Abstract
Objective: There is currently no general consensus on the optimal treatment of chronic radial head dislocation. Material and Methods: Considering that the annular ligament is important in maintaining elbow stability, we developed a modified method for annular ligament reconstruction in pediatric cases of radial head dislocation without ulnar bowing. We retrospectively investigated the therapeutic outcomes of this technique in a series of cases. We used our modified technique for the treatment of five patients between January 2006 and January 2012. The average age of the patients at the time of injury was 9 years (range, 6-14 years), and the patients were followed up for 1 to 3 years. Results: The perioperative and follow-up data of the patients were examined. All five surgical procedures were completed uneventfully and had been tolerated well by the patients, with minimal complications. Remarkable improvement was noted in all the cases at the end of the follow-up period. Conclusions: Our modified technique for annular ligament reconstruction was effective in achieving good reduction of the radial head dislocation with minimal complications in pediatric cases of isolated radial head dislocation without apparent ulnar bowing.
Keywords: Monteggia’s fracture, radial head dislocation, elbow stability, annular ligament
Introduction
Isolated radial head dislocations are rare in children [1] and often occur in patients with a history of Monteggia fractures. The lesion is generally detected in cases where the fracture fixation is inadequate or when the dislocation may have been missed at the initial examination. Occasionally, it is accompanied by palsy of the radial nerve. Radial head dislocation can lead to restricted motion, cubitus deformity, pain, degenerative arthritis, and palsy [2-6]. Several treatment strategies have been proposed for this dislocation, including a conservative approach [7] and open reduction of the radial head along with reconstruction of the annular ligament and/or ulnar osteotomy to maintain the rotational stability of the forearm. The annular ligament plays a fundamental role in maintaining the position of the radial head and the stability of the elbow joint. Therefore, we developed a modified version of the conventional techniques for radial head reduction with reconstruction of the annular ligament. In this paper, we present our findings on the outcomes of this modified technique of annular ligament reconstruction in a series of five cases.
Patients and method
Study protocol
This was designed as a retrospective study of the five cases of unreduced post-traumatic radial head dislocation treated at our hospital between from January 2006 and January 2012. The protocol and study design were reviewed and approved by the local Human Ethics Committee, and all clinical work was completed at the local Hospital.
Patients
The inclusion criteria for the present study were unreduced post-traumatic radial head dislocations and patient age less than 18 years (Table 1). The exclusion criteria were apparent ulnar deformities. The patients included one girl and four boys, with average age of 9 years (range, 6 years to 14 years); the injuries had occurred 2 months to 2 years before presentation at our hospital. None of the 5 patients had received previous treatment at a hospital for the radial head dislocation, and closed reduction was not possible in any of the cases. One of the patients also had radial nerve palsy. All five patients underwent reconstruction of the annular ligament and were reviewed every 3 months. The follow-up period ranged from 1 to 3 years (mean, 2 years). The parameters assessed during the follow up were as follows: the position of the radial head and presence of any osteoarthritic changes or deformities, as observed in the anteroposterior and lateral radiographs; the range of motion (ROM) of both elbows; and pain, elbow stability, and ability to perform daily activities, as evaluated by the patients themselves. Informed consent was obtained
Table 1.
Clinical characteristics of the five patients with isolated radial head dislocation
| Case | Age (y) | Sex | Duration between the trauma and surgery | Follow-up period (y) | Preoperative status of elbow flexion/extension | Preoperative status of forearm pronation/supination | Postoperative status of elbow flexion/extension | Postoperative status of forearm pronation/supination | Carrying angle (valgus) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 6 | F | 2 months | 1 | 120/0° | 50/60° | 135/0° | 75/90° | 9° |
| 2 | 9 | M | 6 months | 2 | 115/0° | 60/60° | 135/0° | 90/90° | 8° |
| 3 | 7 | M | 9 months | 3 | 130/0° | 50/60° | 135/0° | 90/90° | 6° |
| 4 | 14 | M | 2 years | 3 | 100/0° | 40/50° | 135/0° | 90/90° | 11° |
| 5 | 11 | M | 1 year | 2 | 110/0° | 60/80° | 135/0° | 90/90° | 5° |
Surgical technique
The surgery in all the five cases was performed by the same, highly experienced orthopedic trauma surgeon. The surgery was performed with the patient lying in the prone position with the elbow flexed. The posterolateral approach was used since this approach is most feasible for harvesting the triceps tendon (Figure 1). After identification of the joint capsule, the annular ligament, which may be intacted but displaced or ruptured and obstructed the radial head reduction, was located. Then, the intra-articular spaces of the radiocapitellar and the proximal radioulnar joints were cleared of debris by removing any fragments of interposed capsule, ligament, or osteochondral tissue. Reduction of the radial head was then attempted. The congruity between the radial head and the capitellum was then checked for by intraoperative fluoroscopy. If this congruity was obtained, ligament reconstruction was undertaken.
