RVEF derived from the anterior view was much closer to the RVEF derived from MRI compared with that obtained from the LAO view. Conclusions: ERNA is effective for the determination of RVEF. LAO is still preferred for the determination of RVEF, but the RVEF may be underestimated in the patients with right ventricular enlargement. Determination of RVEF based on ANT is solely recommended in the determination of RVEF in patients with right ventricular enlargement and serves as a control.
Keywords: Right ventricular, right ventricular ejection fraction, MRI, equilibrium blood pool imaging
Introduction
Although right ventricle plays important roles in the health and disease historically, knowledge about the role of right ventricle is still lagged behind that of the left ventricle. For patients with severe heart failure and pulmonary disorders, the right ventricular function is closely related to the severity of such conditions [1], and has been acknowledged as a predictor for the prognosis [2].
Right ventricular ejection fraction (RVEF) is an important parameter for the evaluation of right ventricular function. Currently, coronary angiography, with the capacity to display the whole anatomical structure and the hemodynamic features, has been considered as the golden standard for the quantitative analysis of RVEF [3]. However, its application is limited due to the invasive injuries to the individuals. To date, extensive efforts have been made for the development of repeatable and non-invasive methods for the evaluation of parameters associated with right ventricle function (e.g. RVEF). Conventional 2-dimensional echocardiographic images were obtained with the application of Simpson’s rule to determine the RVEF, however, the accuracy of such method was undermined by the irregular geometric profiles of the right ventricle and its location [4]. Real-time 3-dimensional echocardiography (RT-3DE) allows the right ventricle to be viewed in multiple planes, but its accuracy is affected by the low temporal and spacial resolution. Moreover, its imaging quality is lower in adults with fast heart rate and the children [5]. Nowadays, MRI has been considered as the standard method for the non-invasive evaluation of ventricular function [6]. Nevertheless, its application is not satisfactory in patients with implantation of metal devices. In addition, the patients need to hold their breath for a certain duration, which may induce respiratory motion artifact.
First pass radionuclide angiography (FPRNA) has proven to correctly assess the ventricular function, but its application is undermined due to technical difficulties [7,8]. Nowadays, equilibrium radionuclide angiocardiography (ERNA) is also used for the determination of LVEF, but such method leads to no benefits for the long-term follow up and the clinical application due to a large dosage of developer (740~925 MB) and long collection duration. On the contrary, ERNA planar imaging could be used for the calculation of EF based on the dynamic changes of radioactive counting in the ventricular chamber. Such strategy is commonly used in clinical practice as it is not affected by the geometric profile of the ventricle. Meanwhile, a necessity of low dose developer (555~740 MBq) was proposed together with short collection duration [9]. Currently, left anterior oblique (LAO) with a degree of 30 to 45 is commonly used in the image collection and process in the ERNA planar scan. Nevertheless, its efficiency is impaired as the interference caused by overlap of the right atrium and other chambers could not be eliminated [10].
In this study, the region of interest (ROI) in right ventricle was depicted from the LAO and anterior (ANT) view, based on which to calculate the RVEF of LAO and anterior view [designated as ERNA (LAO) and ERNA (ANT), respectively]. In addition, cardiac MRI was performed as served as reference standard to compare correlation between RVEF derived from MRI and ERNA (LAO)/ERNA (ANT), respectively. Moreover, we investigate the effects of image collection and analysis derived from ANT view on the reduction of radioactive count overlapping between the right ventricle and right atrium, based on which to develop a method for the accurate calculation of RVEF.
Materials and methods
Patients
A total of 21 patients (male: 12, female: 9, averaged age 61.6±16.7) with cardiac diseases admitted to our department from March 2009 to December 2013 were included in this retrospective analysis. ERNA planar scan and MRI scan was performed in all patients within 2 weeks after admission. Five patients were diagnosed with coronary heart disease, 8 cases were diagnosed with hypertensive disease, 5 were with myocardiopathy, 2 were congenital heart disease, and 1 was diagnosed with the other disorder. The exclusion criteria were those with frequent arrhythmias, acute cardiac event, hemodynamic instability, fear of confined spaces, as well as contraindications of MRI. Written informed consents were obtained from each patient. The study protocols were approved by the Ethical Committee of Changzhou No. 2 Hospital.