Figure 1.

The skin incision extends from about the central portion of the triceps up to the level just past the radial neck, along the lateral ulnar border. The radiocapitellar joint was exposed between the anconeus and the extensor carpi ulnaris.
First, two bone tunnels were created using a 4.5-mm drill at the level of annular ligament (Figure 2A). A 1-0 absorbable suture [Coated Vicryl™ (polyglactin 910) Suture; (Ethicon, Inc., Somerville, NJ)] was routed through the tunnels (Figure 2B). A strip of tissue with width of 1 cm and length of 7-9 cm was obtained from the central portion of the triceps tendon, taking special care to preserve its insertion at the olecranon. The tendon strip reconstruction material was 3 cm longer than the length of the suture, and it was advanced in a manner similar to the suture (Figure 2C). The reduction of the dislocation at the proximal and distal radioulnar joints was confirmed through intraoperative fluoroscopy.
Figure 2.
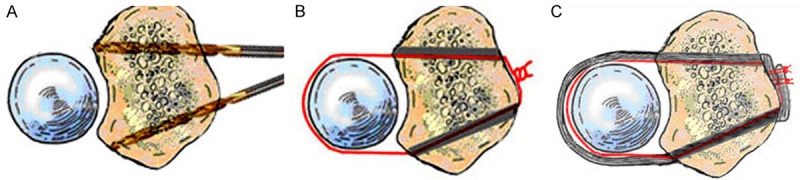
A: One bone tunnel (anterior) was made transversely across the ulna (anterior), while the other one (posterior) was made obliquely. The two drill holes exited the ulna at the point of attachment of the annular ligament. B: A 1-0 absorbable suture was introduced through the first tunnel anteriorly, routed around the neck, advanced posteriorly through the second drill hole, and tied to itself. C: The tendon strip was advanced in the same manner as the suture. The end of the tendon strip was tightened and tied with the suture.
Postoperative care
A long-arm cast was applied for two weeks, with the forearm positioned at 90 degrees of supination (Figure 4). After the removal of the cast, self-managed forearm pronation and supination was recommended for two weeks, followed by rehabilitation exercises for elbow flexion and extension two weeks later.
Figure 4.

Postoperative images of the right elbow obtained in the A-P view (left) and lateral view (right): The images show reduction of the dislocation of the radial head of the 10-year-old boy.
Results
The procedure was tolerated well by all the five patients, without any perioperative complications. The postoperative radiographs showed good reduction of the dislocation of the radial head. At the follow-up visits, all patients reported that they were free of pain and able to perform their daily activities. The ROM of the elbow was limited immediately after the removal of the plaster cast, but gradually increased over time, with complete restoration of the elbow movement about 8 months after the procedure. The ROM for the elbow is recorded in Table 1. In all the cases, the postoperative ROM was greater than the preoperative one, indicating definitive improvement. With regard to clinical appearance, in four of the cases, the elbows appeared normal. In one case, supination was lost to some extent (75°), but the carrying angle was the same as that on the other side. The radiographs obtained at the follow-up visits showed no degenerative change, substantial radial head deformity, or redislocation. Further, the growth plate of the radial head had remained unaffected in all the five cases.
Illustrative case report
A 10-year-old boy sustained an injury to his right elbow due to a fall (Case 1, Table 1). The patient had a Monteggia fracture, with proximal ulnar dislocation of the radial head. Closed reduction of the fracture was performed, and the elbow placed in a cast for 4 weeks. After removal of the cast, the patient had instability in his forearm, paresthesia in the area of the distribution of the radial nerve, and weakness in wrist extension and finger flexion. Two months after the injury, the patient was referred to our hospital for further evaluation. Clinical examination revealed no apparent ulnar bowing. Elbow flexion was 5-140°, pronation, 70°; and supination, 90°. Radiographs showed the persistence of the anterolateral dislocation of the radial head (Figure 3). Further, electromyography confirmed damage to the posterior interosseous nerve.
Figure 3.

Preoperative radiographs of the right elbow obtained in the A-P view (left) and lateral view (right): The images show the anterolateral dislocation of the radial head in a 10-year-old boy.
The patient underwent reconstruction of the annular ligament and received postoperative treatment as described above (Figure 4). Within 4 months of the surgery, the patient was able to resume full activity without any pain. Follow-up radiographs obtained 1 year after the operation showed an intact radial head and the absence of osteoarthritic changes and elbow deformity.
Discussion
In this study, we examined the outcomes of a modified technique for annular ligament reconstruction in pediatric cases of isolated radial head dislocation and found that the technique enabled good reduction of the radial head dislocation and restored the elbow function with minimal complications. Below, we examine in details the various aspects of the findings of this study.
Is reconstruction of the annular ligament necessary?
The annular ligament is essentially a strong band of fibers that encircles about four-fifths of the radial head and attaches to the lesser sigmoid notch of the ulna. The ligament is a component of the lateral ligament complex along with the radial collateral ligament, lateral ulnar collateral ligament, and accessory lateral collateral ligament [8-11]. Several studies have shown that the annular ligament plays an important role in maintaining the stability of the proximal radioulnar and humeroradial joints of the elbow [12-14]. Dunning et al. have shown that if the annular ligament is left intact, transection of the radial collateral ligament or the lateral ulnar collateral ligament alone would not compromise the posterolateral rotatory stability of the elbow [13]. Further, Karol Galik et al. found that during forearm rotation, the anteroposterior movement of the radial head is greater than its mediolateral movement and that the loss of the annular ligament function increases the latter movement [15]. Cohen and Hastings have also shown that lateral elbow stability was provided by the annular ligament [12]. Put together, these evidences highlight the importance of the annular ligament in maintaining normal elbow kinematics by functioning as a constraint of the radial head.
How to reconstruct the annular ligament?
Several resources have been used for the reconstruction of the annular ligament: grafts from the fascial strips of the forearm [16,17], fascia lata [4,18], tendon of palmaris longus [19], triceps tendon [3-7,19-21], and extensor aponeurosis [19] as well as nylon thread [16]. However, each of these tissues has its own drawbacks. The forearm fascia and tendon of the palmaris longus are too weak to restrict the radius. Further, an additional incision is required for harvesting the fascia lata. Non-absorbable artificial suture materials, such as nylon, are unyielding and cannot accommodate the continued radial growth, thereby possibly leading to the narrowing of the radial neck. Bell Tawse and Lloyd-Roberts et al. have reported good outcomes with the use of the slip of the triceps fascia [3,19]; therefore, we used the same material and similarly obtained good results.
The annular ligament is generally reconstructed using any of the following three techniques. (1) The one-hole technique described by Bell-Tawse, wherein a strip of the triceps tendon is passed around the radial neck and through a drilled hole in the ulna with a diameter greater than that of the tendon strip [3]. Lloyd-Roberts and Oner modified the procedure by performing both reconstruction of the annular ligament and ulnar osteotomy [19,20]. (2) The two-hole technique: In their technique, Seel and Peterson drilled two holes into the proximal ulna at the original sites of the normal attachment of the annular ligament [22]. (3) In the third technique, small bone staples and bone-anchoring devices are used as alternatives to drilling holes into the bone [23]. We chose the two-hole technique over the others since it allowed the securing of the radial head in its normal position and provided an osseous anchorage for the new ligament.
Why did we use the absorbable suture?
Some investigators recommend the use of a humeroradial or radioulnar Kirschner wire to secure the reduced radial head in position during the reconstruction of a new annular ligament [24]. However, we have observed that the use of the Kirschner wire can cause elbow stiffness and that pin failure can sometimes occur. Therefore, we used an absorbable suture to secure the radial head. There was no instance of redislocation in this study, which suggests that the absorbable suture was strong enough to prevent failure of the reduction. Furthermore, initiation of early exercise under the protection of the absorbable suture would be beneficial in preventing the development of subsequent elbow stiffness.
In addition, some other complications, such as osteolytic changes and narrowing or growth disturbance of the radial neck, may arise due to excessive pressure by the newly reconstructed ligament on the radial neck [6,7,10,13,15]. We could avoid this excessive pressure exerted by the reconstructed ligament on the radial head by using an absorbable suture. The suture would retain 100% strength for about 2 weeks, after which it would begin to dissolve and disappear completely within 56 to 70 days [25]. The absorbable suture could provide the initial stability necessary for the newly reduced joint and gradually loosen over the next two weeks, when the cast was removed; eventually, over the next 2 months, the suture would have only minimal restrictive effect on the proximal radioulnar joint. Thus, tension on the radial neck from the absorbable suture would decrease within a short period of time, during which the newly reconstructed ligament would attach firmly to the ulna.