ERNA scan
ERNA scan was performed on a SPECT scanner (GE Millennium V5 SPECT) equipped with a high-resolution low-energy parallel-hole collimator. The acquisition parameters were listed as follows: a 20% symmetric window at 140 keV; a 64×64 matrix; and a Zoom of 3.0. In vivo labeling was conducted, in which sodium pyrophosphate and stannous chloride for injection (containing 1-2 mg stannous chloride dissolved in 20 mL normal saline) was injected via intravenous injection. Twenty minutes later, 370-740 MBq dose of 99mTc-MIBI was injected into the bloodstream through intravenous injection. The patient was requested to be in a supine position, followed by connection of the electrodes for the ECG. The images were collected from three views, including ANT, LAO and left lateral (LL) view, respectively. For the LAO view, the images were collected when the left ventricle could be clearly distinguished from the right ventricle. Acquisitions were gated at 24 frames per R-R cycle. For each view, a total of 500 cardiac cycles were collected. The images were collected by two qualified physicians with imaging background blinded to this study. Subsequently, the ROI in the right ventricle was depicted manually by one physician. The depiction was performed in duplicate, and then the results were automatically analyzed using the EF Analyst software.
Cardiac MRI
Cardiac MRI was performed using the 1.5T MR imaging system (Intera Achieva Nova, Dual, Philips Medical System, Best, the Netherlands). Prior to the MRI scan, all patients were requested to hold their breath. The scan was performed using the ECG-gated technique (Balence sequence). Special cares should be taken to guarantee the quality of the ECG electrodes. In addition, the cardiac coils were carefully placed in order to eliminate the signal loss caused by position difference. Afterwards, the images were analyzed using the EWS workstation. Endocardial surface was depicted through manual and automatic manners, and then the RVEF was calculated accordingly.
Statistical analysis
SPSS 13.0 software was used for the data analysis. All the data were presented mean ± standard deviation. Student’s t test was performed for the inter-group comparison. Spearman correlation analysis was conducted to investigate the correlation between ERNA (LAO)/ERNA (ANT) and MRI. Evaluation of repeatability was performed using intraclass correlation coefficient (ICC) as previously described [11]. The agreement was analyzed using the Bland-Altam method using the MedCalc 12.0 software.
Results
A higher repeatability was obtained in the ERNA (LAO) compared with that of ERNA (ANT). The ICC of ERNA (LAO) was 0.97 while that of ERNA (ANT) was 0.92, indicating the repeatability of ERNA (LAO) was higher than that of ERNA (ANT). For the RVEF of patients (n=5) with right ventricular enlargement, significant difference was observed in the ERNA (LAO) and MRI scan results (43.4±6.73% vs. 50.0±7.31%, t=16.5, P<0.01). However, no statistical difference was observed in the ERNA (ANT) and MRI scan results (49.4±7.76% vs. 50.0±7.31%, t=0.44, P=0.683). The RVEF obtained from the ERNA (LAO) view was remarkably decreased compared with that obtained from the ERNA (ANT) view (43.4±6.73% vs. 49.4±7.77%, t=-5.26, P<0.01). For the RVEF of patients (n=16) without right ventricular enlargement, no statistical difference was observed in the ERNA (LAO) compared with that of MRI (44.18±11.19% vs. 44.0±11.49, vs. t=-2.65, P=0.79). In addition, no statistical difference was identified in the FVEF in the ERNA (ANT) compared with that of MRI (45.93±10.79% vs. 44.0±11.49%, t=-2.0, P=0.064). Nevertheless, statistical difference was noticed in the RVEF of the ERNA (LAO) view compared with that of ERNA (ANT) view (43.4±6.73% vs. 45.93±10.79%, t=-2.57, P<0.05).
The correlation and agreement of RVEF derived from MRI and ERNA (LAO)/ERNA (ANT) were summarized in Table 1. For all the patients, the RVEF obtained using MRI showed no statistical difference compared with that of ERNA (LAO) view (45.42±10.8% vs. 44.0±10.15%, t=1.69, P=0.106). Moreover, the RVEF obtained using MRI showed no difference compared with that of ERNA (ANT) view (45.42±10.8% vs. 46.16±10.0%, t=-1.61, P=0.122). The RVEF obtained through MRI was closely correlated with that obtained through ERNA (LAO) view (r=0.883) and ERNA (ANT) view (r=0.891), respectively. Compared with the RVEF obtained from MRI, all the RVEFs of the ERNA (LAO) view were localized in the 95% CI. The absolute value of the maximal difference between the RVEF obtained from MRI and ERNA (LAO) view was 6, among which 5 patients with right ventricular enlargement showed the maximal bias and their absolute value of RVEF difference was ≥6 (Figure 1 and Table 2). For the RVEF obtained from the MRI and the ERNA (ANT) view, all the data points were distributed in 95% CI, and the absolute value of the maximal difference of the RVEF obtained from MRI and ERNA (ANT) view was 6 (Figure 2). For the patients with right ventricular enlargement, data bias was remarkably decreased, and the absolute value of the RVEF difference was ≤3.
Table 1.
Comparison of RVEF obtained from ERNA and MRI
| Item | RVEF (%) | P value | Spearman correlation | Bland-Altam analysis | ||
|---|---|---|---|---|---|---|
|
| ||||||
| 95% CI | Mean | SD | ||||
| MRI~ERNA (LAO) | 43.45±11.69~41.2±10.21 | 0.106 | r=0.883 | -6.1~9.0 | 1.43 | 3.87 |
| MRI~ERNA (ANT) | 43.45±11.69~42.6±11.32 | 0.122 | r=0.891 | -8.8~6.1 | -1.3 | 2.82 |
Figure 1.
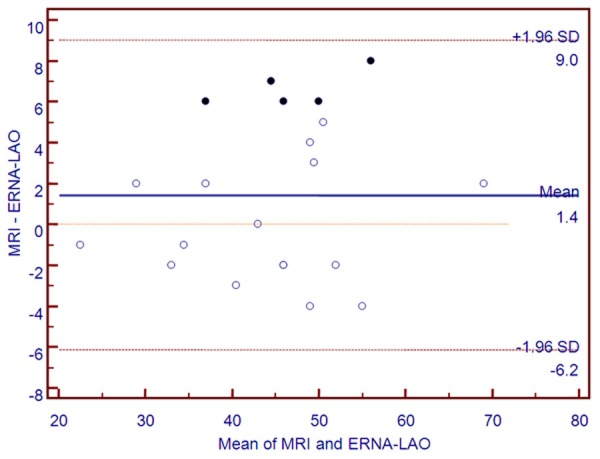
Bland-Altam analysis for the RVEF derived from MRI and ERNA (LAO). Solid center indicated the data of patients with right ventricular enlargement.
Table 2.
Demographic information of the patients with right ventricular enlargement
| Patient No. | Gender | Age (yrs) | Diagnosis | RVEF (%) | Cardiac ultrasonic impressions | ||
|---|---|---|---|---|---|---|---|
|
| |||||||
| MRI | ERNA (LAO) | ERNA (ANT) | |||||
| 01 | Male | 73 | Hypertension | 59 | 52 | 56 | Right atrial enlargement, right ventricular enlargement, tricuspid regurgitation |
| 02 | Male | 80 | Hypertension | 49 | 43 | 52 | Right atrial enlargement, right ventricular enlargement, tricuspid regurgitation |
| 03 | Female | 49 | Congenital heart disease, atrial septal defect | 48 | 41 | 47 | Right atrial enlargement, right ventricular enlargement |
| 04 | Female | 32 | Congenital heart disease, atrial septal defect | 53 | 47 | 55 | Right atrial enlargement, right ventricular enlargement |
| 05 | Female | 36 | Cardiomyopathy | 40 | 34 | 37 | Right atrial enlargement, right ventricular enlargement, tricuspid regurgitation |
Figure 2.