With regard to physical appearance, four elbows were normal, while one lost supination (75°) to a small degree; this was probably due to the long interval between the initial injury and the reconstruction surgery in that case (2 years).
Is it unnecessary to perform osteotomy of the ulna?
According to Lincoln and Mubarak, the term isolated traumatic dislocation of the radial head may be a misnomer; they suggested that the injury was more accurately described as a minimal Monteggia fracture-dislocation and that it is often associated with plastic bowing of the ulna. They recommended that the maximum ulnar bow should be measured to detect ulnar bowing. For the measurement, a straight line is drawn on the lateral roentgenogram of the forearm along the dorsal border of the ulna from the level of the olecranon to the distal ulnar metaphysis. The presence or absence of ulnar bowing is determined by the maximal distance between this line and the ulnar shaft: a value of >1 mm may signify the presence of ulnar bowing, while a value of <1 mm indicates that the deformity does not significantly affect the rotation stability of the forearm [26]. In cases of apparent bowing of the ulna, osteotomy may be necessary. Ligament reconstruction alone would be insufficient to stabilize the radial head in cases of malalignment [8,27]. None of the five patients in this study had ulnar bowing of >1 mm. Therefore, osteotomy of the ulna was not required in any of the cases.
In conclusion, our findings in this case series showed that pediatric cases of isolated radial head dislocation can be successfully managed with minimal complications by using our modified technique for the reconstruction of the annular ligament. Osteotomy of the ulna may be avoided in the absence of the apparent ulnar bowing.
Acknowledgements
This subject is funded by National Natural Science Foundation of China (Nos. 11272134 and 11432016).
Disclosure of conflict of interest
None.
References
- 1.Kim HT, Conjares JNV, Suh JT, Yoo CI. Chronic radial head dislocation in children, Part 1: pathologic changes preventing stable reduction and surgical correction. J Pediatr Orthop. 2002;22:583. [PubMed] [Google Scholar]
- 2.Bell Tawse AJ. The treatment of malunited anterior Monteggia fractures in children. J Bone Joint Surg Br. 1965;47:718–723. [PubMed] [Google Scholar]
- 3.Cappellino A, Wolfe SW, Marsh JS. Use of a modified Bell Tawse procedure for chronic acquired dislocation of the radial head. J Pediatr Orthop. 1998;18:410. [PubMed] [Google Scholar]
- 4.Gyr BM, Stevens PM, Smith JT. Chronic Monteggia fractures in children: outcome after treatment with the Bell–Tawse procedure. J Pediatr Orthop B. 2004;13:402. doi: 10.1097/01202412-200411000-00011. [DOI] [PubMed] [Google Scholar]
- 5.Horii E, Nakamura R, Koh S, Inagaki H, Yajima H, Nakao E. Surgical treatment for chronic radial head dislocation. J Bone Joint Surg Am. 2002;84:1183–1188. doi: 10.2106/00004623-200207000-00014. [DOI] [PubMed] [Google Scholar]
- 6.Thompson JD, Lipscomb AB. Recurrent radial head subluxation treated with annular ligament reconstruction: A case report and follow-up study. Clin Orthop Relat Res. 1989;246:131. [PubMed] [Google Scholar]
- 7.Pollen AG. Fractures and dislocations in children. 1973 [Google Scholar]
- 8.Bozkurt M. The Annular Ligament: An Anatomical Study. Am J Sport Med. 2005;33:114–118. doi: 10.1177/0363546504266070. [DOI] [PubMed] [Google Scholar]
- 9.Cohen MS, Bruno RJ. The collateral ligaments of the elbow: anatomy and clinical correlation. Clin Orthop Relat Res. 2001:123–130. doi: 10.1097/00003086-200102000-00014. [DOI] [PubMed] [Google Scholar]