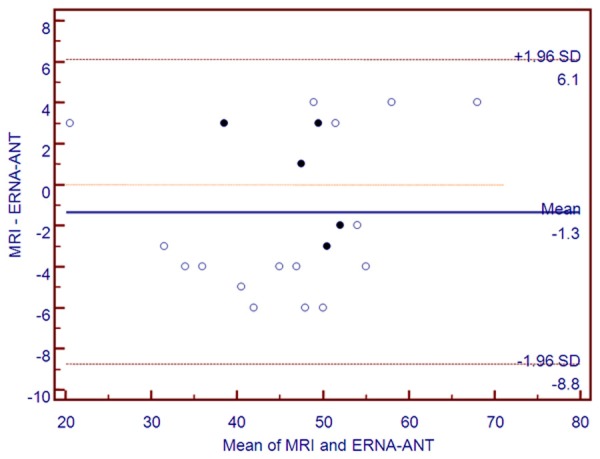
Bland-Altam analysis for the RVEF derived from MRI and ERNA (ANT). Solid center indicated the data of patients with right ventricular enlargement.
Discussion
In the past decades, ERNA with satisfactory repeatability has been commonly used in the evaluation of left ventricle. To date, an increasing number of studies reveals that it can be used for assessment of right ventricular function with reasonable accuracy [12,13]. In these studies, the images were all collected at the LAO view in order to calculate the RVEF. Generally, the right ventricle could be clearly distinguished from the left ventricle at the LAO view, which would contribute to the depiction of the ventricular borders. In a previous study, Nesser et al reported the RVEF derived from ERNA (LAO) was correlated with that derived from MRI (r=0.86), which demonstrated it could be used for the clinical determination of RVEF [14]. However, some researchers indicated partial overlapping between the right ventricle and right atrium at the ERNA (LAO) view (Figure 3). Moreover, underestimation of RVEF was induced as part of the radioactivity of the right atrium may be considered as the time activity curvature of the right ventricle [1]. In this study, the RVEF derived from the ERNA (LAO) view was remarkably decreased in that derived from MRI in the 5 patients with right ventricular enlargement (P<0.01). Bland-Altam analysis indicated a large data bias in these patients together with an absolute value of ≥6 (Figure 1). Therefore, for the patients with right ventricular enlargement, the overlapping radioactive counting would be increased in the presence of enlarged right ventricle and right atrium, which may result in significant underestimation of RVEF. Taken such fact into consideration, the ROI was depicted at the anterior view, based on which to calculate the RVEF. On this condition, the overlapping of right ventricle and right atrium due to the spacial changes was finally the overlapping between the right ventricle and left ventricle (Figure 3B), which could decrease the potential effects of right ventricular enlargement. Our results indicated the RVEF derived from the ERNA (ANT) view in the patients with right ventricular enlargement was remarkably larger than that of the ERNA (LAO) view (t=-5.26, P<0.01), and was similar to that derived from MRI (t=0.44, P=0.683). Meanwhile, Bland-Altam analysis revealed the RVEF derived from the anterior view was much closer to the RVEF derived from MRI compared with that obtained from the LAO view (Figure 2).
Figure 3.
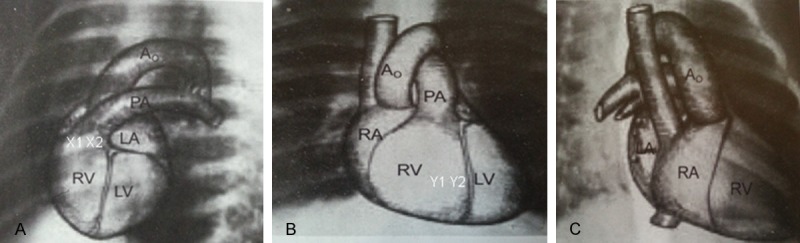
Images of heart derived from LAO view (A), ANT view (B), and RAO view (C). A0, aorta; PA, pulmonary artery; LV, left ventricle; RV, right ventricle; LA, left atrium; RA, right atrium.
In this study, the formula based on which RVEF derived from the ERNA (LAO) and ERNA (ANT) was calculated were presented as follows:
EF (%)=(EDC-ESC)/(EDC-BG) (a)
Where EDC stands for the ventricular end-diastolic radioactive counting (volumes); ESC stands for the ventricular end-systolic volume; BG stands for the background radioactive counting, respectively.
On this basis, the actually forma is as follows:
RVEF (LAO)=[(RVEDC+X1)-(RVESC+X2)]/[(RVEDC+X1)-BG] (b)
Where RVEDC stands for the right ventricular end-diastolic radioactive counting; RVESC stands for the right ventricular end-systolic volume; X1 stands for the overlap between the right ventricular end-diastolic count and the right atrial end-systolic count at the LAO view; X2 stands for the overlap between the right ventricular end-systolic count and the right atrial end-diastolic count.
As the cardiac cycle was completely consistent with that under physiological conditions, the right ventricular end-systolic count, right ventricular end-diastolic count and the background count obtained from LAO view were equalized with those obtained from ANT view. Thus, the previous formula (b) could be transformed as follows:
RVEF (ANT)=[(RVEDC+Y1)-(RVESC+Y2)]/[(RVEDC+Y1)-BG] (c)
Where Y1 stands for the overlap between the right ventricular end-diastolic count and the left ventricular end- diastolic count at the ANT view; Y2 stands for the overlap between the right ventricular end-systolic count and the left ventricular end-systolic count derived from the ANT view.
As revealed in formula (b) and (c), the RVEFs derived from the LAO view and ANT review were relied on the overlapping count. According to the overlapping area and the ventricular and atrial volume in various cardiac cycles, the correlation was ranked in an order of: X1<X2; Y1>Y2; and X1<Y1 (Figure 3). As revealed in the overlapping count, the numerator of the formula (b) was smaller than that of the formula (c). In the presence of right ventricular enlargement, X1 and X2 were increased that resulted in decrease of numerator and increase of denominator of formula (b), which finally led to decrease of calculated RVEF. However, such alternation caused slight or even no difference on the calculation of RVEF (ANT).
A higher repeatability was obtained at the RVEF (LAO) view compared with that of the ANT view (ICC=0.96 vs. ICC=0.92). This is mainly due to the overlapping of the right ventricular margins and the left ventricle, which is difficult for the depiction of the ROI in the right ventricle. On the contrary, less overlapping is noticed in the LAO view as the left ventricle could be distinguished from the right ventricle, which makes the depiction of ROI in right ventricle easily (Figure 4). Thus, in clinical practice, the LAO posture is preferred for the determination of EF. For the depiction of ROI in the right ventricle at the ANT view, we proposed the following tips: (i) enough radioactive count and high resolution are needed for the images. (ii) The right ventricle margin should be firmly distinguished after repeatable observation of the ECG images at ANT view. (iii) Slight right anterior oblique contributes to the depiction of the right ventricular margins.
Figure 4.
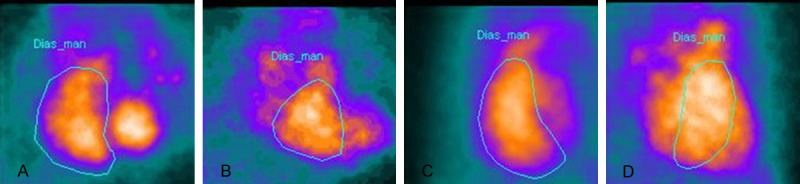
Images of a heart with normal size derived from the LAO view (A), ANT view (B). Images of a heart with right ventricular enlargement derived from LAO view (C) and ANT view (D).
In conclusions, ERNA was effective for the determination of RVEF and showed satisfactory correlation and agreement with that of the MRI results. Thus, it could be used for the determination of right ventricular function. LAO is still preferred for the determination of RVEF; however, the RVEF may be underestimated in the patients with right ventricular enlargement. Determination of RVEF based on ANT is still a challenge due to the depiction of ROI in right ventricle and a lower repeatability. Such method is solely recommended in the determination of RVEF in patients with right ventricular enlargement and serves as a control.
Disclosure of conflict of interest
None.