- 10.Hannouche D, Begue T. Functional anatomy of the lateral collateral ligament complex of the elbow. Surg Radiol Anat. 1999;21:187–191. doi: 10.1007/BF01630899. [DOI] [PubMed] [Google Scholar]
- 11.O’Driscoll SW, Horii E, Morrey BF, Carmichael SW. Anatomy of the ulnar part of the lateral collateral ligament of the elbow. Clin Anat. 1992;5:296–303. [Google Scholar]
- 12.Cohen MS, Hastings H 2nd. Rotatory Instability of the Elbow. The Anatomy and Role of the Lateral Stabilizers. J Bone Joint Surg Am. 1997;79:225–233. [PubMed] [Google Scholar]
- 13.Dunning CE, Zarzour ZD, Patterson SD, Johnson JA, King GJ. Ligamentous stabilizers against posterolateral rotatory instability of the elbow. J Bone Joint Surg Am. 2001;83:1823–1828. doi: 10.2106/00004623-200112000-00009. [DOI] [PubMed] [Google Scholar]
- 14.Søjbjerg J, Ovesen J, Gundorf C. The stability of the elbow following excision of the radial head and transection of the annular ligament. Arch Orthop Trauma Surg. 1987;106:248–250. doi: 10.1007/BF00450463. [DOI] [PubMed] [Google Scholar]
- 15.Galik K, Baratz ME, Butler AL, Dougherty J, Cohen MS, Miller MC. The effect of the annular ligament on kinematics of the radial head. J Hand Surg. 2007;32:1218–1224. doi: 10.1016/j.jhsa.2007.06.008. [DOI] [PubMed] [Google Scholar]
- 16.Fowles JV, Sliman N, Kassab M. The Monteggia lesion in children. Fracture of the ulna and dislocation of the radial head. J Bone Joint Surg Am. 1983;65:1276. [PubMed] [Google Scholar]
- 17.Letts M, Locht R, Wiens J. Monteggia fracture-dislocations in children. J Bone Joint Surg Br. 1985;67:724. doi: 10.1302/0301-620X.67B5.4055869. [DOI] [PubMed] [Google Scholar]
- 18.Attarian D. Annular ligament reconstruction in chronic posttraumatic radial head dislocation in children. Contemp Orthop. 1993;27:259. [PubMed] [Google Scholar]
- 19.Lloyd-Roberts G, Bucknill T. Anterior dislocation of the radial head in children: aetiology, natural history and management. J Bone Joint Surg Br. 1977;59:402. doi: 10.1302/0301-620X.59B4.925049. [DOI] [PubMed] [Google Scholar]
- 20.Oner F, Diepstraten A. Treatment of chronic post-traumatic dislocation of the radial head in children. J Bone Joint Surg Br. 1993;75:577–581. doi: 10.1302/0301-620X.75B4.8331112. [DOI] [PubMed] [Google Scholar]
- 21.Papandrea R, Waters PM. Posttraumatic reconstruction of the elbow in the pediatric patient. Clin Orthop Relat Res. 2000;370:115. doi: 10.1097/00003086-200001000-00011. [DOI] [PubMed] [Google Scholar]
- 22.Seel MJ, Peterson HA. Management of chronic posttraumatic radial head dislocation in children. J Pediatr Orthop. 1999;19:306. [PubMed] [Google Scholar]
- 23.Beaty JH, Rockwood CA, Kasser JR. Rockwood and Wilkins’ fractures in children. Lippincott Williams & Wilkins; 2009. [Google Scholar]
- 24.Haugstvedt JR. Dissociations of the Radius and Ulna: Surgical Anatomy and Biomechanics. Hand Surg. 2004:615–644. [Google Scholar]
- 25.Gomez-Alonso A, Garcia-Criado F, Parreno-Manchado F, Garcia-Sanchez J, Garcia-Sanchez E, Parreno-Manchado A, Zambrano-Cuadrado Y. Study of the efficacy of Coated VICRYL Plus ® Antibacterial suture (coated Polyglactin 910 suture with Triclosan) in two animal models of general surgery. J Infect. 2007;54:82–88. doi: 10.1016/j.jinf.2006.01.008. [DOI] [PubMed] [Google Scholar]
- 26.Lincoln TL, Mubarak SJ. “Isolated” traumatic radial-head dislocation. J Pediatr Orthop. 1994;14:454–457. doi: 10.1097/01241398-199407000-00006. [DOI] [PubMed] [Google Scholar]
- 27.Inoue G, Shionoya K. Corrective ulnar osteotomy for malunited anterior Monteggia lesions in children. 12 patients followed for 1-12 years. Acta Orthop Scand. 1998;69:73–76. doi: 10.3109/17453679809002361. [DOI] [PubMed] [Google Scholar]