References
- 1.Haddad F, Doyle R, Murphy DJ, Hunt SA. Right ventricular function in cardiovascular disease, Part II pathophysiology, clinical importance, and management of right ventricular failure. Circulation. 2008;117:1717–1731. doi: 10.1161/CIRCULATIONAHA.107.653584. [DOI] [PubMed] [Google Scholar]
- 2.Brittain EL, Hemnes AR, Keebler M, Lawson M, Byrd BF 3rd, DiSalvo T. Right ventricular plasticity and functional imaging. Pulm Circ. 2012;2:309. doi: 10.4103/2045-8932.101407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gibson CM, Schömig A. Coronary and Myocardial Angiography Angiographic Assessment of Both Epicardial and Myocardial Perfusion. Circulation. 2004;109:3096–3105. doi: 10.1161/01.CIR.0000134278.50359.CB. [DOI] [PubMed] [Google Scholar]
- 4.Haddad F, Hunt SA, Rosenthal DN, Murphy DJ. Right ventricular function in cardiovascular disease, part I anatomy, physiology, aging, and functional assessment of the right ventricle. Circulation. 2008;117:1436–1448. doi: 10.1161/CIRCULATIONAHA.107.653576. [DOI] [PubMed] [Google Scholar]
- 5.Chua S, Levine RA, Yosefy C, Handschumacher MD, Chu J, Qureshi A, Neary J, Ton-Nu TT, Fu M, Wu CJ, Hung J. Assessment of right ventricular function by real-time three-dimensional echocardiography improves accuracy and decreases interobserver variability compared with conventional two-dimensional views. Eur J Echocardiogr. 2009;10:619–624. doi: 10.1093/ejechocard/jep013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Greyson CR. Evaluation of right ventricular function. Curr Cardiol Rep. 2011;13:194–202. doi: 10.1007/s11886-011-0174-5. [DOI] [PubMed] [Google Scholar]
- 7.Friedman JD, Berman DS, Borges-Neto S, Hayes SW, Johnson LL, Nichols KJ, Pagnanelli RA, Port SC Quality Assurance Committee of the American Society of Nuclear Cardiology. First-pass radionuclide angiography. J Nucl Cardiol. 2006;13:e42–e55. doi: 10.1016/j.nuclcard.2006.08.006. [DOI] [PubMed] [Google Scholar]
- 8.Lee JS, Lee JS, Kim SJ, Kim IJ, Kim YK, Choo KS. Comparison of gated blood pool SPECT and spiral multidetector computed tomography in the assessment of right ventricular functional parameters: Validation with first-pass radionuclide angiography. Ann Nucl Med. 2007;21:159–166. doi: 10.1007/s12149-006-0004-9. [DOI] [PubMed] [Google Scholar]
- 9.Hesse B, Lindhardt TB, Acampa W, Anagnostopoulos C, Ballinger J, Bax JJ, Edenbrandt L, Flotats A, Germano G, Stopar TG. EANM/ESC guidelines for radionuclide imaging of cardiac function. Eur J Nucl Med Mol Imaging. 2008;35:851–885. doi: 10.1007/s00259-007-0694-9. [DOI] [PubMed] [Google Scholar]
- 10.Greil GF, Beerbaum P, Razavi R, Miller O. Imaging the right ventricle. Heart. 2008;94:803–808. doi: 10.1136/hrt.2005.079111. [DOI] [PubMed] [Google Scholar]
- 11.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- 12.Konstam MA, Kahn PC, Curran BH, Idoine J, Wynne J, Holman BL. Equilibrium (gated) radionuclide ejection fraction measurement in the pressure or volume overloaded right ventricle. Comparison of three methods. Chest. 1984;86:681–687. doi: 10.1378/chest.86.5.681. [DOI] [PubMed] [Google Scholar]
- 13.Selimovic N, Andersson B, Bech-Hanssen O, Lomsky M, Riise GC, Rundqvist B. Right ventricular ejection fraction during exercise as a predictor of mortality in patients awaiting lung transplantation: A cohort study. BMJ Open. 2013;3 doi: 10.1136/bmjopen-2012-002108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nesser HJ, Tkalec W, Patel AR, Masani ND, Niel J, Markt B, Pandian NG. Quantitation of Right Ventricular Volumes and Ejection Fraction by Three-Dimensional Echocardiography in Patients: Comparison with Magnetic Resonance Imaging and Radionuclide Ventriculography. Echocardiography. 2006;23:666–680. doi: 10.1111/j.1540-8175.2006.00286.x. [DOI] [PubMed] [Google Scholar]


